The category of drugs-stabilizers of mast cell membranes includes drugs with local action - cromones, as well as systemic drugs with an auxiliary antihistamine property, namely ketotifen.
The mechanism of action of these medications is that they are able to block the entry of calcium and chlorine ions into cells, as a result of which the allergy mediator (histamine) is stabilized and the membrane loses the ability to leave this cell. In addition, membrane stabilizers can prevent the release of other substances that are involved in the development of allergic phenomena.
What it is?
Mast cell membrane stabilizers are drugs that prevent calcium channels from opening and calcium entering mast cells. They block calcium-dependent cell degranulation and the release of histamine from them, a factor that activates platelets and leukotrienes. They also reduce the manifestations of anaphylaxis and other biologically active substances that can induce inflammatory and allergic reactions. Stabilization of mast cell membranes is caused by blockade of cAMP accumulation in them and inhibition of phosphodiesterase.
The main aspect of the antiallergic effect of drugs that stabilize mast cell membranes is the increased perception of catecholamines by adrenergic receptors. In addition, such drugs have the property of blocking chloride channels and thus preventing depolarization of parasympathetic endings in the bronchi. They prevent cellular infiltration of the bronchial mucosa and inhibit delayed hypersensitivity reactions. Some of the drugs in this group have the ability to inhibit H1 receptors.
Medicines eliminate swelling of the bronchial mucosa and prevent an increase in smooth muscle tone. The main indication for their use is the prevention of bronchial obstruction.
Effects
The effects of mast cell membrane stabilizer drugs are:
- reducing the excessive reactivity of the mucous membranes (by inhibiting the release of mediators of allergic cell reactions);
- decreased activity of cells that are involved in the development of allergic reactions (eosinophils, macrophages, neutrophils and others);
- decreased degree of permeability of mucous membranes - due to decreased swelling;
- a decrease in the sensitivity of nerve receptors and subsequent blocking of the reflex narrowing of the lumens of the bronchi - bronchoconstriction.
What is the mechanism of action of mast cell membrane stabilizers?
Types of eye drops for allergies
Vasoconstrictor drops
These antiallergic drugs for instillation constrict blood vessels, thereby reducing redness and swelling of the mucous membrane. With prolonged use, they are addictive, and their subsequent withdrawal can create a “withdrawal effect” - a rapid return of all manifestations of the disease.
This group of drugs includes Visin. "Okumetil", "Octilia".
Antihistamine eye drops
Drugs in this group prevent the accumulation of histamine, which is one of the main factors in the development of allergic reactions. Antihistamine eye drops are effective against symptoms such as itching and swelling. As a rule, they are prescribed as the first remedy for the treatment of allergic eye diseases. This group of drugs includes Allergodil, Lecrolin, Spersallerg, Opatanol.
Anti-inflammatory eye drops for allergies
Anti-inflammatory drugs for instillation are divided into two groups:
Corticosteroid drugs. Eye drops containing corticosteroids are sometimes used to relieve acute allergic symptoms, but they are usually prescribed only for a short period of time due to the fact that they cause side effects with long-term use. This group of drugs includes Prenacid, Dexamethasone, and Maxidex.
Non-steroidal anti-inflammatory drugs (NSAIDs). Eye drops containing non-steroidal anti-inflammatory drugs are prescribed to reduce inflammation, swelling and other manifestations of allergic reactions. Among the drugs in this group: Indocollir, Diclofenac, Naklof, Diklo F.
Mast cell stabilizers
Medicines in this group block the release of histamine and other substances that cause allergy symptoms from mast cells, highly specialized immune cells that play a major role in the development of an allergic reaction.
A feature of drugs belonging to this group is the accumulation effect - they do not act immediately after administration. Therefore, in order to reduce the symptoms, it is recommended to start taking these antiallergic medications in advance, before the start of the allergy season.
This group of drugs includes Kromhexal, Lecrolin, Alomide.
Tear substitutes
Tear substitutes have a moisturizing effect on the eyes, coping with allergy symptoms such as dryness, redness and irritation of the mucous membrane. To provide an additional soothing effect, these eye drops are recommended to be stored in the refrigerator.
Tear substitutes are completely safe, so they can be used without restrictions as needed.
This group of drugs includes “Artificial tear”, “Vidisik”, “Natural tear”, “Systane”.
Pharmacological properties
The use of drugs of this pharmacological group prevents the development of allergic phenomena (bronchospasms, swelling) when potential allergens penetrate the body, as well as when it is influenced by various provoking factors - physical activity, cold air and others.
Ketotifen is a stabilizer for mast cell membranes. It, like cromones, reduces the increased activity of the respiratory tract in the form of a response to an allergen entering the body. In addition, it is a blocker of H1-histamine fibers, that is, it inhibits the progression of allergic processes.
This is the main mechanism of mast cell membrane stabilizers.
In general, membrane stabilizers, when used regularly over a long period of time, reduce the frequency of exacerbations of allergic diseases that occur in a chronic form.
Cromones are used for the prevention of allergic rhinitis and conjunctivitis, bronchial asthma and the development of bronchospasms caused by the influence of provoking factors (physical exercise, cold air and others), as well as before expected contact with potential allergens. Among other things, drugs of this pharmacological category are used in the complex treatment of bronchial asthma - in the form of one of the basic therapy medications. To eliminate bronchospasm, these medical drugs are not used in this classification.
Mast cell membrane stabilizers include Ketotifen. It is used to prevent the atopic form of bronchial asthma, treat atopic dermatitis, conjunctivitis and rhinitis of an allergic nature, and chronic urticaria. The widespread use of this drug is significantly limited by its relatively low antiallergic and anti-inflammatory activity, as well as pronounced side symptoms of 1st generation antihistamines, which are also characteristic of this drug.
The maximum effectiveness of cromones occurs approximately 14 days after their systematic administration. The duration of such therapy should be 4 months or more. The medication is discontinued gradually over a week.
There is no addiction to its use; there is also no decrease in the effectiveness of other medications when taken for a long time (symptoms of tachyphylaxis). Are there any contraindications for mast cell membrane stabilizers?
Antihistamines in the treatment of chronic urticaria: a literature review
Information on the treatment of urticaria and angioedema (AO) presented in this review is based on the principles of evidence-based medicine, i.e., on the results of randomized and other scientific studies. The letters “A–D” are used to indicate levels of evidence, with A being the highest level (good evidence of effectiveness) and D representing recommendations based on weak evidence.
Antihistamines (H1-histamine receptor blockers, H1-HBs) of the second generation are the first choice drugs for all patients with chronic urticaria (CU) (A) [1–3]. Their administration leads to a reduction in itching, the duration of the rash and an improvement in the quality of life of patients. However, the use of drugs does not always result in the complete disappearance of rashes and itching, since the appearance of symptoms can be caused by the action of other mediators, as well as histamine, not only through H1-, but also through H2-receptors.
The place of antihistamines in the treatment of chronic urticaria and evidence of effectiveness
Second generation antihistamines, such as cetirizine [4], desloratadine [3, 5], ebastine [6], fexofenadine [7, 8], levocetirizine [9], loratadine [2], mizolastine [10] and rupatadine [11], have been well studied in randomized clinical trials (RCTs) for the treatment of CU. Despite the fact that some of these drugs are positioned as “III generation antihistamines,” this term should only be used to designate drugs with new properties [12]. Unfortunately, to date there are no drugs with such properties.
Drug treatment should begin with the standard dose of non-sedating H1-BG recommended in the manufacturer's instructions (A) [1]. For daily or frequent symptoms, the drug is prescribed on a regular basis rather than on demand to prevent rashes and itching. It is necessary to offer patients a choice of at least two systemic antihistamines of the second generation, since the effect and tolerability may differ in each individual patient (A) [13].
