Pantoprazole Canon, 28 pcs., 20 mg, enteric-coated tablets
Inside.
The tablet should be swallowed whole, without chewing or breaking, with a small amount of liquid, before meals, usually before breakfast. When taken twice, the second dose of the drug is recommended to be taken before dinner.
Peptic ulcer of the stomach and duodenum, erosive gastritis (including those associated with taking NSAIDs)
The recommended dose is 40–80 mg per day. The course of treatment is 2 weeks for exacerbation of duodenal ulcer and 4–8 weeks for exacerbation of gastric ulcer.
Anti-relapse treatment of gastric and duodenal ulcers - 20 mg/day.
Helicobacter pylori eradication
The following combinations are used as triple therapy:
1. Pantoprazole Canon 20–40 mg 2 times a day + amoxicillin 1000 mg 2 times a day + clarithromycin 500 mg 2 times a day. The course of treatment is 7–14 days.
2. Pantoprazole Canon 20–40 mg 2 times a day + metronidazole 500 mg 2 times a day + clarithromycin 500 mg 2 times a day. The course of treatment is 7–14 days.
3. Pantoprazole Canon 20–40 mg 2 times a day + amoxicillin 1000 mg 2 times a day + metronidazole 500 mg 2 times a day. The course of treatment is 7–14 days.
After the end of combination therapy, taking Pantoprazole Canon can be continued for the purpose of healing the ulcer. For duodenal ulcers, taking Pantoprazole Canon can be extended from 1 to 3 weeks.
For patients with severe renal impairment (Cl creatinine <20 ml/min) or on hemodialysis, Helicobacter pylori
not assigned.
Treatment of mild GERD symptoms (such as heartburn, nausea, sour belching)
The recommended dose of the drug is 20 mg/day. To achieve positive dynamics in eliminating symptoms, it may be necessary to take the drug for 2-3 days, but to completely eliminate symptoms, it may be necessary to take the drug for 7 days. If the condition worsens during the first 3 days of treatment, consultation with a specialist is recommended. The drug should be stopped immediately after symptoms disappear.
Zollinger-Ellison syndrome
The recommended dose is 40–80 mg per day. In patients with severe liver dysfunction, the dose should be reduced to 40 mg once every 2 days. In this case, it is necessary to monitor biochemical blood parameters. If the activity of liver enzymes increases, the use of the drug should be discontinued.
Elderly patients
No dose adjustment is required. However, elderly patients should not exceed a daily dose of 40 mg. An exception is the use of combination antimicrobial therapy against Helicobacter pylori
, when elderly patients should also use the drug Pantoprazole Canon 40 mg 2 times a day.
Patients with kidney failure
Patients with severe renal impairment (creatinine clearance <20 ml/min) or those on hemodialysis should not exceed a daily dose of 40 mg. , Helicobacter pylori eradication therapy
is not prescribed to such patients.
You should not take Pantoprazole Canon for prophylactic purposes.
Efficacy and safety of pantoprazole in the treatment of acid-related diseases
Acid-dependent diseases (ADDs) include functional and organic diseases of the digestive organs, in the pathogenesis of which the level of acid formation in the stomach plays a crucial role. Accordingly, effective treatment of these diseases is possible only with a significant and long-term decrease in the acidity of gastric juice.
When taking antacids, for the required level of neutralization of hydrochloric acid, they must be taken at intervals of 2–3 hours. Fast-acting antacids, when interacting with hydrochloric acid, form carbon dioxide, which, due to distension of the stomach and increased pressure in it, increases the risk of regurgitation and aspiration of gastric contents with the possible development of acute lung injury syndrome (acute respiratory distress syndrome), and may also cause a secondary increase in hydrochloric acid secretion acids. Along with this, all antacids do not have antipepsin activity, do not reduce the secretion of hydrochloric acid, and therefore are not effective for the prevention and relief of bleeding from stress ulcers and erosions. Their simultaneous oral administration with other drugs is unacceptable due to impaired absorption of these drugs [1].
H2 receptor blockers are competitive histamine antagonists. These drugs are capable of significantly blocking basal secretion, but their activity on stimulated secretion is much lower than that of proton pump inhibitors (PPIs) [1]. In addition, H2 blockers bind to the receptor reversibly, so to ensure a lasting effect it is necessary that their significant concentration is constantly maintained in the blood. The drugs block only the histamine pathway of secretion activation, leaving choline, gastrin and other receptors alternatively capable of activation. After using H2 blockers, secretion occurs, which can lead to relapse of the disease. When using H2 blockers, the phenomenon of “receptor fatigue” develops (tachyphylaxis effect), which is accompanied by a rapid loss of antisecretory activity and requires an increase in dose with an increased risk of side effects [1–5].
In 7% of hospitalized patients, when prescribed H2-blockers, anxiety, disorientation, delirium, and hallucinosis are noted, which is extremely undesirable in patients with encephalopathy [1]. The use of H2 receptor blockers can lead to negative chrono- and inotropic effects, rhythm and conduction disturbances, and cause leukopenia, thrombocytopenia, agranulocytosis, pancytopenia, bone marrow hypoplasia and aplasia.
The most effective and safe secretion inhibitors are currently considered to be PPIs, which provide an optimal level of secretion reduction (pH > 4.0) and long-term preservation of the achieved effect (more than 18 hours) and cause the least number of undesirable side effects.
All PPIs are 2-pyridylmethylsulfonylbenzimidazoles, differing in the nature and position of the substituents located in the pyridine and benzene rings. The exception is esomeprazole, which is pure S-omeprazole. Changing the position and structure of substituents in PPI molecules leads to changes in the pyridine ring, which affects the pK value (pK is the pH value at which 50% of the compound is protonated) of the nitrogen of this ring.
All substituted benzimidazoles are weak bases, that is, they are able to bind H+ in an acidic environment. The mechanism of action of PPIs, regardless of their structure, is the same - the compounds formed from them, in an acidic environment, covalently bind to the SH groups of the alpha subunit of H+/K+-ATPase due to the formation of an S–S bond.
The S–S bond is covalent; for this reason, substituted benzimidazoles are irreversible PPIs. Removal of inhibition following covalent binding of the tetracyclic sulfenamide occurs only after the proton pump molecule is eliminated by proteolysis.
Dosage forms of PPIs are coated with an acid-resistant coating and begin to be absorbed in the small intestine. The molecules of substituted benzimidazoles have no charge and are hydrophobic, so they penetrate cell membranes quite easily. Once in the blood, substituted benzimidazoles are quickly redistributed between various tissues. When they enter a solution whose pH value is lower than the pK of the nitrogen of the pyridine ring, they are protonated, with H+ bonding to the nitrogen atom of the pyridine ring. H+ binding makes the molecule positively charged, as a result of which it is unable to penetrate membranes. As a result, protonated PPIs accumulate in those cell compartments that have a pH below the pK value for a given PPI. In cellular tubules, the pH is 0.8–1.0, so PPIs primarily accumulate in the secretory tubules of parietal cells, their concentrations there can be 1000 times higher than their concentration in the blood.
The concentration of PPIs in the secretory tubules of parietal cells is a factor in ensuring the selectivity of their action and explains their high safety, which is a specific property characteristic of this class of drugs, since they are precursors of the drug, that is, they are inactive in the form in which they are used.
Let us recall that, accumulating in the secretory tubules of the parietal cell, PPIs are converted into sulfenamide derivatives, irreversibly blocking the enzyme, binding through a covalent bond at the 813th position with cysteine molecules of H+/K+-ATPase. Blockade of the proton pump leads to the suspension of the synthesis of hydrochloric acid, regardless of the nature and strength of the factors stimulating the parietal cell. It was found that pantoprazole binds to two cysteine molecules of the proton pump (813 and 822), having a much more intense effect on the H+/K+-ATPase. Cysteine 822, which is deeper in the transport domain of the gastric acid pump, is a critical link in ensuring the stability of binding and the time of inhibition of the proton pump, which leads directly to the blockade of hydrochloric acid production [6]. Perhaps this is why, as a result of a stronger connection with H+/K+-ATPase in humans, the half-life of inhibition of acid secretion after taking pantoprazole is about 46 hours, lansoprazole - about 15 hours, omeprazole and rabeprazole - about 30 hours [7, 8]. Consequently, pantoprazole produces the longest-lasting suppression of acid secretion compared to other drugs in its class. This effect of pantoprazole makes it a very reliable treatment for CDZ [1–5, 9].
