Causes
Despite numerous studies, the causes of gestosis remain completely unknown. It is believed that the main reason is the effect on the maternal body of foreign (paternal) components of the fertilized egg. Disturbances in the relationship between the central nervous system and internal organs play an important role in the development of the disease. Women with diseases of the gastrointestinal tract, liver, and asthenovegetative disorders are especially predisposed to the development of early gestosis. Psychogenic factors (negative emotions, fear for the outcome of pregnancy, family conflicts), as well as the undesirability of a real pregnancy or unpreparedness for it, have a significant influence on the appearance of symptoms of early gestosis in pregnant women.
In mild cases of gestosis, the concern is increased sensitivity to odors, nausea, and vomiting no more than 2-3 times a day, often on an empty stomach. In the case when vomiting occurs more than three times a day, appetite decreases, taste and olfactory sensations are disrupted, salivation can be 1 liter per day or more, body weight decreases, then early gestosis during pregnancy requires treatment.
The danger of gestosis when carrying a child
Preeclampsia is considered one of the serious complications of pregnancy, but it all depends on the stage. Naturally, at the onset of pathology, it is possible to stop the symptoms and normalize the condition, safely carrying the child to term. But, at an advanced stage, late toxicosis can be fatal for mother and baby.
Swelling spreads to the woman’s internal organs and can even affect the brain. It negatively affects the placenta, causes hypoxia and, in severe cases, the death of the child. In the event of such a threat, the woman in labor undergoes an emergency caesarean section.
Treatment
Treatment of mild gestosis is carried out on an outpatient basis, at home. For more severe forms, treatment is carried out in a hospital. First of all, non-drug treatment methods are used - physiotherapy, acupuncture, psychotherapy, electrosleep, hypnosis. Drug treatment of gestosis should be comprehensive. Drugs that normalize the function of the central nervous system and suppress the gag reflex are used. Intravenous infusions of saline solutions, glucose, and vitamins are performed. Usually up to 2-2.5 liters of solutions are administered per day. In some cases, medications are prescribed to replace regular meals. When treating pregnant women suffering from early gestosis, it is necessary to monitor biochemical blood parameters and urine tests. In rare cases, with excessive (so-called indomitable) vomiting, which is accompanied by general exhaustion, it is necessary to raise the question of terminating the pregnancy.
Recommendations from experts
Some advice for women who have symptoms of early gestosis:
- Listen to your taste desires, eat only what you want. Food should be easily digestible and contain enough vitamins;
- Eat small meals every 3-4 hours. For nausea, relief comes from chewing (dried fruits, nuts, crackers, salty crackers, lemon, etc.);
- If nausea begins in the morning, after getting up, then you can organize breakfast in bed. In any case, it is recommended to eat something - a piece of white bread or a roll, a cracker, sweet tea. Don’t rush to brush your teeth first thing after getting up!;
- It is recommended to eat dry: food separately, drinks by themselves. In some cases, mixtures and purees for baby food, protein mixtures for pregnant women (femilak, berlamin-modular, enipit) help. Be sure to include alkaline mineral water in your diet. The total amount of liquid drunk can be increased to 2-2.5 liters.
- If you are drooling, it is good to rinse your mouth with an infusion of mint, sage, and chamomile.
Why is late gestosis dangerous?
Late gestosis (late toxicosis) develops in the second half of pregnancy, after the 20th week and is manifested by edema, increased blood pressure and the appearance of protein in the urine. The reasons for the development of this pregnancy complication are not fully understood. According to one of the modern theories, the development of late gestosis is associated with the production of immune antibodies by the maternal body against the cells of the developing fetus. These antibodies have a damaging effect on the wall of blood vessels (primarily small vessels of the kidneys and placenta). As a result, the lumen of the vessels narrows, the blood flow through them slows down, and microthrombi appear in the bloodstream, which disrupt blood circulation in the vessels that supply blood to vital organs. Spasm of blood vessels and changes in the structure of their walls lead to the appearance of edema, increased blood pressure, and impaired renal and placental function. As a result, placental insufficiency develops, the growth and development of the fetus slows down, and the risk of hypoxia increases. The earlier the symptoms of late gestosis appear, the more severe it is and the more unfavorable the prognosis for both the mother and the fetus.
