Galantamine
Galantamine is administered intravenously, intramuscularly, subcutaneously, transdermally (by iontophoresis), orally in tablets.
The dose is selected individually, taking into account the patient’s age, the nature of the disease, the effectiveness and tolerability of the drug. At the beginning of treatment, the minimum effective dose is prescribed, gradually increasing it. Orally, the maximum daily dose for adults is 10-40 mg in 2-4 divided doses. For myasthenia gravis
The daily dose is divided into 3 doses. When treating dementia of the Alzheimer's type, the recommended initial dose is 8 mg per day - 4 mg 2 times a day, after 4 weeks they switch to a maintenance dose - 16 mg (8 mg 2 times a day), which is taken for at least 4 weeks. The question of increasing the maintenance dose to the maximum (24 mg per day) must be decided after assessing the clinical situation (the achieved effect and tolerability). When switching from a drug in the form of tablets, taken 2 times a day, to a dosage form in the form of extended-release capsules, taken 1 time per day, the total daily dose should remain unchanged.
Subcutaneously, adults: 2.5-10 mg 1-2 times a day, maximum single and daily doses of 10 mg and 20 mg, respectively. Subcutaneously, children: 1-2 times a day, at the age of 1-2 years - 0.25-1.0 mg per day, 3-5 years - 0.5-5.0 mg per day, 6-8 years - 0.75-7.5 mg per day, 9-11 years - 1.0-10.0 mg per day, 12-15 years - 1.25-12.5 mg per day, 15-16 years - 12 .5-20.0 mg per day. The larger dose is divided into 2 injections per day.
The duration of treatment depends on the nature and severity of the disease, most often - 40-60 days, the course of treatment can be carried out 2-3 times with intermediate periods of 1-2 months.
Intravenously, as an antagonist of antidepolarizing muscle relaxants: adults - 10-20 mg per day, children from 1 year - 1-2 mg, 3-5 years - 1.5-3 mg, 6-8 years - 2-5 mg, 9-11 years old - 3-8 mg, 12-15 years old - 5-10 mg.
Intramuscularly, for X-ray studies, it is used in adults at a dose of 1-5 mg. For diseases of the peripheral nervous system and for the treatment of bedwetting, it is used in children in the form of iontophoresis in a dose of 1-2 ml of a 0.25% solution.
Use in elderly patients
Use in the elderly has not been systematically studied. Due to the large number of contraindications that are most applicable to older people (for example, chronic heart failure or long-term use of beta blockers), careful examination and subsequent active monitoring of the condition of such patients is necessary.
Use in children
Application is possible according to the dosage regimen. Contraindicated in children under 1 year of age (for solution), under 9 years of age (for tablets).
Galantamine Canon (capsules) 8mg, 16mg, 24mg
Pharmacodynamics
Galantamine (tertiary alkaloid) is a selective, competitive and reversible inhibitor of acetylcholinesterase. In addition, galantamine enhances the effect of acetylcholine on nicotinic receptors, probably due to binding to the allosteric site of the receptor. By increasing the activity of the cholinergic system, cognitive function may improve in patients with dementia of the Alzheimer's type.
Pharmacokinetics
Galantamine is a basic compound with a single dissociation constant (pKa 8.2). It has weak lipophilicity with a distribution coefficient (LogP) between n-octanol and a buffer solution (pH 12) of 1.09. Solubility in water (pH 6) is 31 mg/ml. Galantamine has 3 chiral centers. S, R, S-configuration is natural (natural). Galantamine is partially metabolized by various cytochromes, mainly the isoenzymes CYP2D6 and CYP3A4. Some of the metabolites formed during the degradation of galantamine are active in vitro, but are not significant in vivo.
Suction
The absolute bioavailability of galantamine when taken orally is high - 88.5 ± 5.4%. The area under the concentration-time curve (AUC24h) and the minimum concentration (Cmin) in plasma are similar to those when taking immediate-release galantamine twice a day. The maximum concentration (Cmax) in the blood plasma is reached after 4.4 hours. The Cmax of extended-release galantamine is 24% lower than after taking immediate-release galantamine. Food intake does not have a significant effect on AUC, but causes an increase in Cmax by approximately 12% and an extension of the time to reach Cmax (TCmax) by approximately 30 minutes. However, these changes are not clinically significant.
