Consultation with a proctologist – 1,750 rubles.
- Symptoms of colon polyps
- Risk factors
- Diagnosis of neoplasms
- Treatment
- Popular questions
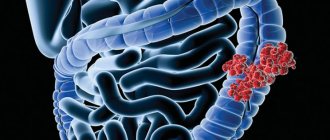
Colon polyps
- these are benign formations, which are usually asymptomatic and are most often found in patients complaining of discomfort, intestinal dysfunction, pain in the anus, pathological discharge from the anus, which also occurs in other diseases (hemorrhoids, paraproctitis, anal fissure , colitis, rectal cancer, etc.).
The prevalence of formations increases with age and ranges from 25 to 35% among the population over 50 years of age.
The clinical significance of this pathology is due to the fact that from 70 to 95% of colorectal cancer cases develop in the “polyps-cancer” sequence Source: Vladimirova A.A. The use of aquascopy in the diagnosis of colorectal polyps / A.A. Vladimirova [and others] // Bulletin of the All-Russian Scientific Center of the Siberian Branch of the Russian Academy of Medical Sciences. - 2006. - No. 6 (52). — P. 32-35. .
What is a polyp?
A polyp is a small, benign growth that sometimes appears on the inside of the colon or rectum (anus). Some people may only have one polyp, but it is also quite common for people to have two or more polyps at the same time. A colonic polyp may have a “leg” and a “head” and resemble a fungus growing from the inner lining of the intestine. There are other types of polyps that have a flatter shape, like a “growth” on the inner surface of the intestine. Most often, polyps form in the left half of the colon - the descending colon and the sigmoid colon. But polyps can also be in other parts of the intestine.
Briefly about the gastrointestinal tract
The colon and rectum (anus) are parts of the gastrointestinal tract. The gastrointestinal tract begins at the level of the mouth and ends in the anal canal. When we eat or drink, food and liquid from the mouth travel through the esophagus to the stomach. The stomach processes food and pushes it into the small intestine. The length of the small intestine is several meters and it is in it that the main processes of digestion and absorption of nutrients occur. Undigested food, water and waste then enter the colon. The largest part of the large intestine is called the colon, and is about 150 centimeters long. It is divided into 4 sections: the ascending colon, the transverse colon, the descending colon and the sigmoid colon. The colon primarily absorbs water and some salts. The colon continues into the rectum, its length is from 15 to 20 centimeters. The rectum accumulates feces (stool) before it is emptied.
Types of colon polyps
Typically, colonic polyps are divided into three types: hyperplastic polyps, adenomatous polyps (adenomas), and polyps in polyposis syndromes.
It is quite difficult to determine the degree of risk of an adenoma degenerating into cancer. Clinical studies have been conducted that have shown that if a patient has a single polyp adenoma measuring 1 cm, then the risk of its degeneration into colon cancer within 10 years is 1 in 12, and within 20 years – 1 in 4. Also described and predisposing factors for the degeneration of an adenoma into a tumor, for example, the larger the adenoma, the higher the risk. There are also different subtypes of adenomas, some of which have a much higher risk of developing into cancer than others.
Further we will talk only about hyperplastic and adenomatous polyps, which are most often found in adults.
How are polyps diagnosed (identified)?
Most often, colon polyps are discovered during this study. Colonoscopy is a diagnostic method in which the doctor examines the entire colon from the inside. A colonoscope is a thin flexible telescope tube. The thickness of a colonoscope is approximately equal to a finger. It enters through the anus and further into all parts of the colon until it reaches the cecum (the junction of the small and large intestines). A colonoscope has fiber optic channels that transmit light to a camera at the end of the machine. This allows the doctor to examine your intestine from the inside.
Sometimes other testing methods are used to diagnose colon polyps, such as barium enema (a special X-ray test with contrast), sigmoidoscopy (similar to colonoscopy, but uses a shorter telescope), and sigmoidoscopy.
