Anticholinergics (anticholinergics) are medications that block different types of cholinergic receptors in organs and tissues, preventing the effects of a natural biologically active substance - the mediator acetylcholine.
Acetylcholine is a transmitter of impulses in the peripheral nervous system, regulating the functioning of many internal organs and systems (in particular, the brain, heart, bronchi, uterus, gastrointestinal tract, urinary system, etc.).
Acetylcholine realizes its effects by interacting with special structural components of cells - receptors, namely cholinergic receptors. Depending on their location and functions, adrenergic receptors are classified into M- and N-cholinergic receptors.
M-cholinergic receptors are located mainly in the brain, heart, bronchi, gastrointestinal tract, iris, and urinary tract. The effects of M-cholinergic receptor stimulation include pupil constriction, decreased intraocular pressure, increased gastric acid production, increased secretion of digestive glands, increased gastrointestinal motility and peristalsis, increased bladder tone, and decreased heart rate.
N-cholinergic receptors are localized mainly in skeletal muscles, as well as in special structures - autonomic ganglia and carotid glomeruli. When they are stimulated, muscle contraction, vasoconstriction (and, as a consequence, increased blood pressure) and stimulation of the respiratory center in the brain are observed.
There is a separate class of drugs that can stimulate cholinergic receptors (cholinomimetics, anticholinergics), and a group of drugs that can block cholinergic receptors (cholinergic blockers, anticholinergics).
Depending on the type of receptors blocked, anticholinergics are divided into M-anticholinergics, as well as N-anticholinergics (which, in turn, are divided into two separate classes: ganglion blockers and muscle relaxants). Let us consider in detail drugs that block M-cholinergic receptors.
Indications for use
M-anticholinergic drugs are used for diseases of the gastrointestinal tract associated with spasms and excessive secretion of glands: gastric and duodenal ulcers, acute pancreatitis, cholecystitis, cholelithiasis, hepatic and intestinal colic.
M-anticholinergic drugs are also used for diseases associated with bronchospasm - bronchial asthma, chronic obstructive pulmonary disease.
M-anticholinergic agents are used to dilate the pupil and examine the fundus of the eye, as well as when selecting glasses and contact lenses to determine the refractive power of the eye lens.
M-anticholinergics are prescribed for an overactive bladder - frequent urination, urinary incontinence, and also for renal colic.
In addition, M-anticholinergic blockers are used for bradycardia, before operations to reduce the negative effects of anesthesia, as well as in case of poisoning with cholinomimetics and anticholinesterase drugs (including pesticides).
Platyphylline hydrotartrate is also used for hypertensive crisis - a sharp excessive increase in blood pressure.
pharmacology of spurs / N-anticholinergics
N-cholinergic blockers: 1) ganglion blockers (benzohydrixonium, pachycarpine, pentamine) 2) muscle relaxants with depolarizing action (ditylin) and antidepolarizing action (tubocurarine, diplacin). The mechanism of action of each group of drugs, practical significance.
N-cholinergic blockers are substances that block nicotinic cholinergic receptors. These include ganglion blockers and peripherally acting muscle relaxants (curare-like drugs).
Ganglioblockers
Ganglioblockers are agents that block the transmission of excitation in the autonomic ganglia (parasympathetic and sympathetic), as well as H-cholinergic receptors in the cells of the adrenal medulla. As a result, peripheral vessels dilate and blood circulation improves, blood vessels dilate (arterial and venous) and blood pressure decreases, and the secretory and motor functions of the stomach and intestines deteriorate.
Benzohexonium has sufficient activity and acts for 3-5 hours. It dilates peripheral vessels and lowers blood pressure, and has an antispasmodic effect.
Indications for use: spasms and diseases of peripheral vessels (endarteritis), hypertensive crisis, peptic ulcer of the stomach and duodenum, pulmonary and cerebral edema, gestosis. The dose is selected individually.
Dimecoline has a pharmacological action similar to benzohec-Sone, but is more active. Used to treat patients with stage II hypertension. Treatment begins with low doses, which are gradually increased until the optimal therapeutic effect is achieved.