Distribution
The average volume of distribution (Vd) is 175 l. The degree of binding to plasma proteins is low and amounts to (18%).
Metabolism
In vitro studies have shown that the main isoenzymes of the cytochrome P450 system involved in the biotransformation of galantamine are CYP2D6 and CYP3A4. The CYP2D6 isoenzyme is involved in the formation of O-desmethylgalantamine, and the CYP3A4 isoenzyme is involved in the formation of N-oxide-galantamine. Excretion of the radioactive dose by the kidneys and through the intestines does not differ in patients with “slow” and “fast” metabolism (low and high activity of the CYP2D6 isoenzyme, respectively). In the blood plasma of patients with “fast” and “slow” metabolism, the main part of the radioactive substances consists of unchanged galantamine and its glucuronide. After a single dose of galantamine, none of the active metabolites of galantamine (norgalantamine, O-desmethylgalantamine and O-desmethylnorgalantamine) were detected in unconjugated form in the blood plasma of patients with “fast” and “slow” metabolizers. Norgalantamine was detected in the blood plasma of patients after long-term use of the drug, and its concentration was no more than 10% of the concentration of galantamine. In vitro studies indicate a very low ability of the main isoenzymes of the human cytochrome P450 system to inhibit galantamine.
Removal
The elimination of galantamine is biexponential. The terminal half-life (T/1/2) in healthy volunteers is 8-10 hours. Based on the results of studies of immediate-release galantamine in population studies, the clearance of oral galantamine in the target population is typically about 200 ml/min, with interindividual variability 30 %. 7 days after a single oral dose of 4 mg of 3H-galantamine, 90-97% of the radioactive dose is excreted by the kidneys in the form of unchanged galantamine and 2.2-6.3% through the intestines. After intravenous and oral administration, 18-22% of the dose was excreted as unchanged galantamine through the kidneys within 24 hours. Renal clearance was 65 ml/min (20-25% of total plasma clearance). Pharmacokinetics are linear in the dose range from 8 mg to 24 mg when administered once daily in elderly and young patients.
Pharmacokinetics of special groups of patients
The results of clinical studies have shown that in patients with Alzheimer's disease, the concentration of galantamine in the blood plasma is 30-40% higher than in young healthy individuals. Based on an analysis of population pharmacokinetic data, clearance in women is 20% lower compared to men. The clearance of galantamine in patients with “slow” metabolizers of the CYP2D6 isoenzyme is 25% lower compared to patients with “fast” metabolizers, while bimodality is not observed in the population. Thus, the patient's metabolic status is not considered clinically significant in the general population. Hepatic impairment: In patients with mild hepatic impairment (Child-Pugh score 5-6), the pharmacokinetic parameters of galantamine were similar to those in healthy subjects. In patients with moderate hepatic impairment (Child-Pugh score 7-9), the AUC and T1/2 of galantamine were increased by approximately 30%. Impaired renal function: In patients with Alzheimer's disease and impaired renal function (creatinine clearance (CC) ≥ 9 ml/min), no dose adjustment is required.
Pharmacokinetic-pharmacodynamic relationship
In large phase III studies with galantamine 12 mg and 16 mg twice daily dosing regimens, there was no apparent correlation between mean plasma concentrations and efficacy measures (changes in Alzheimer's Disease Assessment of Cognitive Scale (ADAS-cog/11) and assessment of the patient's condition based on the impressions of the doctor and caregivers (CIBIC-plus) at the 6th month of therapy). Plasma concentrations in patients with syncope were in the same range as in other patients taking the same dose. The occurrence of nausea correlates with a higher peak plasma concentration.
Experience of clinical use of Reminyl (galantamine)
The problem of population aging affects doctors of all specialties and especially psychiatrists. The reason for this is the increasing incidence of dementia in older people. Accordingly, the socio-economic burden on society for the treatment and care of this category of patients is increasing. According to an epidemiological study of the mental health of the elderly population of Moscow, Alzheimer's disease (AD) affects 4.5% of residents aged 60 years and older (1).
