We continue our special project on psoriasis. The first article in the series allows you to get a general idea of this common disease. And this time we will talk about the molecular mechanisms that cause psoriatic rashes, the subtle interactions between skin cells and immune cells that lead to the development of the disease, the molecules by which cells transmit danger signals to each other, and the molecular scars that are visible in the skin cells even when, it would seem, all the symptoms of the disease have disappeared.
Introduction
According to modern concepts, psoriasis is a multifactorial disease that develops in people with a genetic predisposition under the influence of the external environment. Until now, the pathogenesis of psoriasis has not been fully studied, but over the past decades, scientists have made great progress in its research: they have found explanations for previously observed clinical phenomena, established mechanisms of interaction between cells of the immune system and skin cells, and identified the relationship between the pathogenesis of psoriasis and other diseases. This article focuses on the pathogenesis of psoriasis; the genetic and epigenetic aspects of the disease will be described separately.
As already mentioned in the introductory article [1], with psoriasis, patients with psoriasis develop raised, reddened areas on the skin - plaques. Their appearance is associated with two processes: inflammation in the skin and hyperplasia (overgrowth) of the epithelium. Apparently, the reason for this is misregulation of the interaction of the immune system with skin cells [2]. Therefore, in order to understand the pathogenesis of psoriasis, you first need to learn a little about the structural features of the skin and the principles of operation of the immune system.
The skin I live in
Figure 1. Skin structure.
website bono-esse.ru
Skin is the largest human organ. Taking into account subcutaneous fat tissue, it amounts to up to 17% of body weight.
The skin consists of three main parts (Fig. 1).
- The epidermis is precisely that superficial part of the skin, accessible to our eyes, that peels off after a sunburn or forms calluses after mechanical stress. Thanks to the epidermis, the body's protective barrier is formed from pathogenic bacteria, fungi, viruses, temperature, ultraviolet radiation, water loss and mechanical damage. The epidermis is formed by several types of cells, but the most common type (up to 90% of the total) is keratinocytes . They are called so because they produce the structural protein keratin in huge quantities. The epidermis consists of five layers: basal, spinous, granular, shiny and horny (Fig. 2). Keratinocytes of the basal layer actively divide, displacing older cells to the surface of the skin. On the way to the surface, the cells differentiate - they flatten, become keratinized (produce huge amounts of keratin) and, gradually dying, lose their nuclei. At different stages of differentiation, keratinocytes look different under a light microscope; their appearance gives the name to the layers of the epidermis: basal - cells located on the basement membrane; spinous - cells with spine-like processes; granular - cells containing accumulations of proteins and fats in the form of grains in the cytoplasm; shiny - cells with shiny protein eleidin; horny - horny plates (nuclear-free, keratinized cells). melanocyte cells , which synthesize the pigment melanin, which is responsible for protecting the skin from UV rays, and immune cells (primarily dendritic cells), which are the first to encounter infectious and non-infectious agents that have penetrated the skin.
- The dermis is the deeper part of the skin, separated from the epidermis by a thin layer of basement membrane, formed by blood vessels and structural proteins (primarily collagen and elastin). The dermis consists of two layers: the papillary layer, rich in nourishing vessels, and the reticular layer, rich in proteins responsible for the strength and elasticity of the skin. The main and most numerous cells of this part of the skin are fibroblasts , which secrete collagen and elastin. Also present in the dermis are single melanocytes and some immune cells, primarily macrophages .
- Hypodermis is subcutaneous fatty tissue formed by adipocyte . Since fat is an excellent heat insulator and also an energy depot, the hypodermis performs thermoregulatory and energy functions. In addition, the fiber layer serves as additional protection for underlying tissues from damage.
Figure 2. Five layers of the epidermis.
website
Also in the skin there are sebaceous and sweat glands that open their ducts on its surface, hair follicles, nerve fibers and nerve endings.
Phenotyping of bronchial asthma - the path to personalized therapy
BA is a chronic immunoinflammatory disease of the respiratory tract, manifested by hypersensitivity of the respiratory tract, hypersecretion of mucus, progressive bronchial obstruction and developing as a result of allergic inflammation with the participation of eosinophils, basophils, mast cells, neutrophil granulocytes and various subpopulations of T and B lymphocytes [35]. Previously, asthma was considered an allergic disease with the development of inflammation according to the type of Th2 activation with the synthesis of cytokines: IL-4, IL-5, IL-9 and IL-13 (allergic inflammation type 2), which is normally designed to carry out protective reactions on mucous membranes in barrier tissues . Currently, the world recognizes the division of AD into phenotypes and endotypes, the existence of which was mentioned in the domestic literature by A.D. Ado and G.B. Fedoseev back in the 1970s.
According to GINA-2019, asthma is currently considered a heterogeneous disease, and the most common asthma phenotypes are allergic, non-allergic, late-onset asthma, asthma with fixed bronchial obstruction, and obesity-associated asthma. Basically, asthma can be divided into two broad phenotypes: 1) caused by type 2 inflammation (type 2 high phenotype or T2 asthma), occurring in 50–70% of patients, and 2) not associated with type 2 inflammation (type 2 low phenotype). or non-T2 asthma).
From an immunological point of view, this division was made according to the severity of activation mainly of Th2, ILC2 and the levels of their synthesis of the corresponding cytokines. The first phenotype (T2 high) with a high degree of T2 activation is most often found in patients with allergic asthma, characterized by eosinophilic inflammation, eosinophilia and increased levels of IL-4, IL-5 and IL-13 in the lavage and blood plasma of patients, as well as high levels of mast cells and increased expression of periostin in lung tissue. The most clear biomarkers of this phenotype are: increased levels of IgE in plasma, the number of eosinophils in bronchoalveolar lavage and peripheral blood, and increased levels of nitric oxide (FeNO) in exhaled air [36]. For the second phenotype (T2 low), the synthesis of IL-4, IL-5, IL-13 is not so pronounced, and it is characterized by variants of either neutrophilic or polygranulocytic (mixed) inflammation, possibly associated with activation of Th1 and Th17. In addition, AD is further divided into subtypes based on the age of onset of the disease, body mass index, smoking, IgE level in the blood plasma, dependence on physical activity, etc. [36, 37].
Due to the fact that cytokines act as the most important mediators in the development of allergic inflammation, attempts are being made to therapeutically influence the balance of endogenous cytokines in allergies in the form of anti-cytokine biological therapy. Currently, several monoclonal antibody drugs (MAbs) are approved for anti-cytokine biological therapy of patients with AD: dupilumab (MAbs against the common alpha subunit of the IL-4/IL-13 receptors), mepolizumab and reslizumab (both MAbs against IL-5), benralizumab (mAb against the alpha subunit of the IL-5 receptor). Biological therapy with MAT drugs improves asthma control, reduces the severity of clinical manifestations and dependence on the use of glucocorticoids [36, 38]. Research is underway on the use of anti-cytokine therapy in patients with asthma: against cytokines that stimulate the functions of neutrophil granulocytes - IL-8, IL-17, IL-23; against pro-inflammatory cytokines TNF, IL-6 and IL-1; against cytokines that regulate the early stages of allergic inflammation - TSLP, IL-25, IL-33, as well as some others [38].
