This site was made by experts: toxicologists, narcologists, hepatologists. Strictly scientific. Tested experimentally.
Author of this article, expert: gastroenterologist Daniela Sergeevna Purgina
Briefly: Hepatic encephalopathy develops in the later stages of liver disease, when complications occur in the brain. Treatment, in addition to taking medications, includes a mandatory diet and control of intestinal function.
- What causes hepatic encephalopathy
- Who is at risk of getting sick?
- Where does ammonia come from?
- Classification of hepatic encephalopathy
- What symptoms are typical?
- What helps a doctor identify a disease?
- How to be treated
This article was edited by gastroenterologist Daniela Sergeevna Purgina.
We all know that the liver is one of the most important organs in our body. This is a real chemical laboratory of our body, which performs many functions; and if problems arise in the laboratory, the whole organism suffers.
Liver diseases have a very large impact on the central nervous system. Today we will look at one of the complications that occurs in people with liver disease: hepatic encephalopathy.
What causes hepatic encephalopathy
The appearance of hepatic encephalopathy indicates a further unfavorable prognosis for the course of the underlying disease. Encephalopathy develops in patients with chronic liver failure. The course of hepatic encephalopathy can be acute, subacute or chronic.
Most often, hepatic encephalopathy is latent, that is, “hidden” in nature, and therefore it is not easy to diagnose. Even the patient himself may not be aware of the development of this condition.
The most common causes of hepatic encephalopathy are:
- alcoholic cirrhosis of the liver;
- viral hepatitis "" and "".
Hepatic encephalopathy develops in the later stages of liver disease: this is due to the fact that vascular anastomoses develop, that is, alternative blood circulation routes due to increased pressure in the portal vein, which occurs with cirrhosis of the liver. When these anastomoses appear, blood from the portal vein, bypassing the liver, enters the systemic circulation.
All potentially toxic substances that are normally neutralized in the liver (such as ammonia and mercaptans) enter the bloodstream and reach the brain and have a damaging effect on it. If hepatocytes (liver cells) are damaged, they are not able to filter and neutralize harmful substances that enter the liver through the bloodstream, so these toxic substances enter the brain through the bloodstream.
With normal liver function, encephalopathy is rare, and in this case it is caused precisely by the development of anastomoses.
Read also
Perinatal encephalopathy
Perinatal encephalopathy is a frequently encountered concept in the practice of pediatricians and pediatric neurologists!
What it is? Literally, “perinatal encephalopathy” means “damage to the brain in the perinatal… Read more
Polyneuropathy
Diabetic polyneuropathy is a pressing problem for patients with diabetes. Diabetic polyneuropathy is a serious complication of diabetes mellitus. The incidence of polyneuropathy is 26-50%...
More details
Intracranial hypertension on MRI
Intracranial hypertension is an increase in intracranial pressure. Normal intracranial pressure is 15 mm Hg. When blood pressure doubles, a stroke occurs. At a pressure of 50 mm Hg, the patient can...
More details
Pinched nerve
This morning you arrived at your country house. While taking out a heavy and large bag of tools from the trunk of your car, you suddenly felt a very strong, shooting pain in your lower back on the right side. Raise...
More details
Ankylosing spondylitis/ankylosing spondylitis
Ankylosing spondylitis (ankylosing spondylitis) is a chronic inflammatory disease of the spine and joints, accompanied by progressive pain, stiffness and limited movement at the beginning...
More details
Who is at risk of getting sick?
In addition to the development of anastomoses, risk factors for the development of hepatic encephalopathy include:
- age;
- severe liver disease;
- low level of albumin in the blood;
- high bilirubin levels;
- ascites;
- taking diuretics;
- constipation;
- small intestinal bacterial overgrowth syndrome;
- Helicobacter pylori infection;
- surgical intervention;
- alcohol abuse;
- taking sedatives.
The development of hepatic encephalopathy can be triggered by eating large quantities of protein foods, gastrointestinal bleeding or constipation.
There is an assumption about several mechanisms for the development of hepatic encephalopathy:
- The affected liver synthesizes fewer substances that are necessary for the normal functioning of the brain.
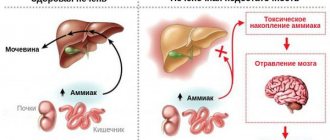
- The neutralizing function of the liver in relation to toxic substances is reduced. If the detoxification function of the liver is impaired, about 20 different substances can be found in the blood that have a toxic effect on the central nervous system. Ammonia has the greatest damaging effect, this has been confirmed by numerous clinical studies.