Table 1. Average total scores of the MMSE, ADAS-Cog, IADL, BEHAVE AD scales before the start of therapy
Figure 1. Dynamics of the average total MMSE score in mild, moderate dementia and for the group as a whole
Table 2. Dynamics of the average difference in the sums of scores of the ADAS-Cog, IADL, BEHAVE-AD scales
Figure 2. Dynamics of the patients’ condition according to the CGL scale
Figure 3. Dynamics of the average total score on the MMSE scale in AD and AD
Figure 4. Dynamics of the average total MMSE indicator in SMD
As is known, dementia is caused mainly by primary neurodegenerative processes, vascular pathology or a mixed vascular-degenerative process. According to the literature, a stroke increases the risk of vascular dementia (VaD) by 4-12 times (9). In our opinion, the current state of psychopharmacotherapy makes it possible not to ignore the decline in cognitive and psychosocial activity associated with the normal aging process.
The common mechanism for the two main types of dementia - Alzheimer's disease (AD) and vascular dementia (VaD) - is cholinergic neurotransmitter deficiency, the involvement of which in the development of dementia in both AD and VOD is now generally accepted, and its compensation with cholinomimetic drugs has become one of the main approaches to the treatment of this disease. It has been proven that an increase in the concentration of central acetylcholine is accompanied by an increase in the processes and number of synaptic contacts (4).
Galantamine (Reminyl) is a selective, competitive, reversible acetylcholinesterase inhibitor that can enhance the effects of acetylcholine through modulation of nicotinic acetylcholinergic receptors (nAChRs). Potentiation of nicotinic receptors makes it possible to enhance the nicotinic response of cholinergic neurons damaged by the degenerative process, but continuing to function. In addition, Reminyl modulates the release of glutamate, dopamine and GABA, thereby reducing the psychological and behavioral symptoms of dementia. As a result of increasing the sensitivity of nAChR (due to the modulating effect of galantamine (Reminyl) on nAChR), the effectiveness of the drug has been proven not only in AD, but also in mixed dementia (MSD) and vascular dementia (VoD).
Purpose
This study was to study the effectiveness and tolerability of Reminyl in clinical practice. We undertook an open, uncontrolled study of the effectiveness and safety of Reminyl in the treatment of AD, AD and SMD.
The objective of the study was to compare the results of therapy depending on the type of dementia, its nosology and severity.
Research methodology
developed jointly with researchers from the Scientific Center for Mental Health (headed by Prof. V.A. Kontseva). According to the study protocol, patients with mild or moderate dementia (according to the Clinical Dementia Rating) (11), AD (according to the NINCDS/ADRDA criteria), AD (according to the NINCDS-AIREN criteria) and “mixed” dementia (MD) (according to the NINCDS criteria) were selected /ADRDA). The study included patients with an MMSE score ranging from 12 to 24 points at the time of the screening visit. The diagnosis took into account clinical laboratory data, including CT or MRI of the head.
Exclusion criteria:
Patients with dementia of other origins - brain tumor, Parkinson's disease, frontotemporal dementia and other brain pathologies, as well as so-called metabolic dementia and pseudodementia were excluded from the study. Patients with severe and/or decompensated somatic pathology were also not included. The simultaneous administration of drugs that affect cognitive function was excluded: acetylcholinesterase inhibitors, NMDA receptor antagonists, peptide drugs, antioxidants, nootropics, antipsychotics and antidepressants with a pronounced anticholinergic effect, as well as those that alter drug absorption or reduce heart rate.
In accordance with the study protocol, patients were treated with Reminil for 3 months at a dose of 8 mg/day. (in 2 doses) in the 1st month of therapy and 16 mg/day. (in 2 doses) over the next 2 months.
Treatment efficacy was analyzed using the following clinical and psychometric scales: MMSE, ADAS-Cog and Activities of Daily Living (IADL), Behavioral Disorder in AD (BEHAVE-AD), and Clinical Global Impression (CGL). In addition, undesirable effects of therapy were recorded in a special table. The MMSE scale was assessed four times: at visit zero and then every month; on other scales - three times: at the “zero” visit, after 1 and 2 months.
