In the modern world, there is a great choice of everything and everyone, including contraceptives. Moreover, each manufacturer praises its means of protection, usually emphasizing only the advantages and keeping silent about the disadvantages.
It is quite difficult to independently understand such a flow of diverse and sometimes contradictory information, but in this article we will try to objectively highlight all the pros and cons of the main means of contraception.
To begin with, it is worth noting that there are quite a few methods of contraception, but only 2 of them are used for long-term protection against pregnancy: intrauterine devices and hormonal contraceptives .
Formacology of Klayra
Qlaira is a contraceptive for oral administration. These are tablets containing a small amount of hormones that have a minimal systemic effect on the body, while completely controlling the female cycle, suppressing ovulation. Tablets of the same package differ in composition, so it is important to follow the order in which they are taken. Some are designed for estrogen and gestagen periods.
In addition to controlling the cycle and suppressing ovulation, Qlaira allows you to increase the thickness of cervical mucus and reduces the sensitivity of uterine epithelial cells to the initial period of embryo formation.
An additional property of the drug is a shortening of the period of withdrawal bleeding (pseudomenstruation) and a decrease in the severity of unpleasant symptoms associated with it. These include headaches, abdominal pain, nervousness and other symptoms.
Birth control pills: advantages and disadvantages
Birth control pills (oral contraceptives) are the most common method of hormonal contraception.
Oral contraceptives use synthetic hormones that are similar in action to those produced by the body itself.
The composition of birth control pills must include the hormone gestagen , which provides protection against pregnancy.
Based on their composition, oral contraceptives are divided into:
- gestagenic (contain only the hormone gestagen)
- combined (contain two hormones: gestagen and estrogen (needed to control the menstrual cycle))
Principles of action of oral contraceptives
Birth control pills:
- suppress or inhibit ovulation
- affect the composition of the cervical mucus of the cervix, making it more viscous and thick, which prevents the passage of sperm into the uterus
- affects the endometrium (mucous lining) of the uterus so that a fertilized egg cannot implant in it
- progestin tablets additionally reduce the mobility of the fallopian tubes , which slows down the movement of the egg through them and, as a result, the likelihood that the sperm will have time to fertilize decreases
Benefits of birth control pills
- High degree of protection – up to 99% when used correctly
- It is possible to become pregnant in the next cycle after stopping oral contraceptives, but it is recommended to wait 3 months
- Can be used by nulliparous women
- Can be used to treat hormonal imbalances and some gynecological diseases
Disadvantages of birth control pills
Many disadvantages of oral contraceptives arise from their principle of action:
- mood swings
- nausea , sometimes vomiting
- breast tenderness
- weight gain (may be caused by fluid retention or changes in carbohydrate-fat metabolism)
- decreased libido
- worsening acne (quite rare)
- increased removal of microelements from the body . If there is a lack of microelements in the body, serious diseases can occur. When taking oral contraceptives, it is important to take vitamin complexes .
- deterioration in glucose absorption (rare)
- headache
- spotting (especially typical for oral contraceptives with one progestogen hormone)
- the hormone estrogen in combined birth control pills increases blood clotting (hypercoagulation), which leads to unpleasant consequences: the risk of thrombophlebitis, heart attack, stroke , and existing cardiovascular problems are aggravated.
- the need to take pills at the same time according to a strictly established schedule , otherwise the risk of becoming pregnant increases sharply
- To avoid negative consequences,
a gynecologist should
prescribe
birth control pills after conducting all the necessary studies
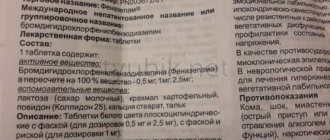
Depending on the type of gestagen (about a dozen different gestagens are used in pharmaceuticals) and on the presence or absence of estrogens (ethinyl estradiol is usually used) various side effects may be observed in oral contraceptives. The list of all side effects is indicated in the instructions for the tablets.
Contraindications to the use of birth control pills
- pregnancy
- presence of malignant tumors
- thrombosis or thromboembolism - the occurrence of blood clots in blood vessels
- previous heart attacks, strokes
- bleeding disorders
- cardiovascular diseases
- diabetes
- liver diseases
- smoking
- postpartum period less than 6 months
Conclusion
The use of birth control pills requires increased responsibility and self-organization, because the effectiveness of this method depends on the regularity of use.