Where does ammonia come from?
Ammonia is formed in the intestines as a result of the activity of bacteria and the process of digesting protein foods. Normally, ammonia levels are regulated by the liver, but when liver function is impaired, it enters the brain through the bloodstream. Ammonia has a toxic effect primarily on astrocytes (brain cells), which are closely related to the functioning of neurons.
The development of hepatic encephalopathy is also caused by the vital activity of intestinal microflora, which releases ammonia. In addition to ammonia, bacteria in the intestines produce mercaptan, short-chain fatty acids, and phenols, which also have a toxic effect on the central nervous system. The higher the ammonia level, the expression of encephalopathy.
Total information
Liver pathology is extremely rarely complicated by hepatic encephalopathy. However, if the disease is nevertheless detected, its outcome is almost always tragic: for 2/3 of those affected, encephalopathy ends in death. Chronic liver diseases are more often complicated by hepatic encephalopathy than acute ones. They are potentially reversible, but significantly affect the patient’s ability to work and lifestyle.
Modern medical science does not yet have a clear idea of the causes of the development of the disease, but recent research allows us to hope for a solution to this problem in the near future. Discovering the mechanisms of the disease will contribute to the development of an effective treatment plan that will not only reduce the number of deaths, but will significantly improve the quality of life of those affected.
Classification of hepatic encephalopathy
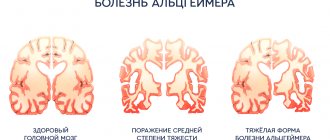
Doctors distinguish four stages of development of this serious condition:
- Stage I - characterized by the appearance of general weakness, headache, increased excitability, euphoria, tinnitus and flickering of “spots” before the eyes, frequent mood swings, impaired coordination of small movements, changes in handwriting, difficulty in performing simple mental tasks (for example, addition and subtraction).
- Stage II - apathy, melancholy, lethargy, drowsiness, aggressiveness, disorientation in time and space occur.
- Stage III - stupor, speech is difficult, severe confusion, stupor, presence of pathological reflexes.
- Stage IV - coma: consciousness is lost, the pupils are dilated and do not respond to light, reflexes disappear.
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Dyachenko Ksenia Vasilievna
Head of the center for the treatment of dizziness and balance disorders.
The doctor is a neurologist of the highest category.
Angioneurologist. Neurorehabilitation specialist. Physiotherapist. Candidate of Medical Sciences.
Experience: 19 years.Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
What symptoms are typical?
Symptoms of hepatic encephalopathy:
- irritability;
- apathy;
- decreased performance;
- lethargy, even to the point of impaired consciousness;
- memory loss;
- nausea;
- sleep disturbance: drowsiness during the day and insomnia at night;
- dyspnea;
- fixed gaze;
- loss of interest in previously loved things;
- alternating irritability with an overly cheerful mood;
- writing disorder;
- impossible to complete simple tasks, for example, sequentially linking numbers (Reitan test);
- speech is slow and monotonous.
In the early stages of hepatic encephalopathy, patients may experience only minor changes in behavior, which others may attribute to the consequences of alcohol consumption:
- attention disorder
- lethargy and slowdown in performing daily routine activities,
- slowing down of psychomotor processes,
- increased irritability,
- emotional instability,
- aggression,
- difficulty performing small movements with your hands.
Therapy
Therapy for this disease is a complex process that requires as quickly as possible clarification of the causes of its occurrence. The course of treatment includes: diet therapy, bowel cleansing, lowering nitrogen levels and symptomatic therapy.
It is necessary to reduce the amount of protein coming from food. It is necessary to adhere to this diet for a long time, since an increase in the amount of protein in the diet of a cured patient can provoke a relapse of the disease.
To speed up the excretion of ammonia in feces, it is necessary to achieve at least two bowel movements per day. For this purpose, cleansing enemas are used.
Antibacterial therapy involves taking antimicrobial drugs, the action of which is especially effective in the intestinal lumen (vancomycin, metronidazole, neomycin).
To achieve a sedative effect, benzodiazepine drugs are used, with preference given to haloperidol.
What helps a doctor identify a disease?
An important sign is the presence of liver disease in the stage of cirrhosis. It is also necessary to exclude other causes that may trigger the development of encephalopathy: for example, vascular diseases.
Liver cirrhosis has the following external symptoms:
- yellowness of the skin,
- fluid retention in the body, which manifests itself as ascites (an increase in the volume of the abdomen and swelling of the lower extremities),
- tendency to bleeding, manifested in the form of bruises and bruises on the skin,
- “jellyfish head” - expansion of the saphenous veins on the abdomen,
- numerous spider veins on the skin of the body,
- palmar erythema - redness of the skin of the palms,
- a special “liver” smell emanating from the patient,
- "popping" tremor.