Mab therapy against Th2 cytokines in the first stages of clinical trials did not produce the expected results. A new wave of interest in anti-cytokine therapy of AD using MAbs against Th2 and Th9 cytokines has appeared in connection with the recognition of the heterogeneity of this disease and the widespread use of the principle of dividing AD patients into phenotypes in clinical practice. Most approaches to anti-cytokine therapy for AD are aimed at treating patients with a Th2 high phenotype, because in this case there are clearer criteria for response to treatment in the form of well-defined biomarkers (levels of eosinophils and cytokines IL-4, IL-5, IL-13). Polygranulocytic inflammation in patients with a low Th2 phenotype is more difficult to assess; these asthma patients respond better to bronchodilator therapy, worse to steroids, but are insensitive to existing anti-cytokine therapy directed against Th2 cytokines [37].
The division of AD into phenotypes and endotypes has made it possible to achieve significant results in the treatment of various MAbs against Th2 cytokines. The use of anti-IL-4 mAb was not effective in the general group of patients with BA, but it turned out to be clinically effective in the group of patients with eosinophilic BA with a high content of eosinophils and in the group of patients with withdrawal of inhaled steroids. This was accompanied by a decrease in IgE levels, the release of eosinophils into the lungs, inflammation and remodeling of lung tissue. MAbs against IL-13 also showed low efficacy in the general group of BA patients and were effective only in a selected group of patients with high levels of IL-13 in lavage. MAbs against IL-5 (reslizumab) and against the IL-5 receptor (benralizumab) led to a decrease in eosinophilia without clinical efficacy in the general group of patients with asthma, but were effective in the group of patients with frequent exacerbations and increased levels of eosinophils in the respiratory tract. Anti-IL-9 mAbs showed average effectiveness in the general group, but were more effective in the group of patients with bronchoconstriction during exercise [39].
On the body's defense
The immune system is a system of organs and cells that protect the body from pathogens: viruses, bacteria, protozoa, helminths, and so on. Every day the body encounters millions of microbes, many of which are pathogens, but due to immune responses, diseases rarely develop. The reason the immune system fights enemies so well is that it can identify them very precisely: it can recognize the characteristic pieces of molecules of the pathogens that attack it, mainly the substances with which they are coated. Such pieces are called antigens.
In order to communicate with each other, immune cells release special information molecules - cytokines.
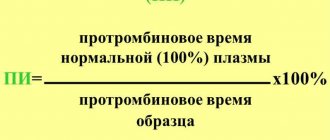
Cytokines can be either stimulating (“we’ve been attacked, call everyone up!”) or inhibitory (“false alarm, let’s return to peaceful life!”). In principle, cytokines can be released by all cells of the body, but immune cells communicate in the language of cytokines especially actively. The table below lists the main groups of cytokines and their functions. Table. Cytokines are molecules produced by immune and non-immune cells that play an important role in regulating the immune response.
| Name | Function | Some representatives* | |||||
| Interferons | A group of molecules released by cells in response to viral invasion; have similar properties and antiviral effects | Interferons alpha (IFN-α), beta (IFN-β), gamma (IFN-γ) | |||||
| Chemokines | Small proteins produced in cells and tissues when a pathogen appears; stimulate cell migration, adhesion and activation | CXC, CC, CX3C, XC | |||||
| Tumor necrosis factors | Proteins synthesized mainly by monocytes and macrophages; cause necrosis of tumor cells and enhance the immune response | Tumor necrosis factors alpha (TNF-α), beta (TNF-β, also known as lymphotoxin-α) | |||||
| Interleukins | Soluble peptides synthesized mainly by T lymphocytes; in isolation stimulate groups of cells to divide or differentiate. Have pro- and anti-inflammatory effects depending on the interleukin and the cell | IL-6, IL-17, IL-23 | |||||
| Hemopoietins | A group of molecules with similar properties; stimulate the reproduction and differentiation of blood cells | Colony-stimulating factors (CSF) | |||||
| Transformative growth factors | Proteins that control proliferation, cell differentiation and other functions in most cells, including immune cells | Transforming growth factor alpha (TGF-α), beta (TGF-β) | |||||
| * Some cytokines have multiple effects and can belong to several groups at once (for example, IL-8 is the chemokine CXCL8, and IL-2-4 affect hematopoiesis) | |||||||
There are two types of immunity: innate and acquired.
- Innate immunity is the sum of all evolutionarily ancient immune cells (among them macrophages, dendritic cells, blood granulocytes, etc.) and molecules (antimicrobial peptides, lysozyme, a special group of proteins called the “complement system”, etc.). Innate immune cells are able to nonspecifically (by antigens common to different groups of foreign agents) recognize pathogens and, attracting other immune cells and molecules, immediately destroy them. Two types of innate immune cells are especially important in the pathogenesis of psoriasis: dendritic cells and neutrophils . Below we will talk about these cells in more detail. Although innate immunity is indispensable for a quick reaction to an enemy, its work lacks specificity: if, for example, one bacteria multiplies very strongly in the body, then innate immunity will lose in the fight against it - it will win in numbers. On the other hand, if the body reacts equally actively to the plague and to a common cold, this will also not lead to anything good. Therefore, the next stage in the evolution of the immune system was the emergence of acquired (adaptive) immunity.
- Cells acquired immunity recognize much more specific antigens. If the cells of the innate immune system are able to understand: “our enemy is some kind of bacterium,” then the cells of the acquired immunity notice: “we were attacked by a bacterium, on the surface of which there is such and such an antigen,” - which, you see, where more useful for defeating the enemy. In addition, acquired immunity has a so-called immunological memory, a “black list”, where the antigens of all pathogens that have ever encroached on the integrity of the body are recorded (by the way: the effect of vaccinations is based on the phenomenon of immunological memory). The combat unit of acquired immunity is special immune cells, lymphocytes. There are two types: B- and T-lymphocytes. B lymphocytes - these are, one might say, the artillerymen of immunity. One of the subtypes of B lymphocytes is plasma cells, which are able to produce special proteins against antigens - antibodies. Antibodies stick to antigens, stick around pathogens from all sides and make them more vulnerable - first of all, attracting innate immune cells, macrophages, which recognize antibodies and safely eat such pathogens. As for T lymphocytes, then they are divided into three main types:
- T-killers kill those cells that have been labeled by the body as “wrong” - for example, infected with viruses or tumor cells;
- Helper T cells give instructions to other immune cells about how to work. There are different groups (populations) of T helper cells: for example, T helper type 1 (Th1) spur T killer cells. T helper cells type 2 (Th2) trigger B lymphocytes to fight; in the case of psoriasis, Th1 is of great importance, as well as another subtype of T helper cells - Th17.
- T-suppressors are needed to calm overly enraged colleagues. They regulate the balance between activation and inhibition of the immune response. Suppressor T cells either directly interact with other cells or use cytokines to send them an inhibitory signal and thus slow or stop the immune response. The importance of T-suppressors is demonstrated by the fact that the development of chronic infections and tumors is associated with their increased activity, and autoimmune diseases (when the native immune system rebels against healthy cells) with reduced activity.
