Tags:
gastrointestinal diseases, colitis
5/5 — (1 vote)
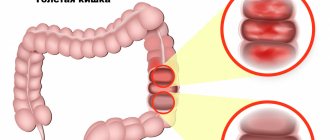
Colitis is one of the most common pathologies of the gastrointestinal tract. It is an inflammatory disease of the large intestine (or rather, its mucous membrane) with pronounced symptoms , which we will talk about later. The disease can be complicated by inflammatory processes in the stomach and small intestine . It often accompanies some other acute and chronic diseases (influenza, pneumonia, typhoid, mumps, malaria, etc.).
It happens that this disease, due to similar symptoms, is confused with irritable bowel syndrome and for this reason is sometimes misdiagnosed. But since irritable bowel syndrome is not associated with the colon, then, accordingly, it cannot have anything in common with colitis.
Colitis
“Hand in hand” with dysbiosis
There are two forms of colitis - acute and chronic . In both the first and second cases, the infectious component plays a special role in the occurrence and development of the disease - most often bacterial dysentery . It can be triggered by other representatives of pathogenic microflora (for example, coli bacteria, staphylococci, streptococci, bacteria of the Proteus group, etc.). In other words, colitis goes “hand in hand” with dysbacteriosis. Inflammation can also be caused by previous intestinal infections and poor diet, as well as inadequate therapy with various medications. As practice shows, the causes of inflammation are indeed multiple. Let's summarize the main factors :
- infection in the gastrointestinal tract;
- infection with salmonella, staphylococci and other pathogenic microflora due to consumption of poor-quality food;
- the presence of worms (but not in all cases);
- inadequate, monotonous diet (mainly carbohydrates);
- allergies to certain types of food;
- chronic constipation;
- alcohol abuse;
- neglect of personal hygiene rules (for example, touching food with dirty hands);
- long-term use of certain antibiotics that can provoke dysbacteriosis;
- intoxication (poisoning with lead, arsenic and its preparations, mushrooms);
- nervous and emotional tension, stress.
Colitis ulcerosa - all Stages
What can you do if you have colitis?
Treatment of any colitis begins with the appointment of a special diet. Further tactics depend on the specific cause of the disease. If the disease is caused by an intestinal infection, antibiotics may be prescribed. If colitis is caused by long-term use of drugs, the drugs are discontinued. For chronic colitis, antispasmodics (for example, no-spa), regulators of intestinal motility, antidiarrheals (for example, loperamide, imodium), anti-inflammatory drugs (for example, sulfasalazine), and in severe cases - glucocorticoid hormones are used.
Acute colitis: causes, symptoms, treatment
This form of the disease is caused by staphylococci, streptococci, salmonella and dysentery microorganisms . It also occurs as a result of common infections (influenza, acute respiratory viral infections, acute respiratory infections, measles), allergies or intolerance to certain medications (usually antibiotics). Often, with acute colitis, the stomach and small intestine become inflamed. As a result, according to the “domino principle,” the normal functioning of other organs of the gastrointestinal tract is disrupted. Depending on the nature of the damage to the large intestine, doctors diagnose several types of acute colitis, namely: catarrhal, ulcerative, erosive, and sometimes fibrinous .
The main symptoms include:
- cramping abdominal pain and bloating;
- the presence of mucus and blood in the stool;
- diarrhea (diarrhea).
The disease usually begins suddenly and, as a rule, with a bowel disorder. Patients feel sick and have no appetite . I am tormented by vomiting and constantly thirsty. They complain of general weakness, a sharp deterioration in health and fever . However, vomiting and diarrhea have their advantages: doctors attribute these manifestations to protective reactions. That is, in this way the body tries to get rid of the poisons that have gotten inside.
Symptoms of acute colitis may depend on the location of the inflammation. For example, when the left half of the colon is affected, pain manifests itself most sharply. Before defecation, they usually intensify and radiate to the perineum and sacrum. Stools are very frequent, up to 20 times a day (sometimes more). The stool has an uneven consistency: dense masses “float” in blood or copious mucus. The areas of the descending and sigmoid colon are painful to palpation. This is where rumbling and splashing sounds are detected.
Colitis
This symptomatology can manifest itself over several weeks and, if left untreated, the acute form usually becomes chronic. Such undesirable developments can be prevented with timely assistance.
Thus, treatment of acute colitis includes the following measures :
- drinking plenty of fluids to replenish fluid losses in the body . It is recommended to drink a specially prepared solution that is well absorbed by the intestines: add a teaspoon of salt and seven to eight teaspoons of sugar per liter of warm boiled water. You can drink mineral water and weak tea, but coffee is undesirable because it affects intestinal motility and increases diarrhea. In some severe cases, fluid is administered intravenously.
- therapeutic fasting for one to two days. Then a strict diet is indicated until the symptoms of the disease completely disappear.
- taking activated carbon. Prescribed for the absorption of toxins in the large intestine.
- taking enzyme preparations, enveloping and adsorbent substances.
- physiotherapeutic treatment.
Diagnostics
The complex of mandatory diagnostics includes macro- and microscopy of stool, coprogram, detection of helminth eggs, as well as bacteriological culture of stool. A general blood test is prescribed to determine the presence of signs of inflammation.