When performing sigmoidoscopy, it is possible to examine the lowest section of the colon - the rectum and the beginning of the sigmoid colon, that is, the final 15-20 centimeters of the colon.
During sigmoidoscopy, the lower third of the colon is examined. Both studies are performed on an outpatient basis and do not require lengthy preparation.
In contrast, a colonoscopy allows you to examine the entire colon. To conduct the study, preliminary preparation of the intestine (cleaning the intestine of feces) is required.
Although stool occult blood testing is an important test for diagnosing various colon diseases, a negative result on this test does NOT guarantee the absence of polyps. If at least one polyp is detected, a complete examination of the colon is required, since in 30% of cases polyps are multiple.
As mentioned earlier, the vast majority of polyps do not manifest themselves in any way. Therefore, in a large number of people who have polyps, they will never be diagnosed (not detected). The above diagnostic methods may be prescribed if you have any characteristic symptoms or if there are other reasons. For example, if a stool test for occult blood is positive, a colonoscopy should be ordered to accurately examine the colon.
Additional materials
To view the video you must be logged in. Did you like the post? Do you find it useful or interesting? Support the author! Interesting 64
Botkin Hospital > Information > Departments > Department of Purulent Traumatology and Surgery No. 21
Podkosov Oleg Dmitrievich
Head of department
Traumatologist orthopedist of the highest qualification category. Proficient in all types of traumatological, orthopedic and reconstructive operations on bones and joints. Performs operations for purulent-inflammatory diseases of the limbs and spine.
The department is located on three floors of the ultra-modern surgical building No. 7. The department includes: a clinical diagnostic center with a registry, a surgeon's office, a dressing room, and an X-ray room. There is a daily reception from 8.30 to 16.30, except Saturday and Sunday, the flow of patients is also distributed for initial treatment and repeated appointments.
On the second floor there is a bed department with 30 beds with comfortable single and double rooms equipped with modern equipment, including a system for treating wounds with negative pressure. There are also ultrasound and physical therapy rooms.
There is also an anesthesiology-reanimation department for the most severe patients of purulent-traumatological and purulent-surgical profiles with 6 beds. It is equipped with an artificial kidney apparatus, modern efferent therapy (plasma exchange) and vacuum therapy. The layout of the rooms minimizes the risk of re-infection of patients.
The third floor is a modern operating block with two operating rooms, which are equipped with X-ray equipment for performing complex reconstructive operations on bones and joints, arthroscopic equipment for performing sonic low-traumatic operations on joints.
The treatment methods used in the clinic fully comply with modern international protocols and algorithms.
Types of surgical treatment
Purulent traumatology and orthopedics:
Treatment of early and late periprosthetic infection:
- reorganization
- installation of articulating antibacterial spacers
- joint arthrodesis
Purulent surgery:
Treatment of all types of acute purulent surgical pathologies (phlegmon, abscesses).
- plastic surgeries for decocubital injuries (bedsores)
- all types of plastic surgery for wound defects
- radical two-stage surgical treatment of all types of osteomyelitis using block-shaped antibacterial spacers
- replacement of bone defects using bone grafting methods, membrane bone transport techniques
- replacement of all types of wound defects of the extremities: non-free full-thickness flaps, free skin grafting
- Limb lengthening surgeries
- elimination of limb deformities
- arthrodesis of large and small joints
- extrafocal osteosynthesis
- intramedullary osteosynthesis
- extramedullary osteosynthesis
- wound treatment with negative pressure system and moist environment
Contacts
Address: Moscow, 2nd Botkinsky pr-d, 5, 7 building, right wing
Phone Head of department +7 (499) 728-82-06 from 07:30 to 8:00 and from 17:00 to 18:00
Reception of patients: from 08:30 to 16:30 daily, except Saturday and Sunday
All information posted on the site is published strictly in accordance with the scope and requirements of Article 8 of the Federal Law “On Personal Data” FZ-152 of July 27, 2006.
