Benfotiamine is a substance obtained artificially by scientists from Japan. The compound was synthesized in an attempt to find a remedy to combat vitamin B1 deficiency, which occurs in people whose diet consists mainly of white rice. Used in 1954, the substance became the most effective and safest remedy for the body to cure vitamin deficiency, which was given the name beriberi. In the process of continuous research, a number of properties of benfotiamine have been discovered that have a beneficial effect on the body.
Benfotiamine - what is it?
Let's figure out what kind of vitamin benfotiamine is by looking at its chemical properties. It refers to compounds that perform the same functions as B vitamins, the deficiency of which is effectively compensated by the use of this type of substance. Benfotiamine is lipid soluble. The increased effectiveness of the compound when used to correct deficiency is due to the fact that it has high bioavailability and is not destroyed by thiaminase.
Diabetic nephropathy
Diabetic nephropathy is a health- and life-threatening, constantly progressive complication of diabetes. It is characterized by significant structural changes in the kidneys, namely: thickening of the glomerular basement membrane, glomerular hypertrophy, sclerosis, expansion of mesangial cells, tubulointerstitial fibrosis and inflammation [10, 11]. Benfotiamine in high doses prevents the development of diabetic nephropathy, acting as described above by activating transketolase in the glomeruli and reducing AGE deposits, reducing inflammation and oxidative stress, and thereby reducing micro- and macroproteinuria, as well as the progression of kidney damage [12, 13].
The combination of benfotiamine and fenofibrate in a pilot study showed a synergistic effect in preventing the progression of diabetic nephropathy in rats [14].
A double-blind, placebo-controlled study in patients with type 2 diabetes at the stage of microalbuminuria examined renal function when treated with benfotiamine (900 mg/s) and placebo for 12 weeks together with angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists [15]. Despite the improvement in thiamine saturation, there was no reduction in the degree of microalbuminuria, which may be due to the short study period.
Benfotiamine and thiamine - what's the difference?
The difference between benfotiamine and thiamine is that the second of them is subject to destruction by thiaminase, which is why it may not be enough for the full functioning of the body, and the first has a lipophilic structure, due to which it is absorbed more quickly by the body. Unlike its analogue, benfotiamine is combined with vitamins , , B12, as well as calcium and magnesium, helping to increase their effectiveness and improve metabolism. This substance does not cause an allergic reaction or side effects from the gastrointestinal tract.
Benfotiamine in clinical practice
In 1929, the Dutch doctor Christian Eijkman (Ch. Eijkman) received the Nobel Prize for discovering the cause of beriberi disease, in which severe polyneuropathy was detected - a deficiency of thiamine (vitamin B1). Thiamine has been widely used for many decades to treat various neurological diseases of the peripheral nervous system [32]. The main disadvantage of the water-soluble thiamine compounds used was their low bioavailability when taken orally, due to the destruction of water-soluble thiamines by intestinal thiaminases. The bioavailability of thiamine limits the absorption barrier. Various studies have shown that the absorption of thiamine is subject to a dose-dependent dual mechanism.
Up to a concentration of approximately 2 mmol, thiamine is actively absorbed through a saturation mechanism, which at higher dosages is superimposed by passive diffusion, which is less effective. The supply of water-soluble thiamine into the cytoplasm of cells is insufficient due to poor penetration through the lipid layers of membranes. These disadvantages do not exist in fat-soluble compounds with thiamine-like activity, which are dose-dependently absorbed in the intestine, are not destroyed by thiaminases, and easily penetrate into the cytoplasm through cell membranes [13, 20]. Considering that only treatment with sufficiently large doses of thiamine is effective, achieving its high concentration in the blood and cytoplasm of cells, lipophilic compounds have undoubted advantages over their water-soluble analogues [44].
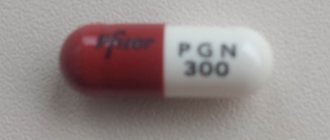
Benfotiamine was synthesized in 1954 in Japan in the laboratories of the Sankyo company, when scientists were looking for an effective treatment for beriberi disease. Many different lipophilic compounds with thiamine-like activity have been created, and the entire group is called "allithiamins." Benfotiamine after oral administration has the greatest bioavailability and safety compared to other allithiamins [19, 21] (
). Benfotiamine also penetrates peripheral nerves better than other allithiamins. Comparative studies of the bioavailability of benfotiamine and water-soluble thiamines have shown that benfotiamine provides the highest concentration of the substance in plasma, red blood cells, cerebrospinal fluid, liver, peripheral nerves and is retained in the body for a longer time [13, 33].
