Pityriasis versicolor is a fungal infection of the skin with certain symptoms that occurs as a result of the malassezia fungus entering the body. It is often diagnosed in countries and regions with warm to hot climates, which is why it is called beach lichen.
This skin disease appears in adolescents and young adults (it is extremely rarely diagnosed in preschool and retirement age), but people prone to dermatomycosis are also at risk. The disease is long-term and protracted; relapses occur (especially in the hot season, regardless of the region of residence), so it is often called chronic.
Ringworm, like many fungal and viral diseases, is rarely a serious threat to life, but it can indicate health problems and reduce quality of life, especially affecting a person's psychological state.
Causes of tinea versicolor
The content of the article
Ringworm affects middle-aged people. Medicine identifies the causes that lead to the appearance of this disease in humans. These include:
- Predisposition to fungal skin diseases.
- Disruptions in the course of physiological processes in the epidermis.
- Endocrine diseases.
- Lack of a good night's sleep.
- Lack of rest.
- Time zone change.
- Excessive hygiene, using antiseptics.
- Improper functioning of the human immune system.
- Frequent bathing in salt water.
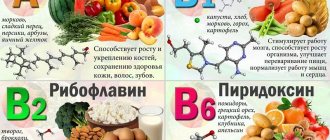
- Lack or excess of vitamins.
- Wearing clothes made of synthetic materials.
- Improper functioning of the lymphatic drainage system.
- Long-term use of steroid hormones.
- Nervous system problems.
- Hormone imbalance.
- Lack of hygiene measures in public places.
Pityriasis versicolor during pregnancy
During pregnancy, women may experience various diseases, including skin inflammation. The causes of lichen, like many ailments, in pregnant women are often a decrease in immunity or hormonal changes.
As a rule, pityriasis versicolor is not treated during pregnancy, or a gentle course with carefully selected components is prescribed so as not to harm the fetus, but to improve the quality of life of the expectant mother. Treatment is always strictly individual.
Pityriasis versicolor in children
This is a common disease in children. It usually affects the scalp, but can appear on the face and body. For young children and adolescents, as well as for pregnant women, treatment can only be prescribed externally (in particularly difficult cases, the use of medications and drugs is possible). Parents of infected children need to monitor the child’s hygiene and not allow the baby to scratch the spots in order to prevent the spread of the disease and not create a favorable background for the occurrence of other diseases.
How dangerous is solar lichen? Is pityriasis versicolor contagious or not?
If the disease does not have complications and does not occur in parallel with other diseases, then it does not pose a danger to human health, except for the psychological discomfort mentioned above, especially if spots appear on the face.
The disease can be called conditionally contagious, since the fungus (causative agent) of skin inflammation is present on the skin of any person (it is part of the microflora) or can be transmitted from person to person, but the disease itself will occur only in the event of an external “irritant”.
Infection is possible:
- during personal contacts;
- through personal and hygiene items;
- in public changing rooms or fitting rooms.
How and how to treat pityriasis versicolor in humans (colored, multi-colored, etc.)?
If you notice signs of this disease, it is important to remember three simple rules:
- do not self-medicate, because the wrong medicine can only worsen the condition;
- do not wait until everything goes away on its own (the disease has a wave-like nature, that is, it can be repeated at different intervals and does not always return in a mild form);
- Do not use dubious, suggested by someone, or self-selected remedies for pityriasis versicolor.
Seeing a doctor is a sure way to not only get cured, but also strengthen your immune system, as well as get rid of annoying aesthetic skin defects that bring psychological discomfort.
Method of infection
Mushrooms can come into contact with the skin of a healthy person, but with strong immunity, the body uses protective functions and the disease does not occur.
Main routes of transmission:
- Skin contact with the carrier.
- In public places: shower, fitting room.
- Use of a person’s personal belongings: towel, washcloth.
When infected with this microorganism, symptoms do not appear for 2 weeks to several months. They may not appear at all unless a situation arises when the immune system weakens.
How to diagnose lichen
Diagnosis of tinea versicolor consists of conducting a visual examination by a dermatologist and ordering a study of the affected area of the epidermis. When examining the patient, it is necessary to identify: for what reason the lichen occurred, the duration of the process and the degree of damage to the skin by colored spots.
To identify lichen, the following research methods can be used:
- Skin scraping. The study reveals round fungal spores with a double contour.
- Culture method. It is based on placing a sample of cells in a nutrient medium in order to develop colonies of the fungus lichen cauliflower.
