Placenta - what is it?
In Latin, the word “placenta” means “pie, flatbread.” It's all about how the placenta looks: the organ received this name due to its flattened shape, because in appearance it resembles a flat disk.
When does the placenta form during pregnancy?
Its formation begins only when conception occurs, and when the child is born, it is excreted along with the membranes.
The placenta performs the following functions:
- respiratory - through it oxygen enters the fetus and carbon dioxide comes out;
- barrier – protects the fetus from those harmful substances that are in the mother’s blood;
- nutritious - nutrients come from mother to fetus;
- hormonal - produces a number of hormones that determine the normal development of pregnancy;
- excretory - waste products of the fetus are excreted through it.
Development of the placenta
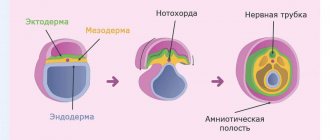
The development of this organ does not occur immediately after conception. In the fourth week of pregnancy, the fertilized egg is surrounded by the chorion - this is a special villous tissue. The formation of the early placenta occurs around the ninth week. It is formed by chorionic villi that penetrate the upper layer of the uterus and connect with the blood vessels there.
By the end of gestation, the placenta already weighs about half a kilogram, and its diameter is 15-20 cm. The permeability of the placenta membrane increases until the 32nd week of pregnancy. After all, every week the size of the fetus increases, and it requires more and more oxygen and nutrients.
Accordingly, in order to provide such nutrition, the number of vessels in the child's place increases, and the membrane becomes thinner. After the thirty-second week, the development of the placenta stops and it begins to age. If this happens earlier, then early aging of the placenta .
Should I worry if an ultrasound reveals abnormalities of the placenta?
The placenta develops from the cells of the fetal egg, and not from the maternal cells, so the organ cannot be ideal. Violations are mild, moderate and significant. If abnormalities are detected, a diagnosis of placental insufficiency is made.
Gynecologists believe that only significant changes are dangerous for the fetus, since thanks to the extensive vascular network, the organ can perform all functions even with partial damage or detachment.
To understand how dangerous the changes are, it is not enough to assess the degree of problems in the placenta; it is important to take into account the quality of fetal development. If there is a discrepancy between the parameters of growth and development and the norms for the period, you need to sound the alarm and take action. If the baby develops normally, you can limit yourself to observation. For this purpose, non-screening (unscheduled) ultrasounds are performed.
Degrees of placenta maturity
During the development of pregnancy, the doctor looks for all internal changes during an ultrasound examination. And the degree of maturity is also determined during the ultrasound process, taking into account certain parameters.
Based on the duration of pregnancy, the degrees of maturity are determined as follows:
- degree of maturity 0 – up to 30 weeks;
- degree of maturity of the placenta 1 – 27-36 weeks;
- degree of maturity of the placenta 2 – 34-39 weeks;
- degree of maturity of the placenta 3 – after 36 weeks.
To determine what degree of aging - first, second or third - the doctor determines its thickness, looks for calcium deposits and cysts.
Not so long ago, the maturity of a child's place was viewed differently than it is now. Thus, it was believed that with premature aging, miscarriages , there is a high risk of antenatal fetal death, and low-weight children are born. However, after scientists conducted a series of studies, such interdependence was refuted.
If a woman has a third degree of maturity before 35 weeks (for example, at 32 weeks), she is considered to be at increased risk.
A gynecologist will explain in more detail about the characteristics of maturity, for example, the degree of placenta maturity 2, what this means.
In the table below you can clearly see the degrees of ripeness by week.
Table of degrees of placenta maturity by week of pregnancy
| Chorionic part (the one that is adjacent to the fetus) | Structure | Are there calcium deposits? | |
| 0 tbsp. (up to 30 weeks) | Completely smooth | Homogeneous | Virtually none |
| I Art. (27-36 weeks) | Wavy | A little seal | Microscopic |
| II stage (34-39 weeks) | There are indentations | There are seals | Visible |
| III Art. (after 36 weeks) | Recesses to the basement membrane | Cysts | A large number of |
Pathogenesis
The second planned ultrasound during pregnancy (20-24th week) in most cases is not indicative of diagnosing the corresponding problem. For the first time, it is possible to detect early maturation of an organ mainly at 27-28 weeks, when the degree of development of the child’s place changes from 0 to 1.
Normally, the structure of the placenta is homogeneous, without undulations. At the first stage of maturity, the body of the organ becomes thicker. Ultrasound shows zones of hyperechogenicity. The first irregularities appear on the chorionic plate.