Benfotiamine realizes its effect by influencing various mechanisms of the formation of pathological conditions. In diabetes mellitus (DM), oxidative stress causes disturbances in carbohydrate metabolism with the accumulation of intermediate products that initiate the activity of the main mechanisms leading to pathology of cells of various organs [15, 16, 36]. Benfotiamine increases the activity of transketolase, an enzyme that regulates carbohydrate metabolism, which normalizes the content of intermediate products of glucose metabolism due to the activation of the pentose phosphate shunt [37]. The activity of transketolase is determined by its cofactors thiamine diphosphate or thiamine pyrophosphate, which are formed during the phosphorylation of benfotiamine. Transketolase activity can be significantly increased when large doses of benfotiamine are administered (
). When benfotiamine is administered, the activity of protein kinase C decreases, the transcription of nuclear factor kappa-bi (NF-kB) decreases, and the production of endothelial nitric oxide synthetase and endothelin-1 decreases.
When administering benfotiamine, it is important to reduce the content of methylglyoxal in the cytoplasm of cells, which reacts with free amino groups of proteins, leading to the formation of advanced glycation endproducts (AGEs) [38]. AGEs are responsible for the formation of cellular dysfunction, the development of inflammatory processes and pathology of the vascular wall. Benfotiamine also reduces changes associated with the activation of the polyol pathway for glucose utilization, primarily caused by the depletion of the antioxidant enzyme reduced glutathione and the accumulation of sorbitol [12]. Benfotiamine significantly improves the condition of endothelial cells by normalizing their replication and reducing the activity of apoptosis processes in them [10, 31, 35]. By activating transketolase in erythrocytes and the glomerular apparatus, benfotiamine protects the kidneys from damage due to high glycemia and prevents the development of diabetic nephropathy [7, 29]. In case of thiamine deficiency in patients with alcoholism and chronic renal pathology, benfotiamine normalizes its deficiency and can prevent the development of nephropathies [30].
The purpose of prescribing benfotiamine may be to fill a deficiency that may occur due to dietary restrictions in poor people or vegetarians, due to exposure to various toxic substances (ethanol) or the use of drugs (for example, isoniazid - an anti-tuberculosis drug), after gastrointestinal surgery tract, with intestinal diseases (malabsorption syndrome). A decrease in thiamine levels is observed in almost 30% of alcoholics due to dietary habits, disruption of the mechanisms of thiamine absorption in the intestines as a result of the action of ethanol and its metabolites (acetaldehyde), liver damage with impaired deposition of vitamin B1. It should be especially noted that patients with alcoholism with thiamine deficiency and polyneuropathy note an insufficient effect when treated with water-soluble forms of thiamine. Thiamine deficiency is observed in many patients with diabetic polyneuropathy (DPN) [39]. Malabsorption syndrome leads to a decrease in thiamine content in plasma and cells after surgical interventions on the stomach and intestines, resulting in the development of polyneuropathy [27]. In all situations when the content of thiamine in the plasma and cytoplasm is reduced, the administration of drugs containing benfotiamine leads to a decrease in the clinical manifestations of polyneuropathy and an improvement in the condition of patients.
In Russia, two drugs containing benfotiamine are deservedly popular: 1) the drug Milgamma compositum, which contains 100 mg of benfotiamine and 100 mg of pyridoxine; 2) the drug Benfogamma containing 150 mg of benfotiamine. It is important for clinicians using drugs containing benfotiamine in their practice that there are no reports of any interaction of benfotiamine with other drugs. In addition, there is no indication in the literature of the possibility of toxic effects of large doses of benfotiamine used (up to 600 mg).
Benfotiamine is used to treat late complications of diabetes, which is based on the results of experimental studies and data from controlled clinical trials. In 1996, it was proven that large doses of benfotiamine can inhibit the formation of AGEs in cells in experimental animals and humans [14]. In 2001, the effect of benfotiamine on the formation of AGEs in peripheral nerves in rats with streptozotocin-induced diabetes was revealed and it was shown that benfotiamine reduces the content of methylglyoxal [35]. Benfotiamine reduces hypoperfusion and improves tissue oxygenation, restores endothelium-dependent vasodilation and inhibits apoptosis [11]. In a study of patients with type 2 diabetes, it was found that taking benfotiamine prevents the development of endothelial dysfunction in blood vessels and oxidative stress after eating fried foods containing large amounts of AGEs. In 2003, an experiment demonstrated the ability of benfotiamine to activate transketolase and reduce the content of intermediate products of glucose metabolism, transferring them to the pentose-erythrose shunt [22]. Despite the fact that there was no significant decrease in transketolase activity in diabetes compared to the norm, the administration of thiamine led to the activation of this enzyme by 2.5 times (). Currently, benfotiamine is the main pathogenetic drug for the treatment of late complications of diabetes.
