Take the first step
make an appointment with a doctor!
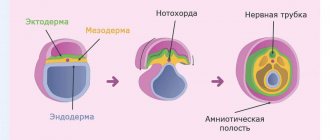
The placenta is a unique organ of the female body that appears during pregnancy and disappears after childbirth. Its task is to provide the fetus with nutrients and oxygen, as well as remove waste products and protect it from the mother’s immune system. However, with low placentation, this same organ can destroy the child, preventing him from leaving the birth canal during childbirth. This pathology is quite common and can occur even in healthy women. What causes it and is it possible to reduce such risks?
What is a low placenta?
Shortly before being born, the baby turns head down in the womb. This position provides him with a relatively easy exit from the genital tract. In this case, the placenta attachment site is normally located at the upper fornix of the uterine cavity. Thus, the path to the baby is blocked only by a thin film of the amniotic membrane, which easily breaks through during childbirth.
Pathology occurs when, before childbirth, the placenta is not located in the upper part of the uterus, but on the side or below, partially or completely blocking the cervical canal. This anomaly occurs quite often (in 10% of cases) in early pregnancy. But over time, as the child grows, due to the process of rising of the placenta, the passage is cleared. As a result, before childbirth, its pathological position is observed only in 0.5-1% of women in labor. Depending on the location of the placenta, its presentation is:
- Full. The placenta is located below, completely blocking the cervical canal. In this case, spontaneous childbirth is impossible and threatens the life of the child and mother due to the high probability of extensive bleeding.
- Incomplete. The placenta is located in the lower part, but shifted to the side, so it only partially covers the os of the uterus. This presentation also makes childbirth impossible and dangerous for the mother or baby due to the high risk of bleeding.
- Low. The placenta is located at a distance of 7 cm from the cervical canal, without blocking it. With this arrangement, childbirth is possible, but requires increased attention from doctors. If the distance from the placenta to the pharynx of the uterus is less than 7 cm, and it touches the edge of the pharynx, such a presentation is called marginal.
Lower presentation is the safest, but it is also an anomaly and certain risks for the mother and her child also exist with it. Therefore, during routine examinations, doctors pay great attention to monitoring the condition of the placenta. Using ultrasound, they determine its location on the anterior or posterior walls of the uterus, and also measure the distance from its edge to the cervical canal. If an anomaly is detected, tactics to save the baby and his mother are developed before birth.
Take the first step
make an appointment with a doctor!
Stem cells can be used to treat both the child and his relatives
Today, stem cell treatment methods are successfully used all over the world. In Ukraine, the leading position in the development and application of such techniques belongs to the Institute of Cell Therapy. Cord blood stem cells are stored in the Cryobank of the Institute of Cell Therapy in special containers under guaranteed maintenance of the necessary conditions.
Causes of low placenta during pregnancy
The location of this organ is determined by where the fertilized egg attaches to the endometrium of the uterus. This is where the placenta will form, and it is impossible to influence this at this stage of medical development. At the same time, several factors can be identified that directly or indirectly contribute to the appearance of such an anomaly:
- Anatomical abnormalities of the uterus. The shape of this organ directly affects where the fertilized egg will “float”. If a woman has congenital or acquired (for example, after surgery) disorders of the anatomical structure of the uterus, then the chances of low placentation increase significantly. This category also includes isthmic-cervical insufficiency, which consists in weakening the muscles of the uterine cervix, which is unable to withstand intrauterine pressure.
- Endometrial damage. These are disturbances in the structure of the uterine mucosa resulting from infections, curettage during abortion, difficult childbirth, cesarean section, etc. Also a common cause of low placentation is endometriosis (inflammation of the endometrium), benign and malignant tumor formations that disrupt the functioning of this layer .
- Fetal factor. The fertilized egg is fixed in the endometrium due to enzymes produced by the embryonic membranes. Sometimes this function is disrupted, and the embryo descends from the fallopian tube too low, embedding itself in the mucous membrane in the lower part of the uterus. Such situations especially often arise in cases of hormonal or endocrine disorders in a woman, inflammatory processes in the ovaries, uterine appendages and tubes.
- Repeated births. It has been noticed that with each subsequent pregnancy the risk of placenta previa increases, especially if the previous one was complicated. This is likely due to damage to the uterus or endometrium, as well as hormonal changes that occur in women as they age.
Other factors that contribute to a low-lying placenta during pregnancy include genetic predisposition, excess weight, smoking, drinking alcohol and other bad habits. Their presence in a woman gives grounds to classify her as a risk group, even if no pathology has yet been identified, and to prescribe special care and more careful monitoring of the state of pregnancy.
Symptoms of low placenta previa during pregnancy
This pathology does not have any specific external signs. Low placentarity is manifested by the following symptoms:
- Bleeding. Already at 12-13 weeks, women with this anomaly may begin to experience uterine discharge mixed with blood, which is associated with microdetachments of the “baby spot” from the endometrium. Most often, this symptom manifests itself in the last trimester of pregnancy, when the fetus grows to a large size and, with movements, more strongly tears the placenta from the uterus. In the later stages, even a slight stress (coughing, orgasm, sneezing, constipation, etc.) can lead to heavy bleeding, threatening the life of the mother and her child. Due to periodic or constant blood loss, women often experience symptoms of anemia - dizziness, weakness, low blood pressure and hemoglobin levels in the blood.
- High position of the uterine fundus. Based on the location of the upper part of the uterus, the doctor usually judges the degree of development of pregnancy. With placental presentation, the uterine fundus is often located too high, which may indirectly indicate a low location of the placenta.
