The liver is one of the most important life-support organs. It is considered the second largest in the human body - it weighs one and a half kilograms. The liver consists of two lobes - right and left. The organ communicates with the diaphragm by tissues, and the vitelline ducts, passing through the liver, collect bile and drain it into the intestines and gallbladder.
The liver filters blood from the digestive tract and is involved in digestion and detoxification. It serves as a storage facility for fats that the body uses during fasting. The liver plays an important role in our body, therefore any violations have a serious impact on the functioning of the body.
Pathologies are the cause of liver dysfunction. Experts identify more than a hundred diseases of the organ, which are provoked by various reasons and have different development, course and prognosis. Diseases can be chronic and hereditary. They appear in people of any gender and age. Some illnesses linger in the body for several years, and some for several days.
So why does the liver hurt? What diseases affect this organ? – Specialists from the Medunion private clinic will talk about this.
1.Common liver diseases
Liver diseases are a long list of diseases that are studied by a special branch of medicine - hepatology. Even though the liver is the only organ that is capable of complete regeneration, liver disease is very common and serious. Liver diseases can be either hereditary or result from various factors. Liver diseases can also be divided into temporary and chronic.
Here are just a few of the common liver diseases:
- Treatment of diffuse liver diseases;
- Functional hyperbilirubinemia;
- Primary biliary cirrhosis of the liver;
- Primary sclerosing cholangitis;
- Hepatolenticular degeneration;
- Chronic hepatitis;
- Liver tumors;
- Liver abscess;
- Acute hepatitis;
- Cirrhosis of the liver;
- Liver steatosis;
- Hemochromatosis;
- Liver cysts;
- Amyloidosis.
Hepatitis
Hepatitis is a general name for a group of inflammatory liver diseases of various etiologies. There are hepatitis A, B, C, D, E and F. Hepatitis, unlike other diseases, spreads to the entire organ, therefore it is considered especially dangerous.
Cirrhosis of the liver
Liver cirrhosis is a serious disease in which the liver becomes enlarged because... parenchymal tissue is replaced by fibrous tissue. Cirrhosis develops after prolonged alcohol abuse or as a result of viral hepatitis.
Liver cancer
Liver cancer is a malignant tumor in the organ. Typical symptoms of liver cancer:
- Jaundice;
- Heaviness and pain in the right side;
- Nausea and vomiting;
- Fever;
- Hemorrhagic syndrome;
- Ascites;
- Cachexia.
A must read! Help with treatment and hospitalization!
Liver function can be impaired due to many pathologies. In total, more than a hundred liver diseases are known, caused by different reasons and having different mechanisms of development, different course and prognosis. They occur in people of any age and can be congenital, hereditary, or acquired.
Some liver diseases have a short duration and end in complete recovery, others can bother a person for years and lead to irreversible changes in the liver tissue and serious, life-threatening complications.
English synonyms
Liver disease, hepatic disease.
Symptoms
In the initial stages, symptoms of liver disease may be nonspecific. Some diseases are asymptomatic. Characteristic signs of liver dysfunction appear when a significant part of the liver tissue is damaged. Main symptoms of liver diseases:
- nausea, vomiting;
- heaviness, pain in the right hypochondrium;
- yellowness of the skin, mucous membranes and sclera.
There are also a large number of additional symptoms, the presence and intensity of which depend on the form of liver pathology, the activity of the disease and the degree of damage to the liver tissue.
General information about the disease
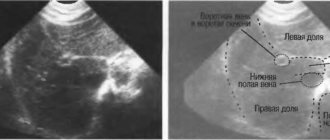
The liver is the largest gland in the human body. It is located in the right hypochondrium under the diaphragm, borders the stomach, right kidney and intestinal loops and consists of two main lobes and many lobules. Blood enters it through the hepatic artery and portal vein (from the gastrointestinal tract), and flows out from it through the hepatic vein. The liver also has a system of bile ducts, through which bile enters the gallbladder and intestines.
The liver performs a number of vital functions necessary for the normal functioning of the body:
- cleansing – cleansing the blood of microorganisms, toxins, allergens, poisons that enter the liver through the portal vein from the gastrointestinal tract, removing excess hormones and toxic metabolic products;
- synthetic – the formation of blood proteins (components of the blood coagulation and anticoagulation systems), hormones, enzymes, cholesterol, fats and their derivatives;
- digestive - synthesis of bile, which accumulates in the gallbladder, enters the intestine through the bile ducts and is involved in the digestion of fats;
- depositing - storage of blood, glycogen (a polysaccharide formed by glucose molecules), fat-soluble hormones, vitamins and microelements.