When exposed to negative factors, a premature transition of the placenta to the second degree of maturity occurs. The number of zones of hyperechogenicity increases, small inclusions appear, and irregularities on the chorionic plate deepen.
The third degree is characterized by the lobar structure of the placenta, blood flow through the vessels to the fetus is reduced, and calcifications can form in the parenchyma of the organ. The described changes can be diagnosed when the third ultrasound is performed during pregnancy (32-34 weeks).
Placenta thickness
This parameter is a very important point in the diagnosis, since deviations from the norm can be evidence of pathologies. There is a special table of placental thickness by week, which indicates the normal limits.
The thickness of the placenta by week is determined by ultrasound, which is performed after 20 weeks. If the process of bearing a baby proceeds normally, then the greatest thickness of the placental tissue is observed at 34 weeks, and at 36 weeks. its growth stops, and its thickness may even decrease slightly.
If the placenta is too thin, placental hypoplasia . However, as a rule, this is not a very threatening phenomenon, unless a significant decrease in size is noted. Very often, such deviations are associated with genetic disposition, the influence of unfavorable factors, and diseases of the woman. If this is due to illness, treatment is carried out; in all other cases, supportive therapy is practiced.
This indicator is also influenced by the physique of the expectant mother. Short, thin women have smaller baby seats than tall, curvy women. If thickening of the placental tissue is diagnosed, this condition can threaten the termination of pregnancy. But with the right approach to treatment, pregnancy can be saved.
Thickening can occur due to Rh conflict , diabetes mellitus , gestosis , iron deficiency anemia , or previous infections . In case of serious deviations, careful monitoring of the expectant mother is important. The fact is that with the rapid growth of a child's place, its active aging occurs. When thickened, hormonal function is disrupted, which can negatively affect pregnancy.
However, if after a series of additional examinations the doctor concludes that the fetus is developing normally, only careful observation will be needed.
Old placenta
Pregnant women are afraid of the “old placenta” like fire, because most of them will be sent to a hospital, where they will be even more frightened by the possible loss of the child, its retardation in growth and development, and, of course, more than one liter of physiological solutions will be injected into the woman’s body together with other medications. They will “rejuvenate” the placenta! Apparently, many doctors have no idea that “rejuvenating” the placenta is a manifestation of illiteracy.
Let's talk about the structure of the placenta and which placental inclusions are normal and which are not. The placenta develops gradually from trophoblast villi in the first and second trimesters of pregnancy; that is, the growth and development of the placenta is a process that takes a certain period of time. The specific mechanism of blood supply allows the exchange of oxygen and nutrients between mother and child without mixing two different circulatory systems - mother and fetus. Thus, the placenta is a kind of bridge between the mother’s body and the baby’s body. Since the placenta is a derivative of the fetus, that is, it develops from certain cells of the fetal egg, often with disorders of fetal development, disturbances in the development of the placenta are observed, as well as changes that are not signs of a “normal” placenta.
The placenta has the unique ability to perform its function even if abnormalities occur on the part of the mother or fetus, as well as with partial damage or detachment. The presence of inclusions in the placenta is not always a sign of poor function, since the function can be performed efficiently until the end of the entire pregnancy. Doctors often talk about placental insufficiency based on only one ultrasound sign, without even looking at the condition of the fetus. The worst thing is that medications are prescribed that have nothing to do with the treatment of placental insufficiency.
Let's discuss the question of what it means to be “deficient” of something from a medical point of view. When they talk about kidney, heart, or liver failure, they mean, first of all, functional failure, that is, the organ ceases to fully perform its function. If an organ does not perform its function, who suffers from it? Naturally, the entire body of a sick person. When we talk about the function of the placenta, what is its role? First of all, the exchange of nutrients, oxygen, carbon dioxide between mother and child. Secondly, the protective function - the placenta does not allow many substances and microorganisms to enter the fetal body, being a good barrier. Thirdly, the placenta produces a number of important biological substances that are necessary for the normal development of the child and the course of pregnancy in general. If the placenta does not perform its function correctly or completely, then who will begin to suffer from such a problem? Not mother! Child first. How does the child suffer? Without receiving enough substances and oxygen, he may be stunted in growth or may show signs of oxygen starvation - hypoxia. Often, ultrasound doctors do not look at the development of the fetus, but after “digging” in the placenta and uterine vessels, they immediately issue a conclusion: placental insufficiency. What about the fruit? If the heart rate is indicated (and it is almost always normal), then this is already good. And this is how they usually write: “The fruit is without features. No pathology was detected." And not a word more. So, if nothing bad is detected on the child’s part, doesn’t this mean that the placenta is coping with its function and the baby is growing and developing as expected?