- Fetal presentation. The location of the baby, uterus and placenta are interdependent. Therefore, pelvic or transverse presentation of the fetus is often accompanied by a low localization of the “baby spot,” which the doctor can judge from the data obtained during an ultrasound examination of the patient.
Often this pathology (especially in the early stages) is completely asymptomatic. The woman may not feel pain or discomfort in the lower abdomen, and she does not have periodic or constant bleeding. Therefore, it is possible to unambiguously identify low placenta previa only with the help of modern diagnostic tools during routine gynecological examinations. Ultrasound is most effective in this regard. This method has the following advantages:
- Minimally invasive. If low placenta previa is suspected, an ultrasound examination is performed abdominally. The scanner is located on the outer surface of the abdomen; the doctor does not make any incisions, so ultrasound does not create any risks for the child or mother.
- Information content. Modern ultrasound machines have high resolution and accurately visualize the position of the baby in the uterus. With their help, the doctor can determine the location of the placenta, the distance from its edge to the uterine os.
If low placental capacity is suspected, your doctor may order an unscheduled scan to monitor placental migration. The procedure is usually performed at 12, 20 and 30 weeks of pregnancy, but more frequent ultrasounds are also possible.
A gynecological examination, which is standard during normal pregnancy, is not performed with this pathology. This is due to the fact that inserting instruments into the vagina can cause strong contractions of the uterus, which will result in premature labor with extensive bleeding.
Take the first step
make an appointment with a doctor!
Why is it worth saving cord blood in Cryobank?
Today, more than 100 diseases can be cured using stem cells. The procedure for collecting umbilical cord blood is possible only at the birth of a child - at the moment of cutting the umbilical cord.
It is absolutely safe and painless for both the child and the mother in labor. When the days are counting, and there is no way to urgently find a suitable donor, then the only way out is treatment with stem cells. While searching for a donor takes months, preparing stem cells takes several hours.
A feeling of maximum peace of mind for the most valuable thing in life - for your children - is only possible if you are 100% sure that the right medicine is at hand. It is stored in the Cryobank of the Institute of Cell Therapy and is available to you and your family upon request.
placenta
What are the dangers of low placental location?
This pathology is considered dangerous to the life and health of both the child and his mother. The greatest risks include:
- Miscarriage or premature birth. The likelihood of this outcome is due to the fact that with placental insufficiency the uterus experiences higher loads than during a normal pregnancy. Any physical stress and even mental stress can cause intense uterine contractions, expelling the fetus. Moreover, the likelihood of this remains throughout the entire pregnancy.
- Fetal presentation. If the placenta has formed low in early pregnancy, the risk of fetal malposition increases by 50%. Developing in the mother's belly, the unborn child strives to take a position so that its head is in contact with anything as little as possible - including the “baby place”. Transverse or breech presentation of the fetus makes natural childbirth impossible and is a pathological condition that threatens both itself and its mother.
- Fetal hypoxia. With inferior placenta previa, the blood supply to the embryo with nutrients and oxygen deteriorates. Chronic and acute hypoxia causes irreversible changes in the child’s brain, delays his intrauterine development, and during childbirth can lead to his death.
- Uterine bleeding. This complication threatens a woman with placental insufficiency throughout pregnancy. This risk is especially great in the later stages, when the fetus becomes quite large and puts more pressure on the walls of the uterus, increasing the likelihood of placental abruption from the endometrium. Mild but regular bleeding provokes the development of anemia in the mother, which, in turn, is one of the causes of chronic embryonic hypoxia. With severe placental abruption, extensive hemorrhage may develop with hemorrhagic shock, fatal for both the woman and her child.
All of these complications make placenta previa a dangerous pathology. Therefore, when it is detected, a woman is at risk. Depending on the type of pathology, doctors develop a special treatment strategy that will save the life of both the mother and her child.
Take the first step
make an appointment with a doctor!
Precautionary measures
It should also be noted that with placenta previa, you should always keep in mind the possibility of severe bleeding. Therefore, it is necessary to discuss with your doctor in advance what to do in this case, which hospital to go to. Staying home, even if the bleeding is light, is dangerous. If there is no prior agreement, you need to go to the nearest maternity hospital. In addition, with placenta previa, it is often necessary to resort to a blood transfusion, so if you have been diagnosed with this, find out in advance which relative has the same blood type as you, and get his consent to donate blood for you if necessary (the relative must get tested for HIV, syphilis, hepatitis in advance).
You can arrange at the hospital where you will be observed so that your relatives donate blood for you in advance. At the same time, it is necessary to obtain a guarantee that the blood will be used specifically for you - and only if you do not need it will it be transferred to a general blood bank. It would be ideal for you to donate blood for yourself, but this is only possible if your condition is not alarming, all indicators are normal and there is no bleeding. It is possible to donate blood for storage several times during your pregnancy, but you also need to ensure that your blood is not used without your knowledge.
Although placenta previa is a serious diagnosis, modern medicine allows you to carry and give birth to a healthy child, but only if this complication is diagnosed in a timely manner and with strict adherence to all doctor’s prescriptions.
When everything is over and you and your baby find yourself at home, try to properly organize your life. Try to get more rest, eat right, and be sure to take your baby for walks. Don't forget about multivitamins and medications to treat anemia. If possible, do not give up breastfeeding. This will not only lay the foundation for the baby’s health, but will also speed up the recovery of your body, because... Stimulation of the nipple through sucking causes the uterus to contract, reducing the risk of postpartum bleeding and inflammation of the uterus. It is advisable that at first you have someone to help you with child care and household chores, because your body has gone through a difficult pregnancy and needs to recover.