The contraceptive effect does not occur immediately, but within a week after starting treatment.
Oral contraceptives affect hormonal levels, which leads to both simply unpleasant and dangerous side effects. However, they can be used in the treatment of certain gynecological diseases.
Intrauterine devices do not affect a woman’s hormonal background; their contraceptive effect is based on the physical properties of the components and appears immediately after installation.
Spontaneous loss of the IUD is possible, so it is necessary to check the presence of IUD threads in the vagina. It is also quite common to experience increased menstrual flow in the first months after installation. In addition, intrauterine devices increase the risk of developing inflammatory processes.
Both methods of contraception are highly effective.
The installation and removal of the IUD is carried out by a gynecologist. After some time, a re-examination is required, and if nothing worries you, further observation by a gynecologist is not necessary.
The selection and prescription of contraceptive pills should be carried out only by a gynecologist. Taking the wrong pills can lead to serious side effects. It is advisable to constantly monitor the condition of the body in order to promptly identify a lack of microelements or the development of concomitant diseases and correct their negative manifestations.
Pharmacokinetics of the drug
Absorption of the drug is assessed as high. An hour after taking the tablet, the maximum possible concentration in the blood is already reached. Food intake does not have any effect on the bioavailability of components, so it is not taken into account and is not mentioned in the recommendations.
About 90% of the substances received with the dose are bound to albumin, while the remaining 10% circulate in an unbound form. Qlaira has no effect on the transport of endogenous steroids.
The plasma half-life of dienogest is 11 hours. Some of it is released in the form of metabolites through the kidneys and intestines. Slightly less than half of the dose is excreted per day, and the larger remainder requires at least 6 days to exit through the kidneys.
The main indication for buying Qlaira is a woman’s desire to protect herself from unwanted pregnancy. It is important to remember that oral contraceptives cannot prevent sexually transmitted infections. Therefore, obstetricians strongly recommend using Qlaira and other tablet forms of contraception only if you have a regular sexual partner.
To protect against pregnancy, in the case of constantly changing partners, it is wiser to use barrier precautions.
In addition, Qlaira is prescribed for long or uneven menstrual cycles, as well as in combination with drugs prescribed by psychotherapists, the action of which is aimed at normalizing the neuropsychic state of a woman during premenstrual syndrome.
Claira
Use during pregnancy and breastfeeding
Taking Qlaira® is contraindicated during pregnancy.
If pregnancy occurs while using the drug Qlaira®, further use must be discontinued. However, large-scale epidemiological studies have not shown an increased risk of birth defects in children born to women who used COCs before pregnancy, nor have there been any teratogenic effects of COCs from accidental use early in pregnancy. COCs can affect lactation because they can reduce the volume of breast milk produced and also change its composition. Therefore, COCs are generally not recommended for use until after lactation. Small amounts of contraceptive hormones and/or their metabolites may be excreted in breast milk.
Use for liver dysfunction
Qlaira is contraindicated in women with severe liver disease until liver function tests return to normal (see also “Contraindications”).
Use for renal impairment
Qlaira has not been specifically studied in patients with impaired renal function. Available data do not suggest adjustment of the dosage regimen in such patients.
Use in children
The drug Qlaira is indicated only after the onset of menarche.
special instructions
If any of the diseases/conditions/risk factors listed below are currently present, the potential risk and expected benefits of using Qlaira® should be carefully weighed in each individual case and discussed with the woman before she decides to start taking it drug. If any of these conditions or risk factors worsen, intensify, or appear for the first time, a woman should consult her doctor, who may decide whether to discontinue the drug.
Diseases of the cardiovascular system
The results of epidemiological studies indicate a relationship between the use of COCs and an increased incidence of venous and arterial thrombosis and thromboembolism (such as DVT, PE, MI and cerebrovascular events). The risk of developing venous thromboembolism (VTE) is greatest in the first year of taking such drugs, mainly during the first 3 months. An increased risk is present after initial use of a COC or resumption of use of the same or different COCs (after a dosing interval of 4 weeks or more).
