Ulcerative colitis
- inflammatory bowel disease, which belongs to the group of immune-mediated chronic diseases of the large intestine.
Inflammatory bowel diseases are one of the most complex pathologies in modern gastroenterology and coloproctology. The treatment of these diseases is based on an interdisciplinary approach, and its effect depends entirely on the mutual understanding and productive interaction of gastroenterologists and coloproctologists, who develop a treatment strategy during a multidisciplinary consultation.
Ulcerative colitis is a chronic autoimmune inflammation of the colon mucosa. Usually the process starts from the rectum and then spreads to the overlying parts of the large intestine (sigmoid, descending, transverse colon, right colon). With extensive damage, the terminal ileum is involved in the pathological process (retrograde ileitis). The pathology is characterized by alternating periods of exacerbation and remission, as well as the development of local and systemic complications.
The disease can also be found under the name ulcerative colitis.
Causes of the disease
The exact etiology of the disease has not yet been determined. Ulcerative colitis is believed to occur when a number of factors interact. Among them: genetic predisposition, disorders of the immune system, imbalance of intestinal microflora and the influence of certain environmental factors.
Thus, the presence of ulcerative colitis or Crohn's disease in relatives increases the risk of its occurrence in the patient. However, genetic predisposition is not associated only with a mutation of one gene. Currently, 163 gene loci responsible for the development of ulcerative colitis or Crohn's disease have been identified. It is also known that genetic factors influence the severity of inflammation of the colon, the localization of the inflammatory process, the occurrence of complications and extraintestinal manifestations.
The state of the symbiont (normal) intestinal microflora plays an important role in the development of the disease. Normally, each gram of feces contains from 1010 to 1012 bacteria (approximately 400-500 species), i.e. up to 60% of the stool mass is represented by microorganisms. Immunocompetent cells of the mucous membrane constantly interact with the contents of the colon, ensuring the tolerance of bacteria. Impaired recognition of bacterial markers leads to activation of the inflammatory process and the onset of the disease.
It is also known that the first attack of ulcerative colitis or its recurrence can be triggered by food-borne antigens that cause allergies, or the cause can be stress.
Are there other surgical alternatives?
Today, a method has been adopted in world practice in which a reservoir is created from the small intestine, connected to the anus. Typically, in this case, it is necessary to form a temporary ileostomy, followed by its closure after a few months.
The reservoir, the so-called pouch, functions as a storage device to reduce the frequency of bowel movements. The use of this technique allows one to achieve physiological stool holding. In cases of complications in the form of inflammation of the reservoir, antibiotic therapy can be carried out, sometimes it is necessary to resort to removal and the creation of a permanent ileostomy.
Pathogenesis of ulcerative colitis
The development of the disease is ensured by various mechanisms of tissue and cellular damage. This leads to immunological imbalance, release of pro-inflammatory mediators and tissue damage. The resulting antigens (bacterial and tissue) cause stimulation of cells of the immune system (T- and B-lymphocytes). Inflammation leads to a deficiency of immunoglobulins. As a result, these processes increase the activity of B cells with the release of immunoglobulins M and G and promote the penetration of microorganisms.
Active synthesis of immunoglobulins M and G is accompanied by the formation of immune complexes and activation of the complement system, which exhibits a cytotoxic effect and causes the migration of neutrophils and macrophages. Immunocompetent cells release inflammatory mediators, causing the destruction of epithelial cells.
In addition to the pathological reaction of the immune system, epithelial tissues are damaged under the influence of active oxygen and protease, which leads to activation of the cell death mechanism.
Defects in the intestinal mucosa also play an important role in the development of the disease. The impaired ability to restore the mucous membrane and damage to its barrier function enable various bacterial and food antigens to penetrate deep tissues, triggering a chain of immune and inflammatory reactions.
The psychological characteristics of the patient’s personality, especially emotional instability, are also important. The trigger for the development of the disease can be an abnormal neurohumoral response obtained during the individual reaction to stress.
