Overactive bladder (OAB) is a widespread problem affecting hundreds of millions of people worldwide.
The total cost of treating such patients amounts to tens of billions of dollars in America alone. Thirty percent of all men and 40 percent of all women in the United States live with symptoms of OAB.
But the number of people suffering and not seeking medical help is likely much higher. Firstly, patients are embarrassed. They don't know how to talk to their doctor about their symptoms. Others don't go to doctors because they think there is no cure for the problem.
If you suspect that you have a health problem, you should under no circumstances wait for improvements, but urgently need to consult with urologists. OAB significantly worsens the quality of life of patients. You need to know that there is a treatment for these disorders and not let the symptoms of OAB ruin your life.
What is overactive bladder and how does it manifest?
Overactive bladder is not a disease. This is a collective concept (syndrome), which includes a complex of urinary symptoms.
The main symptom is a sudden strong urge (imperative or commanding urge) to urinate that you cannot control. At the same time, patients note that in most cases they are unable to run to the toilet and may leak urine (incontinence)
If you live with this problem you very often experience:
- Urine leakage (incontinence): Very often, people with an overactive bladder experience urge incontinence, which is the inability to hold urine after a strong urge to urinate. It is necessary to distinguish this condition from stress urinary incontinence. Women with stress urinary incontinence experience urine leakage when sneezing, laughing, or physical activity.
- Frequent urination: On average, you have to run to the toilet more than eight times a day.
- Nighttime urination (nocturia): Having this symptom more than once is another characteristic sign of an overactive bladder.
This syndrome represents urinary disorders of central and peripheral origin, such as frequent urges during the day and even at night, difficult to control, leading to urinary incontinence. This syndrome is a so-called diagnosis of exclusion, a functional disorder, since one of the diagnostic criteria is the absence of infection and other organic pathology of the urinary system.
The prevalence of “overactive bladder” has recently been increasing, which may be due to the psychogenic cause of the pathology. The disease occurs equally often among men and women of different age groups, but the peak incidence occurs in old age. The main complication of a long-term disease is the development of neurosis-like or borderline mental disorders - somatoform disorders, hypochondria, depression, anxiety-phobic neurosis, obsessive-compulsive neurosis and other pathologies that seriously disrupt the adaptation of patients in all spheres of life. It can be assumed that mental disorders are not only supporting factors, but also predisposing to this syndrome.
Currently, there are several theories that prove the neurogenic cause of this disease (various disorders in the nervous system), but they do not explain all cases of the disease. If it is impossible to determine the cause, then in medicine it is customary to use the concept “idiopathic” - which means the cause of any disease or syndrome has not been established to date.
The neurogenic theory implies any disorder in the central or peripheral nervous system, which leads to disruption of the regulation of the urination process (stroke or other pathological lesions in certain parts of the brain, damage to nerve pathways, multiple sclerosis). Increased excitability of muscle and epithelial tissue is also noted, but as already mentioned, these reasons cannot explain all cases. Predisposing factors include age (the risk of pathology increases with age), smoking, obesity, poor diet, hormonal changes, and mental stress.
Symptoms of “overactive bladder” are mainly associated with disturbances in the urination process and are represented by the following options:
- pollakiuria (frequent urge to urinate)
- nocturia (night urination, which requires a special interruption of sleep to go to the toilet, which is not normally typical for a healthy body)
-enuresis (severe urge to urinate, which is accompanied by urinary incontinence)
All these symptoms are characterized by suddenness, because most often they occur when the bladder is not full.
If you suspect overactive bladder syndrome, you should seek help from a urologist, who may additionally prescribe a consultation with a neurologist and a gynecologist.
A large number of different methods are used for diagnosis, because functional diseases are difficult to diagnose precisely because to establish them it is necessary to exclude other causes. To identify characteristic complaints, the doctor can use specially designed questionnaires. The examination in most cases is of no diagnostic value, but should be carried out in all patients. Laboratory diagnostics includes studies such as general and bacteriological urine tests, general and biochemical blood tests. It is important to properly conduct a neurological examination, which can identify the neurogenic cause of the disease and refer the patient to a neurologist.