If we talk about the functional failure of an organ, it can occur acutely or develop gradually (chronically). Acute failure is a serious condition that requires emergency care. Acute placental insufficiency occurs when placental abruption occurs, especially if it is large in size. In most of these cases, the only treatment option will be urgent delivery, and saving the child and mother (due to bleeding).
Chronic functional failure occurs slowly, without serious danger to the human body, until all compensation mechanisms stop working. For its development, certain conditions must exist: organ failure, a constantly present risk factor, time. For example, heart failure cannot occur in a person with a healthy heart and normal blood pressure, even in old age. Against the background of cardiovascular diseases, heart failure is a complication and often requires serious measures in terms of treatment.
If a person abuses alcohol, then the liver and pancreas for a long period of time compensate for the load and increased metabolic process, neutralizing alcohol in the body, but with damage at the level of the cells of these organs in the form of pancreatitis and cirrhosis of the liver, liver failure, pancreatic insufficiency and a number of other problems. Impending functional failure of an organ can be recognized using a number of diagnostic tests, biochemical indicators of blood and other body fluids, since all processes in our body, including disease, begin at the level of chemical reactions. With regard to chronic placental insufficiency, certain prerequisites must exist in order for this deficiency arose and developed to the extent that deviations in the development of the fetus appear. What are these prerequisites? On the maternal side, these can be general diseases, most often high blood pressure (hypertension in pregnancy) and diabetes, as well as smoking, drug use, and alcohol. These can also be infectious diseases, especially acute viral diseases. On the part of the child and the placenta, these may be malformations of the placenta or fetus, fetal hydrops, placental abruption, and a number of other problems. Again, not all women with high blood pressure experience placental insufficiency, especially if the woman controls the pressure with medications.
Thus, changes in the placenta do not mean poor function of this organ, and vice versa, the absence of changes does not always guarantee good functioning of the placenta. And the criterion for assessing the work of the placenta will always be the state of the “final result” of its function - the condition of the fetus. Of course, there are other assessments of placental function, but these are not necessarily the levels of some hormones that some doctors check so carefully. The approach to the study of any issue should be comprehensive, not superficial, and have a logical sequence. If the condition of the fetus is normal, it is unlikely that the pregnancy is threatened by some kind of placental insufficiency, and even more so against the background of the mother’s excellent health and the absence of bad habits. Therefore, sometimes the conclusions of some doctors about placental insufficiency against the background of the good development of the child and the good health of the mother sound absurd. Such conclusions bring nothing but chaos and fear into the life of the expectant mother and, moreover, lead to the creation of a vicious circle of endless examination and treatment.
What, in fact, “scares” doctors, especially ultrasound doctors, about the placenta so much that they immediately suggest that the woman undergo intensive treatment (the same for all cases). It is not the disease that is being treated, but the ultrasound signs! Most of all, doctors “cling” to the thickness of the placenta and its inclusions - “calcifications”, by which they judge its old age.
Up to 20 weeks, the placenta grows and develops, so most often the size and thickness of the fetal place, as well as the place of its attachment, are examined using ultrasound later, after 20 weeks, if the pregnancy is not accompanied by bleeding or fetal growth retardation. If pregnancy proceeds with complications, examination of the placenta using ultrasound is carried out earlier.
The placenta weighs 1/6-1/7 of the weight of the fetus and at birth weighs 500-600 g. On the maternal side, it has about 20 lobules. The umbilical cord is usually attached in the center of the baby's place, and in rare cases in other places in the placenta.
So, what is usually looked at and measured on an ultrasound, and why are conclusions made that sometimes do not correspond to the truth? How do you know if the research was done correctly or with errors? It is always important to know the placement of the placenta, and most often women are terrified (because they are diligently frightened) of placenta previa, when the attachment and formation of the placenta occurs very close to or in the area of the internal os of the cervix. Fortunately, in most cases, as the placenta grows, its edges “migrate,” that is, they move away from the cervix, which is a good sign regarding the prognosis of pregnancy. But even if a woman has central placenta previa, this does not mean that she should lie almost motionless throughout her pregnancy. It is extremely rare that there is a need to “preserve” pregnancy using strict bed rest. Bed rest, on the contrary, has too many side effects and serious complications, and should never be abused.