With liver disease, it can increase in size, which causes a feeling of heaviness in the abdomen. The outflow of bile, necessary for the digestion of fats, is disrupted, resulting in nausea, vomiting, increased gas formation, bloating, and bowel problems (diarrhea or constipation). The liver does not cope with the cleansing function, which leads to the penetration of poisons and toxins into the blood and causes malaise and weakness. When bile acids enter the bloodstream when liver cells are destroyed, it can cause itching. Yellowness of the skin and mucous membranes is caused by an increase in bilirubin levels. It is formed during the destruction of red blood cells, binds to glucuronic acid in the liver (direct, bound bilirubin is formed) and is excreted in the bile. In liver disease, this process is disrupted, and direct bilirubin enters the blood. Violation of protein (albumin) synthesis leads to a decrease in the osmotic pressure of the blood and the release of fluid into the tissue, as a result, edema occurs. Due to a decrease in the number of clotting factors, bleeding increases.
The following factors can cause liver damage:
- inflammation of the liver tissue, for example, with viral hepatitis;
- direct destruction of liver cells by poisons, toxins or malignant tumor cells;
- impaired blood flow in the liver, for example, with cardiovascular failure, hepatic vein thrombosis (Budd-Chiari syndrome);
- disruption of the outflow of bile, for example, when the bile duct is blocked by a stone;
- accumulation of fats and cholesterol in the liver, that is, steatosis.
Among the many liver diseases, the most common are:
- alcoholic hepatitis - inflammation of the liver as a result of many years of alcohol abuse, which has a toxic effect on liver tissue;
- cholelithiasis - the formation of stones in the gall bladder and bile duct;
- viral hepatitis A, B, C is an inflammation of the liver tissue that is caused by hepatitis viruses;
- non-alcoholic steatohepatitis - a disease that is accompanied by the accumulation of fats in the liver and can be combined with diabetes, obesity and other metabolic diseases;
- Liver cirrhosis is a serious disease in which irreversible changes occur in the liver tissue with the replacement of normal cells by fibrous connective tissue;
- liver cancer – it can also cause damage to the liver tissue by metastases from cancer of another location;
- toxic hepatitis - caused by a direct toxic effect on the liver of poisonous mushrooms, alcohol substitutes, arsenic compounds, toluene, benzene, lead and other substances.
Less common are hereditary and autoimmune liver diseases, tumors, as well as liver pathologies associated with diseases of other organs and systems of the body. The reasons for some of them are not fully understood.
Liver disease associated with other diseases and conditions
- Jaundice in pregnancy is a manifestation of severe pregnancy pathology, in which the liver can no longer cope with the increasing load.
- Sarcoidosis is a disease that affects the liver, lymph nodes, spleen, lungs and other organs with the formation of limited areas of inflammation in them - granulomas. The cause of the disease is not fully understood.
- Neonatal hepatitis is an inflammation of the liver that occurs in children in the first months of life. The most common cause is intrauterine infection with hepatitis A or B viruses. In some cases, the cause of liver damage remains unclear.
- Reye's syndrome is a severe damage to the liver and brain in children after viral infections, which is based on a disruption in the functioning of liver cell enzymes. Often associated with taking medications containing acetylsalicylic acid.
- Amoebic liver abscess is the formation of a purulent focus in the liver, which is caused by a parasite - dysenteric amoeba, which enters the liver from the intestines.
- Autoimmune diseases: autoimmune hepatitis is a disease in which cells of the immune system destroy normal liver cells; the reason for the formation of a pathological immune reaction is not fully known;
- primary sclerosing cholangitis - destruction of the bile ducts by cells of the person’s own immune system; as a result, inflammation and obstruction of the bile ducts develop.