- Balser's test (iodine test). The affected area of skin is covered with iodine solution (or 1-2% aniline solution) to change the color of the epithelium. At the same time, the cells that have been affected by tinea versicolor acquire a loose structure and are painted in a rich dark color, while healthy cells are painted in a light shade. After the examination, the skin is cleansed with an alcohol solution.
- Using a Wood's lamp. Examination of skin areas under an ultraviolet lamp. In this case, the areas that are affected by lichen give off a greenish-blue or red-yellow glow.
- Use of mercury-quartz lamps. The study is used to identify areas of skin that are affected by the fungus, but have no visual manifestation. Under the light of a lamp, these areas acquire noticeable color pigmentation.
Using effective strokes we “kill” the fungus
If you choose among the many antifungal drugs widely represented on the modern Russian market, then preference should be given to those that, firstly, are able to accumulate in those layers of the skin where the fungal process develops, and secondly, do not penetrate into those layers where fungal activity is impossible. Usually, treatment of lichen versicolor is carried out with local drugs, and in severe cases with the use of systemic antimycotics, which can significantly reduce the treatment time and prevent the frequency of relapses. But you should always remember that if you find signs of a disease in yourself, under no circumstances try to treat yourself, but immediately go to a doctor who will accurately determine your diagnosis and prescribe the right treatment for you.
Methods of drug therapy
The main goal of treatment is to eliminate the causative agent of the disease. For this purpose, oral and local antifungal drugs are used. This treatment can be carried out at home.
For your information! If the disease is advanced, treatment will be lengthy.
In order to cope with versicolor, the patient is prescribed a set of measures, including the following medications:
- Selenium preparations, for example, Sulsena.
- Fluconazole or analogue drugs.
- Antimycotic agents.
- Imidazole (Ketaconazole, etc.).
- Ozone therapy.
- Use of products with salicylic acid.
- Enrichment of the diet with vitamins.
In addition to the use of medications, the patient must strictly follow the doctor’s instructions regarding personal hygiene and maintaining a clean home. The duration of treatment in untreated cases is about a week.
Lichen versicolor or vitiligo?
Tinea versicolor can sometimes be confused with vitiligo as both cause patchy discoloration of the skin. There are the following ways to tell the difference:
vitiligo often develops on both sides of the body at the same time, while lichen versicolor can be one-sided;
skin affected by vitiligo usually has a normal texture, while areas affected by tinea versicolor are usually slightly scaly or flaky;
Vitiligo is more common around the mouth, eyes, fingers, wrists, armpits and groin, while tinea versicolor tends to develop on the back, chest, shoulders, neck and abdomen.
| Service | Price | Promotion Price | Promotion Price |
| Appointment (examination, consultation) with a therapist | 1800 rub. primary | 1500 rub. repeated | free appointment with vitamin therapy course |
| Autohemotherapy | 550 rub. 1 session | 2500 rub. 5 sessions | 5000 rub. 10 sessions |
| Ultrasound therapy procedure | 450 rub. | ||
| Plasma therapy | 4500 rub. 1 session | 10500 rub. 3 sessions | 17500 rub. 5 sessions |
| Vitamin therapy (course of 10 injections) | 4000 rub. | 3000 rub. | free appointment with a therapist |
| Recovery course of IVs after COVID-19 (Coronavirus) | 950 rub. 1 session | 4050 rub. 5 sessions | 8100 rub. 10 sessions |
| Intravenous drip administration of drugs (without drugs, 1 bottle) | 800 rub. 1 session | 3375 rub. 5 sessions | 6750 rub. 10 sessions |
| Intravenous drip administration of medications (with existing clinic medications, 1 bottle) | 950 rub. 1 session | 4050 rub. 5 sessions | 8100 rub. 10 sessions |
| Intravenous drip administration of drugs (without drugs, 2 bottles) | 950 rub. 1 session | 4050 rub. 5 sessions | 8100 rub. 10 sessions |
| Intravenous drip administration of medications (with existing clinic medications, 2 bottles) | 1100 rub. 1 session | 4700 rub. 5 sessions | 9400 rub. 10 sessions |
| Intravenous administration of drugs (course) | 450 rub. 1 session | 2140 rub. 5 sessions | 4050 rub. 10 sessions |
| Subcutaneous-intradermal administration of drugs (course) | 250 rub. 1 session | 1180 rub. 5 sessions | 2250 rub. 10 sessions |
| Intramuscular administration of drugs (course) | 300 rub. 1 session | 1575 rub. 5 sessions | 2700 rub. 10 sessions |
| Registration of a certificate for the swimming pool | 500 rub. | ||
| Registration of a sanatorium-resort card | 400 rub. | ||
| Annual examination program - Chek-UP | 4700 rub. | 3999 rub. | free appointment with a therapist |
| Examination program Men's health passport | 9900 rub. | 8999 rub. | free appointment with a therapist |
| Examination program Women's health passport | 7700 rub. | 6999 rub. | free appointment with a therapist |
| Complex body cleansing program RELOAD | 17,000 rub. | 13500 rub. | free appointment with a therapist |
Signs of the disease
Externally, erythrasma manifests itself in the form of light brown, brick-red, brown or yellow-brown spots on the skin, most often round in shape and without signs of inflammation. The diameter of the lesions can reach several centimeters, and they tend to merge, forming large affected areas. First of all, erythrasma spots appear in the folds of the skin, where there is a favorable environment for the proliferation of bacteria.