Pentamine is inferior to benzohexonium for its ganglioblocking properties. Administered only parenterally. Duration of action - 2-4 hours. Prescribed for spasms of peripheral vessels, hypertensive crisis, cerebral edema, pulmonary edema, colic (intestinal, renal), acute attacks of bronchial asthma, eclampsia.
Pyrilene is well absorbed from the gastrointestinal tract and exhibits a constant therapeutic effect within 5-8 hours. The drug blocks the transmission of nerve impulses in the sympathetic and parasympathetic ganglia. Easily penetrates the BBB and blocks N-cholinergic receptors of the central nervous system. Does not accumulate. Prescribed for the treatment of patients with hypertension, endarteritis, gastric and duodenal ulcers, peripheral vascular spasms, and toxicosis of pregnancy.
Hygronium is a drug similar to benzohexonium. The antihypertensive effect after intravenous administration occurs within 2-3 minutes and lasts 10-30 minutes. Prescribed to patients with controlled arterial hypotension, and also used in obstetric practice (for nephropathy in pregnant women, eclampsia).
Side effects and complications of ganglion blockers: orthostic collapse, general weakness, dry mouth, dilated pupils, atony of the bladder and intestines.
Contraindications: myocardial infarction, acute stage of arterial hypotension, kidney and liver damage, thrombosis, degenerative changes in the central nervous system. Use with caution in elderly people.
pharmachologic effect
M-anticholinergics have a wide range of pharmacological effects: dilate the pupil, relax the bronchi, increase the frequency and strength of heart contractions, reduce the formation of gastric acid, inhibit the secretion of glands of the digestive tract, reduce gastrointestinal motility and peristalsis, reduce bladder tone and cause relaxation smooth muscles of the urinary tract.
Platyphylline hydrotartrate additionally dilates blood vessels and lowers blood pressure.
Classification of M-anticholinergic drugs
Drugs of the M-anticholinergic group are classified into:
- systemic drugs: atropine sulfate, butylscopolamine (scopolamine butylbromide), hyoscine, platiphylline hydrotartrate;
- selective M1-anticholinergic blockers that affect the formation of hydrochloric acid in the stomach: pirenzepine, telenzepine;
- drugs affecting bronchial tone: ipratropium bromide, tiotropium bromide, umeclidinium bromide, aclidinium bromide, glycopyrronium bromide;
- drugs that affect bladder tone: tolterodine, oxybutynin, solifenacin, darifenacin, trospium chloride;
- drugs that affect pupil size: atropine sulfate, tropicamide, cyclopentolate.
M-anticholinergics in the treatment of overactive bladder
Overactive bladder (OAB) is a severe urinary disorder that affects at least 17% of the population over 40 years of age, of whom 56% are women and 44% are men (16). At the same time, there are differences due to gender, age, and ethnicity.
Figure 1. Prevalence of OAB in different age groups (Milsom I., Abrams P., Cardozo L. et al., 2001)
Figure 2. Prevalence of OAB symptoms (SIFO Group Survey)
Table 1. Topical characteristics of M-cholinergic receptors in the human body (BJU may 2000; Vol. 85, Supp. 3: 35)
Table 2. Comparison of the affinities for M-cholinergic receptors (in vitro) of tolterodine and oxybutynin
Table 3. Comparative characteristics of the selectivity of various M-anticholinergic drugs (Vesicare SmPC, Astellas, 2005)
Table 4. Changes in core symptoms of detrusor overactivity based on 12-week studies of fesoterodine (Pfizer labs., 2008)
Typically, the prevalence of OAB is underestimated because the vast majority of studies include patients with only one of the symptoms of urge incontinence (14, 16). With age, the number of patients with various disorders of the lower urinary tract function increases significantly, especially with OAB (Figure 1) (8, 20).
Some current evidence suggests that the role of M2 receptors may be more pronounced with age. It is believed that these receptors may play an important role in the age-dependent increase in the α1-adrenergic receptor response in bladder tissue, and facilitation of the contractile response associated with α1A-adrenergic receptors may be the cause of bladder overactivity in older people.