Since many diseases of the urinary system can be accompanied by similar symptoms, it is necessary to conduct a thorough examination to identify them. One of these methods is cystoscopy - insertion of a cystoscope into the cavity of the bladder, which allows you to directly see and evaluate the condition of the mucous membrane of the bladder. Indirect visualization methods - ultrasound, CT, MRI - are of indirect importance. Urodynamic studies make it possible to identify characteristic symptoms and judge the mechanisms of developed disorders. The absence of any disorders in the urinary system gives grounds to make a diagnosis of “Overactive Bladder”.
For treatment, non-drug means such as behavioral therapy (so-called psychotherapy) and maintaining the correct “water” regime are used.
Among the medications, you can use anticholinesterase drugs (blockers of the effects of the parasympathetic nervous system), beta-adrenergic receptor agonists (activate the effects of the sympathetic nervous system) - both groups of drugs allow you to relax the muscle - the detrusor of the bladder (the muscle that promotes urination). The drug desmopressin is used only as indicated in patients with diabetes insipidus and nocturnal enuresis. Neuromodulation methods and the introduction of special blocking drugs into the detrusor (bladder muscle) are used in patients resistant to therapy with the above drugs.
Causes of overactive bladder and who is at risk?
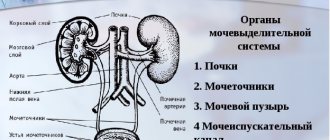
In healthy people, if the bladder is not full, it is in a relaxed state. When nerve signals from the brain indicate that the bladder is full, the urge to urinate occurs. The bladder muscles then contract and expel urine through the urethra (urethra). The urethra has muscles called the sphincter. Due to them, the urethra opens and closes and thus urine does not flow out without our willingness to go to the toilet.
Patients with overactive bladder receive false nerve signals from the brain to the bladder, even when the bladder is not full.
One reason is increased activity of the bladder muscles.
Risk: As you get older, your risk of developing OAB symptoms also increases, regardless of gender. Women who have gone through menopause and men who have had prostate problems are at risk of developing an overactive bladder. In addition, people with neurological diseases such as stroke and multiple sclerosis are also at high risk of developing OAB.
Bladder-irritating foods and drinks (caffeine, alcohol, spicy, hot, sour) contribute to increased symptoms in some patients.
Diagnostics: how it goes, what procedures are performed
Diagnosis of overactive bladder syndrome begins with informing the doctor about the patient’s complaints and medical history. One of the key elements of diagnosis is the analysis of the number of urinations during the day and at night. Monitoring is carried out using the patient's diary, in which it is necessary to enter data on urination for three days.
A diagnosis of pathology in the bladder is made if the patient urinates more than 8 times a day, with uncontrollable urges occurring at least twice a day. The doctor also prescribes laboratory tests, which include the following studies to determine the causes of the pathological condition:
- bacteriological tests to detect the presence of infection in the genitourinary system;
- cystoscopy and urethroscopy;
- Ultrasound, which examines the kidneys, bladder, and prostate gland.
Through these procedures, during an outpatient examination, the doctor identifies various pathologies of the genitourinary system that arise along with the symptoms that characterize an overactive bladder. In order to fully confirm the diagnosis and prescribe appropriate treatment, a urodynamic analysis with fullness cystometry is performed. That is, the Doctor records an increase in detrusor pressure during urgency when the bladder is full.
It is also necessary to inform the specialist about the medications you are taking, since some of them may worsen the symptoms of incontinence.
It is necessary to come for diagnostics with a slightly full bladder, since this way a more detailed ultrasound examination can be carried out, on the basis of which effective treatment will be prescribed. It is also recommended that you first fill out a urination diary for three days, which will allow the doctor to get a complete picture of the patient’s medical history. The following data must be entered into the diary: volume of urine, muscle tension during urination, degree of leakage and intolerance of urge, volume of fluid drunk.
How to diagnose an overactive bladder?
To begin with, the doctor needs information about your past and current health problems, what symptoms you have had and how long they have bothered you, what medications you take, and how much fluid you drink during the day.
Urologists perform examinations aimed at finding out the causes of your complaints, and also assess the condition of the pelvic organs and rectum in women and the prostate and rectum in men.