Further, doctors often scare women with hypertonicity of the uterus, especially at the placenta insertion site. “It’s terrible, I have hypertonicity of the uterus and I’m being put on hold!” The fact is that at the placenta attachment site, the structure of the internal lining of the endometrium has a certain specificity, and the muscular layer of the uterus can and should be “slightly tense.” This place contains a large number of venous vessels and is called the retroplacental complex. It is precisely this that is very often confused with muscle contractions of the uterus and is called “hypertonicity.” The use of color Doppler ultrasound helps to see the difference between the retroplacental complex and local (local) contraction of the uterus. In addition, the use of ultrasound sensors, irritation of the anterior wall of the abdomen and cervix with vaginal sensors can provoke contractile activity of the uterus, which an inexperienced doctor will “attribute” to hypertonicity.
Doctors are interested in the thickness of the placenta - there are also many “scary” conclusions here. Since the formation of the placenta is usually completed by the fourth month of pregnancy, the thickness is measured at the formed placenta, and not earlier, with the exception of those cases where the size of the placenta goes beyond the acceptable limits for a mature placenta. Normally, after 20 weeks, the thickness of the placenta should be from 1.5 to 5 cm. Some doctors take 4 cm as the upper mark, however, in most cases, a thickness of up to 5 cm will not be a pathology (and normal fetal development will be evidence of this norm). Again, errors in measuring placental thickness begin with incorrect markings on the ultrasound image. Sometimes the ultrasound shadow of the fetus, especially when the placenta is attached to the posterior wall of the uterus, is mistaken for the placenta, and the muscular layer of the uterus and the retroplacental uterine complex will also be mistakenly considered as part of the placenta. If the thickness measurement is not carried out strictly perpendicular to the walls of the placenta, then the thickness may also be determined incorrectly. The thickness of the placenta also depends on its shape, and the shape can be in the form of a cake (then the placenta is thin) or spherical (then the placenta is thicker). In most cases, these types of children's places are not a pathology unless other changes or abnormalities are detected in them.
The retroplacental complex (RPC) is a very important part of the uterus, which includes a portion of the inner lining of the uterus, the muscular layer of the uterus and contains a large number of vessels that collect venous blood from the placenta. The width of the retroplacental complex can reach 1 cm, and the RPC is often mistakenly included in the “composition” of the placenta when measuring its thickness. In addition, RPC can be taken not only for “hypertonicity”, but also for hemorrhage, fibromatous nodes and other inclusions.
A “thin” placenta (less than 1.5 cm) is observed less frequently than a “thick” placenta, and is often the result of a malformation of the fetal place. The fetus is usually stunted. Rarely, a thin placenta is observed with such a serious complication as preeclampsia, which we will talk about in another chapter. This type of placenta can occur in women with congenital diabetes mellitus (Type 1).
A “thick” placenta (more than 5 cm) occurs in a number of diseases of the mother and fetus (acquired diabetes mellitus (Type 2), “Rhesus conflict”), and can be a sign of swelling of the fetal place in a number of viral infections of the mother (we are talking about primary infection with viruses , and not the carriage of viruses), as well as syphilis. In women with high blood pressure (hypertension), the placenta may be spherical in shape, so its thickness is often increased. A number of malformations of the placenta may be accompanied by greater thickness.
If the thickness of the placenta is more or less than the permissible norms, hasty treatment cannot be prescribed, because it is impossible to “cure” the placenta, just as it is impossible to rejuvenate it. Therefore, applications for “placenta treatment” are a manifestation of medical illiteracy. In addition to thickness, it is always important to take into account the structure of the placenta, and as I mentioned earlier, the condition of the baby. And here another unpleasant surprise awaits pregnant women - calcifications. “Oh, you, dear, have so much calcium. We will look for hidden infections. We will rejuvenate the placenta, otherwise you won’t carry it to term” – aren’t these the words most often heard by an “unhappy” pregnant woman?
By 12 weeks of pregnancy, the placenta becomes uniform in structure (homogeneity), but from the middle of the second trimester and in the third trimester, inclusions or formations may appear in the placenta, which will not always be a sign of something bad and dangerous for the fetus - in the form of cysts or lumps. The doctor’s task is to clearly determine the difference between “bad” and “good”, and monitoring the condition of the placenta and fetus over a certain period of time (2-4 weeks) will help him in this.
The deposition of calcium salts (phosphates) in the placenta is a normal, physiological phenomenon, and by the end of the second - beginning of the third trimester, calcium deposits can be noticed in the placenta in 50% of women; at the time of birth, in more than 75% of cases, the placenta has calcium deposits inclusions.