The clinical manifestation of detrusor overactivity is characterized by urgency, pollakiuria, nocturia, and urge incontinence (or urge urinary incontinence) (Figure 2). Occurring at any time and often in an inconvenient place, these symptoms bring significant anxiety to patients.
Urinary incontinence, or even urinary incontinence, may also be a consequence of urethral instability caused by fluctuations in maximum urethral pressure of more than 15 cmH2O. Art. Urinary incontinence is not a prerequisite for a diagnosis of OAB, since half of the patients have only sensory symptoms: frequent daytime and nighttime urination, urgency. This variant of the symptom complex is called dry OAB.
It should be borne in mind that the presence of detrusor overactivity detected during urodynamic study does not mean that the patient should suffer from urinary incontinence. For example, asymptomatic detrusor overactivity is reported in 42% of healthy women over 65 years of age (20). In the case of urge urinary incontinence, it is customary to talk about wet, or wet, OAB (14, 20, 22).
With age, researchers note a significant increase in the proportion of wet OAB. Between the ages of 65 and 74 years, up to 20% of women experience urge urinary incontinence. According to a Swedish study, in older people 75 years of age and older, 42% of women and 35% of men suffer from urge urinary incontinence (Stenzelius K., Mattiasson A., Hallberg IR, Westergren A., 2004).
With age, the frequency of symptoms increases to 30% in people over 65 years of age and to 40% after 70 years of age. In European countries, almost 22 million people suffer from this serious disease, but only 27% of them receive treatment, indicating a lack of recognition of the problem by both patients and health care providers (20).
The prevalence of urinary frequency and urgency is similar among men and women, and urge incontinence is more common in women in older age groups. The etiology and pathogenesis of imperative urinary disorders caused by bladder overactivity are still unclear. There are several theories about the development of this disease. Nerve degeneration is a common sign of developing an unstable bladder. It is possible that detrusor overactivity is caused by age-related changes not only in the urinary tract, but also in the central nervous system (CNS). It is obvious that various changes in both the peripheral nervous system and the central nervous system can be the cause of detrusor overactivity.
There is an opinion that the etiology of OAB is associated with qualitative changes in the smooth muscles themselves. Normally, smooth muscle cells in the bladder are in a state of spontaneous activity. During filling, however, their activity is not synchronized because each of the cells is connected to only a few of its neighbors, and there is no particular interconnection between individual bundles. The synchronous activation observed during micturition is not possible without dense dense innervation, and large numbers of smooth muscle cells must be activated by nerve impulses.
Elbadawi A. et al. (1997) used electron microscopy to examine biopsy tissue samples from elderly patients with urodynamically documented voiding dysfunction. The researchers described a so-called circuit breaker pattern, or disconnected pattern, found in patients with OAB. The peculiarity of this model was the moderate expansion of intercellular spaces, the presence of rare intermediate connections between cells, but was distinguished by the excessive content of special characteristic protruding joints and the close fit of cell supports. It has been suggested that protruding junctions and cellular support borders mediate direct communication between individual smooth muscle cells and that they are involved in the generation of muscle contraction in patients with OAB. Five patients initially in this study with detrusor stability developed a detrusor overactive state over time. Ultrastructural studies of new biopsy materials showed the presence of a so-called disconnection pattern, in contrast to previous biopsies performed on the same patients (Elbadawi A., Hailemariam S., Yalla SV, Resnick NM, 1997).
In older men, the development of OAB symptoms is often accompanied by bladder outlet obstruction (IVO) as a result of prostate disease. About 60% of men with BOO report symptoms of OAB. There is no precise explanation for the relationship between bladder outlet obstruction and OAB. According to Wein AJ (2003), OAB occurs in 52-80% of men with BOO due to prostatic hyperplasia, and in 38% of men it continues to occur after surgical removal of obstruction.