The effectiveness of the drug Milgamma compositum was studied in patients with DPN who received it one tablet 3 times a day for 6 weeks. After the course of treatment, the severity of all tested positive neuropathic symptoms (pain, numbness, paresthesia, chilliness) significantly decreased, vibration sensitivity and autonomic innervation improved (decreased tachycardia, increased heart rate variability, decreased latency and increased amplitude of the evoked cutaneous sympathetic response) [3]. The effectiveness of the combination of benfotiamine (100 mg) and pyridoxine (100 mg) was studied in patients with DPN who received Milgamma compositum, one tablet 3 times a day for 6 weeks. After treatment, the severity of all tested positive neuropathic symptoms (pain, numbness, paresthesia, chilliness) significantly decreased, vibration sensitivity and autonomic innervation improved (decreased tachycardia, increased heart rate variability, decreased latency and increased amplitude of the evoked cutaneous sympathetic response). A significant improvement in the function of somatic and autonomic nerves was noted starting from the 3rd week of treatment [2, 5]. In the BEDIP (BEnfotiamine in the treatment of DIabetic Polyneuropathy) study, 20 diabetic patients with DPN received benfotiamine 400 mg and 20 patients received placebo for 3 weeks. While taking benfotiamine, the clinical manifestations of polyneuropathy, primarily pain, significantly decreased (
) [23]. The study results show that even short-term therapy with benfotiamine can improve the condition of patients with DPN.
In the double-blind, placebo-controlled BENDIP (BENfotiamine in DIabetic Polyneuropathy) study, one group of patients with DPN received 300 mg of benfotiamine per day (55 patients), another group received 600 mg of benfotiamine (57 patients), and a third group received placebo (53 patients) [34]. ]. Positive neuropathic symptoms (patient complaints of pain, burning, numbness, tingling sensation with needles and crawling “pins and needles”) decreased to almost the same extent when using doses of 300 and 600 mg of benfotiamine. A significant decrease in the neurological symptoms of polyneuropathy (muscle strength, reflexes, sensitivity) at week 6 compared to the background level was observed in the group of patients receiving 300 and 600 mg of benfotiamine, significantly different from the placebo group, but the dose of 600 mg was more effective (
) (p < 0.033). Of interest from the point of view of choosing the daily dose of the drug is a study in which a large group of patients with type 1 and type 2 diabetes (1154 patients) received various doses of benfotiamine. The effectiveness of a dose of benfotiamine 300 mg/day was significantly higher than that of a dose of 150 mg/day in terms of its effect on neurological deficit.
A certain benchmark in the possibility of using benfotiamine for prophylactic purposes to prevent the development of late complications of diabetes is provided by a pilot study of 9 patients with type 1 diabetes who did not have any late complications of diabetes, who simultaneously received benfotiamine (300 mg 2 times a day) for 28 days. and alpha-lipoic acid (600 mg 2 times a day) [18]. During treatment, an increase in the activity of the transketolase enzyme by 2–3 times was noted, which led to a decrease in the content of intracellular AGEs and a decrease in the hexoseamine pathway of glucose utilization. In addition, the study emphasized the advisability of simultaneous use of drugs in patients with diabetes alpha-lipoic acid and benfotiamine, each of which acts on different mechanisms of impaired metabolism in DPN.
In diabetes, the development of pathology in the microcirculation system is the determining cause of the development of retinopathy and decreased vision, up to complete blindness. Diabetic retinopathy is associated with increased levels of AGEs in the retina and activation of protein kinase C, both indicators of the formation of oxidative stress. As a result, blindness occurs 25 times more often in patients with diabetes than in the general population. In the experimental works of E. Beltramo et al. [8, 9] showed that changes in retinal cells result from glycation of proteins in extracellular deposits and can be reduced by using benfotiamine. The same group of researchers found that the use of benfotiamine reduces the severity of apoptosis in retinal cells and reduces the content of AGEs in them [10, 28]. In an experimental study by H. P. Hames et al. It has been shown that benfotiamine blocks the main mechanisms of formation of cellular pathology during hyperglycemia and prevents the development of retinopathy [22]. Recent studies on human retinal pericyte cultures have shown that benfotiamine can reduce the severity of apoptosis in retinal cells, which is enhanced by hyperglycemia [9]. The results of these studies show that benfotiamine (drugs "Milgamma compositum" or "Benfogamma") can be used to prevent or delay the onset and progression of microcirculatory disorders of the retina in patients with diabetes.