Preeclampsia is a severe complication of pregnancy that significantly increases maternal and infant morbidity and mortality.
According to statistics, in Russia, gestosis ranks third in the structure of maternal mortality, second only to extragenital diseases and bleeding. However, our studies (V.N. Serov et al., 1997, 2002) showed that with bleeding and sepsis, gestosis was the main cause of death in 35–40% of cases. In addition, while maternal mortality from hemorrhage and sepsis is decreasing, mortality from preeclampsia remains stable. In developed countries, gestosis is the leading cause of maternal mortality.
Perinatal mortality with gestosis exceeds the average by 5–7 times.
Preeclampsia (preeclampsia and eclampsia) is called a disease of theories, so they tried to explain the nature of this clinical syndrome with a variety of reasons - kidney damage, endocrine changes, immunological incompatibility, infections, autoimmune pathology, vascular and endothelial dysfunctions, etc. Each individual theory could not cover everything the diversity of the clinic, but many of the listed factors actually participate in the pathogenesis of disorders occurring during gestosis.
Hypovolemia, peripheral vascular spasm, changes in endothelial function, and hemostasis disorders are of greatest importance in the clinic of gestosis. According to V.N. Serov and N.M. Pasmana, etiologically this pathological condition is primarily determined by immunological and autoimmune disorders. It has been shown that the pathogenesis of preeclampsia fits into the systemic inflammatory response syndrome and, in severe cases, is characterized by multiple organ failure.
The frequency of gestosis, according to various authors (V.N. Serov and S.A. Markin, R.I. Shalina, E.M. Shifman), ranges from 5 to 20% in relation to all pregnancies. Such differences are due to different approaches to defining the very concept of “preeclampsia”.
Since the time of W. Zangemeister, this disease has been characterized by a triad of symptoms that develop after 20 weeks of pregnancy and include arterial hypertension, proteinuria and edema.
When assessing the clinical manifestations of gestosis, the main attention is paid to arterial hypertension, the degree of which underlies almost all modern classifications of preeclampsia (preeclampsia). In foreign literature, gestosis is most often referred to as arterial hypertension during pregnancy or preeclampsia.
The International Statistical Classification of Diseases (ICD-10, 1995) provides the following classification of edema, proteinuria and hypertensive disorders during pregnancy, childbirth and the postpartum period.
- Pre-existing hypertension complicating pregnancy, childbirth and the postpartum period.
- Pre-existing hypertension with associated proteinuria.
- Pregnancy-induced edema and proteinuria without hypertension. Pregnancy-induced hypertension without significant proteinuria. Pregnancy-induced hypertension with significant proteinuria – moderate to severe preeclampsia
- Eclampsia during pregnancy, childbirth, and the postpartum period.
Currently, the most commonly used classification of preeclampsia is the American Association of Obstetricians and Gynecologists, which formed the basis of the modern WHO classification (Table 1).
In Russia, the classification of gestosis presented in Table 2 has been adopted.
The main difference between the American and Russian classifications lies in the terms “preeclampsia” and “preeclampsia”. The American classification equates nephropathy with preeclampsia, increasing the alertness of the attending physician. At the same time, it distinguishes between mild and severe preeclampsia, as if blurring the line between them. Particular attention is paid to arterial hypertension, and hypertension that existed before pregnancy is clearly highlighted, which is an undoubted advantage of this classification. In general, the classification of the American Association of Obstetricians and Gynecologists is more consistent with the needs of practice, does not differ from that recommended by WHO and, apparently, will find wider application in our country.
The pathophysiology of preeclampsia deserves special attention, since rational therapeutic practice is impossible without knowledge of the changes occurring in the body of a pregnant woman during this pathological condition.
Preeclampsia is a syndrome that has a negative impact on all organs and systems of the mother’s body. The underlying pathophysiological mechanisms of preeclampsia are not fully understood, but it has been established that the most significant pathological processes occurring in the placenta, kidneys and brain are reduced to vascular endothelial disorders, and pathological changes are localized mainly in the placental area.