The problem is also that when performing an ultrasound, the homogeneity of the placenta and the presence of calcifications will depend on the “technical setting” of the contrast of the image on the screen of the ultrasound machine. To understand this, remember how the image of a black and white screen changes if you add contrast or reduce brightness. In such cases, the image “ripples”, doesn’t it?
Previously, the degree of placental calcification determined the maturity of the fetal lungs, that is, the child’s readiness for life outside the uterus. However, many studies have shown that there is no relationship between the amount of calcium deposits and the maturity of the fetal lungs. The classification of the degree of maturity of the placenta is used less and less in practice, since the determination of the degree (gradation) of maturity depends on what the specialist performing the ultrasound sees, that is, this is a subjectively dependent determination. When doctors found out that the degree of maturity of the placenta does not have any special practical significance in relation to the prognosis of pregnancy, it was assumed that the degree of maturity of the placenta is important in cases of maternal diseases (hypertension, diabetes mellitus, etc.), as well as in cases of growth and development abnormalities fetus But it turns out that these statements do not have serious clinical evidence, that is, this is just a theoretical assumption - practice shows that it is not placental calcification that is important in relation to pregnancy prognosis. But if you have been diagnosed with the degree of maturity of the placenta, then you should know that the norm is considered to be 1 and 2 degrees of maturity after 27 weeks of pregnancy, and 3 degrees of maturity after 32 weeks of pregnancy. If your maturity level is less, it’s okay, no need to worry. At the time of birth, half of the placentas with calcifications have the first degree of maturity, in almost 40% of cases the placenta has the second degree of maturity, and up to 20% have the third degree. This means that after 32 weeks, the first, second and third degrees of placental maturity are a manifestation of the norm. Therefore, the practical significance of determining the maturity of the placenta decreases significantly with the progress of pregnancy.
Rumors that the placenta of primiparous women has fewer calcium inclusions compared to the placenta of multiparous women has also been refuted by clinical studies. The number of calcium inclusions does not depend on the number of pregnancies. Also, no relationship was found between the number of inclusions and the age of the pregnant woman. The dependence of placental calcification on the season of the year has not been confirmed, although this was suggested in earlier clinical studies in the 70-80s.
Premature placental maturity is observed in pregnant women who smoke (5-15 cigarettes per day), and in such women, stage 3 placental maturity at the time of birth is more common. It is known that many women who smoke give birth to children with stunted growth, that is, small children. But when the placentas of the third degree of maturity of smoking women were compared with non-smoking women, the number of fetuses that were stunted was the same in both groups. This means that it is not the degree of vision (“aging”) of the placenta that plays a role in intrauterine growth retardation.
Returning to calcifications, their deposition is a normal (I repeat, normal) process of maturation (not aging!) of the placenta. Because if you find fault with the word “aging,” a logical question arises: doesn’t the fetus, with growth and development, age every day? Doesn’t a pregnant woman grow old during these nine months of bearing her offspring? So let's call a spade a spade. Modern obstetrics does not recognize placental calcification as a pathological sign.
There may be other inclusions in the placenta, which are not always a sign of a serious problem. For example, inclusions of fibrin (a breakdown product of blood) are often found, which is the result of small hemorrhages into the placental tissue in the form of tumor-like or thread-like deposits. Accumulations of blood (hematomas) as a result of small infarctions of the placenta occur in 25% of cases towards the end of pregnancy and at the time of birth.
Of all placental tumors, two types are more common: chorioangioma and teratoma. Small tumors most often do not affect the course of pregnancy. Women whose tumors are large require careful monitoring.
Cyst-shaped inclusions are also often detected during ultrasound. Single cysts usually do not pose a risk for pregnancy. Multiple cysts require medical attention and observation, as they may be a manifestation of trophoblastic disease. Hasty conclusions should not serve as a reason for premature termination of pregnancy.
With regard to the pregnancy prognosis (and this is what women are most often interested in), it is important to understand that from the point of view of modern medicine (I repeat: modern medicine, and not the medicine of 20 years ago) the placenta is abnormal. When it comes to the shape and structure of the placenta, the number of lobes is abnormal, because normally, although the baby’s place has up to 20 lobes, as a whole it consists of one large lobe. Two or more lobes of the placenta are not common (up to 3% of cases), usually one lobe is more developed, and the other is additional. In such cases, the woman is at risk for placental abruption and bleeding. There are also a number of other pathological forms of the placenta.
The size of the placenta also plays a role in pregnancy prognosis. Some doctors tried to measure the volume of the placenta, but it turned out that the volume of the placenta does not play a significant role in the performance of its function. And the place of attachment of the placenta, its proper growth and development plays a role, which is easier to determine by measuring the thickness of the placenta.