Existing studies indicate a number of neurological changes (Steers WD, De Groat WC, 1988, Sibley GN, 1987) and an increase in α-adrenergic activity as a result of detrusor ischemia (Perlberg S., Caine M., 1982) due to its hypertrophy against the background of IVO. With detrusor hypertrophy resulting from obstruction, metabolic demands increase coupled with decreased blood flow, leading to anoxia and neuronal death (Levin RH et al., 1999). Moreover, there is evidence that the density of cholinergic nerve fibers in the detrusor is 60% less in the group of patients with BPH and BOO compared to a group of patients of the same age and without BOO. The authors believe that a significant decrease in nerve fiber density in response to BOO due to BPH may lead to impaired neuromuscular control of the bladder.
A large role in the development of imperative urination disorders in menopausal women is given to estrogen deficiency and associated atrophic changes in the urothelium and dystrophic changes in the bladder muscle (2-4). This may be the cause of the sensory symptoms that accompany dry OAB (pollakiuria, nocturia, urinary urgency). 70% of women associate their appearance with the onset of menopause (16), which is considered one of the main risk factors for the development of OAB in women. According to Versi E. et al. (1995), the frequency of stress urinary incontinence in women decreases with increasing duration of postmenopause, and simultaneously with increasing age, the frequency of detrusor overactivity increases. Some studies have shown that individual neurons in the spinal cord contain estrogen receptors and are targets for estrogen. The presence of estrogen receptors in neurons of central brain regions raises the possibility that endocrine age-related changes may act through supraspinal voiding control.
The development of detrusor hypoxia and, as a consequence, metabolic disorders in its structure impairs its contractility. This suggests that ischemia and hypoxia may underlie intramural neuronal damage and lead to changes in bladder smooth muscle function in patients with detrusor overactivity. Ischemia leads to apoptosis of smooth muscle cells, in addition to disruption of nerve conduction. Nerve tissue is more sensitive to ischemia than smooth muscle, and some of this damage is almost irreversible. Nerve degeneration is a common sign of developing an unstable bladder. With detrusor hypertrophy resulting from obstruction, metabolic demands increase coupled with decreased blood flow, leading to anoxia and neuronal death (Levin RH, 1999).
Abrams P. (1985) believes that detrusor overactivity in patients with BPH is not the result of BOO, but a consequence of age-related changes in the bladder wall. Despite the conflicting data, it should be recognized that both age and BOO can lead to postsynaptic denervation of the bladder. This circumstance once again emphasizes the important role of the nervous system in controlling the storage function of the bladder.
The role of hereditary factors is being studied, and a number of modern studies indicate the possibility of genetic changes in the presence of OAB.
According to the classical physiological concept, bladder function is ensured by the antagonistic interaction of the sympathetic and parasympathetic parts of the nervous system (14). The sympathetic department is responsible for relaxing the detrusor and contracting the urethral sphincter, the parasympathetic department is responsible for contracting the detrusor and relaxing the sphincter. Activation of one or another system determines the condition of the lower urinary tract. Receptors in the area of the endings of the sympathetic nerves of the bladder and urethra, depending on the physiological effects that occur when they are stimulated, are divided into a- and b-adrenergic receptors.
Stimulation of a-adrenergic receptors leads to a contraction of smooth muscle fibers of these parts of the urinary tract and an increase in urethral resistance. Stimulation of b-adrenergic receptors causes inhibition of detrusor activity and its physiological adaptation to the incoming volume of urine. Adrenergic inhibitory neurons mainly arise from n .
hypogastricus
, while the excitatory nerves are believed to arise from the pelvic nerve and are of the cholinergic type. The receptors of the parasympathetic (cholinergic) nerve system are evenly distributed in the muscular wall of the bladder and are almost never found in the area of its base and urethra. Stimulation of these receptors causes detrusor contraction.
There are currently five known molecular subtypes of muscarinic M-cholinergic receptors, and tissues can contain varying numbers of different subtypes (Table 1).