The overall risk of VTE in patients taking low-dose COCs (ethinyl estradiol content less than 50 mcg) is 2-3 times higher than in patients not taking COCs, however, this risk remains lower than the risk of VTE during pregnancy and childbirth.
VTE can be fatal (in 1-2% of cases).
VTE, manifested as DVT or PE, can occur while using any COC.
It is extremely rare when using COCs that thrombosis of other blood vessels occurs, for example, hepatic, mesenteric, renal, cerebral arteries and veins or retinal vessels. There is no consensus regarding the relationship between the occurrence of these events and the use of CCPs. Arterial thromboembolism can be fatal.
The risk of developing thrombosis (venous and/or arterial) and thromboembolism increases:
- with age;
- in smokers (with an increase in the number of cigarettes smoked or an increase in age, the risk increases, especially in women over 35 years of age);
in the presence of:
- family history (for example, venous or arterial thromboembolism ever in close relatives or parents at a relatively young age). In the case of a hereditary or acquired predisposition, the woman should be examined by an appropriate specialist to decide on the possibility of taking Qlaira®;
- obesity (BMI more than 30 kg/m2);
- dyslipoproteinemia;
- arterial hypertension;
- migraine;
- heart valve diseases;
- atrial fibrillation;
- prolonged immobilization; major surgery, any operation on the lower extremities or major trauma. In such situations, it is advisable to stop taking Qlaira® (for planned surgery, at least 4 weeks before it) and not to resume taking it for 2 weeks after the end of immobilization.
The possible role of varicose veins and superficial thrombophlebitis in the development of VTE remains controversial.
The increased risk of thromboembolism in the postpartum period should be taken into account. Peripheral circulatory disorders may also occur in diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn's disease or ulcerative colitis) and sickle cell anemia. An increase in the frequency and severity of migraines while using Qlaira® (which may precede cerebrovascular events) may be grounds for immediate discontinuation of this drug.
Biochemical factors indicating a hereditary or acquired predisposition to arterial or venous thrombosis include the following: resistance to activated protein C, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipid antibodies, lupus anticoagulant).
When assessing the risk-benefit ratio, it should be taken into account that treatment of the relevant condition may reduce the associated risk of thrombosis. It should also be taken into account that the risk of thrombosis and thromboembolism during pregnancy is higher than when taking low-dose oral contraceptives (ethinyl estradiol content less than 50 mcg).
Tumors
The most significant risk factor associated with the development of cervical cancer is persistent human papillomavirus infection (PVI). There are reports of a slight increase in the risk of advanced cervical cancer with long-term use of COCs. The connection with the use of COCs has not been proven. The possibility of the relationship of these data with screening for cervical diseases and characteristics of sexual behavior (less frequent use of barrier methods of contraception) is discussed.
A meta-analysis of 54 epidemiological studies found a small increase in the relative risk (RR = 1.24) of developing breast cancer in women currently taking COCs. The increased risk gradually disappears within 10 years of stopping these drugs. Because breast cancer is rare in women under 40 years of age, the slight increase in breast cancer diagnoses in women who are currently or recently taking COCs is small relative to the overall risk of breast cancer. Its connection with the use of COCs has not been proven. The observed increased risk may also be a consequence of earlier diagnosis of breast cancer in women using COCs. Women who have ever used COCs are diagnosed with earlier stages of breast cancer than women who have never used them.
In rare cases, during the use of COCs, the development of benign, and in extremely rare cases, malignant liver tumors, which in some cases led to life-threatening intra-abdominal bleeding, was observed. If severe pain in the upper abdomen, an increase in liver size, or signs of intra-abdominal bleeding occur in women taking COCs, liver tumors must be excluded in the differential diagnosis.
Other states
Women with hypertriglyceridemia (or a family history of this condition) may have an increased risk of developing pancreatitis while taking COCs.
Although slight increases in blood pressure have been described in many women taking COCs, clinically significant increases have rarely been reported. However, if a persistent, clinically significant increase in blood pressure develops while taking Qlaira®, the drug should be discontinued and treatment of arterial hypertension should be started. Taking Qlaira® can be resumed if necessary if normal blood pressure levels are achieved through antihypertensive therapy.