Sometimes, to control severe urticaria/angioedema, doses of second-generation H1-BG may be required above the therapeutic doses described in the instructions (B). In this case, in patients with no or poor response to therapy with standard doses of H1-BG, the potential effectiveness of an increased dose of the drug usually outweighs the possible risk [14, 15]. One study showed an increase in the effectiveness of therapy in the majority of patients with CU when taking levocetirizine at a daily dose 4 times higher than the manufacturer's recommended dose [16]. Many experts agree that in all cases, if there is a need for second- and third-line drugs, it is better to increase the dose of non-sedating H1-BG to 2-4 times a day, taking into account possible side effects and the patient’s body weight. In this case, it is necessary to weigh the benefits and risks of using the drug and warn the patient about the increased likelihood of side effects. It is important to emphasize here that from a legal point of view, the doctor does not have the right to deviate from the instructions for the use of a particular drug. To date, in all instructions for second generation antihistamines approved in Russia, there are no recommendations for increasing the dose. Prescribing an increased dose of the drug is possible only “off-label” and must be accompanied by the informed consent of the patient and the conclusion of a consultation with an entry in the primary medical documentation.
Some doctors recommend using two different second-generation antihistamines on the same day (eg, morning and evening) (D) because some patients may benefit from one drug better than the other. However, this recommendation is based only on empirical evidence and results from RCTs are needed to confirm it. According to current evidence (B) [1], increasing the daily dose of the same drug should be preferred to using a combination of different drugs.
The addition of H2-GD to CU therapy may result in greater control of urticaria than H1-GD monotherapy (C) [17, 18]. If there is no effect within 3–4 weeks, N2-BG should be discontinued.
RCTs were conducted to compare the effectiveness of treatment of patients with chronic hyperplasia with antihistamine drugs of the first and second generations. In one study, cetirizine 10 mg once daily for control of itching and rash resulted in a faster onset of action than hydroxyzine 25 mg three times daily, although they had similar efficacy (B) [19]. Comparative studies between different second-generation H1-GDs did not demonstrate pronounced statistically and clinically significant differences (B) [7, 20, 21].
Adding sedative H1-BG at night may help with sleep disturbance associated with severe nocturnal itching. Despite the fact that sedatives need to be taken 3–4 times a day, they can be prescribed for urticaria, for example, in the absence of effect from second generation H1-GD (C) [22]. Some doctors recommend regular use of these drugs, believing that tolerance develops to the sedative effect within 1 week. However, objective testing usually does not confirm tolerance. This is because H1 receptors in the central nervous system (CNS) are no different from H1 receptors in peripheral tissues such as the skin.
The evidence base for the use of H1-BG for the treatment of physical urticaria, including dermographic, cold, pressure, cholinergic, and solar urticaria, is still limited, although some studies have shown some effectiveness (C) [23].
Antihistamines are less effective for the treatment of other forms of urticaria, such as pigmentary and cutaneous mastocytosis, as well as urticarial vasculitis and urticaria associated with cryopyrin-mediated autoinflammatory diseases (C) [24].
On the other hand, H1-BG are highly effective in allergic and AO combined with urticaria and itching. The drugs are ineffective for non-allergic isolated AO, including hereditary types I, II, III and acquired, associated with cancer or the use of angiotensin-converting enzyme inhibitors [25].
International generic and trade names, as well as doses and frequency of use in children and adults are given in table. 1.
Side effects
Fexofenadine, loratadine, desloratadine, cetirizine sometimes have a mild anticholinergic effect. Cetirizine and fexofenadine cause sedation in approximately 10% of cases [26]. This may be due to genetic polymorphism of the MDR1 gene, which encodes the P glycoprotein (a transporter involved in the elimination of many drugs, including antihistamines), which mediates changes in the pharmacokinetics of these drugs in some patients.
Sedative H1-BGs have a pronounced effect on the central nervous system (they can cause drowsiness, lethargy, weakness, decreased concentration, etc.) (Table 2).
H2 receptor antagonists are characterized by a significant number of side effects; Cimetidine should be used with caution due to its interaction with many drugs, as well as due to a possible decrease in potency, headache, arthralgia, myalgia, central nervous system damage and the cardiotoxic effect of the drug.
Duration of therapy
For most patients with CC, 3–6 months of regular therapy (D) is recommended [1, 27], with periodic discontinuation or dose reduction of the drug in the absence of symptoms of the disease. In patients with a long history of urticaria and AO, treatment is possible for 6–12 months with gradual withdrawal of drugs for several weeks. In patients with intermittent, episodic symptoms, therapy may be prescribed “on demand” or prophylactically before important life events.
Cromones and ketotifen
Cromones administered orally are not absorbed from the gastrointestinal tract and are usually ineffective for urticaria. However, some authors have noted the effectiveness of the mast cell membrane stabilizer ketotifen in patients with cold [28], cholinergic [29], dermographic [29] and delayed pressure urticaria [30]. Trial therapy with ketotifen is possible in the absence of effect from antihistamines [31, 32].
Features of antihistamine therapy for urticaria in children, pregnant women and the elderly
All antihistamines can be used in children over 12 years of age. Some recommendations from countries in Europe and the USA indicate the possibility of safely prescribing the following drugs in young children: I generation - hydroxyzine and alimemazine (from 6 years), diphenhydramine, clemastine, promethazine, cyproheptadine and ketotifen (from 2 years); II generation - only cetirizine, loratadine and desloratadine can be used for chronic urticaria in children from 2 years of age, ebastine, fexofenadine and levocetirizine - only from 6 years of age [33]. Cetirizine (after processing the results of the ETAC study) became the first antihistamine approved by the Food and Drugs Administration of the United States (FDA) for use in children from 6 months for the treatment of perennial allergic rhinitis and HC. The safety of long-term use (up to 18 months) of non-sedating second-generation H1-GDs in young children, in contrast to first-generation antihistamines, has been proven in RCTs [34–36].
The decision to prescribe these or other drugs in young children is made individually in each specific case after assessing the benefit/risk ratio.
When choosing drugs for a pregnant patient with urticaria, it is necessary to take into account the risk categories of prescribing drugs to pregnant women in the FDA classification (Tables 3 and 4) [37, 38].
It is necessary to avoid the use of systemic drugs in pregnant patients, especially in the first trimester [39]. However, if necessary, it is necessary to begin (or continue) treatment with antihistamines as the drug of choice in patients with urticaria. I generation H1-BG were previously recommended as the most studied and safe drugs during pregnancy. But at present, sufficient information has been accumulated confirming the safety of second-generation antihistamines, which, together with the absence of sedatives and other side effects compared to their predecessors, gives the right to prefer their use during pregnancy (C) [40]. As needed, the smallest doses of loratadine or desloratadine, as the most studied drugs, should be used, and if they are ineffective, diphenhydramine (C) should be used [27, 39]. The use of astemizole and terfenadine is unacceptable due to its arrhythmogenic effect, as well as the embryotoxic effect detected in animal tests.
The potential benefit to the mother should be weighed against the risk to the fetus when prescribing any drugs during pregnancy; explain to the patient the need to take antihistamines during pregnancy in case of acute or recurrent urticaria, inform about the presence of minimal risk and maintaining the health of the mother in the interests of the fetus.
All antihistamines pass into breast milk. Breastfed children receive approximately 0.1% of the drug dose when administered orally by the mother. First generation H1-GD may cause sedation and other side effects in such children [41, 42]. During lactation, it is possible to use (if necessary) the smallest doses of loratadine or cetirizine (C) [39, 43].
Like all drugs during pregnancy and lactation, N1-BG should be used in the minimum effective dose.
Elderly individuals are predisposed to the development of side effects from the central nervous system when using drugs that penetrate the blood-brain barrier. When prescribed to this group of patients, first generation N1-GD, even at the doses recommended by the manufacturer, there is a high risk of sedation, cognitive dysfunction, impairment of attention, speech and other side effects [41, 42].