For example, human bladder smooth muscle contains mixed populations of M2 and M3 subtypes. Particularly noteworthy are the M3 receptors, through which the impulse to contract the detrusor is transmitted, and the M2 receptors, the effect on which prevents the relaxation of its smooth muscles. The main number of muscarinic receptors in the bladder falls on the M2 subtype (80%). It is known that M2 receptors make up 4/5 of all muscarinic receptors in the bladder.
Stimulation of M3 receptors by acetylcholine leads to phosphoinositol hydrolysis and ultimately to the accumulation of intracellular calcium and smooth muscle contraction. Activation of M2 receptors leads to inhibition of adenylate cyclase and restores sympathetic-associated relaxation of bladder smooth muscle. The end result is the most efficient and complete emptying of the bladder.
Some current evidence suggests that the role of M2 muscarinic receptors may be more pronounced with age. The predominance of activity of cholinergic receptors of the parasympathetic part of the autonomic nervous system is characterized by a decrease in the physiological capacity of the bladder during the filling phase, a rapid increase in detrusor pressure, as well as an increase in intravesical and detrusor pressure during the emptying phase with an increase in the maximum volumetric flow rate of urine and a reduction in urination time.
The prevalence of activity of b-adrenergic elements of the sympathetic link is determined by an increase in the physiological capacity of the bladder and a decrease in the maximum values of intravesical and detrusor pressure. The presence of uncoordinated contractions of the detrusor is regarded as evidence of increased activity of muscarinic-sensitive cholinergic neurostructures, evenly distributed throughout the detrusor body. It is known that the function of the lower urinary tract is carried out due to the close antagonistic interaction of adrenergic and cholinergic receptors of the sympathetic and parasympathetic parts of the autonomic nervous system. Therefore, it is clear that if at least one type of receptor is damaged or functionally insufficient, this entire system of harmonious balance is certainly disrupted due to the predominance of the action of the opposite group of receptors (11).
According to modern understanding, many receptors for various transmitters have been found in the lower urinary tract, including such as nitric oxide and substance P. Various co-transmitters and neuromodulators have a stimulating effect on bladder smooth muscle, such as ATP, substance P, GABA, NPY and various others. The possible presence of various neurotransmitters and modulators in the lower urinary tract has been much debated over the past twenty years.
The connection between detrusor hyperactivity and increased activity of the parasympathetic division of the autonomic nervous system has been proven and explains the therapeutic effect of the use of blockers of peripheral muscarinic-sensitive cholinergic receptors. Against their background, the influence of the parasympathetic link weakens, and the sympathetic one increases, thereby reducing intravesical pressure, uncoordinated contractions of the detrusor are reduced or suppressed, the effective capacity of the bladder increases and the adaptive function of the detrusor improves (5, 6).
Pharmacotherapy is one of the most common methods of treating OAB. According to the recommendations, this is the method of choice. This is followed by behavioral therapy, physical therapy and other treatments. The drug method is of interest primarily due to its availability, the possibility of long-term use and individual selection of the dose and treatment regimen. Pathogenetic pharmacotherapy should be focused on the possible mechanisms of development of OAB - myogenic and neurogenic. Pharmacological treatment of overactive bladder is a complex problem. Both domestic and foreign scientists have dealt with the issue of symptomatic treatment of this condition.
For the treatment of OAB, anticholinergic drugs are most often used, first proposed by Langworthy O. (1936), which disrupt the conduction of impulses in the parasympathetic ganglia or prevent the interaction of the parasympathetic transmitter acetylcholine with M-cholinergic receptors (Diokno A. Lapides J., 1972). Most of these drugs cause inevitable side effects, which makes it necessary for the doctor to maintain a balance between the advantages and disadvantages of the drugs. Antimuscarinic action usually causes dry mouth, constipation, difficulty in accommodation, and drowsiness. The drugs should not be prescribed to patients with impaired urine flow from the bladder (obstructive uropathy), bowel obstruction, ulcerative colitis, glaucoma, or myasthenia gravis. In a normal bladder, cohesion between muscle fiber bundles ensures that the occurrence of diffuse activity does not lead to an increase in bladder pressure. In an unstable (overactive) bladder, these connections are strengthened, which leads to a wave of diffuse excitation, urgency and uncontrolled detrusor contractions. This hypothesis explains the effectiveness of antimuscarinic drugs in urge urinary incontinence. If some of the ganglia are excited directly by sensory nerves, then suppression of this effect should lead to the elimination of both urgency and unstable contractions.