The following conditions develop or worsen both during pregnancy and when taking COCs, but their relationship with taking COCs has not been proven: jaundice and/or cholestatic pruritus, cholelithiasis, porphyria, systemic lupus erythematosus, hemolytic-uremic syndrome, Sydenham's chorea, herpes of pregnancy hearing loss caused by otosclerosis.
In women with hereditary forms of angioedema, exogenous estrogens may induce or worsen symptoms of angioedema.
Acute or chronic liver dysfunction may require discontinuation of Qlaira® until liver function tests return to normal. Recurrent cholestatic jaundice, which develops for the first time during pregnancy or previous use of sex hormones, requires discontinuation of the drug Qlaira®.
Although COCs may have an effect on insulin resistance and glucose tolerance, there is no need to change the therapeutic regimen in diabetic patients using Qlaira®. However, women with diabetes need careful monitoring while taking Qlaira®.
Cases of Crohn's disease and ulcerative colitis have also been described with the use of COCs.
Chloasma can sometimes develop, especially in women with a history of chloasma during pregnancy.
Women prone to developing chloasma should avoid exposure to the sun or UV radiation while taking Qlaira®.
Effect on laboratory tests
Taking Qlaira® may affect the results of some laboratory tests, including biochemical parameters of liver, thyroid, adrenal and kidney function, plasma concentrations of transport proteins, such as DRGs and lipid/lipoprotein fractions, parameters of carbohydrate metabolism, coagulation and fibrinolysis. These changes usually remain within laboratory limits.
Medical examinations
Before starting to use the drug Qlaira®, it is necessary to carefully evaluate contraindications to the drug’s use based on the woman’s life history, family history, as well as general medical and gynecological examination. The frequency and nature of these examinations should be based on existing standards of medical practice, with due consideration for the individual characteristics of each patient. As a rule, blood pressure is measured, the condition of the mammary glands, abdominal cavity and pelvic organs is checked, including cervical cytology.
It is necessary to explain to women that Qlaira® does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Reduced efficiency
The effectiveness of Qlaira® may be reduced if tablets with active ingredients are missed, gastrointestinal disorders occur while taking tablets with active ingredients, or during concomitant drug treatment.
Insufficient control of the menstrual cycle
While using the drug Qlaira®, especially in the first months of use, irregular menstrual-like bleeding (spotting or breakthrough uterine bleeding) may occur. Therefore, evaluation of any irregular menstrual-like bleeding should be carried out only after an adaptation period of approximately 3 menstrual-like cycles.
If irregular menstrual-like bleeding recurs or occurs for the first time after previous regular cycles, the possibility of non-hormonal causes should also be considered and a thorough examination should be performed to exclude malignancy or pregnancy. Such measures may include diagnostic curettage.
Some women may not develop menstrual bleeding while taking inactive white tablets. If the drug Qlaira® was taken in accordance with the rules specified in the “Dosage regimen” section, pregnancy is unlikely. However, if before the first absent menstrual-like bleeding the tablets were taken irregularly or there are no 2 menstrual-like bleedings in a row, you should not continue to use the drug Qlaira until pregnancy has been ruled out.
Impact on the ability to drive vehicles and operate machinery
There was no negative effect of the drug Qlaira® on the ability to drive a car or operate machinery, however, patients who experience episodes of dizziness and impaired concentration during the adaptation period (the first 3 months of taking the drug) should be careful.
Qlaira: instructions for use
The basic and most important rule is to take it daily, taking into account the time. If the first tablet was taken in the morning, then all subsequent doses should be taken in the morning. The course is continuous due to the well-developed composition of tablets for each day of the cycle separately.
There is no break between packages. If the last tablet of the pack was taken today, then starting tomorrow you will start taking tablets from the new pack. Withdrawal bleeding does not affect intake in any way. It can begin three to four days before one package runs out and not have time to finish before taking the first tablet of a new package.
Boxes of pills have special stickers to help forgetful ladies control their intake of Qlaira. Since a woman rarely starts taking it on Monday, the manufacturer offers 7 week stickers, in accordance with seven possible options for starting the billing week.