In addition, polypharmacy often occurs in elderly patients, so the likelihood of interaction between sedating antihistamines and other drugs increases.
I generation H1-GDs are contraindicated in patients with glaucoma and prostate hypertrophy [41, 42].
Conclusion
Urticaria/AO is a heterogeneous group of diseases characterized by a variety of clinical manifestations and different mechanisms of development. Therefore, it is logical that a stepwise approach should be used to treat it, based on the form of urticaria, severity, pathogenesis and course characteristics. The algorithm for this approach is given in other publications [1, 15], where recommendations for the use of individual drugs are also discussed and evidence of their effectiveness is provided.
It must be remembered that antihistamines are indicated for almost all patients with urticaria, with the exception of some patients with isolated AO, in particular with hereditary ones. In addition, unless specifically indicated, it is advisable to avoid prescribing antihistamines and other systemic drugs in the first trimester of pregnancy, despite the fact that studies have not shown a teratogenic effect. The addition of a leukotriene receptor blocker to antihistamine therapy in adult patients may have an additional effect when exacerbation of urticaria is associated with food pseudoallergens, aspirin, or the presence of functional autoantibodies.
Currently, additional research is required on existing drugs for the treatment of urticaria, especially chronic, and the search for new highly effective drugs. It should be taken into account that, unlike antihistamines, the use of most second- and third-line drugs, in particular cyclosporine and omalizumab, is associated with high costs and/or a significant risk of severe side effects.
Literature
- Zuberbier T. A Summary of the New International EAACI/GA (2)LEN/EDF/WAO Guidelines in Urticaria // World Allergy Organ J. 2012, Jan; 5(Suppl 1):S1–5. doi: 10.1097/WOX.0 b013 e3181 f13432. Epub 2012, Jan 13.
- Monroe EW, Fox RW, Green AW et al. Efficacy and safety of loratadine (10 mg once daily) in the management of idiopathic chronic urticaria // J. Am. Acad. Dermatol. 1988; 19: 138–139.
- Ring J., Hein R., Gauger A. et al. Once-daily desloratadine improves the signs and symptoms of chronic idiopathic urticaria: a randomized, double-blind, placebo-controlled study // Int. J. Dermatol. 2001; 40: 72–76.
- La Rosa M., Leonardi S., Marchese G. et al. Double-blind multicenter study on the efficacy and tolerability of cetirizine compared with oxatomide in chronic idiopathic urticaria in preschool children // Ann. Allergy Asthma Immunol. 2001; 87:48–53.
- Nettis E., Colanardi MC, Paradiso MT, Ferrannini A. Desloratadine in combination with montelukast in the treatment of chronic urticaria: a randomized, double-blind, placebo-controlled study // Clin. Exp. Allergy. 2004; 34:1401–1407.
- Sastre J. Ebastine in allergic rhinitis and chronic idiopathic urticaria // Allergy. 2008; 63(Suppl. 89): 1–20. Review.
- Handa S., Dogra S., Kumar B. Comparative efficacy of cetirizine and fexofenadine in the treatment of chronic idiopathic urticaria // J. Dermatol. Treat. 2004; 15:55–57.
- Finn AF Jr., Kaplan AP, Fretwell R. et al. A double-blind, placebo-controlled trial of fexofenadine HCl in the treatment of chronic idiopathic urticaria // J. Allergy Clin. Immunol. 1999; 104:1071–1078.
- Nettis E., Colanardi MC, Barra L. et al. Levocetirizine in the treatment of chronic idiopathic urticaria: a randomized, double-blind, placebo-controlled study // Br. J. Dermatol. 2006; 154:533–538.
- Aberer W., Kranke B. One-year treatment of chronic urticaria with mizolastine: efficacy and safety // J. Eur. Acad. Dermatol. Venereol. 2001; 15(1):77–79.
- Gimenez-Arnau A., Pujol R.M., Ianosi S. et al. Rupatadine in the treatment of chronic idiopathic urticaria: a double-blind, randomized, placebo-controlled multicentre study // Allergy. 2007; 62:539–546.
- Holgate S., Canonica G., Simons F. et al. Consensus group on new-generation antihistamines (CONGA): present status and recommendations // Clin. Exp. Allergy. 2003; 33:1305–1324.
- Wedi B., Kapp A. Chronic urticaria: assessment of current treatment. Exp. Rev. Clin. Immunol. 2005; 1:459–473.
- Asero R., Tedeschi A., Cugno M. Treatment of chronic urticaria // Immunol Allergy Clin North Am. Feb 2014; 34 (1): 105–116. doi: 10.1016/j.iac.2013.09.013. Epub 2013, Oct 28.
- Maurer M., Magerl M., Metz M., Zuberbier T. Revisions to the international guidelines on the diagnosis and therapy of chronic urticaria // J Dtsch Dermatol Ges. 2013, Aug 19. doi: 10.1111/ddg.12194. .
- Church D.S., Baiardini I., Staevska M. et al. The effectiveness of antihistamines in up to four-times conventional doses on urticarial discomfort and quality of life in difficult-to-treat urticaria. Abstract 1501, Warsaw: XXVIII EAACI Congress, 2009.
- Bleehen SS, Thomas SE, Greaves MW et al. Cimetidine and chlorpheniramine in the treatment of chronic idiopathic urticaria: a multi-centre randomized double-blind study // Br. J. Dermatol. 1987; 117:81–88.
- Paul E., Bofldeker RH Treatment of chronic urticaria with terfenadine and ranitidine: a randomized double-blind study in 45 patients // Eur. J. Clin. Pharmacol. 1986; 31: 277–280.
- Breneman DL Cetirizine versus hydroxyzine and placebo in chronic idiopathic urticaria // Ann. Pharmacother. 1996; 30: 1075–1079.
- Garg G., Thami GP Comparative efficacy of cetirizine and levocetirizine in chronic idiopathic urticaria // J. Dermatol. Treat. 2007; 18:23–24.
- Potter PC, Kapp A, Mauer M et al. Comparison of the efficacy of levocetirizine 5 mg and desloratadine 5 mg in chronic urticaria patients // Allergy. 2009; 64(4):596–604.
- Kaplan AP Clinical practice. Chronic urticaria and angioedema // N. Engl. J. Med. 2002; 346:175–179.
- Zuberbier T., Bindslev-Jensen C., Canonica W. et al. EAACI/GA2LEN/EDF guideline: management of urticaria // Allergy. 2006; 61:321–331.
- Brodell LA, Beck LA Differential diagnosis of chronic urticaria // Ann. Allergy Asthma Immunol. 2008; 100: 181–188.
- Frank MM Hereditary angioedema // J. Allergy Clin. Immunol. 2008; 121:S398–S401.
- Kolkhir P. V., Ignatiev I. V., Sychev D. A., Kukes V. G. Effect of carriage of genotypes for the polymorphic marker C3435 T of the MDR1 gene encoding glycoprotein-P on the pharmacokinetics of the third generation H1-histamine receptor blocker fexofenadine / / Allergol. and immunol. 2006; 3 (3): 279.
- Zuberbier T., Asero R., Bindslev-Jensen C. et al. EAACI/GA2 LEN/EDF/WAO guideline: management of urticaria // Allergy. 2009; 64:1427–1443.
- St-Pierre JP, Kobric M., Rackham A. Effect of ketotifen treatment on cold-induced urticaria // Ann. Allergy. 1985; 55:840–843.
- Cap JP, Schwanitz HJ, Czarnetzki BM Effect of ketotifen in urticaria factitia and urticaria cholinergica in a crossover double-blind trial // Hautarzt. 1985; 36:509–511.
- Vena GA, D'Argento V., Cassano N., Mastrolonardo M. Sequential therapy with nimesulide and ketotifen in delayed pressure urticaria // Acta Derm. Venereol. 1998; 78:304–305.