It is necessary to conduct ultrasound diagnostics of the pelvic organs in order to exclude concomitant diseases of the bladder and determine residual urine.
Laboratory tests of urine are performed to rule out inflammation and infection of the bladder.
It is recommended to keep a voiding diary to learn more about your symptoms.
Causes
This condition can be provoked by neurogenic or other causes that require timely treatment. The first category includes the following:
- the main reason is brain disorders and pathologies (sclerosis, encephalitis, malignant tumors, Alzheimer's disease);
- diabetes;
- alcohol abuse;
- traumatic brain injury, stroke;
- congenital pathologies.
Other reasons include age-related changes, concomitant pathologies of the genitourinary organs, anatomical structure of organs, and hormonal imbalances. Also, patients who experience stress and depression, disorders, intestinal pathology with irritated mucosa, may suffer from bladder diseases, for which drug treatment is inevitable.
With this disease, the patient experiences general discomfort as sleep disorders, depressive states, and various urinary tract infections develop. Therefore, if even the slightest symptoms are detected, you need to visit a qualified specialist who will prescribe effective medications depending on the causes of the pathology.
Treatment methods
There are several options to help you manage your bladder. These include:
Behavioral therapy: Often the first meaningful steps towards treatment. The patient can and should make some changes to his lifestyle and diet (avoiding caffeine, alcohol and spicy foods).
Quitting smoking and losing excess weight can also improve the patient's condition. Your healthcare provider may ask you to keep a daily voiding diary to track your trips to the toilet. Behavioral changes may include going to the bathroom on a schedule throughout the day and doing "quick motion" Kegel exercises to relax the bladder and pelvic floor muscles. Unfortunately, most patients will not be able to get rid of their symptoms completely with lifestyle changes. But many of them note a reduction in symptoms with this type of treatment.
Medication: There are several medications available to relax the bladder muscles. Patients are prescribed medications in tablet form. Some drugs are used in the form of skin gels or patches.
Neuromodulation therapy: Professionals use this harmless treatment method only for a subset of patients in whom drug and behavioral therapies do not work or when patients have serious side effects from medications.
Botox injections: Some experts believe that botulinum toxin injections, better known as Botox®, can help patients who do not respond to other treatments.
Which doctor should I contact?
For treatment of a disease such as overactive bladder, it is necessary to contact a urologist who can conduct qualified diagnostics and establish a competent diagnosis, taking into account the causes and symptoms of the disease that the patient has. It is wrong to contact a gynecologist with this disease, since this specialist can only indirectly treat the pathology, but will not be able to prescribe competent treatment.
It is often necessary to initially visit a therapist, who will refer you to a specialist who treats a specific problem. Patients can undergo examination at the JSC Meditsina clinic in Moscow, where qualified specialists work to help cope with problems of varying severity. On the clinic’s website, visitors can get acquainted with the doctors who see them, their certificates and specialization.
Indications for the disease
To prevent and effectively treat overactive bladder, you must follow certain recommendations:
- give up strong coffee and tea, carbonated water, since these drinks irritate the organs of the genitourinary system;
- If you have frequent urges at night, it is recommended to stop drinking liquids 3 hours before bedtime. However, the daily fluid intake must be met;
- if the patient has an overactive bladder, it is necessary to completely empty the organ when urinating to the maximum, which will reduce the urge to further frequent visits to the toilet;
- for incontinence, it is recommended to use pads or diapers for adults, which will allow you to maintain personal hygiene and save people from inhaling an unpleasant odor;
- Doing Kegel exercises will help relax your pelvic floor muscles and make your overactive bladder less of a problem. It is necessary to perform gymnastics several times a day to achieve significant effectiveness of treatment.
An important aspect that allows you to effectively treat an overactive bladder is maintaining normal body weight and following a diet, adhering to the principles of a healthy diet. As practice shows, with a weight loss of 5-10%, the manifestations of diseases of the genitourinary system are significantly reduced, since significantly less pressure is placed on the bladder.