Support and development of the site: Center for Information Technologies and Public Relations Department of the State Budgetary Healthcare Institution “State Clinical Hospital named after S.P. Botkin DZM”
- Hyperplastic polyp
© 2008-2021 Hospital named after S.P. Botkin
How are colon polyps treated?
If you have a colon polyp or polyps, you will most likely be asked to have them removed, even if the presence of the polyps is not associated with any symptoms. This is done in order to prevent the risk of malignant degeneration of polyps into a cancerous tumor in the future.
Most colon polyps can be removed during a colonoscopy. The colonoscope has a channel through which special long instruments are inserted into the intestinal lumen, with the help of which the polyp is removed. This may be a forceps-like instrument that grasps and lifts the polyp from the intestinal wall, usually used to remove very small polyps. There are other instruments, at the end of which there is a wire electrosurgical loop, with the help of which the polyp is “cut off” from the intestinal wall and at the same time the vessels are cauterized to prevent bleeding.
Typically, the polyp removal procedure is painless and can be performed on an outpatient basis. Patients may also be offered a colonoscopy with the removal of polyps in a state of medicated sleep (“under sedation”, “under anesthesia”), in which case the risk of pain during the procedure is reduced to zero.
Sometimes, multiple procedures may be required to remove large polyps. If the size and location of the polyps do not allow their endoscopic removal, surgical intervention is required.
After the polyp is removed, it is sent for histological examination (examination under a microscope). This is done to make sure that the polyp has been completely removed, to determine the type of polyp, whether it is benign (not cancerous) or whether there are signs of malignant degeneration.
Risk factors
Risk factors and mechanisms of colon polyps are being actively studied. Among the environmental factors, the nature of nutrition is significant, with a predominance of refined foods in the diet, which contribute to constipation and prolonged stasis of intestinal contents. Dysbacteriosis of the colon has some influence on the occurrence of polyps, reflecting a violation of local and decreased general immunity, contributing to changes in the differentiation and regeneration of mucosal cells. The role of concomitant diseases of the biliary system and impaired production of bile acids, which have a mutagenic effect on the mucous membrane, is also noted as a risk factor. Active chronic inflammation and mucosal dysplasia play a certain role in the occurrence of polyps.
Colonoscopy with removal of polyps (endoscopic polypectomy) is possible:
- free of charge within the framework of compulsory health insurance, that is, under the compulsory medical insurance policy, if there is a referral from a medical institution or a territorial health authority;
- free of charge as part of high-tech medical care, if a previously performed biopsy confirms the malignant degeneration of the polyp;
- on a contractual basis at the request of the patient.
Diagnostic colonoscopy, as well as removal of polyps during colonoscopy, can be performed with intravenous sedation (pain relief).
Symptoms of bowel disease
Depending on the disease, different symptoms may be present. For example, with a benign tumor, there is nagging pain in the abdomen, a false urge to go to the toilet in a big way, secretion of mucus, and less often blood in the feces.
Sometimes there are complaints about bowel regularity and frequent constipation. With large tumors, there is a possibility of developing clinical intestinal obstruction. This condition is manifested by abdominal pain, nausea, bloating without passing gas and vomiting - including mixed with feces.
For a malignant tumor:
- pallor, weakness, progressive anemia;
- abdominal pain of varying severity;
- increased body temperature;
- alternating diarrhea and constipation;
- bloating, rumbling in the intestines;
- discharge from the rectum - mucous, bloody, putrefactive;
- nausea, vomiting, loss of appetite.
- Tumors and formations of the sigmoid and upper rectum. This is the most common reason for surgery. If intestinal obstruction is present, urgent surgery is required.
- Diverticular disease. Diverticula are extensions in the wall of the intestine. Rarely, complications may develop: inflammation of the diverticula with purulent melting of the appendix and the development of peritonitis or ulceration of the diverticula with the development of intestinal bleeding. Then surgery is required.
- Polyps with suspected malignant degeneration.
- Volvulus of the sigmoid colon. Occurs in the presence of a congenital pathology - dolichosigma (pathological increase in the length of the sigmoid colon).
- Foreign bodies, fecal stones.