- Kaplan AP Urticaria and angioedema. In: Allergy: principles and practice, 5th edn. Ed. by E. F. Ellis, E. Middleton et al. St. Louis: Mosby-Year Book, 1998: 1104–1122.
- Katz SI Mechanisms involved in allergic contact dermatitis // J. Allergy Clin. Immunol. 1990; 86:670–672.
- Equipo editorial del Martindale: Antihistaminicos. En Martindale-Guia completa de consulta farmacoterapeutica. Dir. por SC Sweetman. Barcelona: Pharma Editores, 2003: 531–557.
- Simons FER On behalf of the ETAC Study Group. Prospective, long-term safety evaluation of the H1-receptor antagonist cetirizine in very young children with atopic dermatitis // J. Allergy Clin. Immunol. 1999; 104:433–440.
- Simons FER On behalf of the Early Prevention of Asthma in Atopic Children (EPAAC) Study Group. Safety of levocetirizine treatment in young atopic children: an 18-month study // Pediatr. Allergy Immunol. 2007; 18:535–542.
- Grimfeld A., Holgate ST, Canonica GW et al. Preventive management of children at risk for recurrent upper respiratory infections: the Preventia I Study. Clin. Exp. Allergy 2004; 34:1665–1672.
- Yawn V., Knudtson M. Treating Asthma and Comorbid Allergic Rhinitis in Pregnancy: Safety of AR Drug Classes During Pregnancy Antihistamines https://www.medscape.com/viewarticle/558444_13.
- Fassakhov R. S. Treatment of bronchial asthma in pregnant women. Quality of life // Medicine. 2007; 1 (18): 50–55.
- Grattan CE, Humphreys F. British Association of Dermatologists Therapy Guidelines and Audit Subcommittee. Guidelines for evaluation and management of urticaria in adults and children // Br. J. Dermatol. 2007; 157(6):1116–1123.
- Wallace DV, Dykewicz MS et al. The diagnosis and management of rhinitis: An updated practice parameter // J. Allergy Clin. Immunol. Aug 2008: 1–84.
- Simons FER Advances in H1-antihistamines // N. Engl. J. Med. 2004; 351:2203–2217.
- Simons FER, Akdis CA Histamine and antihistamines. In: Middleton's Allergy Principles and Practice, 7th edn. Ed. by N. F. Adkinson Jr., W. W. Busse et al. St. Louis: Mosby Inc. (an affiliate of Elsevier Science), 2008: 1517–1547.
- Powell RJ, Du Toit GL et al. BSACI guidelines for the management of chronic urticaria and angio-oedema // Clin. Exp. Allergy. 2007; 37:631–650.
P. V. Kolkhir1, Candidate of Medical Sciences N. G. Kochergin, Doctor of Medical Sciences, Professor O. A. Kosoukhova
GBOU VPO First Moscow State Medical University named after. I. M. Sechenova Ministry of Health of the Russian Federation, Moscow
1 Contact information
Other uses
Using these drugs in the form of nasal drops containing cromones, patients in some cases note the appearance of symptoms of cough, headache, taste disturbance and irritation of the nasopharyngeal mucosa.
After instillation (dropping into the eyes) of these medications, a burning sensation, a sensation of a foreign body in the eyes, swelling and hyperemia of the conjunctiva (redness) sometimes occur.
"Sodium cromoglycate"
This medication also has some analogues, which include:
- "Cromoglycic acid";
- "Ifiral";
- "Cromoglin";
- "Intal";
- "Cromohexal".
These membrane stabilizers prevent allergic manifestations with immediate action, but do not eliminate them.
When entering the body by inhalation, only 10% of the original dosage is absorbed from the lumens of the respiratory tract of the lungs, when taken orally - even less - only 1%, when used intranasally, 8% penetrates into the blood, and when instilled into the eyes - 0.04% of the drug .
The maximum concentration of the main substances of the substance in the blood is observed after 15-20 minutes. The effect when instilled into the eyes occurs after 2-14 days, when administered inhalation - after 2-4 weeks, when taken orally - after 2-5 weeks.
Indications for the use of this medicine or its analogues are bronchial asthma (as one of the main treatments), allergic diseases of the digestive system, food allergies, ulcerative colitis (as an element of combination treatment), hay fever, allergic rhinitis and conjunctivitis.
For inhalation of this group of medications the following are used:
- "Intal";
- "Cromohexal";
- "Ifiral."
For intranasal use the following are prescribed:
- "Ifiral";
- "CromoHexal";
- "Cromoglin";
- "Kromosol."
As an eye drop:
- "Ifiral";
- "CromoHexal";
- "Cromoglin";
- "Stadaglycine";
- "High Chrome."
What else is on the list of mast cell membrane stabilizer drugs?
Stopping or reducing contact with the allergen are so-called elimination measures.
The basis of any method of successful treatment of allergies is, first of all, the elimination of contact with the allergen.
In most cases, this is enough to completely get rid of allergy symptoms or significantly reduce its manifestations. If the cause is not eliminated, then, unfortunately, even the best anti-allergy medications will only provide a temporary effect. If you know the allergen for sure, try to eliminate it, which will help get rid of the allergy. In some cases, this is easy to do: you can always refuse an exotic fruit or a certain type of cosmetics. Sometimes this is difficult: for example, to completely get rid of dust or not to come into contact with pollen from flowering plants. And in some cases, especially if a person has several irritants at once, it is simply impossible to completely eliminate everything. In this case, it is important to minimize contact with the allergen.
The most common causes of allergies are household allergens and food, which is why during treatment, first of all, attention should be paid to a hypoallergenic lifestyle and a special diet.
The most common household allergen is house dust. This is a whole complex of allergens, which includes the epidermis of humans and animals, microscopic spores of mold and yeast, insect waste products, etc.
What helps against household allergies and creating a hypoallergenic lifestyle is written in detail here. Adhering to a hypoallergenic lifestyle is important not only for those who are allergic to dust, but also for all people suffering from any allergies, as well as those with a hereditary predisposition to allergic diseases.
A hypoallergenic diet is one of the allergy treatment methods that plays a special role in the treatment of allergic diseases, especially if there is a food allergy without clear indications of any type of product. In this case, it is recommended to exclude all highly allergenic foods from the diet: chocolate, strawberries, strawberries, citrus fruits, tomatoes, red apples, fish, chicken, eggs, etc. It is also necessary to avoid foods with dyes and preservatives, hot and spicy dishes, alcohol and carbonated drinks, and limit salt intake. The nonspecific hypoallergenic diet is described in detail here. Adhering to such a diet is recommended for all allergy sufferers and persons predisposed to allergic reactions.
If you are allergic to pollen, then a special diet is prepared that takes into account the risk of cross-reactions with pollen allergens. The dusting/blooming calendar and cross-allergy table can be found at the links above.
"Nedocromil sodium"
This medication, as a stimulator of mast cell membranes, is similar in effect to sodium cromoglycate. It has a bronchodilator and anti-inflammatory effect and is used by inhalation for the prevention and treatment of pathologies such as bronchial asthma. In this case, 4-8 times a day, 4 mg for 2 breaths is used. The maintenance dosage is equal to the therapeutic one, however, the frequency of inhalations is 2 times a day. By the end of the first week of treatment, a therapeutic effect can already be observed.
Side effects may occur: cephalalgia, cough, dyspepsia, bronchospasm. Mutually enhances the effects of β-adrenergic stimulants, glucocorticoids, ipratropium and theophylline bromide.