In an experiment on rats administered various PPIs, the cessation of drug action was determined by the restoration of proton pump activity after incubation for 1 hour with reducing agents such as dithiothreitol or glutathione. Complete reactivation of ATPase activity after its inhibition in vivo by omeprazole, esomeprazole and rabeprazole occurred within 1 hour; activity was restored by 60–70% after its inhibition by lansoprazole. However, during this period, no reactivation was observed after the administration of pantoprazole [9]. This may be due to the binding of pantoprazole to cysteine 822.
Another effect that provides a long-lasting and pronounced antisecretory effect of pantoprazole is the significantly (p < 0.05) largest area under the curve describing the dependence of the drug concentration in the blood on time (AUC) compared to other PPIs [10]. Thus, for pantoprazole the value of this indicator is 12.0 ± 3.5 mol/(l×h), for rabeprazole - 2.0 ± 0.8; for lansoprazole - 5.0 ± 1.7; for omeprazole - 1.3 ± 0.3; for esomeprazole - 5.2 ± 1.4 mol/(l×h), respectively. Due to the high AUC values, it is possible to inhibit the proton pump with pantoprazole during the day.
In a large number of cases, patients suffer from multiple organ pathologies and take a large number of often vital medications. This situation greatly increases the potential for their various interactions, which are a common cause of treatment failure and adverse drug reactions. The potential risk of unwanted drug interactions when taking two drugs simultaneously is 6%, with 5 - 50%, and with 8 it reaches 100% [11].
As a result of the simultaneous use of PPIs and a number of drugs, an increase in the concentration of drugs in the blood plasma and a decrease in their elimination were noted, as a result of which symptoms of the toxic effect of drugs with which the PPI interacts may develop. At the same time, the simultaneous use of PPIs and drugs can reduce the absorption of the drug with which the PPI interacts; on the other hand, in some cases, joint use can lead to an increase in the concentration of PPIs and the occurrence of side effects or PPI overdose [12].
Differences in the metabolism of PPIs may play a significant role in the effectiveness of the treatment of CDZ. About 98% of pantoprazole is bound to plasma proteins. A significant amount of it is metabolized in the liver. However, compared with other PPIs, the affinity of pantoprazole for the cytochrome P450 metabolizing system is very low [13]. PPI metabolism occurs in the liver with the participation of two isoforms of cytochrome P450 - CYP2C19 and CYP3A. Most of omeprazole is metabolized via the enzyme CYP2C19, and a smaller portion (about 10%) via CYP3A4 [14]. In subsequent generations of PPIs, this dependence also persists, but is less pronounced; for example, rabeprazole has a non-enzymatic pathway. Pantoprazole is metabolized mainly by CYP2C19 (subfamily of cytochrome P450) and to a lesser extent by CYP 3A4, 2D6 and 2C9. A number of human studies have shown the absence of pharmacokinetic or pharmacodynamic interactions between pantoprazole and medications metabolized primarily by CYP2C19, CYP2C9, CYP3A, CYP3A4 or other CYP isoenzymes [1–3, 15]. Accordingly, the ability of pantoprazole to interact with other simultaneously administered drugs is very low due to its low affinity for the metabolizing isoenzyme cytochrome P450 [13], which distinguishes this PPI from other drugs in this group (Table). Thus, drug interactions with pantoprazole were not identified in more than 50 studies [15].
When doubling the dose of PPIs, which have nonlinear pharmacokinetics, their serum concentrations are unpredictable. This may result in inadequate control of acid secretion or affect the safety of use of the drug. The use of pantoprazole, which has linear pharmacokinetics, allows for optimal treatment that corresponds to the severity of the disease and the general condition of the patient. The drug does not require dose adjustment in elderly people with liver and kidney failure; unlike omeprazole and esomeprazole, it does not accumulate in the body after taking repeated doses. Pantoprazole has a dosage form for parenteral administration [1–3].
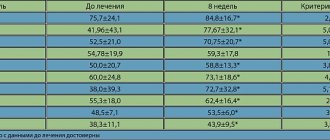
It is probably these properties of pantoprazole that determined the greater clinical effectiveness and safety of this PPI in a number of studies conducted from the standpoint of evidence-based medicine. A multicenter, randomized, double-blind study compared the effectiveness of treatment with pantoprazole (40 mg/day) and esomeprazole (40 mg/day) in 247 patients with varying degrees (from moderate to severe) of gastroesophageal reflux. After 4 weeks of treatment, symptom relief was comparable for both drugs, but it occurred significantly earlier with pantoprazole (3.7 vs. 5.9 days; p = 0.034) [16].
In patients with varying degrees (from moderate to severe) of GERD, it was shown that when treated with pantoprazole at a dose of 40 mg/day, a very high cure rate is achieved - more than 70% of patients after 4 weeks and more than 90% of patients after 8 weeks [17] . It should be noted that comparable results were obtained when treating such patients with pantoprazole (40 mg/day) and esomeprazole (40 mg/day).
The results of recent studies on the effectiveness of using pantoprazole for the correction of extraesophageal manifestations of GERD are extremely interesting. A prospective, open-label, multinational, multicenter study of 1888 patients with gastroesophageal reflux disease (GERD) identified features of irritable bowel syndrome. During treatment with pantoprazole at a dose of 40 mg per day for 8 weeks, a pronounced and significant decrease in the severity of manifestations of not only GERD, but also irritable bowel syndrome was noted [18]. In an open-label, prospective study, 33 patients with GERD and chronic pharyngitis and laryngitis received pantoprazole 80 mg/day daily for 8 weeks. There was a significant decrease in the duration of distal acidification of the esophagus (19.4% versus 7.2%), the total number of refluxes (62.7 versus 28.4) and the number of refluxes lasting more than 5 minutes (10.4 versus 3.9, p for all cases <0.0001), disappearance of symptoms of chronic pharyngitis and laryngitis was detected in 51.5% of cases [19]. Sleep apnea syndrome is a serious extraesophageal manifestation of GERD, in some cases causing fatal and non-fatal cardiac events. We describe the results of a prospective study that included 199 patients with nocturnal sleep disturbance due to GERD. Prescription of pantoprazole contributed not only to significant relief of GERD, but also to improvement of clinical and polysomnographic sleep parameters in 78% of patients [20].
Clinical studies performed with a high level of evidence, including several meta-analyses, have shown that eradication therapy for Helicobacter pylori infection prevents the recurrence of H. pylori-associated gastric and/or duodenal ulcers and reduces the risk of such complications, such as bleeding [4, 5]. None of the available anti-Helicobacter therapy regimens leads to 100% eradication; most of them have side effects. The Maastricht-4 consensus confirmed a decrease in the effectiveness of the triple eradication therapy regimen over the past 13 years (from 1995 to 2008) from 90.6% to 74.8%.
The urgent task today is to search for more effective treatment regimens for H. pylori infection; often it is the choice of one or another PPI that is important for practical use.
Our department conducted a study that included 105 patients with duodenal ulcer associated with H. pylori, randomized into two groups. In group 1, 35 patients were prescribed pantoprazole, amoxicillin, and clarithromycin in standard dosages for 7 days. In group 2, 70 patients were prescribed omeprazole, amoxicillin, and clarithromycin in standard dosages for 7 days. In the pantoprozole group, 29 (82.9%) of 35 patients achieved eradication of H. pylori infection within the control period. Thus, the minimum acceptable level of effectiveness of anti-Helicobacter therapy was exceeded in 80% of cases. In the omeprazole group, the eradication rate was significantly and significantly lower (47 out of 70 patients, which was 67.1%, p < 0.05) [4, 5].