During normal pregnancy, the endothelium, internal elastic layer and muscular plates of the spiral arteries feeding the placenta are replaced by trophoblast and fibrin-containing amorphous matrix (F. Lyall and GA Greer, 1994). The changes that occur in this case cause a decrease in pressure in the vascular bed and additional blood flow, meeting the needs of the fetus and placenta.
Preeclampsia is characterized by the absence or incomplete penetration of trophoblast into the spiral arteries, which leads to a narrowing of their lumen and the subsequent development of placental ischemia. An altered placenta can provoke the formation of one or more factors that destroy vascular cells, causing dysfunction of many body systems (J. Roberts and CW Redman, 1993).
The endothelial cell performs a number of important functions, including regulation of fluid exchange, prevention of intravascular coagulation, changes in the contractility of smooth muscle walls, and maintenance of immune and anti-inflammatory status (SA Freidman et al., 1991).
When damaged, endothelial cells not only lose their regulatory function, but also produce procoagulants, vasoconstrictors and substances that cause transformation of lymphocytes. A pregnant woman with preeclampsia has increased capillary permeability and an excessive response to angiotensin. Increased sensitivity to the vasoconstrictor effect leads to widespread vasospasm and decreased organ perfusion. Prostocyclin production decreases, von Willebrand factor and fibronectin levels increase. Activated neutrophils serve as a source of substances that act as mediators of vascular oscillations that determine changes in blood pressure. It has been shown that accelerated formation of free radicals occurs in the blood of patients with preeclampsia, which in turn disrupts endothelial function (GA Dekker and AA Kraayenbrink, 1991).
The figure shows the changes that develop during preeclampsia in various organs. They indicate that preeclampsia can be characterized as a syndrome of multiple organ failure (V.N. Serov et al., 1997, 2002).
In recent years, it has been shown that with preeclampsia, along with multiple organ failure, a systemic inflammatory response syndrome develops with a characteristic change in the immune state, a cytokine cascade, hemostasis disorders and possible bacterial translocation (V.N. Serov et al., 2002).
A marker of endotoxemia in patients with preeclampsia can be the content of endotoxin, antiendotoxin antibodies, and medium mass molecules (MSM). Table 3 presents data confirming this (V.N. Serov, 2003).
As follows from the data presented in the table, depending on the severity of preeclampsia, the endotoxin level increases in parallel with an increase in the MSM content and a decrease in the level of anti-endotoxin antibodies. Increased endotoxin production induces the release of tumor necrosis factor and the cytokine cascade. Repeated stimulation of cytokines can significantly increase multiple organ failure, disorders of hemostasis, respiratory processes and enzymatic reactions.
In recent years, new data have been obtained on the most severe forms of preeclampsia. It has been found that in the presence of antiphospholipid syndrome or the presence of antiphospholipid antibodies, preeclampsia is especially severe.
With autoimmune pathology, especially forms of preeclampsia develop - HELLP syndrome and acute fatty hepatosis. It seems that autoimmune disorders are a factor that predetermines the development of the most severe complications in gestosis.
Diagnosis of preeclampsia, at first glance, is simple: determining high blood pressure, the presence of edema and proteinuria is not difficult. However, the main thing in diagnosis is determining the severity of gestosis and prognosis of the development of the pathological process. This is due to the main problem - whether it is possible to continue the pregnancy or whether it is necessary to terminate it, regardless of the consequences for the fetus. In severe preeclampsia (see classification in Table 1) or after an attack of eclampsia, treatment tactics consist of relatively short-term intensive preparation for delivery: by cesarean section in an unprepared birth canal or through the natural birth canal.
In cases where preeclampsia can be assessed as moderate severity, and the condition of the fetus in terms of gestational age requires prolongation of pregnancy, conservative tactics can be chosen. However, in such a situation, it is impossible to exclude the progression of preeclampsia and the development of multiple organ disorders in the form of multiple hemorrhages in the liver, lungs and brain, cerebral edema and ischemia, acute renal failure, an attack or attacks of eclampsia with a sharp worsening of the general condition, cerebral coma, pulmonary edema and even fatal.
Thus, the doctor is faced with a dilemma: by stopping the development of pregnancy, the woman’s health can most likely be preserved, but the child, especially a very premature one, may suffer.