The life of each lymphocyte consists of several stages. At first, when the lymphocyte has not yet encountered an enemy, it is called a naive lymphocyte. Having encountered a pathogen, lymphocytes learn to recognize it and become mature. Mature lymphocytes are divided into “fighters” (T-killer cells, T-helper cells, plasma cells, etc.) and memory cells. Memory cells do not participate in battles, but they remember the antigens of all pathogens that have ever encroached on the body: each antigen has its own clone of memory cells. And if later some pathogen attacks again, memory cells will quickly resume populations of “fighters” focused specifically on it, and will defeat the pathogen even before it has time to cause significant harm to the body.
The connecting link between innate and acquired immunity is special innate immune cells, dendritic cells. They encounter a pathogen, capture it, “disassemble” it into antigens and migrate with them to the nearest lymph node, where they transmit information about them to other immune cells. The immune response is launched, T-helpers call T-killers and B-lymphocytes into battle, populations of Th1, Th2 and Th17 mature from naive T-cells, and the immune reaction unfolds to its fullest. And, as already mentioned, dendritic cells play a major role in the pathogenesis of psoriasis.
Colony-stimulating factors
Produced by endothelial cells, fibroblasts, macrophages, mast cells and T helper cells. Designed to stimulate hematopoiesis - the growth of blood cells. Highlight:
Granulocyte colony-stimulating factor (G-CSF) stimulates the growth of neutrophil precursors.
Granulocyte-macrophage colony-stimulating factor (GM-CSF) stimulates the growth of monocytes, neutrophils, eosinophils and basophils, and activates macrophages.
Macrophage colony-stimulating factor (M-CSF) stimulates the growth of monocyte precursors.
| Cytokines | Producer cells | Functions |
Transformative growth factors | ||
| Transforming growth factor alpha | Macrophages, monocytes, epithelial cells, bone marrow cells | Stimulates the growth and development of immune cells. Stimulates mucus production. |
| Transforming growth factor beta | B lymphocytes, macrophages, mast cells | Suppresses the growth of lymphocytes, cancels the effects of many cytokines, switches to the synthesis of IgA. Promotes tissue healing and connective tissue growth at the site of inflammation. |
Onset: what triggers psoriasis
If a person has a genetic predisposition, a small push is enough to trigger the development of psoriasis. Several triggers leading to the manifestation of this disease have now been well studied. We will look at them in this section.
Streptococcus and mimicry
As mentioned in the introductory article “Psoriasis: at war with your own skin” [1], psoriasis often occurs after a person has had a streptococcal infection, such as strep throat. And this is apparently due to the fact that streptococci produce M-protein, a protein similar in structure to the proteins of normal keratinocytes [3]. Immune cells, “awakened” by streptococcus and “trained” to M-protein antigens, after defeating the infection, continue to guard the body’s borders and look for these antigens. They find them on the surface of keratinocytes, mistake numerous harmless keratinocytes for dangerous streptococcus, sound the alarm (after all, according to them, the body has been attacked by a large army of dangerous pathogens), trigger an immune response in the skin and cause psoriatic rashes. This phenomenon - when the antigen on the surface of a microorganism is very similar to the surface protein of normal cells of the macroorganism - is called molecular mimicry. The immune system, misled by mimicry, misfires, mistakes employees for invaders and triggers an immune response where it is not needed at all.
Dysbiosis and distortion of the immune response
People live in harmony with more than ten thousand species of microorganisms and viruses [4]. Sometimes these creatures bring direct benefits to the body (for example, the intestinal microbiota digests what the gastrointestinal tract could not digest). But the benefits of microbes don't stop there. They constantly keep the immune system in good shape, acting as a kind of simulator on which immune cells learn to recognize antigens. And the microbiota of the skin surface plays a major role here [5].
Sometimes the well-being of the normal surface microflora of the skin is disrupted by the active reproduction of “unusual”, although not always harmful, microorganisms - dysbiosis develops. Dysbiosis in one area of the skin entails changes in the normal microbiota in other areas of the skin and mucous membranes. As a result, the immune system, deprived of its usual “simulators,” begins to malfunction. Immune recognition is impaired, which apparently leads to the development of certain diseases, in particular psoriasis and inflammatory bowel diseases. This hypothesis is confirmed, for example, by the fact that in patients with psoriasis, the skin microbiota has an increased number of certain microorganisms - Firmicutes and Actinobacteria [6]. Apparently, an imbalance in the composition of the microbiota, even if it is harmless, “awakens” dendritic cells, and they trigger a snowball of reactions leading to the appearance of a psoriatic rash. True, in this story it is difficult to understand where the cause is and where the effect is. It is possible that it is the development of psoriasis that “distorts” the composition of the microbiota.
Trauma, danger signals and inflammation
Centuries-old clinical observations show that psoriasis often develops and worsens in response to injury - a scratch, wound, piercing, and so on. This phenomenon is called the Koebner phenomenon. There is an explanation for it at the molecular level. Cells that die due to injury release special molecules into the environment, so-called danger signals. These molecules bind to receptors on the surface of innate immune cells and activate the initiation of inflammatory signaling cascades, which lead to the fact that immune cells begin to release a lot of pro-inflammatory cytokines that activate more and more cells - both immune and keratinocytes. This is how inflammation starts. In general, inflammation is a completely normal process that is necessary for the body - for example, so that bacteria do not develop in wounds, so that the skin recovers as quickly as possible. But in the presence of a genetic predisposition, inflammation develops uncontrollably, keratinocytes divide too actively, more and more of them accumulate (and immune cells continue to spur them to divide more and more) - which leads to the formation of a psoriatic plaque. And a specific antigen is not required here: any violation of the integrity of the skin causes a “danger signal”, which in people genetically prone to such uncontrolled inflammation can lead to the development or exacerbation of psoriasis.
Pain and dendritic cells
There may be another mechanism that contributes to the pathophysiology of psoriasis: stimulation of the plaque by nerve fibers. The fact is that a large number of dendritic cells are in close contact with skin nociceptors - sensory neurons, the stimulation of which causes a sensation of pain, or otherwise - neurons that “feel” mechanical and other damage. A study in mice showed that the TRPV1 and Nav1.8 receptors (ion channels) on these neurons could activate skin dendritic cells in experimentally produced lesions. In response, dendritic cells begin to secrete IL-23, an important pro-inflammatory cytokine that stimulates the differentiation of the most fatal lymphocytes for psoriasis—T-helper 17—and thus intensifies psoriatic rashes (Fig. 3) [7]. In other words, even pain can aggravate the course of psoriasis.
Figure 3. Scheme of how cells of the immune system work in psoriasis. DC - dendritic cells; pDC—plasmacytoid DC; MHC—major histocompatibility complex; TNF - tumor necrosis factor; IL—interleukin; IFN - interferon. To see the picture in full size, click on it.