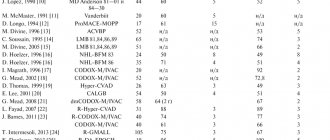
Literature
- Adler DJ, Korelitz BI. The therapeutic e.cacy of 6-mercaptopurine in refractory ulcerative colitis. Am J Gastroenterol 1990;85:717-22.
- Ardizzone S, Molteni P, Imbesi V, Bollani S, Bianchi Porro G, Molteni F. Azathioprine in steroid-resistant and steroid-dependent ulcerative colitis. J Clin Gastroenterol 1997; 25:330-3.
- Bianchi Porro G, Prantera C, Campieri M, Petrillo M, Campanini MC, Gionchetti P et al. Comparative trial of methylprednisolone and budesonide enemas in active distal ulcerative colitis Eur J Gastroenterol Hepatol 1994;6:125-30.).
- Faubion WA Jr, Loftus EV Jr, Harmsen WS, et al.: The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology 2001, 121: 255-260.
- Gionchetti P, Rizzello F, Venturi A, et al. Comparison of oral with rectal mesalazine in the treatment of ulcerative proctitis. Dis Colon Rectum 1998;41:93-7.
- Green JRB, Lobo AJ, Holdsworth CD, et al. Balsalazide is more effective and better tolerated than mesalamine in the treatment of acute ulcerative colitis. Gastroenterology. 1998; 114:15-22.
- Guslandi M, Frego R, Viale E, Testoni PA: Distal ulcerative colitis refractory to rectal mesalamine: role of transdermal nicotine versus oral mesalamine. Can J Gastroenterol 2002, 16:293-296.
- Limann M, Galian A, Rutgeerts P, van Heuverzwijn R, Cortot A, Viteau JM et al. Comparison of budesonide and 5-aminosalicylic acid enemas in active distal ulcerative colitis. Aliment Pharmacol Ther 1995; 9: 557-62.
- Lichtiger S, Present DH. Preliminary report: Cyclosporin in treatment of severe active ulcerative colitis. Lancet 1990;336:16-9.
- Lichtiger S, Present DH, Kornbluth A, et al. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N Engl J Med 1994;330:1841-5.
- Marshall JK, Irvine EJ. Rectal corticosteroids versus alternative treatments in ulcerativecolitis: A meta-analysis. Gut 1997;40:775-81.
- Mulder CJ, Fockens P, Meijer JW, et al. Beclomethasone dipropionate (3 mg) versus 5-aminosalicylic acid (2 g) versus the combination of both (3 mg/2 g) as retention enemas in active ulcerative proctitis. Eur J Gastroenterol Hepatol 1996;8:549-53.).
- Odes HS, Fich A, Reif S, et al.: Effects of current cigarette smoking on the clinical course of Crohn's disease and ulcerative colitis. Dig Dis Sci 2001, 46: 1717-1721.
- Panes J, Esteve M, Cabre E, et al.: Comparison of heparin and steroids in the treatment of moderate and severe ulcerative colitis. Gastroenterology 2000, 119: 903-908.
- Pruitt R, Hanson J, Safdi M, et al. Balsalazide is superior to mesalamine in the time to improvement of signs and symptoms of acute ulcerative colitis. Gastroenterology. 2000; 118(Suppl 2 Part 1): A120-1.
- Rufle W, Fruhmorgen P, Huber W, Kimmig JM: Budesonide foam as a new therapeutic principle in distal ulcerative colitis in comparison with mesalazine enema: an open, controlled, randomized and prospective multicenter pilot study. Z Gastroenterol 2000, 38:287-293.
- Safdi M, DeMicco M, Sninsky C, et al. A double-blind comparison of oral versus rectalmesalamine versus combination therapy in the treatment of distal ulcerative colitis. Am J Gastroenterol 1997;92:1867-71.
- Sandborn W, Tremaine W, Leighton J, et al. Nicotine tartrate liquid enemas for mildly to moderately active left-sided ulcerative colitis unresponsive to .rst-line therapy: A pilot study. Aliment Pharmacol Ther 1997;11:661-71.