List of allergy eye drops
| Drug name | Age | Price in pharmacies (RUB) | |
| Allergodil | from 4 years old | 300 | |
| Alomid | from 2 years | 200 | |
| Visin Allergy | from 12 years old | 240 | |
| Dinaf | from 2 years | 80 | |
| Zaditen | from 12 years old | 340 | |
| Krom-Allerg | from 4 years old | 90 | |
| Cromohexal | from 4 years old | 120 | |
| Cromogolin | from 4 years old | 50 | |
| Lecrolin | from 4 years old | 140 | |
| Nozeilin | from 6 years old | 140 | |
| Opatanol | from 3 years old | 380 | |
| Sanorin-Anolergin | from 2 years | 260 | |
| Spersallerg | from 2 years | no data | |
"Lodoxamide"
This pharmacological drug inhibits the release of histamines and other substances that contribute to allergic reactions. It is available as eye drops. Absorbed in small amounts, the half-life is about 8 hours. This remedy is used for allergic conjunctivitis and keratitis.
It is recommended to instill one or two drops into each eye at intervals of 6 hours. Duration of treatment is up to 1 month.
During therapy with this medicine, it is possible to develop side symptoms from the organs of vision (irritation of the conjunctiva, blurred vision, ulceration of the cornea), organs of smell (dryness of the nasal mucosa), as well as general phenomena (dizziness, nausea, etc.).
During therapy, wearing contact lenses is contraindicated.
The most popular mast cell membrane stabilizer in pharmacology is Ketotifen.
What is it used for?
This medication and its analogues are used for preventive purposes in the event of asthma attacks, allergic rhinitis and dermatoses. It is recommended to take 1-2 mg (in the form of capsules and tablets) or 1-2 tsp. syrup 0.02% twice a day with food.
During treatment with such drugs, it is possible to develop side symptoms, for example, dry mouth, increased appetite and associated weight gain, excessive drowsiness, and inhibition of reaction rates. The drug enhances the effect of sleeping pills and sedatives, as well as alcohol.
ALLERGIC DISEASES: DRUGS OF CHOICE
Preferanskaya Nina Germanovna
Art. Lecturer at the Department of Pharmacology, MMA named after. THEM. Sechenov Substances that can cause allergies are called allergens. Allergens are primarily foreign proteins, but there may also be substances of a non-protein nature, including low molecular weight compounds, such as bromine or iodine. Allergens can enter the body both from the external environment, in which case they are called exoallergens, and they can be produced in one’s own body, in which case they are called autoallergens (endoallergens). Exoallergens include: plant substances (pollen from ragweed, poplar, sticky alder, etc., fruits, leaves, plant roots); substances of animal origin (dander, wool, fluff); household allergens (house dust, book dust, detergents, chitin cover and waste products of house mites, etc.); food products (milk, meat, chocolate, nuts, citrus fruits, seafood); medicines (antibiotics, sulfonamides, hormones); bacterial, viral and other infectious allergens, industrial - various chemical compounds - such as benzopyrene, ethylenediamine, organic solvents, detergents, varnishes, paints, cosmetics and many others. Allergies are based on the body's immune response. With the help of the immune system, the human body detects, recognizes, inactivates (neutralizes) and removes those substances that bear signs of foreign genetic information. Foreign biological objects (foreign substances) that have specificity, immunogenicity and antigenicity are called antigens. In the process of protecting the body from antigens, a complex of specific and nonspecific immune reactions takes part. Having received a signal about the appearance of antigens in the body, the immune system is activated, the formation of antigen-specific clones occurs, their differentiation and intensive biosynthesis of specific antibodies - immunoglobulins involved in the humoral response and thymus-dependent cells involved in cellular immunity. There are four types of allergic hypersensitivity reactions: type I - immediate, type II - cytotoxic, type III - immunocomplex, type IV - delayed. Allergic types of reactions in their pure form are rare; as a rule, they are combined or transform into one another during the course of the disease. Allergies are variants of the immune response (increased perverted specific reaction of the macroorganism) upon repeated contact with an antigen, which are accompanied by structural and functional damage to cells, tissues and organs. Delayed hypersensitivity reactions underlie transplant rejection and autoimmune diseases (contact dermatitis, systemic lupus erythematosus, rheumatoid arthritis, etc.). Medicines used for immediate allergic reactions are not considered within the scope of this article. Immediate type - a specific immune response, which is realized with the participation of B cells, mast cells, basophils, eosinophils, immunoglobulins (IgE), T helper cells of the second type, producing interleukins-4 and -5 and others, as a result of this reaction the following develop: allergic diseases : urticaria, serum sickness, hay fever, Quincke's edema, etc. There are three successive immediate stages: immune reactions, biochemical and pathophysiological disorders. The stage of immune reactions (sensitization) is characterized by the accumulation in the body of antibodies specific to a given allergen. The main producer of immunoglobulins is the mucous membrane of lymphoid tissue. IgE is firmly and long-term (up to 1 year) fixed on mast cells, while the half-life of free IgE is only 2 days. One mast cell can concentrate up to 400,000 IgE molecules. The stage of biochemical disorders develops when the allergen interacts with an antibody on the surface of mast cells, basophils or other immunocompetent cells. IgE is highly cytophilic, at one end they are attached to mast cells and basophils, and at the other end they bind antigen. The mast cell (immunocompetent cells) is sensitized and degranulation occurs, a large number of biologically active substances enter the blood: histamine, serotonin, leukotrienes, prostaglandins, platelet activating factor, chemotoxic factors, kinins, proteoglycans, etc. The most important powerful chemical mediator is histamine, which has a wide range of effects. Histamine activity occurs in extremely small doses. The resulting drop in blood pressure is due to the expansion of the capillary network, which, in turn, entails a decrease in the exchange of circulating blood. This causes redness of the skin, tinnitus, dizziness, increased heart rate and breathing. Under the influence of histamine, capillary permeability increases sharply and plasma is released into the tissues and their swelling occurs, itching and urticaria occur. The effect of histamine is in many ways similar to the clinical picture of allergic diseases (urticaria, hay fever, serum sickness, anaphylactic shock). A slow-reacting substance of anaphylaxis, the main biological components of which are leukotrienes C4, D4, E4, causing persistent bronchospasm. The released kinins (bradykinin, lymphokinin) generate pain, increase vascular permeability, dilate arterioles and constrict venules. Acetylcholine leads to a decrease in blood pressure and bradycardia. The stage of pathophysiological changes occurs as a result of the action of biologically active substances on the cells of organs and tissues. Common signs of allergic diseases are: swelling of the mucous membranes and subcutaneous fatty tissue, spasm of the smooth muscles of internal organs (bronchi, intestines, etc.), redness and rash on the skin, lacrimation, sneezing, etc. Treatment methods for allergic diseases are divided into two groups - specific and nonspecific. The first are aimed at the cause of the disease and involve stopping contact with specific allergens. If this is possible, then the increased sensitivity of the body is reduced with the help of specific hyposensitizing therapy (hyposensitization - decreased sensitivity) by creating specific antiallergic immunity. In this case, the patient is administered appropriate allergoids containing small doses of this allergen, which causes allergic reactions, to which resistance gradually develops. The production of antibodies to histamine and inactivation of free histamine is achieved by the administration of histamine preparations. These include: Histaglobulin, which is a mixture of small doses of histamine hydrochloride (0.00015 mg) and 12 mg of gammaglobulin (immunoglobulin) from human blood. Injected subcutaneously or intramuscularly; hyperemia is possible at the injection site. Course of 6–9 injections. Side effects include difficulty breathing, bronchospasm, rush of blood to the head, increased secretion of the gastric glands. Nonspecific treatment includes the use of drugs that act on all three stages of the development of allergic reactions. Antiallergic drugs are usually classified into groups: a) mast cell membrane stabilizers; b) blockers of H1-histamine receptors; c) leukotriene receptor blockers; d) glucocorticosteroids.