- Hereditary diseases:
- Wilson-Konovalov disease - a disorder of copper metabolism, in which it is deposited in the liver and other organs;
- deficiency of alpha-1-antitrypsin (AAT), a protein that protects the lungs from damage, while a defective AAT enzyme accumulates in the liver, resulting in impaired lung and liver function;
- Alagille syndrome is a hereditary disease characterized by congenital heart defects, pathologies of the spine, eyes, liver and kidneys;
- Glycogen storage diseases - a violation of the synthesis and breakdown of glycogen; defective glycogen can accumulate in the liver, kidneys, intestinal walls and other organs, disrupting their function;
- galactosemia - a violation of the metabolism of galactose (sugar) and its conversion into glucose with the accumulation of its breakdown products, toxic to the liver and other organs;
- hemochromatosis is a disease in which the absorption of iron in the intestine increases and it is deposited in the tissues of the body.
Who is at risk?
- People who require long-term use of medications that are toxic to the liver.
- Drug users.
- Alcohol abusers.
- Not vaccinated against hepatitis A and B.
- Frequently in contact with high doses of toxic chemicals - pesticides, insecticides, household chemicals - without appropriate protective equipment (masks, gloves).
- Pregnant women.
- Obese people.
Diagnostics
Diagnosis of liver diseases is aimed at determining the immediate cause of the pathological process and the degree of damage to the liver tissue. A number of studies are also necessary to monitor the effectiveness of the therapy. Some diagnostic methods can detect the disease in the initial stages, when symptoms are absent or mild.
Laboratory diagnostics
- General blood analysis. The level of leukocytes may be increased, which is caused by insufficient purification of the blood from microorganisms or an infectious cause of liver damage. A lack of platelets may also be detected due to a decrease in the concentration of thrombopoietin, an active substance that is synthesized by the liver and stimulates the formation of platelets.
- AST (aspartate aminotransferase), ALT (alanine aminotransferase). Liver enzymes that enter the bloodstream when liver tissue is damaged. With liver disease, their increase is likely.
- Gamma-glutamyl transpeptidase (gamma-GT). A liver enzyme, the amount of which increases with damage to the liver and bile ducts. This is especially true for alcoholic hepatitis.
- Prothrombin index. Prothrombin is a precursor of thrombin and is involved in blood clotting. The test is used to assess the rate of blood clotting. In liver diseases, the prothrombin index may be reduced.
- Fibrinogen is a blood clotting factor that is synthesized by liver cells. When liver tissue is damaged, it may be reduced.
- Alkaline phosphatase is an enzyme that is found in all tissues of the body, but mainly in the bones, kidneys and liver. In case of liver diseases, it may be increased.
- Total bilirubin. In liver cirrhosis, it is increased mainly due to the direct (bound) fraction.
- Total whey protein. In liver disease, the level of total protein can be reduced by reducing the amount of albumin. Albumins are the main proteins in blood plasma that are synthesized in the liver.
- Total cholesterol is a substance that is synthesized in the liver and is an element of cell membranes, a precursor of bile acids and some hormones. In case of liver diseases, it may be lowered.
- Tests for hepatitis B, C, D. The presence of hepatitis viruses and antibodies to them in the body is determined.
- Ferritin, transferrin. Ferritin is a protein that binds iron in the liver, and transferrin is a protein that transports iron from the intestines to the liver. Their levels may also be elevated in hemochromatosis.
- Copper, ceruloplasmin. The level of these substances is examined if Wilson's disease is suspected, in which there is a decrease in the level of ceruloplasmin and an increase in the amount of copper in the body.
- Alpha-1 antitrypsin. A decrease in the level of this enzyme may indicate congenital alpha-1 antitrypsin deficiency.
- Alpha fetoprotein. This is a protein that is produced in the liver and gastrointestinal tract of the fetus. The maximum level of alpha-fetoprotein is observed in the fetal blood at the 13th week of pregnancy, which causes an increase in the amount of this protein in the mother's blood. Normally, men and non-pregnant women have very low levels of alpha-fetoprotein - less than 1% of the level of alpha-fetoprotein in the fetal blood. However, in diseases that are accompanied by active cell division (proliferation), its amount may increase. In particular, an increase in alpha-fetoprotein levels is a marker for testicular cancer in men or liver cancer.
- Antimitochondrial antibodies are proteins that destroy the membranes of mitochondria (cell components necessary for energy production). Their level may increase in primary sclerosing cholangitis.
- Screening study for the presence of narcotic, psychotropic and potent substances. Determination of compounds that could cause liver cell destruction.