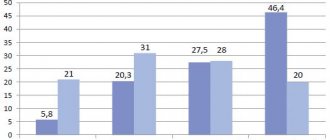
In the literature you can find numerous references to various clinical, biophysical and biochemical studies that help predict the development of preeclampsia (GA Dekker and AA Kraayenbrink, 1991). However, in most cases, their results are quite contradictory. At the present stage, there is no ideal prognostic method that meets all the necessary criteria. As before, the prognosis continues to be mainly based on the absence or presence of childbirth in the woman’s history and family history. Preeclampsia is diagnosed in 5.8% of first pregnancies and only 0.4% of second pregnancies (JM Roberts and CW Redman, 1993).
Doppler ultrasound examination of the deep arcuate arteries at 16–18 weeks of gestation may be useful in identifying abnormalities associated with trophoblast invasion of the spiral arteries, and also has some value in predicting pregnancies at risk for complications due to preeclampsia (SA Steel et al. , 1990).
Due to the lack of comprehensive information about the etiology and pathophysiology of preeclampsia, the development of effective preventive measures is difficult. It was assumed that aspirin may be effective in preventing preeclampsia, but this hypothesis could not be confirmed in numerous studies (BM Sibai and SN Caritis, 1993). On the other hand, calcium supplementation has been shown to achieve some reduction in the incidence of hypertension, preeclampsia and preterm birth (GP Waisman and LM Mayorga, 1988). Attention is drawn to the absence of preeclampsia in pregnant women with a transplanted kidney during treatment with glucocorticoids and cytostatics (L.E. Murashko and A.I. Volobuev, 2002).
Currently, therapy for preeclampsia is based on the treatment of symptoms and signs of its secondary manifestations, with the goal of reducing the incidence of complications from the mother and fetus. It should be remembered that obstetric tactics and determining the optimal timing of delivery are still important.
Severe preeclampsia or full-term pregnancy are indications for delivery.
In preparation for termination of pregnancy, it is necessary to carry out antihypertensive, infusion and anticonvulsant therapy. Antihypertensive drugs used for severe preeclampsia are presented in Table 4.
Anticonvulsant therapy is carried out mainly with the help of magnesium sulfate, the mechanisms of action of which are not fully understood. This drug is expected to have positive effects in conditions of cerebral vasospasm.
Intravenous administration of magnesium sulfate involves a loading dose of 4–6 g (16–24 ml of a 25% solution over 20 minutes). Its maintenance dose is 2 g/hour (80 ml of a 25% solution (20 g) in 500 ml of 0.9% sodium chloride solution or 5% glucose solution. The rate of administration is 50 ml/hour (16 drops/min).
With intramuscular injection of magnesium into the joint, the loading dose is 10 g (5 g - 20 ml of a 25% solution in each buttock), the maintenance dose is 5 g every 4 hours.
Infusion therapy should be low-volume - 800-1200 ml, preferably carried out under the control of venous pressure. For cerebral edema, infusion therapy is advisable if the following conditions are met: small volume, a combination of crystalloids and colloids, the use of large-molecular hydroxyethyl starches (for example, Stabizol) and hypertonic saline solutions (E.M. Shifman and A.D. Tikanadze).
Preeclampsia of moderate severity (nephropathy) allows you to prolong pregnancy until the term of the full-term fetus (36 weeks). Treatment is based on antihypertensive, infusion and anticonvulsant therapy.
Calcium channel blockers (nifedipine, amlodipine), clonidine, methyldopa and labetalol are used as antihypertensive drugs. The use of angiotensin-converting enzyme inhibitors and diuretics is not recommended.
It is advisable to carry out infusion therapy using hydroxyethyl starch preparations, the prescription of which is especially justified in conditions of generalized endothelial damage.
According to our data (V.N. Serov et al., 1999), the use of 10% hydroxyethyl starch (Infucol) contributed to the prolongation of pregnancy in preeclampsia and reduced perinatal mortality by 1.5–2 times.
When infusion therapy was insufficiently effective, we used plasmapheresis. To reduce the level of endogenous intoxication, assessed by endotoxemia, the content of MSM and anti-endotoxin antibodies, entero- and hemosorption were used. Enterosgel sorbent was prescribed 3 times a day for 2 weeks in combination with antihypertensive and infusion therapy. Observations included 40 patients with moderate gestosis (preeclampsia). Of these, early termination of pregnancy was required in only 2 cases, while in the control group, early labor had to be induced in every third patient.