MAST CELL MEMBRANE STABILIZERS Medicines that stabilize the membranes of mast cells and basophils, inhibiting the release of histamine and other nutrients (bradykinin, MRSA, lymphokines, prostaglandins) involved in the development of allergic and other pathological reactions are used for the prevention of bronchial asthma, bronchospasm and the treatment of seasonal allergic reactions. reactions. Cromoglicic acid, nedocromil, ketotifen, oxatomide, and lodoxamide have these properties. The mechanism of action of these drugs is associated with the stabilization of cell membranes. By changing the hydration properties of these cells, the drugs inhibit the entry of calcium ions into the intracellular space, which in turn reduces the contraction of myofibrils and blocks the process of release of mediators from the granules that cause the main symptoms of allergy. Cromoglicic acid
is produced under different trade names and in different dosage forms:
Cromolyn sodium
, a 2% solution of the drug in aerosol packaging (spray) in 15 ml cans (1 mg - 200 single doses);
Cromohexal solution for inhalation
, 10 mg/ml/2 ml, nasal spray 2% – 15 (30) ml;
Cromogen inhaler
,
Cromogen easy breathing
,
Bicromat
- aerosol 15 g, (20 mg/2 ml) and ampoules for inhalation 2% - 10 ml,
Intal
- powder for inhalation in capsules 20 mg and aerosol for inhalation dosed 5 mg dose, 112 doses;
Optikrom, Lecrolin
– eye drops, 20 mg/ml, tube-drop 0.25 or fl-drop 10 ml;
Ifiral
capsules with powder for inhalation 20 mg;
Cromoglin
– eye drops 20 mg/ml, 10 ml bottles and spray 300 mg/15 ml spray bottles;
Sodium romoglycolate
– metered-dose nasal spray;
Lomuzol
is a spray for intranasal use, one dose contains 2.6 mg of sodium cromoglycate, available in bottles of 26 ml of 2% solution;
Nalkrom
- capsules, soluble in the intestines;
Kropoz
is an aerosol for inhalation, 1 dose contains 5 mg of cromoglycic acid, 150 doses in a 15 ml can;
combination drug Ditek
.
One inhalation dose of Ditek
contains 1 mg of sodium cromoglycate and 0.05 mg of fenoterol and exhibits bronchodilator, protective and anti-inflammatory effects.
The presence of two drugs makes it possible to block not only the early phase, but also to influence the later manifestations of bronchospasm. Cromoglicic acid inhibits the entry of calcium ions into the cell and blocks the process of release of biologically active substances from granules. It is believed that the drug inhibits the chemotaxis of eosinophils, neutrophils, and monocytes (directed movement of cells towards the object of phagocytosis). It is effective for the treatment of patients with allergic bronchial asthma and has a preventive effect when used before an asthma attack. The drug is not used to relieve acute asthma attacks. Dosage forms of the drug are prescribed as the main or auxiliary agent, depending on the course of the disease, because its action develops slowly. The maximum effect usually occurs after a week. While taking inhaled forms of the drug, a cough or short-term bronchospasm or laryngeal edema sometimes occurs. In case of severe adverse events, discontinuation of the drug is required. When taking oral forms, nausea, unpleasant taste in the mouth, burning sensation, swelling, and skin rash occur. When taking eye drops, lacrimation, dryness around the eyes, and short-term blurred vision occur. In terms of antihistamine and antiallergic effects, Ketotifen
(Zaditen, Astaphen) is close to cromoglycic acid, but unlike it, it has a weak sedative effect and non-competitively blocks H1-histamine receptors.
The BBB passes through and depresses the central nervous system. Stabilizes mast cells and basophils, inhibits phosphodiesterase, increases cAMP levels in cells, suppresses eosinophil sensitization and prevents the development of symptoms of airway hyperresponsiveness. Passes into breast milk. A pronounced therapeutic effect develops after 6–8 weeks. Available in 1 mg tablets and syrup in bottles. When using it, dizziness, drowsiness, lethargy, dry mouth, increased appetite, and weight gain are observed. Oxatomide
(Tinset, Phensedyl) is similar in pharmacological action to cromoglycic acid, is available in 30 mg tablets, take 1-2 tablets 2 times a day.
Nedocromil
(Tailed, Tilarin, Tilavist), in addition to its antiallergic effect, has anti-inflammatory activity.
Reduces the yield of cationic protein and mobilizes intracellular calcium ions to a lesser extent. Nedocromil is available as an aerosol in cans containing 56 or 112 single doses of the drug, each dose containing 2 mg. The drug improves nighttime symptoms in patients with bronchospastic reactions and reduces the need for bronchodilators. Not used to relieve an acute attack of bronchospasm. Adults and children over 12 years of age are prescribed 2 doses 4 times a day, maintenance therapy - 2 inhalations 2 times a day. Lodoxamide
(Alomid) is mainly used for allergic eye diseases: vernal keratoconjunctivitis, vernal keratitis and others, as well as for allergic reactions caused by wearing contact lenses.
When applied locally, it does not exhibit systemic effects, there are no mutagenic or carcinogenic effects. Prescribed to adults and children over 2 years of age, 1-2 drops 4 times a day for no more than 3 months. It is not recommended to wear contact lenses during treatment. ANTIHISTAMINES (H1-histamine receptor blockers) Antihistamines relieve the effects caused by the action of histamine: nasal congestion, sneezing, itching, rhinorrhea, decreased blood pressure, spasms of smooth muscles (intestines, bronchi, ureter), increased capillary permeability, swelling of the mucous membranes. The mechanism of action of antihistamines is based on the blockade of H1-histamine receptors localized in the bronchi, intestines, blood vessels, and neurons of the central nervous system. As a result, tissue and organ cells become insensitive to histamine. The first drugs of this group were synthesized in the early 40s of the last century; they have a competitive effect on histamine receptors, their effect is reversible and depends on the concentration of the free (pharmacologically active) drug in the blood plasma. In 1977, non-competitive selective antagonists with high affinity for H1-histamine receptors were synthesized. Antihistamines are used not only to: prevent the occurrence of undesirable effects during the development of various allergic reactions, but also to eliminate undesirable histamine effects in case of extensive injuries to the skin and soft tissues, burns, frostbite; for complex treatment of emergency conditions of an allergic nature during an attack of bronchial asthma, with the development of anaphylactic shock, Quincke's edema, acute pulmonary edema. Diphenhydramine
or
Promethazine
are used as the main means of premedication before anesthesia and surgery ;
in the postoperative period for pain syndrome, 1st generation drugs are mainly used to potentiate the effect of analgesics. The antiemetic effect is used for sea and air sickness, less often used for vomiting of pregnant women, using Promethazine
(Diprazine, Pipolfen) or
Diphenhydramine
(Diphenhydramine).
Antihistamines are classified by generation, taking into account the duration of their action and the severity of the pharmacological effect. First-generation antihistamines differ from drugs of other generations in that, in addition to antihistamine activity, they have a depressant effect on the central nervous system with sedative and hypnotic effects. All drugs in this group have an irritant and local anesthetic effect. Some representatives of this group enhance the effect of analgesics, local anesthetics and have an antiemetic effect. When taken orally, the drugs are quickly absorbed and therefore have a short latent period; this property is used for rapidly developing allergic reactions. Long-term use of these drugs somewhat reduces their pharmacological effect, and addiction (tolerance) develops. 1st GENERATION ANTIHISTAMINES short-acting (4-6 hours): diphenhydramine, promethazine, chloropyramine Diphenhydramine
(Diphenhydramine, Allergin), an ethanolamine derivative, in addition to the antihistamine effect, has a ganglion-blocking, as well as moderate hypnotic, antispasmodic and antiemetic effect.
It has local anesthetic activity, so when taking the drug orally, some numbness of the tongue is observed. Diphenhydramine
is prescribed for allergic phenomena caused by taking medications, for allergic diseases (urticaria, hay fever, serum sickness, vasomotor rhinitis, pruritic dermatosis).