For example, if you took your first pill on Thursday, you need to select a sticker with a week whose first day is Thursday. It is glued onto the clamshell package so that Thursday (in this case) is above the first tablet. In this way, a woman will be able to control her intake - if after breakfast, for example, on Tuesday, she does not remember whether she took a dose today or not, she will open the package and see if the cell for Tuesday is empty. The new packaging, given the continuity of the course, will also be used with a sticker in which the first day of the week is Thursday.
Despite the fact that some tablets taken in the last days of the cycle are pacifiers and do not contain a hormone that suppresses ovulation, the woman is protected from unwanted pregnancy during all 28 days of the cycle, provided that the regimen and numbering of the tablets are not violated.
If a woman has previously taken a drug based on one gestagen, wore a uterine device, an implant, or used injections, she can switch to Qlaira any day. In the case of a spiral and an implant - on the day of removal. In a situation with injections - on the day of the expected next injection.
Qlaira®
If any of the conditions/diseases or risk factors listed below currently exist, a careful assessment of the expected benefits versus possible risks of using Qlaira® should be carried out for each woman individually and discussed before taking the drug. If any of these conditions, diseases, or risk factors worsen, become worse, or appear for the first time, a woman should consult her doctor, who may decide whether to stop taking the drug.
The following precautionary information is based primarily on data from clinical and epidemiological studies with COCs containing ethinyl estradiol.
Risk of developing VTE and ATE
The results of epidemiological studies indicate a relationship between the use of COCs and an increased incidence of venous and arterial thrombosis and thromboembolism (such as DVT and PE, myocardial infarction, cerebrovascular disorders). These diseases are rare.
An increased risk is present after initial use of COCs or resumption of use after a break of 4 weeks or more. The greatest risk of developing VTE is observed in the first year of COC use, mainly during the first 3 months.
The use of any COC increases the risk of VTE compared with no use. Drugs containing levonorgestrel, norgestimate, or norethisterone are associated with the lowest risk of VTE. Limited data suggest that Qlaira may have a risk of VTE in the same range. Choosing to take Qlaira® rather than one of the drugs that has the lowest risk of developing VTE. should only be done after discussion with the woman to ensure she fully understands the risk of VTE associated with COC use; the influence of her existing risk factors on the risk of VTE and the fact that the risk of developing VTE is maximum in the first year of using COCs.
VTE can be life-threatening or lead to death (in 1-2% of cases).
It is extremely rare when using COCs that thrombosis of other blood vessels occurs, for example, hepatic, mesenteric, renal, cerebral veins and arteries or retinal vessels.
Symptoms of deep vein thrombosis
: unilateral swelling or swelling along the vein, pain or discomfort in the lower limb only in an upright position or when walking, local increase in temperature, redness or discoloration of the skin of the lower limb.
Symptoms of pulmonary embolism:
difficulty or rapid breathing; sudden cough, including with hemoptysis; sharp pain in the chest, which may intensify with deep inspiration; sense of anxiety; severe dizziness; fast or irregular heartbeat. Some of these symptoms (eg, shortness of breath, cough) are nonspecific and may be misinterpreted as signs of other more common and less severe conditions (eg, respiratory tract infection).
Arterial thromboembolism can lead to stroke, vascular occlusion, or myocardial infarction.
Symptoms of a stroke:
sudden weakness or loss of sensation in the face, limbs, especially on one side of the body, sudden confusion, problems with speech and understanding; sudden unilateral or bilateral vision loss; sudden disturbance in gait, dizziness, loss of balance or coordination; sudden, severe or prolonged headache for no apparent reason; loss of consciousness or fainting with or without a seizure.
Other signs of vascular occlusion:
sudden pain, swelling and slight cyanosis of the extremities, “acute” abdomen.
Symptoms of myocardial infarction:
pain, discomfort, pressure, heaviness, a feeling of compression or fullness in the chest or behind the sternum, radiating to the back, jaw, left upper limb, epigastric region; cold sweat, nausea, vomiting or dizziness, severe weakness, anxiety or shortness of breath; fast or irregular heartbeat.
Arterial thromboembolism can be life-threatening or fatal.