Sequential therapy is currently of great interest. A recent prospective, controlled study included 409 patients with H. pylori infection. The first group received 10 days of sequential therapy, which included pantoprazole 40 mg daily and amoxicillin 1000 mg twice daily for 5 days, followed by pantoprazole, clarithromycin 500 mg and metronidazole twice daily for the next 5 days. The second group used first-line triple therapy, including pantoprazole 40 mg daily, amoxicillin 1000 mg and clarithromycin 500 mg twice daily for 14 days. There was a significant predominance of successful eradication therapy when using a sequential regimen. The intention to treat rate was 85.9% (176/205) and 75.0% (153/205), respectively (p = 0.006). The per protocol rate was 92.6% (175/205) and 85% (153/204), respectively (p = 0.019), with no difference in the incidence of adverse side effects (18.9% and 13.3%, respectively, p = 0.143) [21]. It is noteworthy that the use of pantoprazole in a standard triple regimen also made it possible to exceed the minimum acceptable level of effectiveness of anti-Helicobacter therapy in per protocol analysis.
It is known that the mortality associated with complications of stress ulcers is high, which requires emergency measures for their prevention and relief. Moreover, the combination of a pronounced and long-term antisecretory effect with a low level of interaction with other drugs, the absence of a cumulative effect, and the presence of a dosage form for parenteral administration allow the drug to be used in a complex of means for the prevention of stress ulcers and bleeding from them, promote their scarring, improving patient survival [2 , 3, 22]. Thus, after intravenous administration, pantoprazole begins to act within 15 minutes, and administration of 80 mg suppresses secretion by 86% after 60 minutes [23].
Accordingly, the above qualities make the dosage form of pantoprazole for parenteral administration the drug of choice for use in a complex of means for the prevention of ulcer bleeding. In this context, we would like to mention two studies published in 2012 and 2010 on the effect of intravenous administration of different doses of pantoprazole to patients after endoscopic hemostasis for ulcer bleeding. A retrospective case-control study of 413 patients showed that low-dose intravenous pantoprazole was as effective as high-dose intravenous pantoprazole in preventing recurrent bleeding [24]. A randomized controlled trial that included 120 patients showed a similar high preventive effect of intravenous administration of pantoprazole at a dose of 192 mg and 40 mg 4 times a day for 3 days [25]. This “paradox” is probably associated with the high effectiveness of the drug in normal doses.
A retrospective and observational study of 807 patients with ulcer bleeding found similar prophylactic potential for rebleeding with intravenous pantoprazole and intravenous omeprazole. However, the use of pantoprazole had better pharmacoeconomic indicators [26].
Observation of 164 patients who suffered bleeding from the upper digestive tract, not associated with esophageal varices, led to the conclusion that endoscopic treatment in combination with intravenous pantoprazole 80 mg bolus followed by drip administration at a rate of 8 mg per day for 3 days has a significantly more pronounced effect than the combination of endoscopic treatment and intravenous administration of omeprazole at the same dose. Thus, rebleeding occurred in 3.7% in the pantoprazole group and in 10.2% in the omeprazole group (p = 0.022), blood transfusions were performed in 25% and 50% of cases (p < 0.001), the length of hospital stay was 4 .6 ± 1.2 and 7.1 ± 0.8 days, respectively (p < 0.001). Surgical treatment for uncontrolled bleeding was required in 1 patient out of 81 and 4 out of 83; death occurred in 1 and 2 cases, respectively [27].
In our opinion, it would be appropriate to mention a number of studies in recent years that confirm the data described above about the high safety of the drug and its low metabolic interaction with other drugs.
In a pilot study, a crossover, double-blind, randomized, placebo-controlled study, 10 hemodialysis patients received pantoprazole 40 mg daily or placebo for 6 weeks. In patients receiving pantoprazole, plasma levels of phosphate, calcium, bicarbonates and parathyroid hormone did not differ from those in patients who were given placebo [27], but the small number of patients in the sample does not allow us to draw firm conclusions.
One of the most important components of primary, secondary and tertiary prevention in cardiology and cardiac surgery is the constant use of antithrombotic drugs. At the same time, a number of PPIs can worsen the antithrombotic effect of these drugs. Thus, omeprazole can significantly reduce the inhibitory effect of clopidogrel on platelet P2Y12 receptors, increasing the number of patients resistant to clopidogrel [28].
The safety of the combination of antithrombotic drugs and pantoprazole has been proven by monitoring healthy volunteers and cardiac patients. In a prospective, randomized crossover study involving 20 healthy volunteers, the dose of pantoprazole was 80 mg per day, clopidogrel 600 mg as a single loading dose, then 75 mg per day. Moreover, pantoprazole, used in high doses, did not change the pharmacodynamic effects of clopidogrel at all [28].
A continuation of the work described above was a randomized crossover study that included 34 patients who had suffered acute myocardial infarction one month before the start of observation. After a month of “washing out,” patients received 40 mg of omeprazole or pantoprazole for a month; after a month of “washing out,” PPIs were prescribed in a crossover design. There was a significant decrease in the effect of clopidogrel when taking omeprazole, P2Y12 response units (PRU) increased from 202 ± 52 to 235 ± 58 (p < 0.001). While taking pantoprazole, the effectiveness of clopidogrel was maintained (PRU = 215 ± 54, p = 0.16). During the PPI-free period, 26% of patients were resistant to clopidogrel (PRU > 240); when taking omeprazole, their value increased by 45% versus 23% when taking pantoprazole. It was concluded that, unlike omeprazole, pantoprazole does not interact with clopidogrel [29].
To conclude the topic, it is necessary to mention a comparative study that included 44 patients with stable angina after percutaneous implantation of stents who received standard dual therapy with Aspirin and clopidogrel. 23 patients, along with standard therapy, received 20 mg of pantoprazole for a month. 21 patients were prescribed only standard dual antithrombotic therapy. Platelet function was assessed using impedance aggregometry. Analysis of the data obtained revealed a complete lack of influence of pantoprazole on the effect of antithrombotic therapy [30].
A randomized, double-blind, crossover study examined the interaction of a single dose of intravenous diazepam with 11 days of 40 mg/day esomeprazole or pantoprazole in healthy subjects. In individuals receiving esomeprazole, the AUC, Cmax and t1/2 values of diazepam were higher by 28.0%, 31.4% and 41.1%, respectively, compared with those taking pantoprazole. Pharmacodynamic parameters determined by oculodynamic study were significantly and significantly worse in the esomeprazole group compared to the pantoprazole group. The authors concluded that there is a possibility of undesirable interactions between esomeprazole and diltiazem and a high safety profile of pantoprazole [31].
The above data allows us to draw a number of conclusions. Pantoprazole is a highly effective and safe treatment for acid-related diseases. A long-lasting and pronounced antisecretory effect, along with providing a pronounced clinical effect, allows one to avoid such a “minus” as nighttime acid breakthrough, or a sharp increase in hydrochloric acid production in forgetful patients (skipping a scheduled dose of the drug). This drug can be regarded as the drug of choice in patients receiving several drugs at the same time, in severely ill patients, especially when it is impossible to take medications orally, in patients with liver and kidney failure, in the elderly, for the prevention and relief of stress ulcers, ulcerative bleeding. This drug does not worsen the antithrombotic effect in cardiac patients who have undergone cardiac surgery. The drug has been proven to be highly effective in relieving not only esophageal but also extraesophageal manifestations of GERD.
Literature
- Antonenko O. M. The place of proton pump inhibitors in the prevention of stress damage to the gastrointestinal tract in critically ill patients // Consillium medicum. 2009, no. 1.