The drug is used for sea and air sickness, because it has an antiemetic effect by blocking H1-histamine receptors in the cerebellum, thereby disrupting the conduction of impulses from the vestibular apparatus to the center of vomiting. For bronchial asthma, Diphenhydramine is not very effective, but it is still prescribed in combination with antispasmodics. Locally it has an irritating effect, so it is not injected under the skin, but is taken mainly internally. Due to its hypnotic effect, it is not recommended for use by transport drivers. List “B” Higher doses for adults orally: single dose – 0.1 g; daily – 0.25 g; intramuscularly: single dose – 0.05 g; daily – 0.15 g. Release forms – tablets of 0.03 and 0.05 g; 1% solution in ampoules of 1 ml. Promethazine
(Diprazine, Pipolfen) is a phenothiazine derivative and is somewhat similar in pharmacological properties to aminazine.
Promethazine is superior to diphenhydramine in its antihistamine action. Similar to Aminazine, but to a lesser extent, Promethazine has a sedative, anticholinergic and adrenergic blocking effect. It also enhances the effect of anesthetics, sleeping pills, analgesics and local anesthetics. Indications for use and side effects are the same as for diphenhydramine; sometimes a strong decrease in blood pressure is observed. The drug has a local irritant effect and can cause dermatitis and inflammation of the mucous membranes, so it is recommended to take precautions when working with this drug. List “B” Higher doses for adults orally: single – 0.075 g, daily – 0.5 g; intramuscularly: single dose - 0.05 g, daily - 0.25 g. Release forms: tablets, dragees 0.025, 0.05 g; 2.5% solution in ampoules of 1 and 2 ml. Chloropyramine
(Suprastin) is a short-acting derivative of ethylenediamine.
Take 25 mg tablets orally with meals 2-3 times a day. In severe and acute cases of allergic manifestations, 1–2 ml of a 2% solution is administered intramuscularly or intravenously. First generation antihistamines with an average duration of action include Clemastine
and
Quifenadine. Clemastine
(Tavegil) is close in structure and action to Diphenhydramine, but surpasses it in activity and duration of action (6–12 hours).
Less CNS depressant. Available in tablets of 0.001 g. In the laboratory of M.D. Mashkovsky synthesized the domestic drug Khifenadine
(Fenkarol), the duration of action of which is 6–8 hours, the pharmacological action is somewhat different from other drugs.
It not only blocks H1-histamine receptors, but also activates an enzyme directly in the tissues that destroys histamine diamine oxidase (histaminase). The drug has low lipophilicity, which prevents it from penetrating the blood-brain barrier into the central nervous system and binding to other receptors, does not accumulate in the body and does not cause cardiotoxicity or addiction. Khifenadine (Fenkarol), a derivative of Quinuclidine, unlike Diphenhydramine and Promethazine, does not have a pronounced inhibitory effect on the central nervous system, does not have an adrenergic blocking or anticholinergic effect. The drug has antiserotonin activity, has a pronounced antipruritic effect, and is used to treat allergic skin diseases, hay fever, etc. Selectivity of action and low toxicity determine the good tolerability of the drug. Apply after meals orally at 10, 25 or 50 mg 3-4 times a day. The duration of treatment depends on the nature and severity of the disease and averages 10–20 days. Hifenadine is not recommended for use in pregnant women under 3 months. First generation long-acting antihistamines (36 hours) include the tetrahydrocarboline derivative Mebhydrolin
(Diazolin).
Unlike short-acting drugs, Mebhydrolin has virtually no depressant effect on the central nervous system, does not have a hypnotic or sedative effect, and is well tolerated by patients. Mebhydrolin is characterized by low toxicity and has virtually no side effects. When taken orally, the drug is rapidly absorbed. Locally, if the integrity of the dragee is damaged, Mebhydrolin can have an irritating effect, so it is recommended to swallow it whole without biting it. The classification of antihistamines into 2nd and 3rd generation is conditional, because Their pharmacological characteristics differ little. More often they are divided into first-generation drugs, which are highly lipophilic and penetrate the central nervous system and, therefore, have central side effects, and new-generation drugs (the so-called non-sedating antihistamines), which do not penetrate the blood-brain barrier. SECOND GENERATION ANTIHISTAMINES: Loratadine, Cetirizine, Azelastine, Akrivastine, Levocabastine, Mechitazine, Dimetindene, Eebastine have a high degree of affinity for H1-histamine receptors with a prolonged action of 24 hours. Drugs of this group in therapeutic doses do not penetrate the BBB and have no effect on the central nervous system, but easily penetrate into breast milk, so they are not recommended for use during breastfeeding. If an allergic reaction develops, they are ineffective, because these drugs have a long latent period of 1 to 3 hours and 15–20 minutes after taking the drug will not be able to have a pronounced pharmacological effect, which occurs only after 2–4 hours. Loratadine
(Claritin, Claridol, Erolin) has an antiallergic effect, preventing the development and easing the course of allergic reactions.
Selectively blocks H1-histamine receptors, preventing the effect of histamine on organs and tissues, the antihistamine effect develops after 3 hours, maximum after 8-12 hours. The drug has an antipruritic and antiexudative effect, reduces capillary permeability, reduces erythema, and inhibits exudation. Available in tablets of 0.01 and syrup of 60 and 120 ml, 1 ml contains 1 mg of active substance. Food intake does not have a significant effect on pharmacokinetics, but slows down the time to reach therapeutic concentrations in the blood by one hour, so it is recommended to take the drug before meals and should not be used in children under 2 years of age. The active metabolite of Hydroxyzine is the second generation drug Cetirizine
(Zyrtec, Allertec, Parlazine), which is a competitive antagonist of H1-histamine receptors, affects the early stage of the action of histamine and blocks the release of inflammatory mediators in the late phase of the allergic reaction, stabilizes the membranes of mast cells.
Available in film-coated tablets, 0.01 and 0.02 g in drops for oral administration, in a 10 ml bottle. Other drugs also have a pronounced pharmacological effect on seasonal and year-round allergic diseases. Azelastine
(Allergodil) is available as a nasal spray, dosed 0.14 mg/0.14 ml, 10 ml and eye drops 0.05% - 6 ml.
Acrivastine
(Simprex) does not cause irritation to the gastric mucosa and is available in 8 mg capsules.
Levocabastine
(Histimet) is available in suspension.
eye drops and nasal spray 0.5 mg/ml. Dimetindene
(Fenistil) drops containing 1 mg in 1 ml, long-acting capsules of 4 mg and gel in tubes of 20 and 30 g, is the drug of choice for children starting from 3 months, is not addictive, long-term use is possible for up to a month.
Ebastine
(Kestin) has a long-term action of 48 hours, and after 5 days of taking the drug, activity remains for 72 hours due to the formation of the active metabolite carabastine.
After oral administration, it is quickly absorbed, the action develops after 1 hour. Fatty foods accelerate absorption and blood concentrations increase by 50%. Available in 1 mg syrup in 60 and 120 ml bottles and 10 mg tablets. Mekhitazine
(Primalan), a phenothiazine derivative, blocks H1-histamine receptors.
It has antiallergic, antipruritic and anti-edematous effects. The anticholinergic effect is weakly expressed. Prevents the release of biologically active substances from mast cells that are mediators of allergies and inflammation. Does not have a pronounced effect on the central nervous system. Mechitazine tablets are prescribed for adults and children over 12 years of age, 5 mg 2 times a day, morning and evening (before bed), or 10 mg 1 time (in the evening). Eating does not affect the amount of absorption; the effect begins after 30 minutes. and continues for 24 hours. It has been discovered that many second-generation drugs, when entering the body, are metabolized to form pharmacologically active metabolites. In patients with impaired liver function, the biotransformation of drugs changes with the formation of toxic compounds that have undesirable side effects. Astemizole
(Gismanal, Stemiz) and
Terfenadine
was revealed , which were subsequently withdrawn from the pharmaceutical market (in 11 countries, including Russia, - Astemizole and in 8 countries - Terfenadine).