In women with a combination of several risk factors or high severity of one of them, the possibility of their mutual reinforcement should be considered. In such cases, the increased risk of blood clots may be higher. In this case, taking a combination of dienogest and estradiol valerate is contraindicated.
The risk of developing thrombosis (venous and/or arterial), thromboembolism or cerebrovascular disorders increases:
-with age;
- for smokers (with an increase in the number of cigarettes or an increase in age, the risk increases, especially in women over 35 years old);
in the presence of:
-obesity (body mass index 30 kg/m2 or more);
-family history (for example, venous or arterial thromboembolism ever in close relatives or parents under the age of 50 years). In the case of a hereditary or acquired predisposition, the woman should be examined by an appropriate specialist to decide on the possibility of taking a contraceptive;
- dislipoproteinemia;
- arterial hypertension;
-migraine;
- heart valve diseases;
- atrial fibrillation;
-prolonged immobilization, extensive surgery, any operation on the lower extremities or major trauma. In these cases, the drug must be stopped (in the case of a planned operation, at least four weeks before it) and not resumed for two weeks after the end of immobilization. Temporary immobilization (eg, air travel lasting more than 4 hours) may also be a risk factor for the development of VTE, especially in the presence of other risk factors.
The possible role of varicose veins and superficial thrombophlebitis in the development of VTE remains controversial.
The increased risk of thromboembolism in the postpartum period should be taken into account.
Peripheral circulatory disorders may also occur in diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn's disease or ulcerative colitis) and sickle cell anemia.
An increase in the frequency and severity of migraine during use of the drug (which may precede cerebrovascular disorders) is grounds for immediate discontinuation of the contraceptive.
Biochemical indicators indicating a hereditary or acquired predisposition to venous or arterial thrombosis include the following: resistance to activated protein C, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant).
When assessing the benefit-risk ratio, it should be taken into account that adequate treatment of the relevant condition may reduce the associated risk of thrombosis. It should also be taken into account that the risk of thrombosis and thromboembolism during pregnancy is higher than when taking low-dose COCs (<0.05 mg ethinyl estradiol).
Tumors
Preclinical data
Preclinical data obtained from routine repeated dose toxicity, genotoxicity, carcinogenic potential and reproductive toxicity studies do not indicate a specific risk to humans. However, it should be borne in mind that sex hormones can stimulate the growth of a number of hormone-dependent tissues and tumors.
The most significant risk factor for the development of cervical cancer (CC) is persistent human papillomavirus infection (PVI). There are reports of a slight increase in the risk of developing cervical cancer with long-term use of COCs, but the connection with COC use has not been proven. There is still controversy regarding the extent to which these data are influenced by various factors, in particular, cervical screening examinations or characteristics of a woman’s sexual behavior (number of sexual partners or less frequent use of barrier methods of contraception), as well as the cause-and-effect relationship of these factors.
According to a meta-analysis of the results of 54 epidemiological studies, a slight increase (1.24) in the risk of developing breast cancer in women taking COCs was found. The increased risk gradually disappears within 10 years after stopping COC use. Due to the fact that breast cancer is rare in women under 40 years of age, the increase in the number of breast cancer diagnoses in women who are currently taking COCs or have recently taken them is insignificant in relation to the overall risk of developing this disease. Its connection with COC use has not been proven. The observed increase in the risk of developing breast cancer may be due not only to earlier diagnosis of breast cancer, but also to the biological effect of sex hormones or a combination of these two factors. Women who have ever used COCs show earlier clinical stages of breast cancer than women who have never used them.
In rare cases, during the use of COCs, the development of benign, and in extremely rare cases, malignant liver tumors, which in some cases led to life-threatening intra-abdominal bleeding, was observed. If severe abdominal pain, liver enlargement, or signs of intra-abdominal bleeding occur, this should be taken into account when making a differential diagnosis.
Other states
Women with hypertriglyceridemia (or a family history of this condition) may have an increased risk of developing pancreatitis while taking COCs.
Although slight increases in blood pressure (BP) have been observed in many women taking COCs, clinically significant increases have rarely been observed. However, if a persistent clinically significant increase in blood pressure develops while taking a COC, you should stop taking the COC and begin treatment for hypertension. The drug can be resumed if normal blood pressure values are achieved with antihypertensive therapy.