- Sutherland L, MacDonald JK Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database Syst Rev (England), 2003, (3) pCD000543.
- Vrij AA, Jansen JM, Schoon EJ, et al.: Low molecular weight heparin treatment in steroid refractory ulcerative colitis: clinical outcome and influence on mucosal capillary thrombi. Scand J Gastroenterol 2001, 234(Suppl): 41-47.
Manifestations of the disease
Ulcerative colitis is characterized by a wide variety of clinical manifestations. The Montreal classification helps to systematize manifestations (Table 1). According to it, it is possible to assess the characteristics of the course of the disease, the extent of the lesion, the severity of the attack and the presence of complications.
| Proctitis | The lesion is limited to the rectum |
| Left-sided colitis | The lesion extends to the left flexure of the colon (including proctosigmoiditis) |
| Total colitis | (Including subtotal colitis, as well as total UC with retrograde ileitis) |
Table 1. Montreal classification of ulcerative colitis by extent of lesion.
The course of ulcerative colitis is characterized by three options:
- Acute course (less than 6 months from the onset of the disease). It can occur with a fulminant (quick) or gradual onset.
- Chronic continuous course, which is characterized by the absence of more than 6-month periods of remission against the background of adequate therapy.
- Chronic relapsing course (presence of more than 6-month periods of remission). It can be either rarely recurrent (once a year or less) or frequently recurrent (2 or more times a year).
The presence of extraintestinal manifestations, the development of complications, the intensity and severity of the current exacerbation and the emergence of resistance to treatment in the patient (for example, hormonal dependence) determines the severity of ulcerative colitis.
The severity of the current exacerbation or attack is also used to create a treatment plan and formulate a diagnosis. In clinical practice, the Truelove-Witts criteria and the disease activity index (Mayo index) are used for this purpose. There are three levels of attack: light, medium, heavy.
The course of ulcerative colitis has periods of exacerbation (relapse) and remission.
Relapse (exacerbation or attack) is characterized by the appearance of symptoms of the disease against the background of remission, which was achieved through medication or occurred spontaneously. If a relapse occurs less than 3 months after remission, then it is considered early. Signs of relapse: an increase in the frequency of bowel movements with the release of blood, as well as changes in the colon mucosa, which are found during endoscopic examination.
Remission of ulcerative colitis involves healing of the colon mucosa in the absence of the main symptoms of the disease.
What is the range of possible surgical interventions?
The range of surgical interventions in case of ineffectiveness of drug treatment and diet for nonspecific ulcerative colitis includes several types of operations. In our clinic you can receive high-quality treatment, whatever the causes of UC and its consequences in a particular case. Doctors will choose the most appropriate type of intervention for each patient. One operation is enough to completely eliminate the disease.
Sometimes the doctor will consider removing the colon while preserving the rectum and anus. At the same time, holding the chair is maintained. The disadvantage of this method is that it maintains the risk of developing colitis and cancer in the remaining part of the rectum.
Treatment of ulcerative colitis
Ulcerative colitis requires complex treatment, which includes drug therapy, surgical treatment if complications occur, and a special diet. The choice between a conservative and surgical method takes into account a number of criteria. These include: the extent of damage to the colon, the severity of the exacerbation, the effectiveness of the therapy already carried out, the presence of extraintestinal manifestations and complications.
The main goal of treatment for ulcerative colitis is to achieve long-term and stable remission, healing of the colon mucosa, prevention of surgical complications, and improvement of the patient’s quality of life. If the disease progresses or life-threatening complications develop, surgical treatment is performed.
When remission is achieved, the patient should remain on maintenance (anti-relapse) pharmacotherapy. It is important to note that glucocorticosteroids should not be used as maintenance therapy. They are used in severe attacks to induce remission, and then the patient must be switched to drugs of other groups (5-ASA, cytostatics, biological therapy, etc.)