Low levels of thiamine in plasma in patients with diabetes lead to a decrease in transketolase activity and the activity of the pentose phosphate pathway for utilization of intermediate products of glucose metabolism, which is the basis for the development of cellular pathology in diabetes. A decrease in plasma thiamine content was found in experimental studies on rats with streptozotocin-induced diabetes and in clinical studies (Essex UK Study) in patients with type 1 and type 2 diabetes, which is associated with high renal clearance of thiamine [6, 7]. It is believed that under conditions of hyperglycemia, activation of the hexosamine glycolytic pathway leads to disruption of the function of transporters that ensure the reuptake of thiamine in the proximal renal tubules [27]. Studies conducted in patients with type 1 diabetes showed a decrease in plasma thiamine levels in 86% of patients (p < 0.001 compared with healthy people), and urinary thiamine excretion was significantly higher (p < 0.004) in patients with microalbuminuria compared with patients who did not have microalbuminuria [7]. The authors concluded that impaired maintenance of thiamine levels by the kidneys may be a risk factor for the early development of kidney pathology in diabetes. The possibility of treating disorders of thiamine excretion by the kidneys by taking benfotiamine in the form of drugs (Milgamma compositum and Benfogamma) has clear prospects.
Measuring the level of transketolase concentration in erythrocytes has proven that deficiency occurs in patients with chronic renal failure, which causes the development of polyneuropathy in this group of patients [24]. It has been shown that the administration of benfotiamine to patients even with end-stage renal failure leads to an increase in the concentration of thiamine diphosphate and transketolase activity in erythrocytes [25]. Thus, benfotiamine may be effective in thiamine-deficient patients with chronic renal failure.
Thiamine deficiency plays a major role in the development of alcoholic polyneuropathy (ALP), which in Russia is one of the most common forms of generalized damage to peripheral nerves. Alcohol-induced peripheral nerve damage occurs in 10% of alcoholics, mainly aged 40–70 years, and can be detected in both men and women. LSA begins in the distal lower extremities and then, as the process progresses, may involve the proximal legs and distal arms [26, 45]. In most cases, alcoholic polyneuropathy develops slowly, although there are cases of acute development of polyneuropathy in patients with alcoholism [4], which can also be observed in non-alcoholic thiamine deficiency [24].
The reason for the formation of ALP may be the direct toxic effect of ethanol and its metabolites (acetaldehyde) and the lack of thiamine intake in the body, including those associated not only with poor nutrition of patients with alcoholism, but also with the presence of malabsorption syndrome. Patients with alcoholism have an increased risk of insufficient supply of all B vitamins. When examining 18 patients with alcoholism and polyneuropathy who did not have thiamine deficiency, it was revealed that in this case, predominantly damage to small fibers develops, which differs in clinical, neurophysiological and pathomorphological characteristics from neuropathy in the disease beriberi [25]. ALP without thiamine deficiency is characterized by slow onset, predominantly sensory symptoms, severe pain and burning legs, and axonal degeneration of small fibers is found in the sural nerve. In the presence of thiamine deficiency, the disease often begins acutely with muscle weakness and impairment of deep sensitivity, and in the sural nerve, during biopsy, changes and death of thick nerve fibers are primarily detected. In all cases of ALP, the axonal nature of nerve damage is revealed.
In the controlled study BAP 1 STUDY (Benfotiamine in Treatment of Alcoholic Polyneuropathy), benfotiamine was used for treatment of ALP for 8 weeks in one group of patients (30 patients) at a dose of 320 mg/day, in the second group (26 patients) - a combination of benfotiamine, pyridoxine and cyanocobalamin, and in the third group (28 patients) - placebo [42]. Benfotiamine improved vibration sensitivity, muscle strength, and neuropathic impairment scores in groups receiving benfotiamine alone or in combination with other B vitamins.
Benfotiamine significantly reduced the intensity of pain syndrome in ALP. Fourteen men with ALP treated with oral benfotiamine at a dose of 450 mg/day for 2 weeks and then at a dose of 300 mg/day for an additional 4 weeks [1] and reported improvement in pain, sensory and motor deficits, and improvement in electromyography. It is possible that the decrease in pain intensity during treatment with ALP is due not only to the replenishment of thiamine deficiency, but also to the direct antinociceptive effect of the drug.
From the point of view of the prospects for the use of the drugs Milgamma compositum and Benfotiamine, the results of an experimental study in which mice with diabetes were administered large doses of benfotiamine were interesting and showed a decrease in oxidative stress in the cerebral cortex and myocardium of the left ventricle, and myocardial contractility improved [43,17]. The effect of benfotiamine on the state of the structures of the central nervous system is especially important, since it is known that vitamin B1 deficiency plays an important role in the formation of cerebral disorders in alcoholism [40]. At the same time, there is evidence that some other allithiamins penetrate better into the cytoplasm of brain neurons [41].