The following conditions have been reported to develop or worsen both during pregnancy and while taking COCs, but their relationship with COC use has not been proven: jaundice and/or pruritus associated with cholestasis; formation of gallstones; porphyria; systemic lupus erythematosus; hemolytic-uremic syndrome; Sydenham's chorea, gestational herpes; hearing loss associated with otosclerosis.
Cases of worsening the course of endogenous depression, epilepsy, Crohn's disease and ulcerative colitis during the use of COCs have also been described.
In women with hereditary forms of angioedema, exogenous estrogens may cause or worsen symptoms of angioedema.
Acute or chronic liver dysfunction may require discontinuation of the contraceptive until liver function tests normalize. Recurrence of cholestatic jaundice, which developed for the first time during a previous pregnancy or previous use of sex hormones, requires discontinuation of COC use.
Although COCs may have an effect on insulin resistance and glucose tolerance, there is usually no need to adjust the dose of hypoglycemic drugs in diabetic patients using low-dose COCs (<0.05 mg ethinyl estradiol). However, women with diabetes mellitus should be closely monitored while taking COCs.
Because estrogens can cause fluid retention, women with chronic heart or kidney failure should also be under close medical supervision.
Chloasma can sometimes develop, especially in women with a history of pregnancy chloasma. Women with a tendency to chloasma should avoid prolonged exposure to the sun and exposure to ultraviolet radiation while taking the drug.
Effect on laboratory tests
Taking Qlaira® may affect the results of some laboratory tests, including biochemical parameters of liver, thyroid, adrenal and kidney function, the concentration of transport proteins in plasma, for example, DSG and lipid/lipoprotein fractions, parameters of carbohydrate metabolism and hemostasis. These changes usually remain within laboratory limits.
Medical examinations
Before starting (or resuming) taking a contraceptive, it is necessary to familiarize yourself with the woman’s life history, family history, conduct a thorough general medical examination (including measuring blood pressure, heart rate, determining BMI) and gynecological examination, including examination of the mammary glands and cytological examination of the cervix (for example, Papanicolaou test), pregnancy should be excluded.
It is important to draw a woman's attention to information about venous and arterial thrombosis, including information about the risk of taking Qlaira® compared to other COCs, symptoms of VTE and ATE, known risk factors and actions in case of suspected thrombosis.
The volume of additional studies and the frequency of follow-up examinations are determined individually, but at least once every 6 months.
It must be borne in mind that the drug does not protect against HIV infection (AIDS) and other sexually transmitted diseases!
Reduced efficiency
The effectiveness of the contraceptive drug may be reduced in the following cases: if you miss taking hormonal pills, gastrointestinal disorders while taking hormonal pills, or as a result of drug interactions.
Insufficient control of the menstrual cycle
While using the drug Qlaira®, especially in the first months of use, irregular menstrual-like bleeding (“spotting” or “breakthrough” uterine bleeding) may occur. Therefore, evaluation of any irregular menstrual-like bleeding should be carried out only after an adaptation period of approximately 3 menstrual-like cycles.
If irregular menstrual-like bleeding recurs or occurs for the first time after previous regular cycles, the possibility of non-hormonal causes should be considered and a thorough examination should be performed to exclude malignancy or pregnancy. Such measures may include diagnostic curettage.
Some women may not experience menstrual bleeding while taking hormone-free (white) pills. If the drug Qlaira® was taken in accordance with the recommendations specified in the section “Method of administration and dosage”, pregnancy is unlikely. However, if before the first absent menstrual bleeding the tablets were taken irregularly, or there are no 2 menstrual bleeding in a row, you should not continue to use the drug Qlaira® until pregnancy has been ruled out.
special instructions
The transition from Qlaira to the ring should take place after consultation with a gynecologist, since the amount of hormone in the ring is significantly less than what is contained in the tablets. In contrast, the body may not notice a small dose, as a result of which ovulation will occur unhindered.
After changing the type of contraceptive, even from one form of tablet to another, in the first 9 days of using the new product, it is strongly recommended to additionally protect yourself using a barrier method.