Additional research:
- Ultrasound of the abdominal organs. Used to determine the size and structure of the liver. It also allows you to identify abscesses, granulomas and other pathological elements in the liver tissue.
- Radiography. Used to determine the size and structure of the liver, and to exclude other liver diseases. With cirrhosis, the liver can be enlarged or reduced, the liver tissue is heterogeneous, with areas of compaction.
- Angiography is of great importance in diagnosis - an x-ray examination with the introduction of a contrast agent into the liver vessels, which is clearly visible in the pictures. Used to assess hepatic blood flow.
- Cholangiography. X-ray examination, which is carried out after the injection of a contrast agent into the bile ducts. Allows you to assess the patency of the bile ducts.
- CT, MRI. Methods that resemble radiography, but provide more detailed and clear information about the structure of the liver.
- Radionuclide scintigraphy. This test involves injecting a special short-lived radioactive substance into the body, which is absorbed by liver cells, and then obtaining an image by recording the radiation it emits. Allows you to assess the condition of liver cells and the patency of the bile ducts.
- Fibroelastometry. A method reminiscent of ultrasound. A sensor is used that generates oscillations of a certain frequency. Used for liver cirrhosis to determine the percentage of connective tissue in the liver.
- Liver biopsy. The procedure for taking a sample of liver tissue is carried out using a thin hollow needle, which is inserted through the skin of the abdominal wall after preliminary anesthesia.
Treatment
Treatment of liver diseases is directly determined by the cause of the development of the pathological process. For example, antiviral and antibacterial drugs can be used to treat infectious liver lesions. The treatment regimen also depends on the stage of the disease and the degree of damage to the liver tissue.
Many liver diseases require long-term, complex treatment, which, in addition to treating the immediate cause of the disease, includes monitoring the main symptoms of liver pathology, diet, and general health procedures. In Russia, so-called hepatoprotectors are also used, that is, medications that protect liver tissue. However, there is still no reliable evidence of the effectiveness of these drugs, and they are not used in other countries.
In certain cases, surgical treatment is effective, for example, for cholelithiasis, portal hypertension. Some patients with severe liver disease that cannot be treated with medication may require a liver transplant.
Prevention
- Timely vaccination against hepatitis A and B
- Use of personal hygiene products
- Quitting alcohol and drugs
Recommended tests
- General blood analysis
- Coagulogram No. 2 (PI, INR, fibrinogen)
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Alkaline total phosphatase
- Total bilirubin
- Direct bilirubin
- Total protein in whey
- Serum albumin
- Total cholesterol
- Transferrin
- Ferritin
- Ceruloplasmin
- Copper in the blood
- Alpha 1-antitrypsin
- α-fetoprotein (alpha-FP)
- HBsAg
- Anti-HCV
- Anti-mitochondrial antibodies (AMA)
- Screening study for the presence of narcotic, psychotropic and potent substances
- Cytological examination of punctates, scrapings of other organs and tissues
3.Risk factors
Risk factors that affect the likelihood of developing liver disease:
- Work in chemical laboratories conducting analyzes of body fluids;
- Increased levels of cholesterol and triglycerides in the blood;
- Work involving chemicals and toxins;
- Some medicines;
- Alcohol abuse;
- Piercing and tattoos;
- Blood transfusion;
- Unsafe sex;
- Obesity;
- Diabetes.
About our clinic Chistye Prudy metro station Medintercom page!
How does the disease manifest itself?
This organ is located in the abdominal cavity under the diaphragm, in the right upper quadrant of the abdomen. Many people who suspect they have certain diseases are interested in three questions: “How does the liver hurt and where?”, “What does pain and discomfort in the right hypochondrium indicate?” It should be noted here that there are no nerve endings in the organ itself, so the sensation of pain in the liver is impossible. However, there are a lot of nerve endings in the outer shell (capsule) of the liver. Therefore, if the liver enlarges and begins to put pressure on the capsule, the person experiences discomfort. There is never any acute pain. As a rule, she is stupid and persistent, and does not let go for a long time. As problems increase, the pain intensifies, becomes constant, and is especially evident when moving. In some cases, discomfort occurs in the right shoulder blade and back. If the pain is severe and cramping, then, as a rule, it speaks not of diseases of the liver, but of the gallbladder and biliary tract.