The use of Milgamma compositum and Benfogamma for ALP, malabsorption syndrome, and chronic renal failure is justified due to the decrease in the level of thiamine in plasma and cells in these conditions. The use of the drugs Milgamma compositum and Benfogamma, containing large doses of benfotiamine, in diabetes is justified by the drug’s effect on the pathogenetic mechanisms of the formation of late complications. Numerous studies within the framework of evidence-based medicine have shown the clinical effectiveness of Milgamma compositum and Benfogamma in diabetic polyneuropathy, retinopathy and nephropathy. ЃЎ
Literature
- Anisimova E. I., Danilov A. B. Efficacy of benfotiamine in the treatment of alcoholic polyneuropathy // Journal of Neurol and Psychiatry named after. S. S. Korsakova. 2001. ‡‚ 4, p. 216–221.
- Vertkin A.L., Gorodetsky V.V. Advantages of benfotiamine-containing drugs in the treatment of diabetic polyneuropathy // Pharmateka, 2005, ‡‚ 10, p. 1–6.3.
- Sadekov R. A., Danilov A. B., Vein A. M. Treatment of diabetic polyneuropathy with Milgamma 100 // Journal of Neurology and Psychiatry, 1998, ‡‚ 9, p. 30–32.
- Strokov I.A., Alekseev V.V., Aizenberg I.V., Volodina A.V. Acute alcoholic polyneuropathy // Neurological journal. 2004, vol. 9, ‡‚ 1, p. 45–50.5.
- Markina O. A. The importance of the dosage form and route of administration of B vitamins to ensure effective treatment of diabetic polyneuropathy // Clinical pharmacology and therapy, 2003, ‡‚ 2, p. 6–9.
- Antonysunil A., Perkins B., Krolewski A. et al. Thiamine status and risk of early renal function decline in type 1 diabetic patients // Diabetologia. 2008. Vol. 51. S98.7.
- Babaei-Jadid R., Karachalias N., Ahmedm N. et al. Prevention of incipient diabetic nephropathy by high-dose thiamine and benfotiamine // Diabetes, 2003. Vol. 52. P. 2110–2120.
- Beltramo E., Pomero F., Allione A. et al. Pericyte adhesion is impaired on extracellular matrix produced by endothelial cells in high hexose concentrations // Diabetologia. 2002. Vol. 45. P. 416–419.
- Beltramo E., Buttiglieri S., Pomero F. et al. A study of cappollary pericyte viability on extracellular matrix produced by endothelial cells in high glucose // Diabetologia. 2003. Vol. 46. P. 409–415.
- Beltramo E.,Berrone E.,Buttiglieri S.et al.Thiamine and benfotiamine prevent increased apoptosis in endothelial cells and pericytes cultured in high glucose//Diabetes Metab Res Rev.2004.Vol.20.P.330–336.
- Beltramo E., Berrone E., Tarallo S. et al. Thiamine and benfotiamine normalize apoptosis of human retinal pericytes on high glucose extracellular matrix // Diabetologia. 2008. Vol. 51, Suppl. 1. S97 (abstr).
- Berrone E., Beltramo E., Solimine C. et al. Regulation of intracellular glucose and polyol pathway by thiamine and benfotiamine in vascular cells cultured in high glucose // J Biol Chem, 2006. Vol. 281. P. 9307–9313.
- Bitsch R. Biovailability assessment of the lipophilic benfotiamine as compared to a water-soluble thiamin derivative // Ann Nutr Metab, 1991. Vol. 35. P. 292–296.
- Booth AA, Khalifah RG, Hudson BG Thiamine pyrophosphate and pyridoxamine inhibit the formation of antigenic advanced glycation end-products: comparison with aminoguanidine // Biochem Biophys Res Comm, 1996. Vol. 220. P. 113–119.
- Brownlee M. Biochemistry and molecular cell biology of diabetic complications // Nature, 2001. Vol. 414. P. 813–820.
- Brownlee M. The pathobiology of diabetic complications. A unifying mechanism // Diabetes. 2005. Vol. 54. P. 1615–1625.
- Ceylan-Isik AF, Wu S, Li Q. et al. High-dose benfotiamine rescues cardiomyocyte contractile dysfunction in streptozotocin-induced diabetes mellitus // J. Appl Phisiol. 2006. Vol. 100. P. 150–156.