In addition to spots, erythrasma is characterized by:
- Peeling of the skin on the affected areas, aggravated by touch. Usually this is where the development of the disease begins.
- Mild, irregular itching. It intensifies and begins to cause significant discomfort only if a secondary infection is added to the primary disease.
- Absence of fever, wounds, ulcers and ulcers with copious discharge. This distinguishes erythrasma from most bacterial skin pathologies.
- Getting wet. An optional symptom, the manifestation of which depends on the amount of sweating and the quality of skin care.
It is noteworthy that in children, symptoms of erythrasma appear extremely rarely. The risk group includes adults, primarily men, who are predominantly overweight and prone to excessive sweating. In this case, in men, the skin in the groin, navel and inner thighs is usually affected, and in women, the entire abdomen, armpits and areas under the breasts are affected.
General provisions of therapeutic measures for tinea versicolor
The main condition for eliminating tinea versicolor is to contact a dermatologist, since self-prescription of drugs or the use of folk remedies is irrational. Incorrect selection of a course of medications during treatment or non-compliance with the dosage of medications can cause complications or relapse of the disease (repeated skin damage by the pathogen). The use of infusions, ointments, lotions and sprays, which are prepared according to folk recipes, is allowed to a person only after consultation with the attending physician and under his strict supervision.
Treatment of tinea versicolor is carried out strictly under the supervision of a specialist and consists of the use of medications, various ointments, special diets and physiotherapeutic procedures. Medicines are selected for each patient individually, depending on the cause of the fungal infection, the area of development of color pigmentation and the individual characteristics of the patient.
Depending on the degree of infection of the patient by the colored fungus, the method of therapeutic treatment is selected - outpatient (in the absence of a bacterial infection) or inpatient. Specialists use an integrated approach to treatment using local and systemic drugs. Ointments and creams cannot completely remove the causative agent of the disease, since they only have a superficial effect.
Treatment of tinea versicolor requires the dermatologist to prescribe medications and vitamin-mineral complexes to the patient that support the immune system and increase the body’s defenses. To enhance the healing effect of skin affected by lichen, physiotherapeutic techniques are used, which are carried out in the form of ultraviolet irradiation.
Relapses
Tinea versicolor often returns after treatment, especially in the summer or while on vacation in warm, humid countries. The patient can reduce this likelihood by regularly using antifungal shampoos as a preventative measure. For example, using shampoo once a day for a few days before going on vacation can help prevent a recurrence of tinea versicolor.
If a patient develops tinea versicolor again after treatment, they can try treating it themselves with an antifungal shampoo or contact their GP for advice and other treatments. If the patient has frequent and severe episodes of tinea versicolor, the GP may consider prescribing antifungal tablets several times a month to prevent recurrence of the condition and recommend consultation with a dermatologist.
Symptoms of the disease
When infected with pityriasis versicolor, the pathogens multiply in the superficial layers of the skin, disrupting the normal functioning of cells. First of all, melanocytes, which are responsible for the production of the pigment melanin, are affected, thanks to which the skin has one color or another. This means that under the influence of pathogenic microorganisms, the affected areas acquire an uncharacteristic, painful shade. Hence the second name for pityriasis versicolor - versicolor.
The main symptoms of pityriasis versicolor include:
- Spots of yellow, coffee, scarlet or dark brown shades, located mainly on the back, head and neck, shoulders and stomach. In children, they also appear on the limbs, armpits and scalp. The affected areas can be of different sizes, but usually their size does not exceed 1 cm. Subsequently, the spots merge with each other, forming significant areas of the affected skin.