- Yakovenko E. P., Levchuk A. L., Yakovenko A. V. et al. Stress ulcers: prevention and treatment // Farmateka. 2009, no. 2, p. 40–43.
- Yakovenko E. P., Yakovenko A. V., Illarionova et al. Pantoprazole in the treatment of acid-related diseases // Farmateka. 2012, no. 2, p. 45–50.
- Maev I.V., Kucheryavyi Yu.A., Oganesyan T.S. Pantoprazole: significance and place in the treatment of acid-related diseases // Breast Cancer. 2010, vol. 18, no. 28 (392), p. 1749–1753.
- Maev I.V., Oganesyan T.S., Kucheryavyi Yu.A. Comparative effectiveness of first-line triple anti-Helicobacter therapy using pantoprazole and omeprazole // Treating Physician. 2010; 2:92–95.
- Modlin I. & Sachs G. Acid Related Diseases, Schnetztor-Verlag GmbH, Konstanz, 1998.
- Gedda K., Besancon M., Lorentzon P., Sachs G. Turnover of the gastric H+, K (+)-adenosine triphosphatase alpha subunit and its effect on inhibition of rat gastric acid secretion // Gastroenterology. 1995. Vol. 109, p. 1134–1141.
- Katashima M., Yamamoto K., Tokuma Y. et al. Comparative pharmacokinetic/pharmacodynamic analysis of proton pump inhibitors omeprazole, lansoprazole and pantoprazole, in humans // Eur. J. Drug Metab. Pharmacokinet. 1998. Vol. 23 (1), p. 19–26.
- Sachs G., Shin JM, Pratha V., Hogan D. Synthesis or rupture: duration of acid inhibition by proton pump inhibitors // Drugs Today (Barc). 2003. Vol. 39, Suppl A, p. 11–14.
- Wolfe MM, Welage LS, Sachs G. Proton pump inhibitors and gastric acid secretion. Am J Gastroenterol // 2001. Vol. 96(12), p. 3467–3468.
- Johnson AG, Seidemann P., Day RO NSAID-related adverse drug interactions with clinical relevance. An update // Int. J. Clin. Pharmacol. Ther. 1994, Oct; 32(10):509–532.
- Farber A.V., Nikonov E.L. Use of off-label proton pump inhibitors // Pharmateka. 2010, no. 2, p. 94–99.
- Maton P., Burton M. Clinician's Manual on Drug Interactions in Gastroenterology, Life Science Communication, 1996.
- Giannini EG, Savarino V., Testa R. Monitoring cytochrome P–450 activity during rabeprazole treatment in patients with gastresophageal reflux disease // Dig. Dis. Sci. 2006. Vol. 51, p. 1602–1609.
- Blume H., Donath F., Warnke A., Schug BS Pharmacokinetic drug interaction profiles of proton pump inhibitors // Drug Safety. 2006. Vol. 29 (9), p. 769–784.
- Scholten T., Gatz G., Hole U. Once-daily pantoprazole 40 mg and esomeprazole 40 mg have equivalent overall efficacy in relieving GERD-related symptoms // Aliment Pharmacol Ther. 2003, Sep 15; 18(6):587–594.
- Bardhan KD Pantoprazole: a new proton pump inhibitor in the management of upper gastrointestinal disease // Drugs Today (Barc). 1999. Vol. 35 (10), p. 773–808.
- Monnikes H., Heading RC, Schmittand H., Doerfler H. Influence of irritable bowel syndrome on treatment outcome in gastroesophageal reflux disease // World J. Gastroenterol. 2011. Vol. 17 (27), p. 3235–3241.
- Karoui S., Bibani N., Sahtout S. Effect of pantoprazole in patients with chronic laryngitis and pharyngitis related to gastroesophageal reflux disease: clinical, proximal, and distal pH monitoring results // Dis. Esophagus. 2010. Vol. 23(4), p. 290–295.
- Modolell I., Esteller E., Segarra F., Mearin F. Proton-pump inhibitors in sleep-related breathing disorders: clinical response and predictive factors // Eur J Gastroenterol. Hepatol. 2011. Vol. 23 (10), p. 852–858.
- Kim YS, Kim SJ, Yoon JH Randomised clinical trial: the efficacy of a 10-ay sequential therapy vs. a 14-ay standard proton pump inhibitor-based triple therapy for Helicobacter pylori in Korea // Aliment Pharmacol Ther. 2011. Vol. 34 (9), p. 1098–1105.
- Zolotovskaya N. B., Leiderman I. N. Prevention of stress gastrointestinal bleeding in patients with acute necrotizing pancreatitis // Anesthesiology and Reanimatology. 2011. No. 6, p. 74–78.
- Simon B., Muller P., Bliesath H. et al. Single intravenous administration of the H+, K (+)-ATPase inhibitor BY 1023/SK&F 96022—inhibition of pentagastrin-stimulated gastric acid secretion and pharmacokinetics in man // Aliment. Pharmacol. Ther. 1990. Vol. 4 (3), p. 239–245.
- Liang CM, Lee JH Kuo YH et al. Intravenous non-high-dose pantoprazole is equally effective as high-dose pantoprazole in preventing rebleeding among low risk patients with a bleeding peptic ulcer after initial endoscopic hemostasis // BMC Gastroenterol. 2012. Vol. 28, p. 12:28.
- Hsu Y.-C., Perng C.-L., Yang T.-H. et al. A randomized controlled trial comparing two different dosages of infusional pantoprazole in peptic ulcer bleeding // Br. J. Clin. Pharmacol. 2010. Vol. 69(3), p. 245–251.
- Serrano AG, Colomino II, Franch ES et al. Prevalence of rebleeding from peptic ulcer in patients treated with proton pump inhibitors // Med. Clin. (Barc). 2010. Vol. 134(13), p. 577–582.
- Chahin NJ, Meli M., Zaca F. Endoscopic injection plus continuous intravenous pantoprazole vs endoscopic injection plus continuous intravenous omeprazole for treatment of upper nonvariceal bleeding // Can. J. Gastroenterol. 2006. Vol. 20, Suppl A: 112.
- Lai B., Cervelli MJ Effect of gastric acid suppression with pantoprazole on the efficacy of sevelamer hydrochloride as a phosphate binder in haemodialysis patients: a pilot study // Nephrology (Carlton). 2012. Vol. 17 (4), p. 402–406.
- Fontes-Carvalho R., Albuquerque F. Clopidogrel — proton pump inhibitors drug interaction: implications to clinical practice // Rev. Port. Cardiol. 2010. Vol. 29 (10), p. 1555–1567.
- Fontes-Carvalho R., Albuquerque A., Araujo C. et al. Omeprazole, but not pantoprazole, reduces the antiplatelet effect of clopidogrel: a randomized clinical crossover trial in patients after myocardial infarction evaluating the clopidogrel-PPIs drug interaction // Eur J Gastroenterol Hepatol. 2011. Vol. 23 (5), p. 396–404.
- Mizia-Stec K., Haberka M., Mizia M. et al. Effects of pantoprazole on dual antiplatelet therapy in stable angina pectoris patients after percutaneous coronary intervention // Pharmacol. Rep. 2012. Vol. 64(2), p. 360–368.
- Drewelow B., Schaffler K., Reitmeir P., Bethke TD Effects of multiple-dose esomeprazole and pantoprazole on diazepam pharmacokinetic profile and pharmacodynamic effects on cognitive and psychomotor function in healthy volunteers // Arzneimittelforschung. 2010. Vol. 60 (8), p. 483–491.