[17]
Innate lymphoid cells type 2 (ILC2) in the regulation of allergic reactions
ILC2s, representing the innate immune system, are one of the main participants in the development of allergic reactions in various organs. Now these cells are receiving much attention as analogues or unique counterparts of Th2, which also synthesize the cytokines IL-4, IL-5, IL-9, IL-13 and amphiregulin in response to the action of TSLP, IL-25 and IL-33 [23–25 ]. Actually, this is why the name “type 2 immune response” is adopted, and not the Th2 response, as it was previously designated. Among ILC2, additional subpopulations are currently being identified based on their ability to respond to IL-25 and IL-33. The subpopulation that responds to IL-33 are quiescent cells called natural ILC2s (nILC2s), while the cells that respond to IL-25 are called inflammatory ILC2s (iILC2s) [26]. In addition, a subpopulation of ILC2 that produces IL-10 is isolated [27]. Perhaps they normally function to limit the excessive synthesis of proinflammatory cytokines during the development of a response to parasite invasion.
ILC2s are involved in the immunopathogenesis of allergic rhinitis and are found in large numbers in nasal polyp tissue. Their number increases in the peripheral blood of patients, and these cells appear in the nasal mucosa with the development of allergic rhinitis. At the same time, successful allergen-specific immunotherapy leads to a decrease in the number of ILC2 in patients [28, 29]. The use of anti-cytokine therapy using monoclonal antibodies against IL-5 gives a good therapeutic effect in polypous rhinosinusitis [30]. ILC2s serve as an important component of AD development. In patients with asthma, an increase in the number of ILC2s in the peripheral blood, activation of ILC2s in lung tissue, and active synthesis of cytokines characteristic of type 2 immune response were noted [31]. In particular, ILC2 secrete IL-13, which stimulates the migration of activated DCs to draining lymph nodes, where they trigger Th2 differentiation [32]. In AD patients, an encounter with an allergen causes a sharp increase in the number and activation of ILC2s secreting IL-5 and IL-13 [33]. The levels of ILC2 and IL-33 in bronchoalveolar lavages of patients correlated with the severity of asthma [34].
What happens to the skin with psoriasis
All of the above events lead to one effect - hyperactivation of the immune system, which begins, as a rule, with dendritic cells. These cells secrete various cytokines, primarily TNF and IL-23, which serve as a signal of such serious danger that they greatly rearrange the metabolism of other cells and force them to release more and more new cytokines - there is literally a ninth wave of pro-inflammatory molecules, and inflammation starts. As a result, the normal functioning of almost all types of skin cells is disrupted. The most numerous skin cells - keratinocytes - experience enormous pressure on their receptors and respond to the impact with hyperproliferation (accelerated reproduction) and the production of new cytokines, as well as the secretion of antimicrobial peptides. In turn, the molecules released by keratinocytes attract even more neutrophils and lymphocytes. This is how a positive feedback is formed: the cells of the immune system act with cytokines on the cells of the epidermis, and those, in response to this action, additionally activate the cells of the immune system [8]. With such a volume of work, T-suppressors feel like accountants who had to submit a quarterly report yesterday and cannot resolve the current pathological situation.
Hyperproliferation of keratinocytes leads to the proliferation of epithelial tissue in some areas - psoriatic plaques are formed. Due to the fact that the proliferation of keratinocytes in the plaque is accelerated (their cell cycle is shortened from 23 to 3-5 days), they cannot differentiate normally. Cells that normally lose their nuclei in the granular layer, in psoriasis, retain their nuclei even when approaching the surface of the epidermis. This phenomenon is called parakeratosis and is a diagnostic sign of psoriasis. It is accompanied by disturbances in the synthesis of lipids, which normally hold the cells of the stratum corneum of the epidermis together. The latter is clinically manifested by peeling psoriatic rashes.
In addition to inflammation and proliferation of the epidermis, there is a third key element in the pathogenesis of psoriasis - angioneogenesis (formation of new vessels). The inflammatory environment changes vascular permeability and produces factors that stimulate the growth of new vessels. New vessels grow; at the same time, the cells of their endothelium (inner membrane), under the influence of the inflammatory environment, secrete special cytokines - adhesion molecules, which attract more and more leukocytes to the psoriatic skin. At the same time, the microenvironment of growing vessels influences T-helper and killer cells located at the site of inflammation in such a way that they further enhance the proliferation of the epidermis [9].
In addition to the epithelial cells themselves, changes in the sebaceous glands occur in psoriasis, but they have been little studied. With rashes on the scalp, deep atrophy of the sebaceous glands is usually observed with a decrease in their number and size, and in more than half of the cases their complete atrophy occurs. In the foci of rashes, both normal and atrophied sebaceous glands are mixed. In acutely inflamed scalp skin, atrophy of the sebaceous glands is accompanied by a decrease in hair diameter. Overall, although initial studies demonstrated histological changes in the sebaceous glands, there were no changes in the lipids they secreted. But studies of the “psoriatic” lipid profile of the sebaceous glands are few, therefore it is necessary to further study its differences from the normal one, and also to evaluate the prospects for modifying the work of the sebaceous glands as one of the therapeutic components for psoriasis [10].
Chemokines
Chemokines stimulate chemotaxis - the directed movement and movement of leukocytes. Chemokines are produced by leukocytes, platelets, epithelial and endothelial cells. These cells are located in places where pathogens most often penetrate (skin, mucous membranes, blood vessels) and, through chemokines, call leukocytes to help quickly neutralize foreign antigens. On the downside, the human immunodeficiency virus has adapted to chemokine receptors on the surface of T-lymphocytes, using them to penetrate the cell.
Features of the immune system in psoriasis
We have already briefly touched on the features of the immune system in psoriasis, and now we will consider them in more detail.
Let's start with keratinocytes . Although these are not immune cells, but skin cells, they are in close interaction with the immune system and, in any danger, ask immune cells for help. Unfortunately, in the case of psoriasis, keratinocytes can be compared to a grenade, the pin of which is just about to fall off. As already mentioned, when keratinocytes die, “danger signals” are released - antimicrobial peptides (including LL37, S100, β-defensins). Normally, as the name implies, these peptides are aimed at fighting pathogens. However, in psoriasis, so many of them are released that they attract excessive attention of immune cells. Antimicrobial peptides activate the immune response, increasing the synthesis and release of cytokines IL-6, IL-10, IL-8 (CXCL8) and CXCL10 by various immune and non-immune cells, which in turn attracts innate immune cells - neutrophils and macrophages . By the way, the abundance of antimicrobial peptides and immune cells in the area of inflammation explains an interesting feature of psoriasis: despite the disturbed structure of the skin, which in the area of the plaque is more like a half-healed wound, secondary infections in patients with psoriasis are very rare.
In addition to pro-inflammatory cytokines and antimicrobial peptides, keratinocytes contain special protein complexes that trigger inflammation - inflammosomes (note in parentheses that neutrophils and macrophages also have inflammosomes). One of the main proteins of inflammosomes, caspase-1, in case of danger, cleaves the sluggish, inactive precursors of the cytokines pro-IL-1 and pro-IL-8 into active forms. Then a chain reaction begins: IL-1 and IL-8 influence surrounding keratinocytes and initiate the production of one of the main pro-inflammatory cytokines - TNF - inflammatory reactions grow like a snowball and as a result lead to the formation and release of strong pro-inflammatory cytokines IL-18 and IL -1β.