14 patients (7 men and 7 women) participated in the study. 4 of them were diagnosed with late-onset BA, 6 had SD and 4 had SMD. 11 patients had mild and 3 had moderate dementia. The average age of onset of the disease (onset of dementia) was 65.3 ± 6.4 years. The average age of patients at the start of therapy was 71.7 ± 7.8 years. The duration of dementia ranged from 2 to 10 years, on average - 5.8 ± 3.9 g. More than half of the patients (n = 8; 57%) suffered from one or another somatic disease, mainly arterial hypertension, coronary artery disease, cardiosclerosis, and vascular encephalopathy.
All patients completed a three-month course of treatment. SPSS 12 programs were used for statistical data processing.
The dynamics of the MMSE scale data was assessed based on the calculation of its total indicator; analysis of the results of the ADAS Cog, IADL and BEHAVE-AD scales was based on the difference in their total scores between the initial and follow-up assessments (Table 1). In this case, the average indicators of the mentioned scales were calculated by pairwise comparison of their initial value with each of the subsequent ones using the Wilcoxon method. CGL scale data were subjected to frequency (percentage) analysis.
The initial data demonstrate a significant correspondence between the severity of dementia and its assessment according to the MMSE and ADAS-Cog scales, which characterize various parameters of the cognitive functions of patients, as well as the IADL scale, which reveals the degree of adaptation in everyday life. A similar trend, which, however, did not reach the level of statistical significance, was observed according to the BEHAVE-AD scale, which records very heterogeneous symptoms, of which the most common in the patients we examined were mild (within 1-2 points) sleep disturbances (98 %), anxiety and phobias (78.5%), subdepression (64%), individual delusional symptoms (14.2%).
Research results
Figure 1 demonstrates statistically significant positive dynamics in the cognitive functioning of patients, according to the MMSE scale, both for the group as a whole and for mild and moderate dementia by the end of the first month of therapy. Noteworthy is the stabilization of this indicator after two months of therapy in patients with moderate dementia, while in patients with mild dementia a statistically significant increase in this indicator occurred throughout the entire observation period.
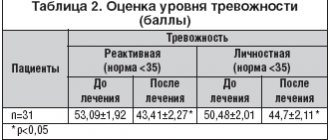
Information on the dynamics of the average difference in the total indicators of the ADAS-Сog, IADL and BEHAVE-AD scales is given in Table 2.
According to the ADAS-Cog scale, both in mild and moderate dementia, and in the group as a whole, a statistically significant improvement in the cognitive functions of patients was noted after 2 months of therapy. The rates of this improvement increased by approximately another half by the end of 3 months of therapy. The corresponding indicators of the BEHAVE-AD scale underwent similar dynamics, which indicated a reduction in the productive psychopathological symptoms and behavioral disorders associated with dementia. The IADL scale scores in patients with mild dementia demonstrated a significant improvement in the functional abilities of patients by the 2nd month of therapy, with a slight subsequent improvement by the end of the 3rd month. Whereas in patients with moderate dementia, such a trend was not observed, possibly due to the small number of patients.
According to the CGL scale (Figure 2), there was a varying degree of positive dynamics in the condition of patients in the group as a whole, both after 1 and after 3 months. therapy was observed in 80% of patients. In all types of dementia, minimal improvement prevailed, and there were no cases of worsening of the condition. Marked improvement was observed in only a third of patients with mild dementia by 2 months of therapy. Upon completion of therapy, improvement in overall condition was observed 2 times more often in mild than in moderately severe dementia.
Depending on the diagnostic affiliation of dementia, it was possible to compare the results of therapy only for mild dementia, since almost all cases of AD corresponded to mild dementia. Individuals with AD (n = 3) and AD (n = 4) selected for comparison differed in the age of onset of dementia (74.3 ± 9.8 and 66.5 ± 6.3 years, respectively), as well as in the age of the patients at the start of therapy (79.2 ± 11.5 and 70.75 ± 9.5 years, respectively).