A. N. Kazyulin , Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Natural Sciences I. E. Kalyagin , Candidate of Medical Sciences
GBOU VPO MGMSU Ministry of Health and Social Development of Russia, Moscow
Contact information for authors for correspondence
Pantoprazole: worthy among the strongest
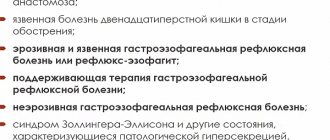
The five main PPIs in a doctor's practice are omeprazole, esomeprazole, rabeprazole, lansoprazole and pantoprazole. PPIs differ in the speed of onset and duration of antisecretory action, metabolic characteristics, and release form (in capsules, enteric-coated tablets - MAPS (Multiple Unit Pellet System)), in the form of a solution for intravenous administration) [2]. After oral administration, PPIs are released and absorbed in the small intestine. The active substance accumulates in areas with the lowest pH values; in the area of the secretory tubules of parietal cells, where pH = 1÷2, the concentration of PPI is almost 1000 times higher than that in the blood. Under these conditions, PPIs are protonated and converted into the active form, sulfenamide. The latter irreversibly binds to the cysteine residue of H+/K+–ATPase (proton pump) and blocks its function. This is accompanied by suppression of basal and stimulated secretion of hydrochloric acid (regardless of the nature of the stimulus). Acid production is restored as newly synthesized H+/K+–ATPase molecules are incorporated into the membrane of parietal cells. The pH range at which PPIs are activated is determined by the characteristics of their molecules. The rate of activation of pantoprazole with an increase in pH to 3 drops by half and practically stops at pH=4. Activation of other PPIs continues at higher pH: thus, the rate of formation of isomeprazole sulfenamide, esomeprazole and lansoprazole decreases by 2 times at pH=4, rabeprazole - at pH=4.9. This feature allows us to consider pantoprazole as a drug selective for the parietal cells of the stomach, in the area of which the pH reaches the lowest values. The pharmacodynamics of pantoprazole does not imply the possibility of blocking H+/K+–ATPases and H+/Na+–ATPases of other types of cells - biliary epithelium, blood-brain barrier, intestinal epithelium, renal tubules, corneal epithelium, muscles, immunocompetent cells, osteoclasts, as well as effects on organelles with an acidic environment - lysosomes, neurosecretory granules and endosomes, where pH = 4.5–5.0. Selectivity of action implies a lower likelihood of adverse events, especially with long-term use [1,2]. PPIs are metabolized in liver microsomes with the participation of cytochrome P450 subunits - CYP2C9, CYP2C19, CYP2D6 and CYP3A4. At the same time, they inhibit the oxidative activity of CYP enzymes to varying degrees. Their interaction with CYP2C19 and CYP3A4 is of greatest importance. According to the results of in vitro studies, among the five most commonly used PPIs, pantoprazole inhibits CYP2C19 to the least extent and CYP3A4 to the greatest extent. In terms of severity of inhibition of CYP2C19 function, lansoprazole is followed by omeprazole, esomeprazole, rabeprazole and pantoprazole; In terms of the strength of their effect on CYP3A4, pantoprazole is followed by omeprazole, esomeprazole, rabeprazole, and lansoprazole [1,2,3]. The CYP2C19 gene is polymorphic, which affects the therapeutic effect of PPIs. CYP2C19 is involved in the metabolism of a significant number of drugs, so the influence of PPIs on this subunit of cytochrome P450 is of great practical importance. Pantoprazole has the least potential for interaction with drugs that are detoxified by CYP2C19. CYP3A4 also plays an important role in drug metabolism; its activity varies significantly. This cytochrome P450 subunit is also expressed on the apical membrane of the intestinal epithelium, which can significantly influence the bioavailability of drugs, contributing to the “first pass effect”. In general, among the above PPIs, pantoprazole has the lowest affinity for the cytochrome P450 system, since immediately after phase I of detoxification with the participation of CYP2C19 and CYP3A4, it enters phase 2 - the formation of sulfate, which occurs in the cytosol and sharply reduces the reactogenicity of the molecule. In studies involving healthy volunteers and patients with various pathologies, no significant interactions were identified between pantoprazole and antacids, digoxin, diazepam, diclofenac, ethanol, phenytoin, glibenclamide, carbamazepine, caffeine, metoprolol, naproxen, nifedipine, piroxicam, theophylline, oral contraceptives, R –warfarin, clarithromycin, cyclosporine, tacrolimus, sodium levothyroxine [1,2,3]. When taking pantoprazole and coumarin anticoagulants simultaneously, more careful monitoring of the INR is necessary. The interaction of pantoprazole with methotrexate has not been sufficiently studied [3]. Pantoprazole is presented on the Russian market by the drug Nolpaza® (KRKA company, Slovenia) in the form of enteric-coated tablets. They are small in size and easy to use. The pharmacokinetics of pantoprazole is characterized by rapid absorption from the gastrointestinal tract; bioavailability when taken orally is 77% and does not depend on food intake. The time to reach the maximum concentration of the drug in plasma (Cmax) when taken orally is 2–2.5 hours. With regular use of pantoprazole, the Cmax value remains constant. The area under the concentration-time pharmacokinetic curve (AUC) and Cmax are also independent of food intake. AUC reflects the amount of the drug that reaches the target of action - proton pump molecules, and correlates with the severity of the antisecretory effect. For pantoprazole, the AUC is 9.93 mmol/l.h, which is comparable to the AUC for 40 mg esomeprazole. There is an intravenous form of pantoprazole. Pantoprazole is 98% bound to plasma proteins. The half-life (T1/2) is 1 hour. 80% of the metabolites are excreted by the kidneys, 20% by the bile. In case of chronic renal failure (including in patients on hemodialysis), no change in dosage of the drug is required. In severe liver diseases, T1/2 increases to 3–6 hours, AUC increases by 3–5 times, Cmax increases by 1.3 times compared to healthy individuals, and therefore a daily dose of pantoprazole is recommended not exceeding 20 mg. In elderly patients, there is a slight increase in AUC and Cmax, which has no clinical significance [4]. In addition to the narrow pH range at which the drug is activated, what distinguishes pantoprazole from other PPIs is its longer binding to the proton pump due to the formation of a covalent bond with an additional cysteine residue (Cys 822). As a result, the half-life of the drug does not correlate with the duration of the antisecretory effect, and after stopping pantoprazole, gastric secretion is restored after 46 hours. We believe it is necessary to provide data on the effectiveness and safety of pantoprazole based on studies and reviews of the most recent years. Efficacy of pantoprazole for GERD. PPIs have firmly established themselves as first-line drugs in the treatment of moderate to severe GERD. These drugs reduce the volume of gastric secretion, increase the pH of gastric contents, preventing damage to the esophagus by hydrochloric acid, bile components and digestive enzymes. The recommended dose of pantoprazole for reflux disease, depending on the severity of esophagitis and sensitivity to treatment, is 20–80 mg per day (in one or two doses). A dose of 20 mg is more often prescribed for milder forms of GERD. A dose of 40 mg in the treatment of moderate and severe reflux esophagitis is comparable in effectiveness to omeprazole, lansoprazole, and esomeprazole [9]. Maintenance treatment with pantoprazole at a dose of 20–40 mg per day for up to two years prevents relapses of reflux esophagitis in the vast majority of patients [9]. It can also be recommended to take 20–40 mg of pantoprazole “on demand” in case of heartburn and regurgitation [26]. The work of Scholten et al. It has been shown that on-demand use of pantoprazole at a dose