So, too many neutrophils - innate immune cells that protect the body from bacterial and fungal infections. These cells can be compared to kamikazes: they phagocytose (that is, absorb) a wide variety of prey - from molecules to whole cells of pathogens - but when enemy forces prevail, they fire a final salvo of pro-inflammatory cytokines and are destroyed, “spitting out” bactericidal molecules. In addition, neutrophils manage to create a trap for pathogens from their own contents: when self-destructing, a neutrophil, in addition to immunogenic molecules, throws out its DNA, in which, like in a spider’s web, bacteria and other strangers become entangled. Unfortunately, this trap turns out to be a double-edged sword: in psoriasis and some other diseases, it causes autoimmune inflammation.
Normally, neutrophils circulate in the blood vessels of the dermis and hypodermis and are sent to the epidermis only if they hear (having caught an increased amount of cytokines on the receptors) about the inflammation taking place there. In psoriasis, on the contrary, they are found predominantly in the epidermis, because they were “called” by the cytokines CXCL1, CXCL2, IL-8 and IL-18.
Neutrophils play an important role in the early stage of psoriasis development: they attract and activate T-lymphocytes into the developing plaque, and also stimulate the proliferation and differentiation of keratinocytes.
The role of macrophages in psoriasis has not been well studied. Available observations indicate their participation in inflammation and the correlation of their number in the foci of the disease with the intensity of inflammation. But the question of their active role remains open.
Dendritic cells also play an important role in psoriasis . They, as already mentioned in the section on the immune system, transmit a signal about pathogens that have attacked the body to acquired immune cells - T-helpers. There are two main types of dendritic cells: myeloid and plasmacytoid. Myeloid cells are primarily engaged in the presentation of antigen to T-helper cells: they catch the pathogen, secrete its antigens, and, having met a naive T-helper cell, these antigens are shown to him. Plasmacytoid cells mainly act as “chemical weapons”: they control the differentiation of T-helper cells with the help of cytokines.
In the pathogenesis of psoriasis, the main role is played by the skin subpopulation of dendritic cells - Langerhans cells . These cells roam in search of pathogens throughout all layers of the epidermis except the stratum corneum; They are also found in the dermis, oral mucosa, foreskin and vagina.
In psoriasis, Langerhans cells, for one reason or another, excessively activate their “supplements” - T-helpers. An important role in the initial stages of psoriasis is played by cytokines secreted by Langerhans cells: integrin alpha-X (CD11c) of myeloid cells and type I interferon of plasmacytoid cells.
You may have already noticed that almost all of the pathways described above in the pathogenesis of psoriasis lead to one type of cell - T helper cells . Indeed, T helper cells are the main immune cells associated with psoriasis, and they mediate the main course of the disease. They are attracted to the skin by cytokines from dendritic cells, keratinocytes, and neutrophils. In psoriasis, the majority of T-lymphocytes in the skin are type I T-helper cells (Th1), which, through interferon-γ, reduce the activity of type II T-helper cells and increase the activity of killer T-cells . The latter begin to attack keratinocytes, which, when destroyed, again release immunogenic molecules to attract T-lymphocytes. Thus the circle closes, and the process begins to support itself. As a result, a patient with skin rashes occupying 20% of the body surface has about 8 billion T-lymphocytes in the circulating blood, while in psoriatic plaques their number reaches 20 billion (normally, this number accounts for the entire skin) [ eleven].
In recent years, it has been discovered that another subpopulation of T helper cells, T helper 17 (Th17), plays a significant role in the development of psoriasis. They produce many pro-inflammatory cytokines, such as IL-17F, IL-17 (Th17 lymphocytes get their name from the active secretion of IL-17) and IL-22, leading, among other things, to the proliferation of keratinocytes - the main characteristic of psoriasis [12], [13]. ]. The latest “breakthrough” in the treatment of psoriasis, the drug secukinumab (Cosentyx), is precisely an antibody to the Th17-secreted cytokine IL-17A.
Finally, there is another type of immune cell that is involved in the development of psoriasis. These are myeloid suppressor cells , a diverse group of immune cells that originate in the bone marrow.
They are able to inhibit T lymphocytes, dendritic cells and macrophages [14]. This property could play an invaluable role in the treatment of psoriasis, but so far studies of the functions of these cells in this disease are scarce. Some studies have shown an increase in the number of monocytic myeloid suppressor cells in areas of inflammation and in the blood. However, they were characterized by low functional activity [15]. Perhaps in the future it will be possible to develop ways to increase the activity of myeloid suppressor cells, that is, to use regulators already existing in the body rather than external immune inhibitors to treat the disease.
Cytokines: interleukins and interferons
Cytokines - interleukins and interferons - are generally known, if not as highly effective, but practically as the only antitumor agents for melanoma and kidney cancer. This is the best thing that immunology has brought to oncology; colony-stimulating factors are intended exclusively for influencing stem cells in order to stimulate hematopoiesis; their necessity and significance is unconditional. Interleukins have common properties: they are synthesized by cells of the immune system; active at very low concentrations; serve as mediators of immune and inflammatory reactions, have autocrine, paracrine and endocrine activity; act as cell growth and differentiation factors; form a regulatory network; have multifunctional activity [96].
Interleukins are presented in the pharmaceutical formulations IL-1b (Betaleukin) and IL-2 (Aldesleukin, Roncoleukin).
Aldesleukin ( proleukin ) is produced by fermentation in the presence of tetracycline from genetically engineered Escherichia colli, whose DNA contains the interleukin-2 gene, similar to that of humans. The difference from endogenous interleukin-2 is that it has a different aggregation state and is non-glycosylated due to the fact that two amino acid residues are replaced during the process of genetic engineering. The exact mechanism of antitumor action is unknown. It is thought to involve stimulating the body's immune response to the tumor.
Endogenous interleukin-2 activates T lymphocytes and NK cells, which recognize and destroy tumor cells, increases the production of antibodies by B lymphocytes, and increases the production of interferon gamma and TNF. Recombinant interleukin-2 has the same biological activity as the endogenous cytokine. The action of aldesleukin includes activation of cellular immunity with pronounced lymphocytosis, eosinophilia and thrombocytopenia. The most effective drug for metastatic renal cell cancer has been widely introduced into treatment standards [20].
The treatment is associated with high toxicity, which really limits its use along with its extremely high cost [21,97]. Aldesleukin, as a result of increased capillary permeability, causes a dose-dependent capillary leakage syndrome (CLE), leading to the formation of extravasation and contributing to a decrease in vascular resistance. It is believed that many toxic effects are associated with hypotension and reduced organ perfusion resulting from SPC: arrhythmias, angina pectoris and myocardial infarction; respiratory failure requiring intubation; gastrointestinal bleeding and intestinal infarction; renal failure and mental reactions. SPC develops immediately after the start of treatment, initially causing a decrease in blood pressure up to 2-12 hours. As a result of the formation of extravasation, edema and effusion develop, and in some patients pleurisy and ascites are possible. The secretion of TNF and interleukin-1 can explain hemodynamic effects similar to those recorded in septic shock.