- Du X., Edelstein D., Brownlee M. Oral benfotiamine plus alfa-lipoic acid normalises complication-causing pathways in type 1 diabetes // Diabetilogia. 2008. Vol. 51. P. 1930–1932.
- Fujiwara M. Allithiamine and its properties // J Nutr Sci Vitaminol (Tokyo)? 1967. Vol. 22. P. 57–62.
- Gadau S., Emanueli C., Van Linthous S. et al. Benfotiamine accelerates the healing of ischemic diabetic limbs in mice through protein kinase B/Akt-mediated potentiation of angiogenesis and inhibition of apoptosis // Diabetologia, 2006. Vol. 49. P. 405–420.
- 21. Greb A., Bitsch R. Comparative bioavailability of various thiamine derivatives after oral administration // Int J Clin Pharmacol Ther, 1998. Vol. 36. P. 216–221.
- 22. Hammes HP, Du X, Edelstein D et al. Benfotiamine blocks three major pathways of hyperglycemic damage and prevents expirimental diabetic retinopathy // Nature Med, 2003. Vol. 9 P. 1–6.
- Haupt E., Ledermann H., Kopcke W. Benfotiamine in the treatment of diabetic polyneuropathy. a three-week randomized, controlled pilot study (BEDIP study)//Int J Clin Pharmacol Ther, 2005. Vol. 43. P. 71–77.
- Koike H., Ito S., Morozumi S. et al. Rapidly developing weakness mimicking Guillain-Barre syndrome in berybery neuropathy: two case reports // Nutrition. 2008. Vol. 24 (7–8). P. 776–780.
- Koike H., Iijima M., Suqiura M. et al. Alcoholic neuropathy in clinicopathologically distinct from thiamine-deficiency neuropathy // Ann Neurol. 2003. Vol. 55. P. 19–29.
- Koike H., Mori K., Misu K. et al. Painful alcoholic polyneuropathy with predominant small-fiber loss and normal thiamine status // Neurology. 2001. Vol. 56. P. 1727–1732.
- Koike H., Misu K., Hattori N. et al. Postgastrectomy polyneuropathy with thiamine deficiency // J. Neurol. Neurosurg Psychiatry. 2001. Vol. 71. P. 357–362.
- La Selva M., Beltramo E., Pagnozzi F. et al. Thiamine corrects delayed replication and decreased production of lactate and advanced glycation endproducts in bovine retinal and umbilical vein endothelial cells cultured under high-glucose conditions // Diabetologia. 1996. Vol. 39. P. 1263–1268.
- Larkin JR, Thornalley PJ High glucose causes a decrease in expression of thiamine transporters in human proximal tubule epithelial cells in vitro // Diabetologia. 2008. Vol. 51.S97.
- Mestyan I., Jobst K., Hazafi K. et al. Erythrocyte transketolase activity in patients with chronic renal disease // Acta Med Hung. 1986. Vol. 43. P. 315–319.
- Pomero F., Molinar Min A., La Selva M. et al. Benfotiamine is similar to thiamine in correcting endothelial cell defects induced by high glucose // Acta Diabetol. 2001. Vol. 38. P. 135–138.
- Schmidt J. Wirksamkeit von benfotiamin bei diabetischer neuropathie. breite anwendungsbeobachtung unterstreicht praxisbenefit // Der KaSSENARZT, Helt, 2002, 14/15, P. 40–43.
- Schreeb KH, Freudenthaler S, Vormfelde SV et al. Comparative bioavailability of two vitamin B1 preparations: benfotiamine and thiamine mononitrate // Eur J Clin Pharmacol, 1997, Vol. 52, pp. 773–788.
- Stracke H., Gaus W., Achenbach U. et al. Benfotiamine in diabetic polyneuropathy (BENDIP): results of a randomized, double blind, placebo-controlled clinical trial // Exp Clin Endocrinil Diabetes. 2008. Vol. 116. P. 1–6.
- Stracke H., Hammes HP, Werkmann K. et al. Efficacy of benfotiamine versus thiamine on function and glycation products of peripheral nerves in diabetic rats // Exp Clin Diabetes, 2001. Vol. 109. P. 330–336.
- Thornalley PJ Glioxalase 1. Structure, function, and a critical role in the enzymatic defense against glycation // Biochem Soc Trans. 2003. Vol. 31. P. 1343–1348.
- Thornalley PJ The potential role of thiamine (vitamin B1) in diabetic complications // Curr Diabetes Rev. 2005. Vol. 1. P. 287–298.
- Thornalley PJ, Jahan I., Ng R. Suppression of the accumulation of triosephosphates and increased formation of methylglyoxal in human red blood cells during hyperglycaemia by thiamine in vitro // J. Biochem. 2001. Vol. 129. P. 543–549.
