Prostate cancer (prostate cancer, pancreas) is a hormonally dependent tumor - its growth is provoked by the influence of sex hormones, in particular testosterone. In gland cells, it is converted into another, more active androgen - dihydrotestosterone (DHT), which, when malignant transformation occurs, stimulates the activation of oncogenes and, as a result, uncontrolled division and proliferation of tumor cells. If this effect is stopped, the growth of the tumor will stop. Hormonal therapy is not a method of radically removing cancer, but it can curb its progression and prolong remission for quite a long time.
- Molecular basis of hormonal treatment for pancreatic cancer
- How androgen blockade works
- Bilateral orchiectomy (castration)
- Use of estrogens
- LHRH agonists
- LHRH antagonists (degarelix)
- Antiandrogen treatment (androgen receptor antagonists)
- Combined hormonal treatment
- Intermittent hormonal treatment
- Immediate or delayed hormonal treatment for prostate cancer
- Monitoring patients undergoing hormonal treatment
- Complications of hormonal treatment for pancreatic cancer
Hormonal treatment is effective in more than 90% of patients with prostate cancer, even in the case of disseminated forms. Therefore, it can also be used for palliative purposes. But even with curable (potentially curable) tumors, this method is of great importance as part of a combined effect together with radical surgery or radiation therapy. Adjuvant and neoadjuvant therapy regimens are used as a complement to surgery or radiation. In addition, alternative designs and regimens, such as intermittent therapy, are being explored.
Molecular basis of hormonal treatment for pancreatic cancer
To understand how hormone therapy works, let's understand how the male reproductive system functions.
Male sex hormones are called androgens. The main one is testosterone. It is produced by the testicles (testicles). It accounts for about 95% of all androgens in the male body. Testosterone production is regulated by the hypothalamic-pituitary system. The hypothalamus produces luteinizing hormone releasing hormone (LHRH), which acts on the pituitary gland, which in turn produces luteinizing hormone (LH). It is LH that acts on special cells in the testicles that produce testosterone.
This entire system is regulated by the feedback principle. For example, if testosterone levels decrease, the hypothalamus will release more LHRH and stimulate testicular activity. Conversely, if the amount of testosterone is higher than necessary, the hypothalamus reduces the synthesis of LHRH to “slow down” the testicles.
The remaining 5% of androgens are produced by the adrenal glands. At the same time, both direct testosterone and its precursors - androstenedione and dehydroepiandrosterone - are synthesized here. They are converted into testosterone already in the prostate tissue.
After entering the cells of the pancreas, testosterone is converted into dihydrotestosterone (DHT), a substance that is 2.5 times more active than its predecessor. It is he who is responsible for the regulation of intracellular processes by attaching to nuclear receptors and stimulating gene expression. This includes stimulation of oncogenes, which lead to uncontrolled growth and reproduction of malignant cells.
Thus, the testicles and adrenal glands are the two sources of androgens in the male body. Previously, hormone therapy only involved suppressing testosterone production in the testicles. However, there is now evidence that androgens can also trigger tumor growth. Therefore, it is now recommended to carry out the blockade in two directions.
How androgen blockade works
Antiandrogen blockade is aimed at preventing stimulation of cancer cells by male sex hormones. For this purpose, the following activities can be carried out:
- Surgical removal of the testicles, which, as mentioned above, produce about 95% of all androgens.
- Blockade of androgen synthesis with medications. Blocks can be carried out at different levels of the hypothalamic-pituitary-androgenic system.
- Blockade of circulating androgens. In this case, the cells of the pancreas become immune to the action of sex hormones, but the total level of testosterone in the blood remains within normal limits.
Thus, the following types of hormonal treatment are used:
- Surgical removal of the testicles - bilateral orchiectomy.
- Use of luteinizing hormone releasing hormone (LHRH) agonists.
- Therapy with LHRH antagonists.
- Estrogen therapy.
- Antiandrogen therapy.