- No signs of inflammation in the form of redness, swelling, hyperemia and pain to the touch.
- Severe peeling of the skin in infected areas, aggravated by touch.
- No tanning on the affected areas.
Pityriasis versicolor is not characterized by itching and discomfort, so patients often mistake the manifestations of the disease for minor cosmetic defects, postponing a visit to the doctor and full treatment.
Such spots begin to itch and scratch only if a secondary infection occurs.
Prevention
To prevent relapses, you need to treat chronic diseases, maintain immunity at the proper level, harden yourself, and eat well. Wear clothes made from natural fabrics that do not restrict movement.
Do not wear other people's clothes, do not use other people's objects. On particularly hot days, wipe the skin with water with the addition of alcohol or lemon. Maintain cleanliness and order.
Take antifungal medications once monthly. Although the lesion is not accompanied by painful sensations, it spoils the appearance and causes inconvenience.
Ringworm on the arm - 115 photos of what lichen looks like and video recommendations from dermatologists for treating the diseaseRingworm - symptoms, development, types, tips on how to quickly and effectively cure at home (105 photos and videos)
Lichen planus - first symptoms, causes, information about the disease and effective treatment (100 photos)
Multicolored leather
Pityriasis versicolor usually begins with the appearance of a small, not very inflamed pink spot that does not rise above the surface of the skin. Sometimes the color may be yellowish or coffee-colored. Gradually, the spot becomes overgrown with “brothers”; they merge into bizarre outlines, forming “geographical” patterns. Elements of multi-colored lichen are located on the skin of the chest, upper back, neck, and shoulders. Against the background of tanned skin, the spots look lighter. The spots tend to merge to form large foci, but can exist in isolation. There are no inflammatory phenomena, there is slight pityriasis-like peeling.
Causes of pathology
Corynebacteria, which are the causative agents of the disease, are normally always present on human skin. Moreover, they provoke the development of pathology only under certain, favorable conditions. Corynebacteria do not penetrate deeper than the epidermis, and also do not affect nails and hair. Since the appearance of erythrasma is directly related to increased sweating, the disease most often manifests itself in the hot summer season.
Among the main reasons for the development of erythrasma are:
- hyperhidrosis;
- deviation of the normal pH of the skin to the alkaline side;
- diaper rash, constant friction and mechanical damage to the skin;
- dermatitis and other skin diseases;
- neglect of personal hygiene rules;
- wearing synthetic, overly warm clothing;
- the use of low-quality care products or the abuse of soap with an antibacterial effect, which destroys the natural protection of the skin.
Erythrasma is transmitted by contact, most often after the use of clothing, bedding and personal hygiene products of the patient. You can also become infected during sexual intercourse, when visiting a pool or bathhouse, and when walking barefoot on the ground or beach. At the same time, it is not always possible to accurately determine the source of infection, because the carrier may not have obvious external manifestations of the disease in the form of characteristic spots and peeling.
Publications
Versicolor (pityriasis versicolor) (Tinea versicolor) is a mycotic skin infection characterized by widespread distribution and a chronic relapsing course. The disease affects 10% of the population. In hot countries, lichen versicolor is more common.
In mid-latitudes, most cases of the disease occur in the summer. Adults and young people get sick more often; The disease is rare in children and the elderly. Transmission of the pathogen from a patient or carrier: for example, through a shared bed or clothing (underwear), is possible, however, in most cases, the source of infection is endogenous. Therefore, lichen versicolor is not considered a contagious disease. Some authors consider iatrogenic immunodeficiencies, pregnancy, and hormonal contraception to be predisposing conditions. A hereditary predisposition to the disease cannot be ruled out.
In the International Classification of Diseases (ICD-10), lichen versicolor is included in the section “Other superficial mycoses” (B36.0) and has code B36.1. Its causative agents are opportunistic imperfect yeast lipophilic fungi. In recent years, the causative agents of pityriasis versicolor have been assigned to the genus Malassezia [2,4]. Currently, the genus Malassezia has 9 described species of fungi, among which the main causative agents of pityriasis versicolor are M. globosa, M. sympodialis, M. sloolliae |6, 7|. Fungi of the genus Malassezia are imperfect yeast fungi, basidiomycetes. A common characteristic of most Malassezia species is lipophilicity: (requirement of a source of lipids for growth). Malassezia are distinguished by polymorphism, consisting in different cell shapes (round or oval) in representatives of the same genus and even species, and the ability to form mycelial forms.