of 20 mg or esomeprazole at a dose of 20 mg is equally effective as long-term maintenance treatment of non-erosive GERD and stages A-B of esophagitis according to the Los Angeles classification. When taking pantoprazole, the severity of heartburn was less [27]. Pantoprazole 40 mg provides sufficient control of nocturnal reflux symptoms and is comparable in this regard to esomeprazole [23]. Reviewed by Lehmann FS. and Beglinger C. and other works of recent years provide data on the high effectiveness of pantoprazole in the treatment of various forms of GERD and good tolerability of the drug [12,20,22,23,26]. Treatment with this drug reduces the incidence of complications and improves the quality of life of patients with reflux disease [26]. The effectiveness of pantoprazole depends on the genetically determined activity of CYP2C19 – S-mephenytoin 4'-hydroxylase. In Sheu BS et al. 240 patients with reflux esophagitis stages C and D according to the Los Angeles classification received pantoprazole at a dose of 40 mg per day for six months. Those patients who managed to achieve complete healing of erosions and resolution of reflux symptoms (n=200) were recommended to continue treatment with pantoprazole 40 mg “on demand” for a year. Based on the CYP2C19 genotype, “fast”, “intermediate” and “slow” metabolizers were distinguished. The effectiveness of on-demand therapy was higher in “slow metabolizers”: they took an average of 11.5 tablets per month (versus 16.3 in “intermediate” and 18.6 in “fast metabolizers”, p<0.05) [ 28]. In patients with excess body weight, the administration of pantoprazole in a “double dose” – 40 mg 2 times a day improves the results of treatment of reflux esophagitis and allows for a faster transition to an “on demand” regimen. The effectiveness of dose escalation is especially noticeable in “rapid metabolizers” [10]. Two randomized, double-blind studies assessed the rate of onset of clinical effect - relief of symptoms of non-erosive reflux disease and Savary-Miller stage 1 reflux esophagitis - during treatment with low-dose pantoprazole (20 mg per day) or second-generation histamine type 2 receptor blockers ( nizatidine 150 mg 2 times a day and ranitidine 150 mg 2 times a day). The studies were conducted in parallel groups, the severity of symptoms was assessed on a 4-point scale. During treatment with pantoprazole, a significantly larger proportion of patients noted the disappearance of heartburn already on the second day of treatment (39% versus 14.5% in the group receiving nizatidine, p < 0.01). A significant difference in the proportion of patients who no longer suffered from heartburn persisted during the first week, and then the drugs showed equal effectiveness [14]. GERD is often accompanied by sleep disorders. A cohort study examined the effects of pantoprazole on the well-being of patients with symptoms of reflux disease and obstructive sleep apnea. Patients received 40 mg pantoprazole per day for 3 months. During therapy, a significant improvement was noted: a decrease in daytime sleepiness (p = 0.002), episodes of awakening from reflux symptoms (p < 0.0001), and severity of snoring (p = 0.03) [29]. In another study, 84% of patients with GERD who were not overweight reported sleep disorders: symptoms of reflux in the supine position and in the morning, difficulty falling asleep, interrupted sleep, morning weakness. During treatment with pantoprazole for an average of 1.4 months, the quality of sleep significantly improved in 75% of those examined; the vast majority experienced relief from reflux symptoms at night [18]. Modolell I. et al., in addition to assessing the clinical signs of sleep disturbance in such patients (snoring, apnea, drowsiness), conducted a polysomnographic study. The clinical and polysomnographic effect of taking pantoprazole was confirmed in 78% of patients [20]. Pantoprazole has also found application in anesthesiology. One of the most dangerous complications of general anesthesia is aspiration of gastric juice; A gastric pH of 2.5 and a gastric volume of 25 ml (0.4 ml/kg body weight) before surgery are considered high-risk indicators. A double-blind study showed that pantoprazole 40 mg was significantly more effective than the prokinetic agent erythromycin 250 mg in reducing the risk of aspiration complications (when administered as a single dose at least 1 hour before anesthesia) [8]. The issue of the effectiveness and safety of PPIs in children remains insufficiently studied (insufficient evidence has been accumulated). Therefore, the instructions for prescribing pantoprazole may include children’s age among the contraindications [31]. However, in pediatrics, some studies have been devoted to this drug. When studying the pharmacokinetics and safety of pantoprazole at a daily dose of 20–40 mg in children 6–16 years old suffering from GERD, no data were obtained in favor of the accumulation of pantoprazole and no serious adverse events were recorded [32]. Two studies examined the effectiveness and safety of different doses of the drug in the treatment of GERD in children aged 1 month to 5 years, including premature infants. Pantoprazole was shown to be well tolerated, symptom relief and healing of erosive changes in the esophagus by the 8th week of treatment. The incidence of adverse events did not increase with increasing dose [17, 30]. Pantoprazole in the treatment of peptic ulcer, functional dyspepsia, drug gastropathy. For gastric and duodenal ulcers, pantoprazole is used in a dose of 40 mg 1–2 times a day. As part of eradication therapy (usually in combination with metronidazole, clarithromycin or amoxicillin), without prior testing of antibiotic resistance, pantoprazole at a dose of 40 mg 2 times a day provides a Helicobacter pylori eradication rate of 71–93.8% (intent analysis). to-treat). A triple eradication regimen with pantoprazole is not inferior in effectiveness to that including omeprazole or lansoprazole [9]. A Malaysian study assessed the eradication rate, tolerability and adherence of patients to triple anti-Helicobacter therapy with pantoprazole. Participants included 26 patients with peptic ulcer disease and 165 patients with non-ulcer dyspepsia infected with H. pylori. Patients received standard triple anti-Helicobacter therapy with pantoprazole 40 mg 2 times a day for 7 days. The effectiveness of eradication was assessed using the urease breath test. Treatment according to the protocol was completed by 84.4% of patients, the eradication rate was 71.2%. During the treatment period, adverse events were recorded in 68 (42.5%) participants: dyspepsia, loose stools, dizziness, skin rash. In no case was the adverse event reported as serious. The authors conclude that the triple eradication regimen with pantoprazole is very well tolerated [25]. Pantoprazole in a daily dose of 20 mg orally is effective in the prevention of gastropathy associated with the use of nonsteroidal anti-inflammatory drugs (NSAIDs) [9]. For the treatment of medicinal erosive and ulcerative lesions of the stomach and duodenum, pantoprazole is prescribed 40 mg 1-2 times a day. A double-blind, placebo-controlled study with a total of 800 participants examined the effectiveness of pantoprazole in controlling symptoms when taking NSAIDs and assessed the influence of various factors (such as gender, age, alcohol consumption, smoking, Helicobacter pylori infection) on therapeutic effectiveness. Pantoprazole was prescribed at a dose of 20 mg per day, the duration of therapy was 4 weeks. The severity of dyspeptic symptoms was significantly lower in the group receiving pantoprazole (p<0.0001); the effect of the drug became most pronounced after 7 days of treatment, regardless of the influence of the main risk factors [15]. For high gastric hypersecretion, including Zollinger-Ellison syndrome, pantoprazole is prescribed in doses of 80 to 160–240 mg per day orally or intravenously; The duration of treatment is selected individually [9]. Pantoprazole is safe for long-term use [4]. A British study examined the