According to the MMSE scale (Figure 3), with approximately the same score at the start of therapy in the AD and SoD groups after 3 months of therapy, the improvement in cognitive functions in SoD turned out to be more pronounced (by about 2.5 points) than in AD. A similar trend was noted according to the ADAS-Cog and IADL scales. The mean BEHAVE-AD total score improved more markedly in AD. However, the small number of observations makes statistical processing of data on the above scales incorrect. After 1 month of therapy, cases with minimal improvement were observed in BA, and cases with moderate improvement dominated in SoD. With SoD, already at this early stage of treatment, approximately 21% of patients showed a pronounced and 9% a moderate improvement.
In the 4 patients with SMD included in the study, the severity of dementia was mild. The average age at the onset of dementia was 64.0 ± 4.9 years, the average age of patients at the start of treatment was 67.75 ± 7.7 years.
Figure 4 demonstrates the positive dynamics of the cognitive functions of patients with SMD according to the MMSE scale; the improvement was almost 5 points compared to the initial assessment. A clear improvement in patients with SMD was also observed in terms of other scales, but it was especially noticeable at the end of therapy.
Adverse events
Moderately severe adverse events were observed in 2 patients (14.2%). In one case, nausea was noted, in the second - headache, difficulty falling asleep when the dose of the drug was increased in the second month of treatment. Reducing the daily dose of the drug (from 16 to 8 mg) led to the disappearance of adverse events and improvement in the patients' condition at the end of therapy, despite the use of a dose of 8 mg/day.
The discussion of the results
Thus, a clinical study of Reminil made it possible to establish its effectiveness in the treatment of the main types of dementia. According to the literature, the drug demonstrates a complex therapeutic effect on various components of dementia: cognitive and psychopathological disorders, behavioral disorders, and maladjustment of patients in everyday life. Significant improvement, according to our data, becomes obvious by the end of the first month of therapy and gradually increases by the time it is completed. Noteworthy is the stabilization of indicators after two months of therapy in patients with moderate dementia. It should be noted that, according to the CGI scale, there was not a single case of deterioration in the condition of patients in general, and some degree of improvement was detected in the majority of patients (80%).
Despite a fairly harmonious reduction in the manifestations of dementia in all its variants, the greatest therapeutic effect in relation to the state of cognitive functions and parameters of the general condition of patients was achieved in mild dementia (MMSE, ADAS-cog and CGI scales). A pronounced improvement was observed only in mild dementia (by the 2nd month of therapy in 1/3 of cases). Upon completion of therapy, improvement in overall condition was observed 2 times more often in mild than in moderately severe dementia.
The reduction of productive psychopathological symptoms and behavioral disorders accompanying dementia, according to the dynamics of the IADL and BEHAVE-AD scales, in patients with mild dementia was significant by the end of 3 months of therapy, while in patients with moderate dementia no such trend was noted.
An assessment of the effectiveness of galantamine therapy in patients with mild dementia in SoD and AD showed that in SoD, indicators of the cognitive sphere and everyday life skills improve more clearly (on the MMSE, ADAS-cog, IDAL scales). The condition of patients in general definitely improved by the second month of treatment with AD, and by the third month of treatment with AD.
In the studied sample of patients, moderately severe adverse events (mainly headache, nausea) were noted in two patients. They occurred when the dose of the drug was increased in the second month of treatment to 16 mg/day and disappeared after returning to the original dose. This makes it advisable to treat dementia even with low doses of the drug in cases where higher doses lead to adverse events.
Thus, this study demonstrated the greater effectiveness of treatment with galantamine SoD compared to BA and its good tolerability.
PsyAndNeuro.ru
In recent years, several studies have been published on the use of galantamine-memantine combination in Alzheimer's disease (AD). In a two-year randomized controlled trial (RCT) of prodromal AD, the cognitive performance of patients receiving a combination of galantamine and memantine was significantly better than the cognitive performance of those receiving galantamine alone [1].
In a retrospective cohort study, the combination of galantamine-memantine significantly improved cognitive performance compared with the combination of donepezil-memantine in the treatment of AD [2]. In a naturalistic study, patients with dementia with Lewy bodies received galantamine for 6 months. Patients who responded to treatment were then also given memantine. The addition of memantine to galantamine significantly improved cognition and behavior compared with galantamine alone [3].