The disease begins with the appearance of small spots with a clear edge, or papules slightly raised above the surface of the skin. Small spots are often located around the hair follicles. The color of the spots ranges from yellowish-pink to brown in different shades. The spots often merge, forming large lesions with scalloped edges. On the surface of the spots you can notice a gentle “pityriasis-like” peeling. Peeling intensifies with scraping (symptom of shavings, or “nail strike” of Beignets). The color of the spots differs from the color of the surrounding skin: in people with fair skin, the lesions look darker, in people with dark or tanned skin - lighter, depigmented (pseudo-leukoderma, pityriasis versicolor alba). The same patient may have both hyperpigmented and hypopigmented macules. The color of the spots is mainly determined by exposure to ultraviolet radiation: unlike the color of the surrounding skin, it does not change after tanning. In rare cases, inflammatory lesions with erythema and slight infiltration occur. Typical localization of lesions in lichen versicolor is areas of the body rich in sebaceous glands: chest, back, neck, shoulders. Less commonly, the axillary, groin, forearms and lower legs are involved. In tropical climates, lesions on the face, abdomen, and scalp are more common. The inverse form (tinea versicolor inversa) is the lesion of large, usually inguinal, folds. Hair and nails are not affected. Changes in the skin, as a rule, are not accompanied by subjective sensations. The disease is characterized by a long-term relapsing course.
The variety of clinical manifestations makes timely diagnosis of mycosis difficult [6]. A long-term recurrent course, significant contamination of the skin and scalp with pathogens, and their penetration into the pilosebaceous follicles cause certain difficulties in the treatment of patients with lichen versicolor [1]. Until recently, keratolytic agents, which have low antifungal activity, are inconvenient to use and do not reduce the number of disease relapses, have been widely used in treatment.
N.V. Kungurov et al. developed an algorithm for the management of patients with lichen versicolor. When detected in patients on the skin in typical localizations (areas rich in sebaceous glands), spots of a round or oval shape, non-inflammatory in nature, not rising above the surface of the skin, with clear boundaries, scalloped edges, of various colors (from yellowish-pink, light brown to brown) and gentle pityriasis-like peeling on the surface for the purpose of diagnosis, a Balser test is performed (when the lesions are smeared with alcohol solutions of iodine or aniline dyes, the affected skin is colored much brighter than healthy), and the symptom of “chips” is revealed - with careful scraping of the spot, a barely noticeable tender pityriasis peeling intensifies, which is due to loosening of the stratum corneum of the epidermis.
The skin of the torso and extremities is examined under a Wood's lamp in order to identify non-visual, atypical forms of the disease. Lesions occupying up to 18% of the area are limited (localized) forms, more than 18% are widespread. The erythematous-squamous form (the most typical) is recorded in 98.5% of cases and is characterized by the clinical manifestations described above. The follicular variant, found in 7% of patients, is characterized by the appearance of perifollicular papules or pustules of a yellowish color, located on an erythematous background, while in the middle of the spots, point-shaped follicular openings are clearly visible. In the inverted variant (3.5%) of the clinical course, the lesions are localized in the inguinal-femoral folds, in the pubic area, on the thighs and legs. Less commonly, rashes of pityriasis versicolor rise above the skin and to the touch create the impression of nodules the size of a lentil or smaller, located in groups (pseudo-papular form). Certain difficulties in making a preliminary clinical diagnosis arise in the presence of hypopigmented lesions on the skin that appear in place of typical spots of pityriasis versicolor, usually after irradiation with ultraviolet rays or insolation. Differential diagnosis is carried out with diseases such as Zhiber's pityriasis rosea, syphilis (primary and secondary), seborrheic dermatitis, chloasma, vitiligo, as well as other skin dyspigmentations.
After making a preliminary clinical diagnosis of lichen versicolor, taking into account the course and extent of the process, it is confirmed in the laboratory. During microscopic examination, scales of the stratum corneum of the epidermis of the skin, obtained by scraping with a scalpel from the lesions, are treated with a 20% solution of potassium hydroxide and, after 30 minutes of exposure, are subjected to microscopic examination. The preparation shows short, slightly curved, septate, thick filaments of pseudomycelium and round spores with a double-circuited shell, located in clusters and singly.