Contrast irrigoscopy is also performed to visualize the anatomical and functional features of the large intestine. Colonoscopy makes it possible to thoroughly examine the condition of the mucous membrane of the entire colon. During this study, it is also possible to obtain biopsies of the intestinal mucosa necessary for histological examination.
To exclude hemorrhoids, anal fissures, paraproctitis and other proctological pathologies, the proctologist performs a digital examination of the anus.
About the causes, symptoms and treatment of chronic colitis
Chronic colitis is a disease where the leading provoking factor is the presence of infection in the gastrointestinal tract . Its manifestations are “many-faced”. It occurs in the form of periodic exacerbations. The latter occur as a result of consuming foods that irritate the colon; manifestations of allergies; long-term use of various antibiotics; general fatigue.
The main symptoms of chronic colitis include:
- cramping pain in the abdomen (but does not always occur, more often accompanying the act of defecation);
- diarrhea alternating with constipation;
- secretion of mucus (in some cases mixed with blood);
- lack of appetite;
- nausea, belching of air, unpleasant taste in the mouth;
- a feeling of heaviness and distension in the abdomen (as a result of flatulence);
- a feeling of pressure in the epigastric region (often manifests itself in connection with gastritis);
- deterioration in general health (weakness, poor sleep, headaches, irritability, depressed mood).
Chronic colitis sometimes occurs as a consequence of functional disorders of the intestines (for example, with prolonged constipation). The causes also include dyskinesia (impaired motor function), which is associated with reflex effects from the gallbladder, bladder, prostate and other organs.
The basis for the treatment of chronic colitis (regardless of its etiology) is a dietary regimen. Drug therapy is effective only in cases where the cause is clearly established. When constructing a diet, the nature of dyspepsia (putrefactive or fermentative) and the state of the pancreas and its secretory function are taken into account . A too strict diet is not needed, as there is a risk of exhaustion and the development of hypovitaminosis, which will only complicate the course of colitis.
Strict dietary restrictions are allowed only during periods of exacerbation of the disease . Then foods that irritate the intestines both mechanically and chemically are excluded . Food is consumed boiled or pureed. Meals are split (6-7 times during the day). The consumption of table salt is limited (up to 8-10 g). Allowed: non-rich meat broth, steamed cutlets from lean meats, boiled fish (also low-fat), non-acidic cottage cheese, water porridge, juices, jelly. There is a strict taboo on black bread, spicy dishes, and various smoked foods. It is undesirable to eat lard and pork, goose meat and milk, sour cream, eggs, canned food, etc. Patients prone to diarrhea should not eat cold food, and the same applies to drinking.
If chronic colitis is accompanied by constipation, then the diet must include foods to stimulate intestinal function: minced meat, boiled vegetables and fruits.
Clinical picture
In world practice, the severity of an attack (exacerbation) of UC is assessed using the disease activity index. There are several indices of UC activity (Rakhmilevich, Mayo, Oxford index, Swedish index, Truelov and Witts severity rating system, Montreal classification). There is no consensus among experts regarding the preferability of using any particular index, since all of them are not sufficiently validated. Currently, there is a tendency to additionally use the level of C-reactive protein (CRP) to assess activity, which is reflected in the European consensus (ECCO-consensus) on the diagnosis and treatment of UC. This document discusses all indices, with experts making the following conclusion: currently, to assess the severity of UC, it is necessary to take into account all parameters of the disease - clinical, laboratory, instrumental and histological [4]. The Expert Council of the Russian Group for the Study of Inflammatory Bowel Diseases (IBD) proposes a set of criteria that includes easily determined parameters for exacerbation of UC, including the level of CRP. This complex is broader than what is usually used when assessing activity indices, and therefore is more informative. The set of assessed disease parameters, to a greater extent than any indices (section 2.2.2.), corresponds to the expert assessment of the ECCO-consensus and takes into account both clinical and laboratory manifestations of the disease. This scoring system is an expanded modification of the UC severity criteria proposed by Truelov and Witts [6]. In accordance with the severity of clinical and laboratory symptoms, mild, moderate and severe UC are distinguished (see table).
The clinical picture of UC includes several groups of symptoms [1]:
• intestinal (blood in the stool, diarrhea, tenesmus);
• systemic extraintestinal autoimmune manifestations (arthropathy, skin lesions, aphthous stomatitis, eye lesions, primary sclerosing cholangitis, etc.);
• endotoxemia syndrome (general intoxication, febrile fever, tachycardia, anemia, increased ESR, leukocytosis with a shift in the leukocyte formula to immature forms, toxic granularity of neutrophils, increased levels of acute-phase proteins - CRP, seromucoid, fibrinogen);
• metabolic disorders (weight loss, dehydration, hypoproteinemia, hypoalbuminemia, hypokalemia and other electrolyte disturbances).
Prevention of colitis
They say that disease is easier to prevent than to treat. Therefore, preventive measures are very important.
Prevention of acute colitis consists of following the norms of proper nutrition and a healthy lifestyle, maintaining hygiene and sanitary rules.
In the prevention of chronic colitis, special attention is paid to the prevention and timely treatment of acute colitis and especially dysentery. A large role in the prevention of diseases of the gastrointestinal tract is played by high-quality nutrition and, accordingly, maintaining the intestinal microflora in a healthy state . Not to mention the good condition of the chewing apparatus and strengthening of the nervous system.