Also read a detailed article about the symptoms of liver cirrhosis.
Signs of hepatic encephalopathy are quite nonspecific, which makes diagnosis difficult. Often this condition is difficult to distinguish from other causes of damage to the central nervous system, accompanied by changes in mental state:
- metabolic,
- tumor,
- infectious,
- medicinal,
- drugs,
- traumatic,
- cerebrovascular, etc.
At the moment, there are no clear criteria to distinguish hepatic encephalopathy from other causes of encephalopathy. The main diagnostic method is to collect anamnesis: the presence of signs indicating liver cirrhosis. The most commonly used are psychometric tests for the digital sequence of numbers, as well as tests that analyze the patient’s psycho-emotional state and assess the level of anxiety and depression.
An instrumental diagnostic method is an electroencephalogram, which allows one to detect changes in the activity of the cerebral cortex. Computer or magnetic resonance therapy reveals various changes in the structure of the brain.
Diagnosis of hepatoencephalopathy
If the damage to the liver and brain is alcoholic, the doctor is interested in:
- symptomatic picture;
- establishing the severity of the disease;
- stage of the process.
Based on the data obtained, during a survey and examination, the doctor prescribes additional types of diagnosis of hepatic ecephalopathy.
These include:
- A detailed clinical blood test with determination of the content of erythrocytes, leukocytes, hemoglobin, platelets.
- Biochemistry data with liver tests, bilirubin, alkaline phosphatase, gamma globulin transferase.
- Ultrasound of the parenchymal organs of the abdominal cavity. The specialist is especially interested in the condition of the liver, pancreas, and kidneys.
- Computed tomography is the most informative method of x-ray diagnostics.
- MRI in doubtful cases, as an additional diagnostic method.
- Needle biopsy as the most accurate option for differential diagnosis.
Forms of the disease
Depending on the etiological factor, several types of hepatic encephalopathy are distinguished:
- type A – caused by acute liver failure;
- type B - caused by the release of neurotoxins from the intestines into the bloodstream;
- type C – associated with cirrhosis of the liver.
Based on the rate of increase in symptoms, hepatic encephalopathy is divided into two forms:
- acute – develops rapidly, accompanied by severe mental disorders;
- chronic – symptoms increase slowly over months, and sometimes even years.
Sources
- I. L. Klyaritskaya Hepatic encephalopathy. 2005. Crimean therapeutic journal;
- Polukhina A.V., Khaimenova T.Yu., Vinnitskaya E.V. Hepatic encephalopathy: the problem of pharmacotherapy. 2021. Medical Council;
- Ivanikov I. O., Syutkin V. E. Hepatic (porto-systemic) encephalopathy. 2003. Practical medicine;
- Podymova Svetlana Dmitrievna New approaches to the pathogenesis, clinical picture, treatment of hepatic encephalopathy. 2021. Therapeutic Archive;
- Tsapyak T. A., Klopotiy E. V., Viltsanyuk I. A. Hepatic encephalopathy and the possibilities of its drug correction. 2007. Crimean therapeutic journal;
- Polunina T. E., Maev I. V. Hepatic (porto-systemic) encephalopathy. 2011. Medical advice.
Video from YouTube on the topic of the article:
Treatment
Therapy is carried out only in inpatient settings, patients are assigned to the intensive care unit. Treatment for hepatic encephalopathy depends on the intensity of its symptoms. However, the main goal of treatment procedures is to normalize liver function and eliminate the toxic effects of ammonia on the brain.
An integrated approach to treatment involves organizing:
- symptomatic treatment;
- special low-protein nutrition;
- detoxification procedures;
- drug therapy.
The latter involves the use of medications, including those based on lactulose. It helps suppress the synthesis of ammonia in the intestines and remove its excess in feces, as well as inhibit the excessive growth of pathogenic intestinal microflora. Antibiotics are usually taken orally, as intravenous use places a high burden on the liver.
The use of antibacterial drugs helps to destroy harmful microorganisms in the intestines that produce ammonia.
Drugs are also prescribed to promote the normal breakdown of ammonia in the liver. Such drugs are administered intravenously in the maximum allowable dosage. Sorbents are prescribed to remove toxins from the intestines before they penetrate into the blood. To reduce the volume of acidic gastric juice produced, special medications are indicated.