To realize the pathogenic properties of the fungus, its transformation from a non-pathogenic form of blastospore into a pathogenic mycelial, certain conditions are necessary, therefore it is necessary to establish factors contributing to the occurrence and spread of fungal infection, analyzing anamnestic data, prescribing consultations and examinations with specialists. Pathology of the gastrointestinal tract, dysfunction of the endocrine system, diseases and functional disorders of the cardiovascular system, seborrheic processes, foci of acute and chronic infection - these conditions directly or indirectly contribute to hyperhidrosis, which results in changes in the physicochemical properties of sweat and sebum (in side of increasing the alkaline reaction), reducing the rate of physiological peeling of the stratum corneum or its loosening, which contributes to the spread of fungal colonies [3].
The choice of treatment tactics depends on the duration, prevalence and form of the fungal process, and identified concomitant diseases.
Most cases of lichen versicolor can be treated with external remedies. Patients with a limited form of lichen versicolor (the fungal process occupies less than 18% of the body skin area), whose disease duration is no more than 2 years, who have not previously been treated, as well as patients with widespread keratomycosis (affected area more than 18%), who have absolute contraindications for use systemic antimycotics, one of the external antimycotic drugs is recommended. The use of external forms that allow covering a significant surface of the body is of considerable importance in the treatment of lichen versicolor. Even if the lesion occurs in the form of separate small lesions, it is recommended to treat all areas where lichen versicolor usually develops. The shampoo is used once a day for 5 days.
Other imidazole antimycotics in the form of creams ( Fungazol "Farmakar") are used 2 times a day for at least 2 weeks. The use of modern antifungal aerosols is promising.
Lichen versicolor is characterized by relapses after treatment. As a rule, a year after treatment, a relapse is observed in every second patient, and within two years - in almost all. To reduce the likelihood of relapses, longer treatment and treatment of larger surfaces are recommended. For frequent relapses, systemic antimycotics, azole derivatives, are prescribed. Systemic antimycotics are prescribed to the following groups of patients: with the prevalence of the fungal process exceeding 18% of the skin area; with limited forms (less than 18% of the skin area), with a disease duration of more than 2 years, with relapses after treatment; with follicular and pseudopapular clinical variants of the course of keratomycosis, regardless of the area of the lesion; with the lightning-fast form of the fungal process.
Itraconazole ( Mikotrox "Farmakar") is an antimycotic with the widest spectrum of action, also effective in the treatment of lichen versicolor. It is prescribed at 200 mg/day for 1 week. Fluconazole ( Diflox "Farmakar") is prescribed once at a dose of 400 mg/day. These same drugs, with single or short-term use, can be used to prevent relapses.
We observed 24 patients with a common form of lichen versicolor, who were repeatedly treated with external antifungal drugs. To treat these patients, we chose the drug itraconazole ( Mikotrox ), which was prescribed at a dose of 100 mg 2 times a day for 1 week. All patients tolerated the therapy well, there were no side effects or cases of negative attitude of patients towards treatment. The criteria for achieving complete clinical and laboratory recovery are the absence of skin rashes, negative specific clinical tests, and the absence of fungal mycelium on microscopy.
Thus, despite the fact that lichen versicolor is a very common disease, it often causes difficulties in diagnosis and treatment, especially in recurrent forms. The use of the modern systemic antimycotic Mikotrox helps solve this problem and improve the quality of life of patients.
LITERATURE:
- Bragina E. E., Novoselov A. Yu., Stepanova Zh. V. // Esthet. honey. - 2002. - T. I, No. 5. - P. 447-453.
- Dmitriev G. A., Grammatikova N. E., Bibikova M. V. et al. // Vestn. dermatol. - 2002. - No. 2. - P. 7-9.
- Kungurov N.V., Skurikhina M.E., Budumyan T.M. etc. //Russian Journal of Dermatovenerol. - 2004. - No. 4. – P.49-51.
- Novoselov A. Yu., Bragina E. E., Stepanova Zh. V. // Immunopathol., allergol., infectol. - 2000. - No. 4. - P. 95-98.
- Potekaev II. P. // Ross. Journal dermatovenerol. - 2001. - No. 3. - P. 9-10.
- Sergeev L. Yu., Sergeev Yu. V. Fungal infections: A guide for doctors. - M., 2003. - 440 p.
- Crespo E, Ojeda M, Vera. A. et al. // JEADV. — 2000. -Vol. 14. - R. 47.
E.A. Levonchuk
Medical news, 2007 No. 13