- Thornalley PJ, Babaei-Jadidi R., Al Ali H. et al. High prevalence of low plasma thiamine concentration in diabetes linked to a marker of vascular disease // Diabetologia. 2007. Vol. 50. P. 2164–2170.
- Thomson AD Mechanisms of vitamin deficiency in chronic alcohol misusers and the development of the Wernicke-Korsakoff syndrome // Alcohol/Alcohol Suppl. 2000. Vol. 35. P. 2–7.
- Volvert M.L., Seven S., Piette M. et al. Benfotiamine, a synthetic S-acyl thiamine derivative, has different mechamisms of action and a different pharmacological profile then lipid-soluble thiamine disulfide derivatives // BMC Parmacol, 2008. Vol. 8. P. 10.
- Woelk H., Lehrl S., Bitsch R. et al. Benfotiamine in treatment of alcoholic polyneuropathy: an 8-week randomized controlled study (BAP 1 Study) // Alcohol Alcohol. 1998. Vol. 33. P. 631–638.
- Wu S., Ren J. Benfotiamine alleviates diabetes-induced cerebral oxidative damage independent of advanced glycation end-product, tissue factor and TNF-alpha // Neurosci Lett. 2006. Vol. 394. P. 158–162.
- Ziems M., Netzel M., Bitsch I. Biokinetic parameters and metabolism of S-benzoylthiamine-O-monophosphate // BioFactors. 2000. Vol. 11. P. 109–110.
- Zambelis T., Karandreas N., Tzavellas E. et al. Large and small fiber neuropathy in chronic alcohol-dependent subject // J Periph Nerv Sys. 2005. Vol. 10. P. 375–38.
Key words: benfotiamine, endothelial dysfunction, oxidative stress, diabetic retinopathy, chronic renal failure, alcoholic polyneuropathy, pain syndrome.
I. A. Strokov *, Candidate of Medical Sciences, Associate Professor K. I. Strokov ** Zh. S. Albekova * *MMA named after. I. M. Sechenova , ** RMAPO , Moscow
Properties and benefits of benfotiamine
Preparations containing this vitamin-like compound help accelerate carbohydrate metabolism, while improving the functioning of the nervous system. Their benefit lies in performing the following functions:
- improving memory and attention;
- reducing the rate of development of dementia;
- prevention of depression;
- prevention of damage to the walls of blood vessels;
- maintaining healthy intestinal motility.
Speaking about what benfotiamine is needed for, it is worth paying attention to its participation in the process of producing myelin, which forms the sheaths of peripheral nerves. This prevents the formation of motor and sensory disorders. The benefits of benfotiamine are also reflected in the fact that it prevents the spread of inflammatory processes and provides an analgesic effect.
Diabetic retinopathy
Diabetic retinopathy is a leading cause of blindness and its incidence is increasing worldwide. Early and selective loss of pericytes and thickening of the retinal capillary basement membrane are key determinants of clinical prognosis. Administration of large doses of benfotiamine to rats with streptozotocin-induced diabetes prevented the accumulation of AGEs and thus prevented the development of retinopathy [16]. In addition, benfotiamine prevented the increase in PCC and hexosamine levels, and also reduced aldose reductase-induced mRNA expression and increased cellular glucose concentrations. In addition to these effects, benfotiamine prevented diabetic retinopathy in experimental animals by normalizing pericyte apoptosis and normalizing extracellular matrix turnover [17].
In addition to the described AGE-dependent action of benfotiamine, there appears to be an AGE-independent pathway of its action, which consists in restoring glutathione and reducing oxidative stress [18], as shown in an experiment on normalizing endothelial function in rats without diabetes.
Recommendations for use
According to the instructions for use, benfotiamine is prescribed for Alzheimer's disease and diabetes mellitus. It is recommended to use it if dysfunctions of the nervous system and heart muscle are detected, as well as in case of diagnosis of liver cirrhosis, viral hepatitis or dermatosis. The instructions for benfotiamine state that its use is indicated for alcoholic neuropathy, atherosclerosis and acute or chronic intoxication. The drug is also necessary for people with circulatory problems.
Diabetic neuropathy
Benfotiamine prevents the development of diabetic neuropathy, which has been confirmed in a number of studies [5]. There is a dose-dependent effect of the drug, most significant when using high doses (600 mg/day) of benfotiamine [6]. The combination of benfotiamine and pyridoxine (vitamin B6), as well as cyanocobalamin (vitamin B12), prevents the progression of neuropathy, as evidenced by improvements in symptoms, sensory function, vibration threshold and nerve conduction velocity. In patients with diabetes with thiamine deficiency after bariatric surgery, as well as with alcoholic neuropathy, the administration of benfotiamine leads to rapid relief of symptoms of thiamine deficiency. Currently, from the standpoint of effectiveness and safety, benfotiamine is considered as the first choice drug for preventing the progression of neuropathy [7].