OAB in children
The problem of OAB is not related to the age category, and children quite often outgrow this condition upon reaching seven years of age. If we are talking about incontinence or excessively frequent urinary processes in a child under three years old, this phenomenon should be treated as completely normal and not a problem.
Let's consider what factors can provoke an overactive bladder in children:
- Development of infectious processes in the urinary tract.
- Presence of neurological diseases.
- Development of acute or chronic constipation.
- The occurrence of stressful situations, especially if they are associated with the urination process.
- Inability to go to the toilet for a long time.
- Overactive bladder syndrome occurs when the capacity of the organ is not large enough.
- Presence of foods containing caffeine in the diet. This applies to chocolate, sweet carbonated waters and tea.
- Structural changes affecting the organs of the urinary system.
An allergic reaction to certain foods and irritation of the organ lining can have a negative impact. According to foreign statistics, after a child turns five years old, cases of OAB in this age category decrease, this figure reaches about 15%. As children grow older, they acquire the ability to respond in a timely manner to signals sent by the body indicating the need to go to the toilet.
Treatment: modern techniques
Several treatment approaches have been developed. The chosen technique depends on how severe the symptoms are and the stage of the disease.
For mild symptoms, exercises can be used as prevention and treatment to train the bladder muscles so that the patient can control urge and urination. The main goal of such exercises is to go to the toilet less often due to the fact that the muscles will be able to hold an increased amount of urine. The training includes two stages: going to the toilet if necessary in the morning and practicing urinary control throughout the day.
At the first stage of treatment, the patient learns to control urges and tries to visit the toilet at increased intervals. So, if previously the patient went to the toilet every half hour, the time gradually increases to 45 minutes or an hour. If you have a strong and uncontrollable urge to urinate when your bladder is empty, you can perform Kegel exercises by contracting your muscles. It is necessary to gradually increase the intervals between urinations. The norm is to visit the toilet 4-5 times during the day and once at night.
Contraindications for illness
When treating the syndrome it is necessary:
- stop eating citrus fruits, pineapples, chocolate, sweets, spicy and sour foods, dairy products, since these products cause irritation to the mucous membrane of the genitourinary system;
- avoid excessive consumption of water and any liquid in general; excessive reduction of the daily water intake is also contraindicated;
- Minimize the consumption of alcohol and energy drinks.
By following these recommendations, you can cope with hyperactivity syndrome, reduce pain to a minimum and increase the effectiveness of drug treatment.
Pathogenesis
Most authors associate the pathogenesis of the disease with ischemic changes in the detrusor that occur due to atherosclerosis or bladder outlet obstruction. When the blood circulation in the detrusor is impaired, postsynaptic denervation occurs and subsequent structural changes occur in the intercellular junction of myocytes. The above-described structural changes are one of the main reasons for the formation of detrusor hyperactivity, which is manifested by frequent and urgent urination.
A long-term and detailed study of the structure of the mucous membrane of the bladder led to the conclusion that even minor changes and formations affect the regulatory function of the bladder.
Tests and diagnostics
The diagnosis is established by a urologist based on data from anamnesis, physical examination, and the results of instrumental and laboratory diagnostics.
The patient is required to fill out a urination diary and a special questionnaire. In certain cases, additional consultation with a gynecologist and neurologist is required.
Patient examination algorithm:
- Lab tests . If a general urine test reveals bacteriuria or leukocyturia , then an additional culture is prescribed to identify the pathogen, and subsequently to determine the sensitivity of the microorganism to antibiotics and antimicrobial agents. To exclude a neoplastic process when a large number of red blood cells are detected, a cytological examination is indicated. Glucosuria is also performed to exclude diabetes mellitus .
- Instrumental diagnostics. The examination plan includes the following research methods: cystoscopy; ultrasound examination of the urinary tract with mandatory monitoring of residual urine volume; complex urodynamic study.
It is necessary to carry out differential diagnosis with diseases such as:
- vesicovaginal fistula;
- atrophic vaginitis with decreased estrogen levels;
- malignant and benign neoplasms ;
- urolithiasis disease;
- uterine prolapse.
Advantages of treatment at the clinic of JSC "Medicine"
Treatment in the hospital of the clinic of JSC "Medicine" takes place in comfortable conditions - patients are provided with rooms with all amenities.