Impaired neutrophil function may increase the risk of developing disseminated bacterial infection. Treatment with aldesleukin in high doses should be carried out in hospitals where highly specialized care is provided, with equipment for intensive care by doctors with experience in cardiology and pulmonology.
Roncoleukin , a domestic recombinant IL-2, is a complete structural and functional analogue of endogenous interleukin-2. The drug has direct and indirect effects on the immune system [137]. Direct: activation of clonal proliferation of T-lymphocytes, stimulation of cellular differentiation of cytotoxic lymphocytes, stimulation of clonal proliferation of B-lymphocytes, increase in the functional activity of phagocytes, decrease in the level of spontaneous apoptosis of T-helper cells. Indirect: correction of T-helper subpolation, correction of the cytokine profile, intensification of eosinophil differentiation processes, etc.
The drug has a pronounced immunocorrective activity of all types of bacterial, viral and antifungal immunity [137].
It is used to prevent immune deficiency once or twice with an interval of 2-3 days, 250 thousand IU [137]. To compensate for immunodeficiency - 2-3 times with a break of 48 hours at a dose of 250-500 thousand IU. For infections, depending on severity, starting from 500 thousand IU to 2.5 million IU.
Toxic reactions are characteristic of all IL-2.
IL-1b ( Betaleukin ) increases the production of IL-6 and endogenous CSF, through which the proliferation and differentiation of cells belonging to various hematopoietic lineages, including pluripotent stem cells, is enhanced. Under the influence of Betaleukin, the number of granulocytes, lymphocytes and platelets is restored, but only in the presence of a sufficient number of precursor cells. The peculiarity of Betaleukin is its protective effect with the induction of rapid recovery of granulocytes: for grade 2 leukopenia - on the 5th day, grade 4 - on the 12th day [72,132]. After cessation of stimulation, granulocytes may return to baseline levels.
Betaleukin changes the level of immunity little; existing T-cell immunosuppression may persist. But the functional activity of neutrophil granulocytes, namely migration, bactericidal activity and phagocytosis, increases significantly.
The drug significantly accelerates wound healing in purulent-septic surgical infections (secondary sutures are applied 3-4 days earlier), postoperative mortality is reduced, and the condition of patients significantly improves [133]. Betaleukin can be injected into the pleural cavity in case of empyema, into abscesses, including pulmonary ones, without systemic toxicity. Betaleukin ointment promotes rapid cleansing and healing of wounds.
Standard treatment regimen: 15-20 ng/kg of the patient’s body weight once a day in 500 ml of isotonic solution intravenously for 5 days.
Like most cytokines, when treating 60% of patients, grade 2-3 hyperthermia is observed, which is twice as often as when using Leucomax; chills – 80%; arthralgia – in 10%, which is comparable to leucomax.
Betaleukin is currently practically not used due to the availability of more effective and less toxic colony-stimulating drugs, despite the fact that the effects of Betaleukin and CSF are somewhat different [132]. Unlike CSF, the use of which leads to thrombocytopenia, IL-1b stimulates thrombopoiesis and enhances phagocytosis and chemotaxis of leukocytes.
All interferons - secretory glycopeptides - are divided into three groups: alfa-, beta- and gamma-interferons. IFN-alpha (produced by leukocytes) and IFN-beta (produced by fibroblasts) are formed in response to cell treatment with viruses and are called type I interferons. They have immunoregulatory, antitumor, antiviral, and radioprotective activity. The main biological effect of type I interferons is the suppression of the synthesis of viral proteins (antiviral) and tumor cells (antiproliferative) due to interaction with specific membrane receptors, increasing the activity of cytotoxic lymphocytes (immunomodulatory), stimulating apoptosis, and reducing the formation of fibrous tissue [96,127]. IFN drugs have an antiproliferative effect on lymphoid cells, less on myeloid cells and a very small effect on erythrocytes.
Interferons are produced by macrophages and lymphocytes. Normally, macrophages, T-helper cells and neutrophil phagocytes sequentially, with the help of cytokines, carry out nonspecific cellular immunity. At physiological concentrations, interferons are activators of cytotoxicity effectors and B-lymphocytes; at high concentrations, they inhibit the differentiation and activity of all immune effectors.
In the treatment of a number of human tumors, type I IFNs play a dominant role. Endogenous interferons have high bioavailability, acting through specific membrane receptors and do not accumulate. For type I interferons, there is one receptor; for gamma interferons, there is a “personal” membrane receptor. With daily administration of high doses (1 million units), the number of receptors decreases and only after 2-3 days it returns to normal. Therefore, high doses of IFN should be administered at intervals, otherwise positive treatment results are not expected.
IFN-gamma, produced by mature and immature T lymphocytes, NK cells and, possibly, macrophages, has other immunoregulatory functions and therefore has less antitumor activity. But the antiproliferative potential of interferon-gamma is 10-20 times higher than that of IFN-alfa (antiproliferative and antitumor activities should not be confused). Main functions: activation of mononuclear phagocytes, increased expression of MHC I and II, activation of neutrophils and NK cells, differentiation of T and B lymphocytes [96]. IFN-gamma belongs to type II.
Of the alpha interferons, Interferon Alfa, Interferon-alfa-2a (Roferon-A), Interferon-alfa-2b (Intron-A, Realdiron, Viferon), Interferon-alfa-2c (Berofor), Interferon-alfa-n1 are used in medicine. (Wellferon), interferon-alfa-n3 (Alferon N).
All alpha interferons are classified according to the method of production into natural and recombinant. Natural ones, in turn, are divided into lymphoblastoid, leukocyte (native, concentrated) and diploid. Native ones have low specific activity, but retain natural cytokines, due to which they retain immunological properties. Concentrated ones have higher activity, but due to the removal of cytokines they lose their immunobiological properties.
Recombinant interferons consist of 165 amino acids, but differ in 1-2 amino acid residues and are therefore divided into subtypes -2a, -2b, -2c. Natural forms are excreted more slowly than recombinant forms; the differences in pharmacokinetics are due to the fact that natural forms consist of several subtypes, while recombinant forms consist of a homogeneous protein of one subtype [121]. Natural forms have high immunobiological and antibacterial activity, recombinant ones have predominantly antiviral and antitumor activity [128].
Interferons alpha-2a, -2b, -n1 and -n3 are not interchangeable, although their spectrum of activity is similar. The toxicity of the drugs is also identical (flu-like syndrome, anorexia, fatigue, partial hair loss, etc.), but the severity of adverse effects is directly dependent on the amount of interferon contained. Alpha interferons can exacerbate the neuro-, cardio- and myelotoxicity of drugs used in conjunction with them [122]. Table 1 shows alpha interferons available to Russians.