Placenta accreta poses a particular danger. Normally, between the placenta and the muscular layer of the uterus there is a corresponding layer that does not allow chorionic villi to penetrate into the muscular layer of the uterus. But in a number of cases, the development of this “protective” layer is disrupted, and such a disruption is most often observed in women who have undergone uterine surgery (cesarean section, removal of fibromatous nodes, abortion). In 2/3 of cases, not only placenta accreta is observed, but also placenta previa.
There are three forms of placenta accreta, depending on the degree of penetration of the chorion into the wall of the uterus and even beyond it: placenta accreta, placenta increta, placenta percreta. The last two types of placenta are the worst option, when the placental villi penetrate the entire muscular layer of the uterus, reaching the outer lining and beyond the uterus. Such a placenta can grow into the bladder or rectum, causing bleeding from these organs. Doctors mistakenly make other diagnoses (kidney stones, hemorrhoids, etc.), which leads to incorrect management tactics for such pregnant women. Therefore, if bloody discharge appears in urine or feces, it is necessary to undergo a thorough examination. Previously, in most cases, such a pregnancy ended in termination with the removal of the uterus and part of the damaged organ, but recently doctors have begun to use conservative treatment methods - after childbirth, the placenta is left in the uterine cavity and in some cases chemotherapy is prescribed.
In addition to changes in the placenta, changes in the membranes and umbilical cord can also be a manifestation of both normal and abnormal conditions. If any abnormalities in the development of the fetus are detected, a decision must be made to continue the pregnancy or terminate it, taking into account the duration of the pregnancy and the viability of the fetus outside the mother's body. If the fetus develops normally, without growth retardation, then such a pregnancy can be observed until birth.
Returning to the issue of placental insufficiency, I would like to touch upon the modern point of view on biochemical indicators of placental function, which are still used by some doctors in post-Soviet countries. In the late 60s and early 70s, a number of countries measured the level of the female hormone estriol, and it was assumed that women with low levels of this hormone had a significantly lower chance of bearing and giving birth to a child than with normal levels of this hormone. However, as practice has shown, this type of diagnosis had low sensitivity for most pregnancy complications, that is, in a number of serious obstetric problems, estriol levels were normal. In addition, it turned out that women with a normal pregnancy and normal outcome may also have low estriol levels. The course and outcome of pregnancy does not depend on the level of estriol. Therefore, this type of analysis has lost its practical value.
A little later, they began to determine another hormone - placental lactogen, however, in this direction, the data obtained were very contradictory and insignificant. It turned out that clinical studies to determine the relationship between lactogen levels and pregnancy outcomes were carried out very chaotically, with large errors. In addition, it turned out that deviations in lactogen levels from the norm were in the same number of women, both in the high-risk group and in the no-risk group. The outcome of high-risk pregnancies was taken into account, leading to the suggestion that lactogen levels are associated with poor pregnancy prognosis. But the pregnancy outcome in other groups (low risk and control) was missed, which from a scientific point of view reduces the practical value of such a clinical study to zero. Unfortunately, some doctors in post-Soviet countries still use the determination of biochemical blood markers to determine the function of the placenta, while abroad this type of diagnosis is a thing of the past.
The same can be said about the passion of our doctors for determining the “hormonal mirror” of a pregnant woman by studying cytological (cellular) smears from the surface of the cervix and vagina. For foreign doctors, such determination of hormonal levels has become history, and, simply put, why guess by cells when the levels of all necessary hormones and other substances can be determined in the blood? But behind all the biochemical tests lies one more truth - they are too expensive both for the budget of the medical institution and for the pregnant woman (depending on whose pocket the payment comes from), and with regard to the pregnancy prognosis, they are not very informative.
Thus, when talking about the placenta and its function, it is always important to look at the “end result” of its influence - the fetus. Let me remind you once again that there is no treatment for the placenta, its “rejuvenation,” and everything that Soviet and post-Soviet doctors prescribe is a tribute to old dogmatic traditions and reinsurance. You can treat a mother’s disease, and in some cases (rare cases) you can treat fetal diseases, but the approach must be individual and depend on the type of disease and the availability of appropriate medications in the obstetrics arsenal.
Share link:
- Click to share on WhatsApp (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Skype (Opens in new window)
- Send this to a friend (Opens in new window)
- Click to print (Opens in new window)
By
Why does the placenta age too early?
If an old placenta is diagnosed during pregnancy, this may be due to various factors.