Third -generation antihistamines were created on the basis of second -generation active metabolites to eliminate cardiotoxic effects and enhance pharmacological effects. The active metabolite of the terphenin is the fecophenadin
(allergen, telfast, feced).
Disloratadin
(Erius) was created on the basis of the active metabolite of Loratadin,
Levo -Setirizin
(Xizal) - Cetirizin.
After oral administration, their effect develops after 1 hour, the maximum concentration in the blood is reached 3-7 hours after taking. They have a long pharmacological effect - 24 hours. The antihistamine effect of third-generation drugs is associated with high affinity with H1-gistamine receptors, this affinity is 2 times higher than that of its predecessors. The anti -allergic effect of this group of drugs is much higher than antihistamine, because They stabilize fat cells and other cells involved in an allergic response, the secretion and release of allergies are inhibited. The third-generation preparations are highly chosen and do not affect other receptors (adreno and holino-and-), do not penetrate through the hematoencephalic barrier and do not affect the central nervous system. Secret in breast milk. These drugs effectively eliminate symptoms such as nasal congestion, lacrimation, sneezing, bronchospasm. With prolonged admission (month), the development of tolerance was noted. The absence of a pronounced sedative and other central side effects improves the qualitative condition of patients taking new generation antihistamines. However, when working, requiring an increased concentration of attention, it is necessary to check the individual reaction of the body to their intake. The main side effects of antihistamines of all groups are drowsiness, worsening attention, weakness, lethargy, inhibitory, impaired coordination, decreased performance, visual impairment, dry mouth, tachycardia, respiratory impairment, cramps, changes in appetite, dyspeptic disorders, etc. Preventions and treatment of the stage of pathophysiological disorders use antihistamines and antiserotonin drugs. Tsiprogeptadine
(peritol),
dimetinden, dimetenspiride
(Erepal) have antihistamine, antiserotonin, anti -colridikinin, and cholinolytic activity.
The most effective for itching dermatoses, eczema, neurodermatitis and allergic reactions caused by insect bites. Reduce the permeability of capillaries and the severity of local exudative manifestations. They have a sedative effect: they cause drowsiness, increased fatigue, so you should not prescribe the drug to persons whose work requires increased attentiveness. The drugs prevent the development of allergic reactions of an immediate type, as well as their possible strengthening, provoked by the release of new portions of histamine. Blocks of leukotriene receptors for bronchial asthma and diseases accompanied by bronchospastic reactions use leukotrien receptors that have anti -allergic, broncholitic, anti -inflammatory activity: corrugated
(aculat) and
montelucast
(Singular).
The drugs selectively competently block leukotrienes, reduce the severity of spasm of smooth muscles of bronchiol, blood vessels and reduce the secretion of mucus. Mucociliary transport improves, vascular permeability decreases and swelling is reduced. The preparations inhibit cheemotaxis eosinophils to light and reduce the products of superoxide alveolar macrophages. Physiological functions of the lungs against the background of their use are significantly improved. With the simultaneous use of acetylsalicylic acid and the spiralcast, the concentration of the latter in the blood plasma increases 1.5 times. However, gastrointestinal disorders, headache and allergic reactions can develop. Drugs are not used to stop bronchospasm. Glucocorticoids during the stages of allergic reactions can use glucocorticoid preparations. They inhibit the development of the stage of immune reactions, as they inhibit the production of antibodies in lymphocytes. Glucocorticoids stabilize the shells of cells on which allergens interact with antibodies, and thereby prevent their damage and release into the blood of abnormally large amounts of biologically active substances. Glucocorticosteroids are used only in extremely severe cases of allergic reactions. So, for example, hormonal drugs are used to combat swelling of the mucous membranes and respiratory tract. Glucocorticoids, with prolonged systemic use, give a number of severe complications and, therefore, should only be prescribed with ineffective treatment with other drugs or in vital indications. The dosage forms for external use are wider for various skin manifestations of allergies, this is the eye hydrocortisone ointment
and ointment:
prenisolone
(dermosolone),
triamcinolon
(fluorocort),
fluocinolon
(synalam, flucinar),
fluomethasone
(Lorinden A and C, Localcorean), and locomotive),
Betamethason
(CEO V, Acriderm, Beloderm), etc. To relieve spastic attacks with allergic asthma or allergies, use drugs that relieve spasm of smooth muscles of the bronchi-such as selective agonists of B2-adrenergic receptors:
phenoterol
(Beritek),
Salbutamol
(Venttolin),
Berodual
,
TERBUTALIN, Klenbuterol
(spiropent),
Salmeterol
(Serentent),
hexaprenalin
(Ipraddol),
orciprenaline sulfate
(alules, asthmopent);
M-cholinoblocators
(Iprotropy bromide (atrovent), Aerosol Troventol and Efatin); antispasmodics of myotropic action (Eufillin, Theophylline), prolonged action - theopack, Theopack; as well as means that reduce the permeability of the walls of the vessels and increase blood pressure. For a detailed description of broncholitic drugs, see MA 11/06). Phyto- and homeopathic therapy
For allergic diseases, auxiliary treatment methods are herbal medicine and homeopathic therapy
.
We should not forget that many herbal remedies are allergenic, especially for people suffering from hay fever. Specially selected mixtures containing from 5 to 10 herbal components, the herbal preparation Glyceram,
cough
,
drugs
Alpizarin, Tonsilgon N, Helepin D, Flacozid .
To prevent allergic conditions, it is recommended to use various echinacea preparations:
“Doctor Theiss Echinacea Extract”, Immunal, Immunorm, Sana-Sol, Echinacea-E.
The following tablets are used as homeopathic medicines: Rhinital, Influcid, Cinnabsin, Iricar, Luffel,
drops:
Schwef-hel, Allergopent-EDAS, Rinitol-EDAS, Karsat-EDAS
,
etc. It should be remembered that when using homeopathic medicines, an exacerbation of allergic symptoms may initially occur.
Luffel
is available in the form of tablets and nasal spray and has anti-allergic and anti-inflammatory effects.
For allergic rhinitis and rhinoconjunctivitis, which occurs if the allergen is pollen, tablets of the drug should be taken 4 weeks before the appearance and additionally use a nasal spray during the appearance of pollen. Iricar
, which is available in 50 g tubes in the form of ointment and cream for external use, has antipruritic and anti-inflammatory effects Indications for use are skin diseases accompanied by itching; skin reactions to insect bites and as part of complex therapy.
The right choice, an individual approach to selection and regular use of antihistamines eliminates the main symptoms and alleviates the course of allergic diseases.
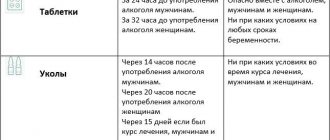
Pregnancy and membrane stabilizers
The use of systemic membrane stabilizers during pregnancy is contraindicated. Topical substances - cromones - are contraindicated for use only in the first trimester and are used with caution in subsequent periods. If there are indications, for example, with allergic rhinitis and conjunctivitis of the same nature in a chronic form, after 15 weeks of pregnancy it is allowed to use a 2% cromohexal solution in the form of eye drops or a spray for nasal use - in standard dosages.
During the lactation process, the use of cromones is carried out only if there are strict indications.
We examined the mechanism of action of mast cell membrane stabilizers.
Types of eye allergies
There are a wide variety of forms of eye allergies, the most common of which are allergic dermatitis and conjunctivitis. But it should be noted that an allergic reaction can affect all structures of the eye and cause damage to them, for example, keratitis, papilledema, uveitis, etc. An allergic process in the eyes or eyelids can be either an independent disease (a reaction to the ingestion of cosmetics, medications, or be a manifestation of a systemic disease (hay fever, etc.).