Stabilization of the oncological process and, as a consequence, the quality of life of patients directly depends on how long the cancer will respond to antihormonal therapy. The fact is that a malignant neoplasm is an accumulation of relatively heterogeneous cells. In pancreatic cancer, most of them initially have a dependence on hormonal stimulation. With constant therapy, some of them die or stop growing and reproducing. However, there is always at least 20% hormonally independent cells. Over time, their clone becomes predominant, and the disease goes beyond hormonal control - hormonal resistance develops.
The diagnosis of hormonally resistant prostate cancer is established when the disease progresses against the background of adequate androgen blockade, confirmed by laboratory tests. In other words, the tumor progresses against the background of castration testosterone levels (not higher than 2 nmol/l). Currently, one of the areas of treatment for prostate cancer is to prolong hormonal sensitivity. For this purpose, various treatment regimens are being developed:
- Intermittent androgen blockade (IAB).
- Minimal androgen blockade.
- Delayed hormonal therapy.
Bilateral orchiectomy (castration)
Bilateral orchiectomy, or surgical castration, was the very first method of hormonal blockade for pancreatic cancer. A decrease in testosterone levels in this case is achieved within 12 hours. Psychologically, this operation is very difficult for patients to endure, since it has an irreversible effect. Moreover, the irreversibility of the effect also adversely affects the progression of the disease, since it limits the reserves of influence.
But recently it is gaining popularity again due to certain circumstances:
- LHRH analogues are characterized by fairly high cardiotoxic risks. External and aesthetic changes when taking them are similar to castration.
- Surgical removal has a rapid therapeutic effect.
- The cost of such treatment is much lower than lifelong medication.
Etiology and pathogenesis
The hormonal level and structural features of the hair follicle determine the condition of the hair - its length, thickness, crimp, growth rate, localization, etc.
After birth, thin and weakly pigmented hair gradually begins to grow on the child’s body - they are called vellus (vellus). Their diameter does not exceed 30 microns, their length is less than 2 cm. Vellus hair is devoid of medulla and the muscle that lifts the hair, and its bulb is located at the level of the reticular layer of the dermis. In adults, vellus is present on the scalp - for example, in the frontoparietal zone (here the norm is 20% of vellus hair).
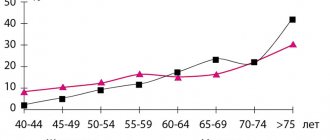
As we grow older, androgens are activated in the body, which contribute to the transformation of vellus hair into terminal hair (larger and more pigmented). The degree of transformation is influenced by the level and duration of androgenic effects, local activity of 5-alpha reductase in the area of hair follicles and their sensitivity to hormonal influences. At the same time, vellus hair remains in some areas of the body, which is normal (parietal area of the head, eyebrows, eyelashes).
In its development, hair goes through three phases - anagen (growth), catagen (transition to rest) and telogen (rest):
- In anagen, the hair actively grows, its bulb takes on a complete shape.
- In catagen, atrophy of the hair follicle begins to develop.
- In telogen, the hair shaft breaks away from the follicle and falls out over time, and young hair begins to mature near the follicle.
The main hormone to which the hair follicle reacts is dihydrotestosterone. It is not only present in human blood, but is also synthesized in the bulb area from its precursor, testosterone. Local production of dihydrotestosterone is determined by the activity of 5-alpha reductase in the skin. Differences in the activity of this enzyme are a criterion for why women with the same plasma testosterone levels may have varying degrees of hirsutism or no hirsutism at all.
The main causes of hirsutism:
- Polycystic ovary syndrome (PCOS) is the most common cause of hirsutism. PCOS is characterized by an imbalance of sex hormones, which leads to menstrual irregularities, obesity, multiple ovarian cysts and infertility.
- Cushing's syndrome occurs when there are high levels of cortisol in the blood. Its cause is either excess production of this hormone by the adrenal glands, or long-term use of certain medications (for example, glucocorticoids).
- Congenital adrenal hyperplasia is a hereditary pathology in which the adrenal glands synthesize large amounts of steroid hormones, including cortisol and androgens.