One of the most well-known anticholinergic drugs is atropine, which has a pronounced systemic effect. And although some pilot studies have shown significant effectiveness and safety of its intravesical use for hyperreflexia, the most common method of administration at present is electrophoresis. The lack of selectivity of the drug's action, without a doubt, becomes a negative factor, since it determines the low effectiveness of its therapeutic doses against the symptoms of hyperactivity. The drug is currently of more historical interest, and is practically not used in the treatment of detrusor overactivity.
Fowler S. (1996) proposed an anticholinergic drug - oxybutynin. Previously, oxybutynin, which has antimuscarinic, antispasmodic and local anesthetic effects, was called the “gold standard” in the treatment of OAB, although not all of the above properties are observed when using therapeutic doses. Individual dosage adjustment is necessary, and patients are warned that this will take a certain period of time, during which it is necessary to visit a doctor. The optimal dose is considered to be the one that gives the desired effect with minimal side effects. Doses for oral administration range from 2.5 mg once to 5 mg 4 times a day. The standard starting dose for adults is 5 mg 2-3 times a day. In the elderly, a rational starting dose is 2.5 mg 2-3 times a day. The dose must be maintained for 7 days before adjustment (either decreasing or increasing, depending on the severity of the clinical effect). In order to reduce the severity of side effects, the dose of oxybutynin is reduced. Malone-Lee J. et al. (1992) suggested reducing the dose to 5 mg per day, Moore K. et al. (1990) – up to 3 mg, and Bemelmans BLH et al. (2002) – up to 2.5 mg 3 times a day.
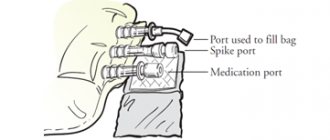
If oral administration of oxybutynin is not possible, Brendler C. et al. (1989), Maderbacher H., Jilg G. et al. (1985), Weese D. et al. (1993) proposed a method of administering 5 mg of oxybutynin directly into the bladder, dissolved in 30 ml of sterile water, 2-3 times a day. Enzelsberger et al. (1995) proposed 20 mg of oxybutynin dissolved in 40 ml of water to be administered into the bladder for 10 days. In a double-blind, randomized study, no adverse reactions were noted, and the use of intravesical oxybutynin was recommended in case of severe side effects with oral administration.
An alternative method of using oxybutynin in rectal suppositories was proposed by Wiskind AK et al. (1994). A good therapeutic effect was noted, but side effects such as dry mouth and inhibition of peristalsis persisted.
Tolterodine is the first drug specifically developed for the treatment of patients with bladder overactivity, manifested by frequent urinary urgency and urge urinary incontinence. This drug is developed using an integrated approach to achieve bladder selectivity. Tolterodine is a competitive antagonist of M-cholinergic receptors, which is a mixed antagonist of M2 and M3 cholinergic receptors localized in the bladder and salivary glands, blocks calcium channels and, thus, has a dual effect on the bladder. The drug is selective for the bladder. The safety, efficacy and tolerability of tolterodine were assessed in four randomized, double-blind, parallel, multicenter, 12-week studies in patients with overactive bladder (Appell RA, et al., 2001, Drutz H., Appell RA, 1997, Nilvebrant L. et al., 1997). Studies have shown good tolerability of the drug, high efficiency and pronounced selectivity for cholinergic muscarinic receptors of the bladder compared to receptors of the salivary glands, in contrast to oxybutynin (Table 2).
The selectivity of tolterodine allows for long-term use of the drug. Moreover, according to research results, the frequency of side effects with long-term (up to 2 years) use of tolterodine does not increase, but rather decreases. Thus, the incidence of dry mouth after a year of using the drug is 36%, and by the second year of taking the drug it decreases to 19% (16). The frequency of urination after 12 months of use decreased by 22% and the frequency of episodes of urge incontinence by 58%.