effectiveness and tolerability of 5 years of pantoprazole in 150 patients suffering from acid-related diseases (peptic ulcers or erosive reflux esophagitis), which occurred with frequent exacerbations and were resistant to treatment with H2 blockers. During exacerbation of diseases, the daily dose of pantoprazole was 80 mg; if it was ineffective within 12 weeks, the dose was increased to 120 mg, and during healing, it was reduced to 40 mg. Among others, parameters such as histological changes, serum gastrin levels, and the population of enterochromaffin cells in the mucosa were assessed. The proportion of patients in a state of stable remission after one year was 82%, two years – 75%, three years – 72%, four years – 70%, five years – 68%. The duration of remission in reflux disease did not depend on H. pylori infection. During treatment, the level of serum gastrin increased by 1.5–2 times (especially high values were noted with Helicobacter pylori infection). In some patients, episodic increases in gastrin >500 ng/l were recorded. In patients infected with H. pylori, there was a decrease in the severity of gastritis in the antrum and an increase in the body of the stomach, with the appearance of signs of atrophy. The number of enterochromaffin cells in the antrum changed slightly over 5 years, but in the body of the stomach decreased by about a third. Adverse events definitely related to pantoprazole were reported in 4 patients. Thus, the tolerance of prolonged treatment with a pantrazol generally corresponds to this when taking other IPP [7]. Pantoprazole and clopidogrel. In recent years, the question arose about the drug interaction of the IPP and clopidogrel, which is accompanied by a decrease in the therapeutic and preventive effect of the anti -signs, an increase in inclination to arterial thrombosis in patients with risk groups. IPP is often prescribed to such patients to prevent drug gastropathy and bleeding. The basis for anxiety was, in particular, the results of cohort retrospective examination, which analyzes the course of the disease in 16,690 patients who underwent stenting of coronary arteries and received therapy with clopidogrel (9862 patients) or clopidogrel in combination with IPP (6828 patients) with a high commitment to treatment . The frequency of “large cardiovascular events” (stroke, transient ischemic attack with hospitalization, acute coronary syndrome, coronary revascularization, death due to cardiovascular pathology) was estimated as the primary endpoint. In the cohort of patients who received only clopidogrel, the frequency of “large cardiovascular events” amounted to 17.9%, in the cohort of Klopidogrel and IPP - 25%(the adjusted hazard ratio of 1.51, 95%of the confidence interval (DI), 1, 39–1.64, p <0,0001). In this work, no significant differences in risk were found when taking individual IPP [19]. Clopidogrel's prodiganism turns into an active metabolite with the participation of CYP2C19 liver. Since the majority of the IPP suppresses the activity of this subunit of the p450 cytochrome, this can reduce the therapeutic and preventive effect of clopidogrel: to be accompanied by an increase in the reactivity of platelets and inclinations to arterial thrombosis. So, Omeprazole reduces the AUC of the active metabolite of the clopidogrel by 50% [1.2]. The existence of other mechanisms for the influence of IPP on the activity of clopidogrel. In the recommendations of the All -Russian Scientific Society of Cardiologists (NNCs), patients with stable manifestations of atherotrombosis emphasize that although the clinical value of the interaction of IPP and clopidogrel is not finally determined, the manufacturer of the original clopidogrel does not recommend it simultaneously intake with drugs that overwhelm CYP2C19 [5]. In August 2011, the Congress of the European Society of Cardiologists in Paris presented new recommendations for the treatment of OCS without lifting the ST segment, according to which the use of new antitromobocytic preparations of Prasugrel and thicrelor was recommended for the treatment of ACS. Treatment of clopidogrel is justified only in cases where the prescription of the first two drugs is impossible. Patients receiving double antitrocyte therapy are indicated by the treatment with a proton pump inhibitor (preferably not omeprazol) in the presence of gastrointestinal bleeding or peptic ulcer in an anamnesis, as well as in the presence of several risk factors for gastrointestinal bleeding. It should be noted that the effect of pantrazole on the activity of CYP2C19 is much weaker than that of other IPPs. Its neutrality in relation to Clopidogrel was demonstrated in a population -control -control population, which included 13,636 patients, who, after a myocardial infarction, was recommended to take this anti -generator. The study studied the frequency of a recurrent or re -heart attack within 90 days after discharge from the hospital and its connection with the receipt of the SPP. Statistical analysis showed that the simultaneous (within 30 previous days) IPP reception was associated with an increased risk of recurrent/re -infarction of myocardial (chances rates of 1.27, 95% of CI 1.03–1.57). There was no connection with the receipt of IPP more than 30 days before a repeated coronary event. With a stratified analysis, it was shown that the pantrazole took did not suppress the preventive effect of clopidogrel and did not increase the risk of recurrent/re -infarction of myocardial (the ratio of a chance of 1.02, 95% CI 0.70–1,47) [16]. For a more in -depth study of the interaction of clopidogrel, omeprazole and pantrazole, 4 randomized placebo -controlled studies with cross -design were carried out; They participated in 282 healthy volunteers. Clopidogrel was prescribed at a load dose of 300 mg, then in a supporting dose of 75 mg per day, omeprazole 80 mg at the same time (study 1); Then with an interval of 12 hours (study 2). The effect of increasing the dose of clopidogrel to 600 mg (loading) and 150 mg (supporting) (study 3) and interaction with pantrazol (at a dose of 80 mg) (study 4) were also studied. The study showed that the annexation of omeprazole led to a decrease in the area under the pharmacokinetic curve (AUC) for an active metabolite of clopidogrel, as well as an increase in platelet aggregation in the presence of adenosyndifosfate, increased the reactivity of thrombocyes. Pantoprazole did not affect the pharmacodynamics and the effect of clopidogrel [6]. Another randomized study with cross -design is devoted to the study of the interaction of clopidogrel and pantrazole in a double dose. 20 healthy volunteers received clopidogrel during the week (600 mg - a load dose and 75 mg per day - a maintenance dose) and pantoprazole (80 mg per day). Pantoprazole was prescribed simultaneously with a clopidogrel or with a gap of 8 or 12 hours. Prior to the randomization procedure, the examinations received only clopidogrel during the week. Various methods evaluated the function of platelets at different time points. It was shown that pantoprazole in a high dose does not affect the pharmacodynamic effects of clopidogrel, regardless of the reception mode [13]. Thus, pantoprazole (Nolpase®) is characterized by high efficiency in the treatment of acid -dependent diseases comparable to the effectiveness of other modern IPPs, good tolerance even with prolonged use. High selectivity of pH - mediated activation of pantoprazole involves a lower systemic effect of the drug. This issue requires special comparative studies. The drug is safe in old age; It is not contraindicated in severe pathology of the liver and kidneys. The undoubted advantage of pantrazole is the low potential of interaction with other drugs, which is especially important in the treatment of elderly patients who can take several drugs or receive drugs with a narrow “therapeutic corridor” [3]. In patients taking clopidogrel, pantoprazole has established itself as a means that significantly does not affect the action of the anti -signs [2].