The competitive advantage that the clinic has is cooperation with insurance companies. The modern clinic provides medical services at the highest professional level, providing effective treatment for patients even with complex forms of the disease.
Treatment and diagnostics are carried out by qualified specialists of our clinic using modern equipment, using effective medications, in order to completely relieve patients from pain and discomfort.
Main causes of the disease
There are two main types of GMF:
- With increased detrusor tone (with neurological pathology);
- Ideopathic detrusor instability (various causes).
However, there is no doubt that other health problems or medications you are taking can also cause symptoms of hyperactivity. To find out the exact cause of the disease, you should make an appointment with a specialist who, with the help of examinations and tests, can prescribe appropriate treatment.
In a normal bladder condition, a person should urinate no more than eight times. In this case, the daily amount of fluid released is about two liters. But in the case of the development of various pathologies, these parameters can change. In the case of an overactive organ, trips to the toilet become more frequent, but the volume of discharge does not change. But the size of each portion becomes different. As a rule, the impetus for the development of OAB is given by increased conductivity of impulses in those muscles that are located around it. As a result, even slight irritation of the organ’s receptors provokes muscle contraction and the desire to empty the bladder. This condition occurs as a result of neurogenic or non-neurogenic factors. The first include:
- Pathologies of the brain of the head or back, the list includes multiple sclerosis, Alzheimer's and Parkinson's diseases, various neoplasms and encephalitis. The cause of an overactive bladder can be alcoholic, diabetic neuropathy.
- Injuries and damage to the spinal cord and brain - these can be compression ruptures, results of surgery and stroke.
- Birth defects affecting the spinal cord.
- Congenital pathologies of the bladder.
Non-neurogenic factors include age, diseases developing in the genitourinary area, anatomical features and sensory disorders, in which changes in hormonal levels and the sensitivity of bladder receptors are observed against the background of atrophy of the mucous layer. Those who suffer from depression, fibromyalgia, irritable bowel syndrome and attention disorders are often prone to developing an overactive organ. The development of the pathological condition is accompanied by a number of unpleasant phenomena; the symptoms of OAB and treatment are closely related:
- Sleep may become worse.
- Quite often, infectious processes begin to develop in the urinary tract.
- Pollakiuria – increased frequency of urination – may be observed.
- Nocturia, in which urination occurs at night.
- The urge to urinate becomes urgent, in other words, urgent. This urge can last for several seconds or minutes.
- Optional but possible symptoms include urge urinary incontinence.
Important. The main problem is that these symptoms can occur in a patient regardless of the time of day or place. Accordingly, there is a noticeable deterioration in his quality of life.
OAB in men
Overactive bladder, according to various sources, occurs in 15-16 percent of men, and symptoms of the disease more often appear with age.
One of the most common causes of OAB symptoms in men is an enlarged prostate. The prostate may simply increase in size as you age, or it may be a sign of a serious disease, such as prostate cancer. If the prostate becomes large enough, it interferes with the flow of urine from the urethra. In addition, hyperactivity occurs due to a number of other factors:
- Urinary tract infections;
- Prostate and bladder stones;
- Uncontrolled diabetes;
- Poor nutrition and sedentary lifestyle;
- Taking certain types of medications (caffeine, diuretics;)
- Neurological conditions such as Parkinson's disease, etc.
Symptoms of OAB can affect every aspect of a person's life. People usually perceive this problem as personal, so they often do not seek medical help until the last minute. The doctors at our clinic understand the sensitivity of this problem and will provide the most comfortable treatment possible. Fortunately, there are several effective treatments available.
Overactive bladder in women
Clinical symptoms largely depend on the severity of the process. Patients complain of frequent urination in small portions when the bladder is not yet full. Urgent incontinence and imperative urges are recorded. Women visit the toilet more than twice a night.
The desire to visit the toilet arises in response to the sound of pouring liquid. With a mild degree of severity of the disease, a woman loses only a few drops of urine, and with a severe form of the pathology, the entire volume. Nocturia and pollakiuria may be present in isolation. In some cases, immediately after urination, a feeling of discomfort in the perineum persists.