Table 1
. Interferon-alpha drugs.
| Interferon-alpha subtype | A drug | Distinctive features |
| Recombinant alpha-2a | Roferon A | From bacterial strains of Escherichia coli |
| Recombinant alpha-2b | Intron A | From bacterial strains of Escherichia coli |
| Realdiron | From the bacterial strain Pseudomonas putida | |
| Reaferon | From the bacterial strain Pseudomonas pseudomallei | |
| Viferon | From the bacterial strain Pseudomonas pseudomallei with membrane stabilizing additives | |
| Recombinant alpha-2c | Berofor | From bacterial strains of Escherichia coli |
| Natural alpha-1n | Wellferon | From a culture of human Namalwa lymphoblastoid cells induced by Sendai virus |
| Natural alpha-3n | Alferon, Egiferon | From normal human leukocytes induced by Sendai virus |
| Natural Alpha | Alfaferon | From normal human blood leukocytes |
| Leukinferon | From normal human blood leukocytes in combination with cytokines |
Interferon Alfa (a mixture of various subtypes of natural alfa-INF from human blood leukocytes) changes the properties of cell membranes, increases the activity of macrophages and NK cells, which makes it possible to use the intranasal form for the prevention and treatment of influenza and ARVI. Perhaps this is the most “ancient” and widely used immunostimulating agent. It is also effective for viral hepatitis, Kaposi's sarcoma, and lymphomas. Rarely, but used in the treatment of intraepithelial lesions of the cervix [126]. Hypernephroma and melanoma have been noted to be sensitive to it, but in modern practical oncology, with the advent of recombinant forms, it has lost its significance both because it contains impurities of blood proteins, lymphocyte products, Xindai viruses and proteins of embryonic cells in which the virus was cultivated, and because 20 liters cell suspension is obtained from 100-200 donors. To obtain 1 gram of pure interferon, it is necessary to take blood from 200 thousand donors [68].
Under the name Alfaferon, it is produced by the Italian company Ismunit; in Russia, Human Leukocyte Interferon (HLI) is produced by NPF Interkor.
It has an injection form and suppositories, mainly for the treatment of viral hepatitis. Inhalations protect against influenza, the ointment is effective against chronic tonsillitis, aphthous stomatitis, and herpes.
Natural alpha-interferon from human leukocytes in combination with cytokines Leukinferon is produced in Russia. Interleukins: IL1, IL6, IL12; tumor necrosis factor, macrophage migration inhibitory factor MIF and leukocyte migration inhibitory factor LIF - a complex of phase I cytokines of the immune response - is contained in leukinferon in natural ratios that are not disturbed during the purification process.
The drug, when administered parenterally, reduces the level of circulating IFN and restores the IFN-producing ability of leukocytes, both for alpha and gamma IFN. Increases the differentiation and activity of T-lymphocytes (on days 3-4), stimulates the phagocytic function of macrophages, reduces the number of circulating immune complexes, and stimulates hematopoiesis in the early stages [129]. The maximum hematopoietic effect is achieved in the second week of therapy.
The drug significantly accelerates wound healing and almost doubles the recovery process in purulent surgical diseases [117,119,120]. Reduces post-radiation rehabilitation time by 2-3 times, improves quality of life during chemotherapy, reduces the frequency of opportunistic and viral infections, normalizing immune parameters [118,125].
The drug, depending on the purpose, is used in several modes: to prevent immunodeficiency - three times a year for 5 injections; every other day - to prevent cytopenia. In cancer patients it can be used in short courses throughout life. The dosage of the drug is 10 thousand IU.
The antiviral potential of the drug is small, but to prevent influenza, you can use Leukinferon ointment or an injection solution (dropped into the nose or eyes). The ointment is also suitable for the treatment of viral skin lesions.
The role of Roferon-A (alfa-2a) and Intron-A (alfa-2b) is well known as a highly effective drug for the treatment of melanoma, kidney cancer, Kaposi's sarcoma, basal cell carcinoma, etc. [22, 71]. In three hematological diseases - hairy cell leukemia, chronic myeloid leukemia, essential thrombocythemia - interferon monotherapy leads to complete remissions in 80-90% of patients. In the treatment of multiple myeloma, chronic lymphocytic leukemia and non-Hodgkin's lymphoma, it significantly increases the duration of remission achieved as a result of chemotherapy.
Interferons trigger a cascade of intracellular reactions that cause antiproliferative, immunomodulatory, antiangiogenic, and antiviral effects. The antiproliferative effect is manifested in slowing down the cell cycle, blocking essential enzymes, and the expression of oncogenes. Expression of leukocyte antigens of the HLA1 class under the influence of IFN-alpha increases sensitivity to cytotoxic T lymphocytes. Expression of HLA class II antigens accelerates the immune response. IFN stimulates macrophages, their activity increases, and their production of cytokines increases.
The drugs are different subtypes of interferon: Roferon A - alpha-2a, Intron A - subtype 2b, that is, they differ in two amino acid residues with one and a half hundred identical. The spectrum of diseases is the same, toxicity is the same, but there is a very significant difference that determines their effectiveness - this is the body’s reaction to the presence of the drug - the production of neutralizing antibodies.
The production of antibodies significantly affects the results of treatment; a high titer may indicate the likelihood of an unfavorable response. Two types of antibodies are produced: CAT (immunoglobulin M) and NAT (immunoglobulin G); and if SATs are not directed against antigens and, therefore, do not determine the biological activity of IFN, then NATs significantly reduce antiviral and antiproliferative activities. Intron A is absolutely identical to human IFN, therefore the titer of antibodies to Intron A is low [56]. It was noted that during treatment with Roferon, NAT is produced several times more than during treatment with Intron [60]. Thus, when treating carcinoid with equivalent doses of Roferon A and Intron A, a high titer of NAT was detected in 50% of patients in the first group, in the second - 0%, the effectiveness of therapy was 17% and 60%, respectively [57]. When treating kidney cancer with Roferon, NAT is detected in 33-38%, Intron – in 5% [58,59].
Both drugs modulate the activity of chemotherapy drugs used together with them in two ways, predominantly increasing them [123]. The direct way to increase efficiency is associated with the regulation of gene activity during the penetration of the membrane receptor associated with interferon into the cell. Subsequent quantitative and qualitative changes in membrane receptors affect the metabolism of the target cell. The indirect pathway is mediated through immunocompetent cells, which, in the presence of interferons, increase their antitumor activity.
Realdiron and Reaferon , Reaferon EC (alfa-2b), compared to Intron-A, have an advantage not only in cost, but also their spectrum of action is somewhat limited, it does not include, in particular, melanoma, ovarian and colon cancer. The drug is made from bacterial strains of Pseudomonas, and not Escherichia coli, like Intron.
Antibody production significantly reduces the effectiveness of therapy [124]. When treated with daily low doses, antibodies are formed earlier and in greater quantities than when treated with high doses at intervals between administrations. The drug remains in the blood serum for the longest possible time (up to 24 hours) after intramuscular and subcutaneous administration. When administered intravenously - only 1.5-2 hours.
In order to enhance activity and reduce adverse reactions, ointment forms of Reaferon based on lanolin and hydrogel have been created. These ointments are used to treat viral skin lesions, herpes, and prevent influenza and acute respiratory infections. Lanolin ointment with antiviral activity of 5,000 IU/g is retained on the skin and mucous membranes for no more than 6 hours, so it is applied three times a day. A hydrogel-based ointment has an activity of 10,000 IU/g, forms a film that lasts up to 12 hours and is not washed off by clothing; accordingly, it is applied only 2 times a day [60].