Literature 1. Bordin D.S. Safety of treatment as a criterion for choosing a proton pump inhibitor in a patient with gastroesophageal reflux disease // Consilium Medicum. – 2010. – Volume 12. – No. 8. 2. Bordin D.S. What should be considered when choosing a proton pump inhibitor for a patient with GERD? // Medical almanac. – 2010. – No. 1(10) March. – pp. 127–130. 3. Blume H., Donat F., Warnke A., Schug B.S. Pharmacokinetic drug interactions involving proton pump inhibitors. Russian medical journal. 2009; volume 17; No. 9; pp. 622–631. 4. Isakov V.A. Safety of proton pump inhibitors during long-term use // Clinical pharmacology and therapy. – 2004. – No. 13(1). 5. National recommendations for antithrombotic therapy in patients with stable manifestations of atherothrombosis. Cardiovascular Therapy and Prevention 2009; 8(6), Appendix 6. 6. Angiolillo DJ, Gibson CM, Cheng S et al. Differential effects of omeprazole and pantoprazole on the pharmacodynamics and pharmacokinetics of clopidogrel in healthy subjects: randomized, placebo–controlled, crossover comparison studies. Clin Pharmacol Ther. 2011 Jan;89(1):65–74. 7. Bardhan KD., Bishop AE., Polak JM. et al. Pantoprazole in severe acid–peptic disease: the effectiveness and safety of 5 years' continuous treatment. Digestive and Liver Disease 2005; 37(1); 10–22. 8. Bhatia N, Palta S, Arora K. Comparison of the effect of a single dose of erythromycin with pantoprazole on gastric content volume and acidity in elective general surgery patients. J Anaesthesiol Clin Pharmacol. 2011 Apr;27(2):195–8. 9. Cheer SM, Prakash A, Faulds D, Lamb HM. Pantoprazole: an update of its pharmacological properties and therapeutic use in the management of acid–related disorders. Drugs. 2003;63(1):101–33. 10. Chen WY, Chang WL, Tsai YC, Cheng HC, Lu CC, Sheu BS. Double-dosed pantoprazole accelerates the sustained symptomatic response in overweight and obese patients with reflux esophagitis in Los Angeles grades A and B. Am J Gastroenterol. 2010 May;105(5):1046–52. 11. Cummins CL, Jacobsen W, Benet LZ. Unmasking the dynamic interplay between intestinal P-glycoprotein and CYP3A4. J Pharmacol Exp Ther 2002; 300:1036–45. 12. de Bortoli N, Martinucci I, Piaggi P et al. Randomised clinical trial: twice daily esomeprazole 40 mg vs. pantoprazole 40 mg in Barrett's oesophagus for 1 year. Aliment Pharmacol Ther. 2011 May;33(9):1019–27. 13. Ferreiro JL, Ueno M, Tomasello SD et al. Pharmacodynamic evaluation of pantoprazole therapy on clopidogrel effects: results of a prospective, randomized, crossover study. Circ Cardiovasc Interv. 2011 Jun;4(3):273–9. 14. Haag S, Holtmann G. Onset of relief of symptoms of gastroesophageal reflux disease: post hoc analysis of two previously published studies comparing pantoprazole 20 mg once daily with nizatidine or ranitidine 150 mg twice daily. Clin Ther. 2010 Apr;32(4):678–90. 15. Holtmann G, van Rensburg C, Schwan T et al. Improvement of Non–Steroidal Anti–Inflammatory Drug–Induced Gastrointestinal Symptoms during Proton Pump Inhibitor Treatment: Are G–Protein β3 Subunit Genotype, Helicobacter pylori Status, and Environmental Factors Response Modifiers? Digestion. 2011 Oct 26;84(4):289–298]. 16. Juurlink DN, Gomes T, Ko DT et al. A population–based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ 2009; 180(7):713–8. 17. Kierkus J, Furmaga–Jablonska W, Sullivan JE et al. Pharmacodynamics and safety of pantoprazole in neonates, preterm infants, and infants aged 1 through 11 months with a clinical diagnosis of gastroesophageal reflux disease. Dig Dis Sci. 2011 Feb;56(2):425–34. 18. Kindt S, Imschoot J, Tack J. Prevalence of and impact of pantoprazole on nocturnal heartburn and associated sleep complaints in patients with erosive esophagitis. Dis Esophagus. 2011 Mar 18. 19. Kreutz RP, Stanek EJ, Aubert R et al. Impact of proton pump inhibitors on the effectiveness of clopidogrel after coronary stent placement: the clopidogrel Medco outcomes study. Pharmacotherapy. 2010 Aug;30(8):787–96. 20. Modolell I, Esteller E, Segarra F, Mearin F. Proton-pump inhibitors in sleep-related breathing disorders: clinical response and predictive factors. Eur J Gastroenterol Hepatol. 2011 Oct;23(10):852–8. 21. Morgan D, Pandolfino J, Katz PO, Goldstein JL, Barker PN, Illueca M. Clinical trial: gastric acid suppression in Hispanic adults with symptomatic gastro-oesophageal reflux disease – comparator study of esomeprazole, lansoprazole and pantoprazole. Aliment Pharmacol Ther. 2010 Jul;32(2):200–8. 22. Lehmann FS., Beglinger C. Role of pantoprasole in the treatment of gastro-oesophageal reflux disease. Expert opinion pharmacother., 2005; 6:93–104. 23. Orr WC. Night–time gastro–oesophageal reflux disease: prevalence, hazards, and management. Eur J Gastroenterol Hepatol. 2005 Jan;17(1):113–20. 24. Pauli–Magnus C, Rekersbrink S, Klotz U, et al. Interaction of omeprazole, lansoprazole and pantoprazole with Plycoprote–in. Naunyn Schniedebergs Arch Pharmacol 2001; 364:551–7. 25. Qua Ch.–S., Manikam J., Goh Kh.–L. Efficacy of 1–week proton pump inhibitor triple therapy as rst–line Helicobacter pylori eradication regime in Asian patients: Is it still effective 10 years on? Journal of Digestive Diseases 2010; eleven; 244–248. 26. Scholten T. Long-term management of gastroesophageal reflux disease with pantoprazole. Ther Clin Risk Manag. 2007 Jun;3(2):231–43. 27. Scholten T, Teutsch I, Bohuschke M, Gatz G. Pantoprazole on-demand effectively treats symptoms in patients with gastro-oesophageal reflux disease. Clin Drug Investig. 2007;27(4):287–96. 28. Sheu BS, Cheng HC, Yeh YC, Chang WL.CYP2C19 Genotypes Determine the Efficacy of On-demand Therapy of Pantoprazole for Reflux Esophagitis as Los Angeles Grade C & D. J Gastroenterol Hepatol. 2011 Jul 20 . 29. Steward DL. Pantoprasole for sleepness associated with acid reflux and obstructive sleep disordered breathing. Laryngoscope 2004; 114:1525–8. 30. Tammara BK, Sullivan JE, Adcock KG, Kierkus J, Giblin J, Rath N, Meng X, Maguire MK, Comer GM, Ward RM. Randomized, open–label, multicentre pharmacokinetic studies of two dose levels of pantoprazole granules in infants and children aged 1 month through <6 years with gastro–oesophageal reflux disease. Clin Pharmacokinet. 2011 Aug 1;50(8):541–50. 31. van der Pol RJ, Smits MJ, van Wijk MP et al. Efficacy of proton-pump inhibitors in children with gastroesophageal reflux disease: a systematic review. Pediatrics. 2011 May;127(5):925–35. 32. Ward RM, Kearns GL, Tammara B et al. A multicenter, randomized, open–label, pharmacokinetics and safety study of pantoprazole tablets in children and adolescents aged 6 through 16 years with gastroesophageal reflux disease. J Clin Pharmacol. 2011 Jun;51(6):876–87.
Compound
| Enteric film-coated tablets | 1 table |
| active substance: | |
| pantoprazole sodium sesquihydrate | 22.57 mg |
| (in terms of pantoprazole - 20 mg) | |
| excipients: heavy magnesium hydroxycarbonate - 7.53 mg; macrogol (polyethylene glycol) - 1.2 mg; mannitol - 63 mg; calcium stearate - 1.2 mg; colloidal silicon dioxide - 1 mg; crospovidone - 20 mg; povidone K30 - 3.5 mg | |
| film shell: Opadry transparent (hypromellose (hydroxypropyl methylcellulose) - 1.920 mg, macrogol (polyethylene glycol) - 0.48 mg) - 2.4 mg; Acrylic-Iz green (methacrylic acid and ethyl acrylate copolymer (1:1) - 5.676 mg, colloidal silicon dioxide - 0.086 mg, sodium bicarbonate - 0.086 mg, sodium lauryl sulfate - 0.043 mg, yellow iron oxide - 0.06 mg, indigo carmine dye - 0.069 mg, brilliant blue dye - 0.026 mg, talc - 1.419 mg, titanium dioxide - 1.135 mg) - 8.6 mg; triethyl citrate - 1 mg |
| Enteric film-coated tablets | 1 table |
| active substance: | |
| pantoprazole sodium sesquihydrate | 45.14 mg |
| (in terms of pantoprazole - 40 mg) | |
| excipients: heavy magnesium hydroxycarbonate - 15.06 mg; macrogol (polyethylene glycol) - 2.4 mg; mannitol - 126 mg; calcium stearate - 2.4 mg; colloidal silicon dioxide - 2 mg; crospovidone - 40 mg; Povidone K30 – 7 mg | |
| film shell: Opadry transparent (hypromellose (hydroxypropyl methylcellulose) - 3.84 mg, macrogol (polyethylene glycol) - 0.96 mg) - 4.8 mg; Acrylic-Iz green (methacrylic acid and ethyl acrylate copolymer (1:1) - 11.352 mg, colloidal silicon dioxide - 0.172 mg, sodium bicarbonate - 0.172 mg, sodium lauryl sulfate - 0.086 mg, yellow iron oxide - 0.12 mg, indigo carmine dye - 0.138 mg, brilliant blue dye - 0.052 mg, talc - 2.838 mg, titanium dioxide - 2.27 mg) - 17.2 mg; triethyl citrate - 2 mg |