In foreign literature there is data on the use of tolterodine in children 1 mg 2 times a day, which led to a decrease in the frequency of urination, a decrease in episodes of urinary incontinence, and there were no serious side effects. A study by M. Munding and H. Wessells (2001) found that tolterodine reduces the number of episodes of urge incontinence. Improvement or cure was observed in 73% of children taking the drug. According to P. Abrams et al. (2001), tolterodine does not significantly reduce peak urinary flow rate, does not reduce detrusor pressure at peak urinary flow rate, and does not cause a clinically significant increase in residual urine in men with OAB and BOO due to BPH. This effect of tolterodine is undoubtedly very important in such a large category of urological patients.
Another form of tolterodine is extended-release capsules of 4 mg, used once a day (except for patients with severe impairment of liver and kidney function, in which case capsules of 2 mg per day are used).
Another M-anticholinergic drug that is used to treat OAB is trospium chloride. It is a parasympatholytic with peripheral, atropine-like effects, as well as ganglionic myotropic effects similar to papaverine. Trospium chloride is a competitive antagonist of acetylcholine at postsynaptic membrane receptors, blocks the muscarinic action of acetylcholine and inhibits the response caused by postganglionic parasympathetic activation of the vagus nerve. It has a high affinity for M1 and M3 cholinergic receptors. Trospium chloride reduces the tone of the smooth muscles of the bladder, has a relaxing effect on the smooth muscles of the detrusor bladder, both due to the anticholinergic effect and due to the direct myotropic antispastic effect.
Trospium chloride is a quaternary ammonium compound with an antimuscarinic type of action. Although the bioavailability of trospium chloride is inferior to that of tertiary amines, this does not affect its effectiveness, but only determines the need for its use in higher doses. The dose of the drug is selected individually from 30 to 90 mg per day, depending on the clinical picture and severity of the disease. The concentration of trospium chloride after a single dose ranges from 20 to 60 mg, proportional to the dose taken. Trospium chloride is more hydrophilic relative to the tertiary compounds oxybutynin and tolterodine, penetrates the blood-brain barrier less well and is less likely to cause side effects from the central nervous system.
A study of 75 women with OAB incontinence (Fuertes et al., 2000) demonstrated not only an effective effect of trospium chloride (daily dose 40 mg, treatment duration 8 weeks) on the clinical manifestations of detrusor overactivity and urodynamic parameters, but also an improvement in quality indicators patients' lives by 35%. When comparing the effectiveness of trospium chloride and tolterodine in a double placebo-controlled study in patients with urinary urgency disorders, both drugs showed a decrease in urinary frequency - by 23% and 28% for tolterodine and trospium chloride, respectively, and an increase in urinary volume - by 39% and 33% respectively. The number of episodes of urinary incontinence was reduced by 67% and 73% for tolterodine and trospium chloride, respectively. The severity of side effects was similar in both subgroups (12). According to D.Yu. Pushkarya et al. (2004), while taking trospium chloride for 12 weeks, there was a decrease in the number of urinations per day by 20%, a decrease in the average number of episodes of urinary incontinence by up to 40%, and an increase in the volume of urination by 18.8%.
A new drug successfully used to treat OAB is the M-anticholinergic blocker solifenacin (Vesicare). Solifenacin, the active substance of Vesicare, is a specific competitive inhibitor of muscarinic receptors (M-cholinergic receptors), predominantly of the M3 subtype. However, solifenacin has low or no affinity for other receptors and ion channels. The maximum effect after taking Vesicare in doses of 5 or 10 mg can be detected after 4 weeks, which was shown in double-blind randomized clinical trials in men and women with OAB syndrome. The clinical effect of taking Vesicare is observed within the first week of treatment, and effectiveness remains for at least 12 months. There is no need to adjust the dose of Vesicare depending on the patient's age. The area under the concentration/time curve (AUC) is similar in elderly (65-80 years) and healthy young adults (<55 years). The time to reach maximum concentration is slightly lower, and the half-life is increased by 20% in elderly patients. These differences are not clinically significant.