Hypertension
Gestational hypertension , that is, increased blood pressure during pregnancy, is very often associated with the function of the placenta. Due to various reasons, defective blood vessels are formed in the child's place, and this affects both the condition of the fetus and the health of the woman. As a result, the expectant mother develops edema , high blood pressure, and sometimes, in severe cases, preeclampsia . A child, developing in the womb, does not receive enough oxygen due to defective blood vessels. As a result, the placenta has to “work” at full capacity, which is why it ages prematurely.
Infections
If the expectant mother falls ill with any infectious disease, then the placental tissue works more actively. It filters the mother's blood from viruses, allows more oxygen and antibodies to pass through to the baby in order to intensify the fight against the disease. As a result, its maturation and, accordingly, aging accelerates.
Eating Excessive Calcium
Calcium deposits are one of the main signs of aging in a child's place. The closer to the end of pregnancy, the more calcifications are detected in the placenta. And if a woman’s body constantly receives a large amount of this microelement, then gradually calcium replaces the placental tissue, which provokes its active premature aging. This often happens if a pregnant woman takes vitamin supplements uncontrollably.
How does maturation occur?
The formation of the organ begins 6-8 days after conception, when the fertilized egg attaches to the wall of the uterus and the chorionic villi grow into the endometrial tissue. Normally, the placentation process takes about 12-14 weeks. The baby's place takes its final form closer to the 20th week of gestation and from that moment on it completely ensures the metabolism between mother and child.
Active growth of placental tissue is observed throughout the first half of pregnancy. During this period, many blood vessels are formed in them, and the organ itself thickens. Starting from the middle of the second trimester, the development of the baby's place stops, its structure becomes more dense due to the appearance of salt deposits. Normally, the organ reaches maturity by the 36th week of gestation, after which its functions gradually fade away.
What does early maturation of the placenta lead to?
For every expectant mother who is interested in the dangers of early maturation of the placenta during pregnancy, it is important to realize that this phenomenon in itself is not a threat to the health of the mother and baby. Only if other signs of fetal aging are observed during aging can a health threat be noted. Such signs are the following manifestations:
- Severe intrauterine developmental delay.
- Violation of the fetal-placental and uteroplacental blood supply.
- Presence of signs of Rh conflict in the fetus.
- Severe hypertension in the mother.
- Diabetes mellitus in a pregnant woman (decompensated).
It is important to understand that even if there is no premature maturation of the placenta at 32 weeks of pregnancy or at another period, the conditions listed above are dangerous in themselves. In such conditions, special therapy is required, and in some cases, urgent delivery is necessary.
Causes of premature ripening of the placenta:
- Diseases of the expectant mother (diseases of the cardiovascular system, diabetes, hypertension, infectious diseases, etc.).
- Multiple pregnancy.
- Complications of pregnancy: Rh conflict, gestosis, hormonal disorders.
- Pathologies of the location of the placenta: low placentation, previa, and partial placental abruption.
- Excess calcium in the body of the expectant mother.
- Bad habits of a pregnant woman (drinking alcohol, drugs, smoking).
- Taking certain medications (medicines during pregnancy can only be taken as prescribed by a doctor).
- Poor environmental ecology.
What is an immature placenta and why is it dangerous?
If the placenta does not reach 2-3 degrees of maturity by the end of pregnancy, it is considered immature. This is a fairly rare occurrence; as a rule, it is associated with errors in the diagnostic process.
For example, if there is a Rh conflict between mother and fetus, then the baby’s place may “swell.” When an ultrasound examination is performed, due to the edematous smoothness, the placenta looks like it is at 0 degree of maturity. Therefore, an immature placenta is not a dangerous phenomenon, but such signs can often mask dangerous complications for the mother and child.
Norms for placental thickness, reasons for too low or high values
Over the course of 9 months, the baby's place is constantly growing and developing, and its thickness also changes. The gains are insignificant - an average of 2 mm per week. The standard indicators look like this: 20th week - 21.8 mm, 30th - 30.5 mm, 36th - 35.6 mm. At the end of pregnancy, the placenta thins a little; at 39-40 weeks its normal thickness is 34.1-33.5 mm. The parameter is checked using ultrasound.
Exceeding the standard values for the thickness of a child's seat may be associated with illness or poor lifestyle of the expectant mother. Changes in the parameter lead to disruptions in the functioning of the organ and create a certain danger for the life of the fetus.
Possible reasons for this phenomenon:
- infectious diseases;
- gestosis;
- anemia;
- Rhesus conflict;
- diabetes;
- smoking and drinking alcohol;
- drugs.