The neuroprotective effect of benfotiamine has been demonstrated in four blind clinical randomized studies (see table).
Note. BT – benfotiamine; NSS – scale of neuropathic sensations (according to Katznewald); VHF – vibration sensitivity threshold; SPN – nerve conduction velocity.
Two recent placebo-controlled studies in patients with diabetic polyneuropathy demonstrated a combined benefit on both the symptoms of neuropathy and its clinical manifestations. In the BEDIP study (BEnfotiamine in the treatment of DIabetic Polyneuropathy), oral administration of benfotiamine at a dose of 400 mg/day in patients with type 1 and type 2 diabetes with signs of peripheral symptomatic neuropathy for 3 weeks led to a statistically significant positive change in the neuropathic sensation scale, especially pain. component (“shooting” pain, burning in the feet), compared with placebo [8]. There was a higher rating given by doctors and patients when comparing groups. There were no statistically significant improvements in vibration threshold scores, which is most likely due to the timing of the study. However, clinical improvement is perhaps the most important outcome of the study. Another 6-week study, BENDIP (BENnfotiamine in DIabetic Polyneuropathy), showed a positive effect of benfotiamine 600 mg on neuropathic symptoms [6]. In both studies, the effect of the drug was independent of glycohemoglobin levels and glycemic levels. The main advantage of benfotiamine shown in the study is the absence of side effects.
Endothelial dysfunction
Endothelial dysfunction is the most significant pathophysiological link in the generalized process of vascular damage in diabetes. Firstly, the endothelium is a structure that regulates vascular tone. Secondly, endothelial dysfunction leads to a decrease in the ability of blood vessels to dilate, a prothrombotic and pro-inflammatory state of the vascular wall. Endothelial dysfunction can be caused by a decrease in the formation of nitric oxide in the endothelium, as well as oxidative stress [19]. Additional exposure to factors such as smoking, alcohol intake, and oxidative stress caused by eating foods with elevated AGE levels increases endothelial vascular dysfunction.
Benfotiamine prevents micro- and macrovascular dysfunction, as shown in several clinical studies. Prevention of microvascular endothelial dysfunction with the use of megadoses of benfotiamine (1050 mg for 3 days) was shown in an experiment involving volunteers and is expressed in the normalization of the prandial microvascular response in a test with reactive hyperemia [20]. A study conducted in patients with type 2 diabetes demonstrated a decrease in vasoconstriction after eating a meal rich in advanced glycation end products (subjected to high and prolonged heat treatment), which may indicate better function of the capillary endothelium under conditions of aggressive exposure to foods that contribute to the “aging” of blood vessels [ 21].
Benfotiamine has protective anti-inflammatory effects, reducing not only the glucotoxic, but also the lipotoxic effect; in an experiment on animals with diabetes, it prevents apoptosis induced by lipopolysaccharides, which is carried out through a decrease in the expression of caspase-3 protein and nuclear factor PARP. As a result, the possibility of using benfotiamine in the treatment of chronic inflammation was shown [22].
Diabetes mellitus is a risk factor for heart failure independent of coronary atherosclerosis and arterial hypertension. As a result of the production of factors induced by hyperglycemia, changes in the structure and function of cardiomyocytes occur, provoking the development of diabetic cardiomyopathy.
Diabetic cardiomyopathy
Diabetic cardiomyopathy is characterized by sudden onset, initially manifesting as reversible isolated diastolic dysfunction, which progresses over time to global heart failure, accompanied by myocardial remodeling and dilatation of the cardiac chambers.
In an experimental animal study, benfotiamine administration improved systolic and diastolic function and prevented increases in end-diastolic pressure as well as cardiac chamber dilatation [23]. In addition, benfotiamine improved cardiac perfusion, reduced cardiomyocyte apoptosis, and prevented the development of interstitial fibrosis. It has been demonstrated that this effect is due to the effect on the expression of the Akt/Pim-1 factor, activation of the pentose phosphate pathway, suppression of oxidative stress, and prevention of AGE accumulation in myocardiocytes.
Thus, the use of drugs containing benfotiamine (Milgamma compositum) has a multidisciplinary effect in the treatment of people suffering from diabetes. The therapeutic prospects of benfotiamine open up new possibilities for the pathogenetic treatment of vascular complications of diabetes.