- Tumors are an uncommon but possible cause of hirsutism. The disease is usually caused by androgen-secreting tumors of the ovaries or adrenal glands.
- Medications —hirsutism can be caused by taking certain medications (synthetic androgens, systemic corticosteroids, a number of antidepressants).
Sometimes the disease occurs for no apparent reason - this is idiopathic hirsutism. It is a diagnosis of exclusion, i.e. it is diagnosed when all other possible causes of the disease are excluded. Most often, idiopathic hirsutism is recorded in women from the Middle Eastern, Mediterranean and South Asian regions.
Risk factors for hirsutism:
- Family history - it is worth paying attention not to cases of excess hair growth in the family, but to hormonal diseases in close relatives. Particular attention is paid to the presence of PCOS and adrenal hyperplasia.
- Origin - as mentioned above, women from the Middle Eastern, Mediterranean and South Asian regions experience hirsutism more often.
- Obesity increases the production of androgens, which increases the likelihood of hirsutism.
Use of estrogens
Estrogens block the production of LH and FSH and, accordingly, this leads to the suppression of testosterone synthesis. As a result, clinical and biochemical remission of prostate cancer occurs. Estrogens can be used as part of first- and second-line therapy. Their disadvantages are the following aspects:
- The need for daily administration via intramuscular injection.
- High cardiotoxic risks leading to myocardial and vascular damage. The risks are especially high when using high doses of drugs.
LHRH agonists
LHRH analogues (goserelin, leuprorelin, etc.). These drugs suppress the release of LH by the pituitary gland by desensitizing its receptors, which leads to a decrease in testosterone levels. When the drugs are discontinued, hormone production normalizes and returns to normal.
A feature of this treatment is an increase in testosterone release in the initial stages of therapy. This phenomenon is called the flash effect. This happens due to the fact that when taken for the first time, the drug causes the release of a large amount of LH into the blood, which leads to the production of a large amount of testosterone that exceeds normal values. This phenomenon is called the flash effect.
After a few weeks (usually 3-4), LHRH receptors are “overloaded” (desensitized) by this concentration of the hormone and become insensitive. Accordingly, the level of testosterone in the blood decreases to 50 ng/ml. To prevent the pathological effect of the flash effect, antiandrogens are prescribed in parallel, which prevent testosterone from binding to cell receptors, and it simply cannot exert its effect.
LHRH agonists are widely used for the treatment of prostate cancer due to a number of advantages. The main ones are the reversibility of the effect and a fairly favorable complication profile.
LHRH antagonists (degarelix)
Competitive binding to LHRH receptors in the pituitary gland is what underlies the mechanism of action of this group of drugs. They quite quickly lead to a decrease in testosterone levels and do not cause a “flash” effect. However, some patients may develop a severe allergic reaction. Therefore, the drug is prescribed only when it is impossible to use other types of antihormonal treatment.
Degarelix is administered by injection, always in the presence of a doctor. In the first month it is used once every 2 weeks, and then once every 4 weeks. After each injection, the patient remains under the supervision of medical staff for about half an hour to make sure there is no allergic reaction.
Clinical manifestations
Hirsutism is manifested by excessive growth of coarse and dark hair in places where women usually do not have it - most often on the face, chest and back ( Fig. 1 ). In this case, excess hair growth should be considered in connection with the racial characteristics of a particular person. What may be considered excessive for representatives of one race, will be within the average norm for others.
If hirsutism is triggered by very high levels of androgens, a woman may eventually develop virilism - the appearance of male secondary sexual characteristics:
- Deepening the voice
- Increased hair loss on the scalp followed by baldness
- Acne on the face and body
- Reducing breast size
- Increased muscle mass
- Increasing the size of the clitoris
Rice. 1. Signs of hirsutism on the face of an elderly woman (www.medscape.com)
Combined hormonal treatment
Combined hormonal treatment involves the simultaneous use of drugs with different mechanisms of action. These include minimal and maximal androgen blockade.