The initial dose of Vesicare is 5 mg 1 time per day; if necessary, the dose can be increased to 10 mg 1 time per day. The most common side effect of Vesicare is dry mouth (occurring in 11% of patients receiving a daily dose of 5 mg and 4% receiving placebo). Solifenacin is characterized by a low incidence of side effects typical of antimuscarinics (for example, dry mouth), which is due to the higher selectivity of the drug to bladder tissue. Vesicare is more bladder selective than tolterodine and oxybutynin (Table 3).
The effectiveness of the drug in doses of 5 mg 10 mg has been studied and proven in many clinical studies in patients with OAB syndrome: a statistically significant decrease in the number of urinations (including at night), episodes of urgency, and an increase in the average volume of urination was noted. The effect appeared already during the 1st week of treatment, reaching its maximum value after 4 weeks. The effectiveness of the drug is maintained over long-term use (at least 12 months).
According to studies, with the use of solifenacin at a dose of 5 mg and 10 mg per day, the number of episodes of urgency is reduced by 49% and 55%, respectively, the number of episodes of urgent urinary incontinence - by 58% and 62%, respectively, the frequency of urination (by 5 mg per day) – by 19%, and the volume of urine excreted increases by 21% (VesicareÒ SmPC, Astellas, 2005).
Taking into account the high selectivity and good tolerability of the drug, its high effectiveness is noted with long-term (up to 60 weeks) use. According to the results of a study conducted by Haab F. et al. (2005), after 60 weeks of use of solifenacin at a dosage of 5 mg per day, 62.7% of patients began to retain urine, 43.1% decreased episodes of urgency, 41.8% decreased urinary frequency, 23.1% of patients got rid of nocturia. 81% of patients participating in the study completed the study, and only 4.8% dropped out due to adverse events.
Of the M-anticholinergic blockers that are not yet registered in Russia, darifenacin and fesoterodine should be noted. Darifenacin is an M3 receptor antagonist, but is characterized by a more selective effect compared to other anticholinergic drugs. So far it is known that at a dose of 2.5 mg it does not affect the salivary glands. With darifenacin treatment, urodynamic parameters improve only at a dose of 10 mg per day (24).
Fesoterodine is a new muscarinic receptor antagonist also used as a drug to treat OAB syndrome. The effectiveness of fesoterodine was shown in blinded randomized controlled trials in comparison with placebo and with tolterodine. The European Medicines Agency approved the use of fesoterodine in clinical practice in April 2007. The recommended starting dose of fesoterodine is 4 mg per day once (the dose can be increased to 8 mg once). The bioaccumulation of the active metabolite of fesoterodine is 52%. After a single or multiple oral
dose of fesoterodine from 4 mg to 28 mg, plasma concentrations of the active metabolite are proportional to the dose taken . After approximately 5 hours, maximum plasma levels of the drug are reached. Accumulation of the drug in the blood does not occur even with multiple doses of fesoterodine. The results of clinical 12-week studies of fesoterodine in relation to the main symptoms of OAB are presented in Table 4.
In addition to the above-mentioned selectivity for the bladder, an important property of Vesicare and other selective M-anticholinergics is the convenience of administration - once a day, which, along with high safety, significantly increases adherence to treatment on the part of patients. The emergence of such modern drugs gives hope for more effective, safe and convenient treatment of patients with OAB in the future. The results of the studies demonstrate more significant indicators of the effectiveness of M-anticholinergic blockers in combination with a-blockers in various groups of patients, as well as drugs for hormone replacement therapy in menopausal women.
It is likely that in the future it is necessary to move away from the principles of monotherapy for symptoms of a complex of imperative urination disorders, since we see a real way to increase the effectiveness of treatment of this complex disease in complex therapy, including not only various types of pharmacotherapy, but also physical, psychological and other methods of treatment.