Despite compelling evidence, the galantamine-memantine combination is still underutilized in clinical practice. In the United States, galantamine and memantine are approved for the treatment of AD. The donepezil-memantine combination is also approved for the treatment of AD, but the galantamine-memantine combination is not.
Galantamine is superior to donepezil because it is a positive allosteric modulator of alpha7-nicotinic acetylcholine receptors and acts as an acetylcholinesterase inhibitor. Finally, in addition to cognitive impairment, psychosis and negative symptoms are often observed in AD. The galantamine-memantine combination can not only improve cognitive function, but also be used against psychosis and negative symptoms.
When analyzing the results of RCTs on the treatment of AD, it must be taken into account that many of them give a negative result due to the fact that patients are often recruited at an advanced stage of the disease. Treatment may be ineffective in late stages of AD because chronic neuroinflammatory processes cause irreversible damage over time. Typically, RCTs involve patients whose plaque burden and degree of neurodegeneration are already quite high, so their disease has probably already become irreversible. Clinical data suggest that treatment of asthma in the early stages is more promising. The best results are achieved in patients at the prodromal stage or in patients with mild cognitive impairment. This situation can be compared with carcinoma in situ and stage 1 or 2 cancer versus stages 3 and 4; in later stages, intervention usually does not produce results.
It is probably often the case that one drug is not enough to stabilize all pathophysiological mechanisms and reduce the symptoms of asthma. Neurodegenerative diseases include many pathologies, so combination treatment seems to be the most rational choice.
At the same time, taking a significant amount of medications by patients with asthma places a serious financial burden on their families. Previously, we published an analysis to find out which memantine is more economically beneficial. In the Russian Federation, 11 manufacturers of memantine are available in pharmacies, of which 6 contain an Indian substance, and 5 – a European one. However, the production of tablets for three of them is localized in the Russian Federation, and only two memantines - Akatinol and Memantal - are entirely produced in Europe. It is noteworthy that the first of them is the original drug, and the second is the only generic with proven therapeutic equivalence.
The combination of galantamine and memantine can be effective not only for asthma, but also for traumatic brain injury, autism and other neuropsychiatric diseases. In 22 patients with AD, memantine improved biomarkers of oxidative stress such as non-protein thiols and 3-nitrotyrosine in the cerebrospinal fluid [4]. Redox reactions mediated by NMDA receptors and their interactions with other molecules may be involved in synaptic dysfunction.
Simultaneous effects on nicotinic and NMDA receptors can be a very successful method for improving the basic parameters of cognitive functions of the brain [5].
Author: Filippov D.S.
Sources:
[1] Peters, O. et al. 2012. A combination of galantamine and memantine modifies cognitive function in subjects with amnestic MCI. J. Nutr. Health Aging 16(6), 544–548
[2] Matsuzono, K. et al. 2015. Combination therapy of cholinesterase inhibitor (donepezil or galantamine) plus memantine in the okayama memantine study. J. Alzheimer's Dis. 45(3), 771–780
[3] Vasenina, EE, Gankina, OA, Levin, OS, 2021. The addition of memantine to galantamine increases treatment efficacy in patients with moderate dementia with Lewy bodies. Zh Nevrol Psikhiatr Im S Korsakova 118 (6. Vyp. 2), 32–36
[4] Valis, M. et al. 2021. The Concentration of Memantine in the Cerebrospinal Fluid of Alzheimer's Disease Patients and Its Consequence to Oxidative Stress Biomarkers. Front. Pharmacol. 10,943
[5] Koola, Maju. (2020). Galantamine-Memantine Combination in the Treatment of Alzheimer's Disease and Beyond. Psychiatry Research. 293.113409.
![Table 3. Pharmacokinetic and pharmacodynamic parameters of fluoroquinolones with a single standard dose taken orally [7, 13]](https://irknotary.ru/wp-content/uploads/tablica-3-farmakokineticheskie-i-farmakodinamicheskie-parametry-ftorhinolonov-pri-odnokratnom-prieme-330x140.jpg)