4. Diagnosis and treatment of liver diseases
Diagnosis of liver diseases
To diagnose liver diseases, the first step is to consult a general practitioner. He will take a history and ask you about your symptoms. If your GP decides that you have any liver disease, they will refer you to a hepatologist. The hepatologist, depending on the complaints and symptoms, will prescribe the following diagnostic methods:
- CT, MRI, ultrasound or any other research technique that allows you to see the organ;
- Various blood tests;
- Liver biopsy.
The most obvious signs of liver disease and their causes
Persons suffering from liver pathologies experience a number of characteristic symptoms that unmistakably indicate severe diseases of the organ. These include:
- Jaundice.
- Bleeding.
- Ascites.
- Encephalopathy.
- Liver fibrosis.
Jaundice
This is a clear sign of liver damage. It is expressed by yellowing of the entire body, also mucous membranes and eyes. There is skin itching and malaise. The condition is associated with liver dysfunction, when a lot of bile pigment accumulates in the body due to the inability to fully filter the blood.
Bleeding
As a rule, bleeding develops from nearby organs - the esophagus or stomach due to high pressure in the liver. The main symptoms of blood loss are severe nausea with bloody vomiting and black, sticky stools. The condition requires urgent medical attention.
Ascites
It represents extensive congestion throughout the body due to increased pressure in the liver. The abdomen increases in size, appetite and general well-being worsen. There are breathing problems, especially when lying down.
As a result of malnutrition, the body does not receive enough vitamins and nutrients it needs.
This condition is dangerous because the fluid in the body can become infected, causing extremely serious consequences.
Characteristic signs of ascites: acute and severe abdominal pain, fever. Medical intervention required.
Encephalopathy
It occurs due to severe intoxication of the body, as a result of which the brain suffers. The initial symptoms of encephalopathy are sudden changes in mood, sleep and memory disturbances. Late symptoms include confusion, drowsiness, chronic fatigue and unusual behavior.
All of these symptoms appear differently, depending on the degree of liver damage.
Contributing factors are:
- Causative agents of hepatitis.
- Overweight.
- Genetic disorders.
- Improper nutrition.
- Autoimmune diseases.
Tips for liver disease
Those who suffer from liver disease need to give up bad habits, eating spicy, hot, fatty foods. Heat and tanning should be avoided. Food should be consumed steamed, boiled, or stewed. It is not recommended to eat yesterday's food. You should not eat onions and garlic, but it is better to add horseradish and mustard to your food; eat boiled chicken, not fried chicken. You also can’t eat duck, goat meat, or dried meat. Eat vegetables raw. Do not eat too much dairy products, eat often, but little by little.
You can eat sweets; sweet tea can help with liver pain. Also eat foods that are sweet, bitter, or astringent.
Help the liver with Phosphogliv*
If liver problems are detected, the patient is prescribed diet and exercise; if this is not enough, therapy is supplemented with medications. It often includes the use of hepatoprotectors - drugs for treating the liver. One such drug is Phosphogliv*. Phosphogliv* is used as a means of pathogenetic therapy. This product contains 2 active ingredients: glycyrrhizic acid and essential phospholipids.
Glycyrrhizic acid has anti-inflammatory, antioxidant and antifibrotic effects, which allows the drug to be used both at the stage of treating inflammation and for preventing its development, and essential phospholipids restore damaged liver cell membranes. The use of the drug Phosphogliv* ensures normalization of the patient’s general condition, relief of the inflammatory process in the liver - a decrease in ALT and AST enzymes, and also helps prevent the development of fibrosis and cirrhosis.
Treatment technologies
After processing all the data, three options are possible: the doctor will prescribe a special diet for you; will prescribe complex drug treatment to eliminate the causative agent of the disease; or will also prescribe additional treatment, taking into account the existence of other pathologies (diseases of the cardiovascular system, respiratory, urinary, etc.)
Acute diseases of the liver and gallbladder are completely curable in most cases, but chronic diseases are almost impossible to completely cure. During chronic treatment in our clinic, doctors achieve rapid relief of exacerbation, long-term remission, preservation of maximum liver function (that is, compensation for liver failure), and the gall bladder.
Timely diagnosis and prompt initiation of treatment will reduce medical intervention, as well as the consequences of the disease, to a minimum. Contacting a gastroenterologist at our clinic guarantees you qualified diagnostic and therapeutic services. You will be treated according to an individual program.