Maximum androgen blockade
Chemical or surgical castration only eliminates the testosterone produced by the testicles. However, there are still hormones produced by the adrenal glands. Their proportion of the total number, although small, can still stimulate the growth and development of pancreatic cancer cells.
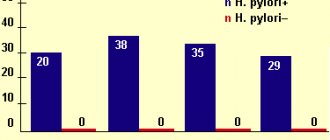
To prevent this, additional drugs are used that block the synthesis of adrenal hormones. In this way, a complete blockade of all androgens circulating in the blood is achieved. This therapy is called maximum androgen blockade (MAB). It was previously thought to improve overall patient survival. But in large clinical trials, it was found that a significant prolongation of life for patients with metastases could not be achieved. At the same time, surgical castration, as an independent method of treatment, provided a slightly better quality of life for such patients compared to drug therapy.
Thus, the following conclusions can be drawn regarding MAB:
- The use of maximum androgen blockade gives better treatment results compared to castration in no more than 10% of patients undergoing primary therapy.
- No significant difference in 2-year overall survival.
- Has many more side effects.
- Much more expensive than other types of treatment.
It is mainly used in cases where the possibilities of chemical or surgical castration have already been exhausted.
Minimal androgen blockade
Minimal androgen blockade involves the use of an antiandrogen and a 5-alpha reductase inhibitor (finastrenide). This drug blocks the action of 5-alpha reductase, an enzyme that converts testosterone into its active form, dihydrotestosterone. And nonsteroidal antiandrogens prevent the interaction of residual DHT with receptors of malignant cells. Sexual function is preserved in 60-88% of patients.
For some time, this treatment inhibits tumor growth and delays the need for castration. On average, this period is about 37 months. And only when the treatment stops working do they resort to more radical steps. This treatment is currently undergoing clinical trials and is being studied for its potential to delay the onset of secondary hormone resistance in prostate cancer.
Intermittent hormonal treatment
Intermittent hormonal treatment is a targeted alternation of periods of blocking and restoring hormonal stimulation of cancer. This makes it possible to partially preserve the hormonally dependent clone of malignant cells, thereby delaying the development of hormonal resistance.
Treatment is carried out according to the following scheme:
- First of all, hormonal therapy is prescribed. This happens until the PSA level drops below 4 ng/ml.
- Therapy is then discontinued and PSA levels continue to be monitored.
- When PSA exceeds the set value, for example, 20 ng/ml, therapy is resumed, and so on in a circle.
This scheme allows you to prolong the period of remission and produces fewer side effects than a permanent blockade. And what is important for the healthcare system in general is that it is cheaper than a permanent course of drugs.
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Hirsutism in women is excess male-pattern hair growth. Contrary to popular belief, the disease can also occur in men, but this article discusses only the female version.
In our company you can purchase the following equipment for the treatment of hirtusism in women:
- M22 (Lumenis)
- Lightsheer DUET (Lumenis)
- LightSheer DESIRE (Lumenis)
According to statistics, approximately 10% of women living in the United States and Northern European countries have signs of hirsutism. There is little reliable information for other regions of the world.
Immediate or delayed hormonal treatment for prostate cancer
At the end of the twentieth century, it was suggested that hormonal therapy for pancreatic cancer could be delayed until the tumor begins to progress, i.e., until the primary lesion begins to grow, or distant metastases occur. It was believed that in this case there would be one more chance of going into remission.
However, clinical trials have shown mixed results. For example, in the group of delayed hormonal treatment, cancer progression began more often and earlier and distant metastases occurred more often. Overall mortality during the follow-up period was also higher in the deferred therapy group. Thus, most researchers today are inclined to the need for immediate initiation of hormonal treatment.
Principles of treatment
Treatment for hirsutism begins with determining the cause of the condition. When the main etiological factor has been established, efforts should be directed towards its elimination - therapy for PCOS or a tumor, abolition of medications that affect hormonal levels, etc.