The dynamics of endotoxin and MSM concentrations after enterosorption and hemosorption are presented in Table 5.
Thus, despite certain successes achieved, the treatment of gestosis (preeclampsia) remains a rather difficult task. Further research is needed to determine the exact mechanisms of etiopathogenesis of this disease, which will contribute to the development of effective methods for its prevention and treatment.
How does gestosis occur?
The disease usually begins with swelling of the lower extremities (it is difficult to put on usual shoes), then there is morning stiffness and swelling of the hands (it is difficult to remove a ring from a finger), swelling in the abdomen (a mark from underwear remains) and, finally, puffiness of the face. When measuring blood pressure, attention is drawn to the asymmetry of blood pressure numbers on the left and right arms. If this stage of gestosis is not treated, blood pressure rises, protein appears in the urine, and swelling becomes more noticeable. Pressure above 135/85 mm Hg during pregnancy is elevated; when the diastolic (lower) pressure is 95 mm Hg, persistent spasm of the placental vessels develops and the conditions for fetal development are disrupted, and the diastolic blood pressure is above 110 mm Hg. Not only is it dangerous to the life of the fetus, but it can cause serious complications for the mother.
The peculiarity of late gestosis is that expectant mothers do not worry about anything for a long time in the presence of the disease. They often do not follow doctor's recommendations and are reluctant to go to hospital for treatment. And in vain. If the disease is not treated in the early stages, it progresses to more severe stages - preeclampsia and eclampsia. Against the background of high blood pressure, edema and high protein content in the urine (more than 1 g/l in a single portion of urine), a pregnant woman develops headache, nausea, vomiting, and visual disturbances (“flies flash before the eyes”). These are symptoms of developing cerebral edema. If the woman is not given medical assistance at this stage, her condition will quickly deteriorate and eclampsia will develop. A pregnant woman suddenly develops convulsions and loss of consciousness. Preeclampsia and eclampsia can result in severe complications - cerebral hemorrhage, placental abruption, intrauterine fetal death, retinal detachment, massive bleeding. Treatment of severe forms of late gestosis is carried out only in the maternity hospital. After stabilization of the pregnant woman's condition, it is usually necessary to carry out a gentle delivery.
Stages of pathology
Preeclampsia is classified as follows:
- Dropsy
- swelling in the arms and legs. But this is not only a sign of this pathology, so it is necessary to undergo tests to confirm. - Nephropathy
- high blood pressure is added to swelling. Already at this stage there is a danger to the woman’s life and she needs to urgently consult a doctor. The complication can quickly develop into another lethal form. - Preeclampsia
- the blood flow of the central nervous system is disrupted, at the same time nausea, high blood pressure, insomnia, migraine, protein in urine are observed. It is quite possible that there is a mental disorder due to pathology. - Eclampsia
requires urgent medical intervention. Convulsions are added to the previous symptoms, stroke, coma and death are possible. The placenta rapidly ages, and the baby may die.
Any form of gestosis poses a danger to the baby: it provokes hypoxia, lack of nutrition, and disrupts blood flow.
Unfortunately, gestosis begins unnoticed, but develops rapidly and moves from one stage to another, so doctors prescribe additional tests at the first sign.
Prevention of gestosis
Prevention of late gestosis consists of creating the correct work and rest regime for the pregnant woman. It is necessary to protect the pregnant woman from working on the night shift; when the first signs of the disease appear, she should be released from work altogether and a protective regime should be created, ensuring a calm emotional state for the pregnant woman. Decoctions of soothing herbs (motherwort, valerian), complex herbal preparations - persen, novapassit, sanosan; preparations containing magnesium ions - MagneB6, Magnelis or Magnerot. You should not significantly limit the amount of liquid you drink; it is better to drink green tea, rosehip decoctions and mineral water. For edema, diuretic preparations containing lingonberry leaf, bearberry and others are recommended.
If edema increases, blood pressure increases, or protein appears in the urine, treatment must be carried out in a hospital setting.