Viferon - Reaferon rectal suppositories - contains, in addition to interferon, tocopherol acetate and ascorbic acid, which increases antiviral activity due to the antioxidant and membrane-stabilizing effects of vitamins by 10-14 times.
The range of childhood infections for which Viferon is used is amazing: pneumonia of various etiologies, viral hepatitis, herpes, cytomegalovirus infection, toxoplasmosis, chlamydia, diphtheria, mumps, tick-borne encephalitis, etc.
Berofor (alfa-2c) is a recombinant alpha-2c interferon from bacterial strains of E. coli. It has a spectrum of antitumor action similar to roferon, intron and reaferon, but in practice it is used mainly in the treatment of laryngeal papillomatosis and hairy cell leukemia. Has an antiviral effect.
At the end of the 90s, a suspicion arose, which had a catastrophic effect on its use, that the human lymphoblastoid interferon Wellferon (alfa-n1), in comparison with recombinant forms obtained from bacteria, into the genetic apparatus of which the human interferon gene is built in, cannot guarantee absolute purity from intracellular infections. Meanwhile, contamination of lymphoblastoid interferon with viruses is completely eliminated by careful processing. The degree of purification of the drug reaches 98%.
The drug is obtained by exposing the interferon inducer Sendai paramyxovirus to a suspension of Namalwa cell culture, which are human lymphoblastoid cells transformed by the Epstein-Barr virus. The cell line was first derived from Burkitt's lymphoma cells from an African boy named Namalwa. Currently, there is a standardized culture of Namalwa cells from the Master Cell Bank.
Wellferon stimulates the activity of macrophages and NK cells, and in hairy cell leukemia directly affects tumor cells. In viral hepatitis, it increases the resistance of cells not infected with the virus, affects the RNA of the virus and prevents its replication.
The drug is a mixture of 18 interferon subtypes, while recombinant forms are one subtype. This difference may be the reason why the formation of antibodies (NAB) is not typical during treatment with Wellferon.
The spectrum of action and toxic reactions are almost identical to roferon A and intron A.
Alferon N (alfa-n3) is obtained from a pool of human leukocytes induced as a result of incomplete infection with the avian Sendai virus. The process of obtaining the drug includes immunoaffinity, using mouse monoclonal antibodies, and gel filtration chromatography. Contains 14 natural subtypes. Inhibits viral replication in infected cells, increases the phagocytic activity of macrophages and enhances the specific cytotoxic effect of lymphocytes on target cells. Under the name Egiferon it is produced by the Hungarian “EGIS”.
Used for local treatment of large genital warts: a dose of 250,000 IU is injected twice a week into the base of the wart for 8 weeks. For the treatment of multiple warts, Intron A is preferable, when 1 million IU is injected under each wart three times a week for 12-16 weeks.
The spectrum of action of interferons alpha and beta is close, but the latter are quickly broken down and absorbed into tissues. Of the Interferons-beta, Interferon Beta, INF-beta-1a (Avonex) and INF-beta-1b (Betaferon) have found application.
The immunomodulatory activity of INF Beta is due to the activation of phagocytosis, stimulation of the formation of antibodies and lymphokines. It has a moderate antiproliferative effect in intraepithelial cervical cancer, kidney cancer, glioblastoma, and hairy cell leukemia.
In breast cancer, it can be used to induce steroid hormone receptors. With progression on tamoxifen, 67 patients were administered B-interferon 3 times a week, 3 million units. The effect was achieved in 67%, the time to progression was 19.6 weeks [73].
There is a report on the use of interferon-Beta as a radiomodifier in radiation therapy of anal cancer in 5 patients. The drug was administered three times a week, 1-3 million units. 2 hours before radiation therapy ROD 2 Gy, SOD 30-40 Gy. All patients achieved regression of varying degrees without significant complications [94]. But the drug is mainly used as an antiviral agent.
Avonex binds to specific receptors on the cell surface and triggers a complex cascade of intercellular interactions, leading to the expression of numerous gene products and markers.
Betaferon reduces the formation of gamma interferons, activates the function of T-suppressors, thereby weakening the effect of antibodies against the main component of myelin. Both drugs are used for multiple sclerosis.
Interferon-gamma Imukin is known as immune interferon. Activates macrophages, increases the activity of NK cells, reduces the expression of a subpopulation of B lymphocytes, monocytes and eosinophils, stimulates B cell differentiation, and reduces IgE production. Prescribed for chronic granulomatous disease, psoriasis, leprosy.
Meshcheryakova N.G.
A thin scar on your favorite skin
Despite the fact that every day we are learning more and more about the contribution of the immune system to the development of psoriasis, it is not yet possible to completely cure this disease. Even the most successful treatment methods can only achieve periods of remission - but sooner or later the plaques reappear on the skin. The search for the reason for this state of affairs led researchers to carefully study the keratinocytes in the area of the skin where the plaque used to be. It turned out that, despite the visual improvement characteristic of remission, the disappearance of the characteristic histological symptoms of psoriasis and “extra” immune cells from the skin, the expression of some genes in keratinocytes remains altered. This change has been called a molecular scar, and it may be the reason why the disease comes back again and again. Here are some genes whose activity never returns to normal: the MMP9 gene, which encodes an enzyme that breaks down different types of collagen and gelatin in the skin, helping skin cells to be more mobile; the WNT5A gene, encoding an important regulatory protein that monitors the proper development of skin and hair follicles, and can also regulate skin color by influencing melanocytes; genes of various cytokines (CCL2, CXCR4, CCL18, LTB) and several hundred more genes [16]. Perhaps studying these genes will tell us something new about the role of keratinocytes in the development and recurrence of psoriasis.
References
- Shipilov, M.V. Molecular mechanisms of the “cytokine storm” in acute infectious diseases. General Medicine, 2013. - No. 1.
- Nedomolkina, S.A., Velikaya, O.V., Zoloedov, V.I. Cytokine status in patients with chronic obstructive pulmonary disease and type 2 diabetes mellitus. Kazan medical journal, 2021. - No. 2.
- Iyer, S., Cheng, G. Role of interleukin 10 transcriptional regulation in inflammation and autoimmune disease. Crit Rev Immunol., 2012. - Vol. 32(1). - P. 23-63.
- Chu, W. Tumor necrosis factor. Cancer Lett., 2013. - Vol. 328(2). — P. 222-225.
- Ligong, L., Zhang, H., Danielle, J. Dauphars, You-Wen He, A Potential Role of Interleukin 10 in COVID-19 Pathogenesis, Trends in Immunology, 2021. - Vol. 42(1). — P. 3-5.
- Giovannini, S., Onder, G., Liperoti, R. et al. Interleukin-6, C-reactive protein, and tumor necrosis factor-alpha as predictors of mortality in frail, community-living elderly individuals. J Am Geriatr Soc., 2011. - Vol. 59(9). — P. 1679-1685.