For some patients, cosmetic procedures will be sufficient; others will need to include systemic medications, surgery, and other techniques. The most effective strategy is considered to be complex treatment, which is based on a combination of drug therapy with hair depilation. Systemic drugs act gradually, so the effect of taking them develops after some time. To quickly improve the patient's condition (including psychological status), aesthetic procedures can be used.
Medicines for hirsutism
Glucocorticoids - suppress the production of adrenocorticotropic hormone (ACTH), which can be used for congenital adrenal hyperplasia or idiopathic hyperandrogenism. Unfortunately, some patients experience weight gain and Cushingoid symptoms during this therapy, even on low doses of medication.
Oral contraceptives are a fairly inexpensive and effective way to normalize the menstrual cycle. Their combination with antiandrogens or other types of therapy is optimal. Oral contraceptives are not recommended for use in patients with migraine, thromboembolic disease, breast or uterine cancer.
It should also be borne in mind that in 50% of cases, low-dose oral contraceptives and mini-pills are unable to suppress ovulation. The androgens produced continue to circulate in the blood, maintaining the symptoms of hirsutism. The likelihood of such an event depends on androgenic activity and the woman’s individual susceptibility to this therapy.
Spironolactone - reduces testosterone production by blocking androgen receptors, making it effective as an adjunctive therapy for hirsutism. Typically, spironolactone is prescribed at a dose of 50–200 mg per day.
Finasteride is a 5-alpha reductase inhibitor, which may be useful in hirsutism. Finasteride has a number of side effects, in particular a negative effect on libido. Therefore, it is recommended for postmenopausal women who no longer plan to become pregnant.
Flutamide is a non-steroidal selective antiandrogen that does not have progestinal, estrogenic, corticoid or antigonadotropin activity. It is an example of a modern drug therapy strategy. Preliminary data indicate that flutamide is effective in treating hirsutism, but the drug is very expensive and can cause severe hepatitis in some cases.
Cosmetic care for hirsutism
To remove unwanted hair, you can use shaving, plucking, waxing, chemical or machine depilation, electrolysis or short-wave diathermy. It should be taken into account that chemical depilation can cause skin irritation, plucking can cause folliculitis, diathermy and waxing can cause scarring.
Hardware methods of hair removal for hirsutism
Hardware methods for getting rid of unwanted hair in hirsutism include two areas - lasers and intense pulsed light (IPL). Both of them selectively target hair follicles with light, heating them and causing destruction. Hair stops growing until new follicles form in the skin.
The main difference between laser systems and IPL is the duration of the procedure and the cost of the device itself. Intense pulsed light does not remove hair as quickly or efficiently as lasers, so each session takes longer. However, the cost of IPL devices is on average lower.
Among lasers, the most versatile solution for removing unwanted hair on the face and body are 800–810 nm diode lasers . They can be used in patients with any skin phototype (up to V–VI) and any hair color, including blond or red. At the same time, the skin and surrounding tissues practically do not heat up, and for greater patient comfort, a cooling system can be built into the handle of the device.
Questions from our users:
- hirsutism treatment drugs
- hirsutism laser hair removal
- hirsutism with normal hormones
- hirsutism additional symptoms
Monitoring patients undergoing hormonal treatment
The effect of hormonal treatment for pancreatic cancer is assessed 3 and 6 months after its initiation. The examination includes PSA level measurement and digital rectal examination. In the absence of metastases, further observation is recommended every 6 months. If there are metastases, but the treatment has had a positive effect, observation is carried out every 3 months. If the malignant process is stabilized, additional medical imaging methods are not required (ultrasound, CT, scintigraphy, etc.).
Basics of treatment with antitumor drugs - androgens
All antitumor drugs, including androgen drugs, are prescribed only by an experienced oncologist.
The use of antitumor drugs is also under the strict supervision of a physician. This is due to the high toxicity of cancer treatments, as well as the high risk of interaction with other drugs or food.
Androgen preparations are used in the form of oil solutions intramuscularly once every few weeks for a long time.
The duration of androgen treatment is determined by the doctor depending on the form and severity of the disease.