If ultrasound or Doppler sonography showed thickening of the placenta, the doctor prescribes drugs to the patient that stimulate uteroplacental exchange. They help stop the process of increasing the thickness of the baby's place and support the proper development of the lungs and other organs of the fetus. A baby's lungs are fully mature at 37-38 weeks. In the absence of obvious threats to the health of the child, the doctor limits himself to careful monitoring of the progress of the pregnancy.
Doctors often associate thinning of the walls of the placenta with organ hypoplasia (developmental failure). A decrease in the thickness of the baby's place compared to the norm is observed in women with a miniature physique. Other reasons:
- infectious diseases suffered by the expectant mother;
- hemolytic disease;
- hypertension;
- atherosclerosis.
Insufficient placental thickness caused by the disease can be corrected by timely treatment of the disease. For factors not related to diseases, the doctor prescribes drugs to the woman, the action of which is aimed at ensuring the normal development of the fetus and eliminating negative consequences for it. Along with the study of organ thickness parameters, special attention is paid to its maturity.
What additional research methods are practiced?
To determine the degree of maturity of the fetus and placenta and to diagnose or exclude dangerous conditions, additional research methods are practiced.
Ultrasound with Doppler
It is impossible to assess the child’s condition based on information about the degree of maturity of the placenta. Therefore, it is the data obtained from Doppler ultrasound that is considered to be indicators of a normal pregnancy.
Data is obtained due to the reflection of ultrasonic waves from a variety of biological media. They make it possible to assess blood circulation through the placenta. Provided that everything goes well, after 20 weeks the blood resistance in the vessels that connect the uterus, fetus and baby's place decreases. Thanks to stable resistance, oxygen and nutrients are constantly supplied to the fetus. If a good result was obtained during an ultrasound with Doppler, then there is no need to be afraid, even if during an ultrasound examination the placental tissue looks older than it should be at this moment.
It is also important to take into account that the opposite situation is possible: placental tissue may be of normal maturity, but it may not perform its functions as needed. Accordingly, this will negatively affect the child’s condition. Therefore, it is important to carry out regular examinations.
Cardiotocography CTG
This method is good because it makes it possible to assess the baby’s current condition. With the help of special sensors, it is possible to detect the fetal heartbeat, count the number of its movements, and register how the uterus contracts. The totality of the data obtained allows us to determine even the most minor disturbances in the functions of the placenta.
If an ultrasound examination reveals premature aging of the placental tissue, then it is necessary to perform CTG and Dopplerography to determine the condition of the child.
Possible pathologies
The most common violations:
- discrepancy between the pace of development of the placenta and the baby;
- the appearance of blood clots that obstruct blood flow;
- incorrect location of the organ;
- excessive thickening;
- heart attack - cessation of blood flow through the arteries;
- various inflammations, tumors.
The reasons for these phenomena may be:
- toxicosis;
- diabetes;
- atherosclerosis;
- infectious phenomena in the mother's body;
- Rhesus conflict;
- excessive or insufficient weight of a woman;
- emotional stress;
- bad habits;
- woman's age over 35 years.
It is important that the expectant mother monitors her own well-being throughout the entire period of carrying the child. The appearance of any unusual symptoms - vaginal discharge, pain, cramps, increased swelling should be a signal for urgent contact to our center.
How to stop the aging process?
If the doctor, based on research results, has concluded that the placental tissue is aging prematurely, then pregnant women, of course, worry about this and try to find out how to “rejuvenate” it. If it is diagnosed that aging of the placenta is stage 3 during pregnancy, or aging of a lesser degree, any attempts at “rejuvenation” are pointless.
Every expectant mother needs to be aware of the following:
- Immediately early maturation of the child's place is not a threatening condition for either the mother or the baby.
- If ultrasound reveals aging of the placental tissue, additional studies must be performed - CTG and Dopplerography. However, this fact is not a reason to worry.
- In the process of determining the maturity of a child's place, diagnostic errors occur quite often.
- If, in the course of additional studies, normal indicators of the fetal heartbeat and placental blood flow are determined, then the expectant mother has no reason to worry about the aging of the placenta.
- Provided that severe fetal hypoxia , then the condition of the pregnant woman and child must be monitored. The doctor makes a decision on treatment or emergency delivery.
- There are no drugs or methods to slow down the aging process of placental tissue.
- Currently, there is no evidence base regarding the use of Curantil , Actovegin , Pentoxifylline , multivitamin complexes, etc. for this purpose.
What to do if premature maturation of the placenta is determined?
If, during an ultrasound examination, the doctor suspects premature aging of the placenta, first of all you need to calm down, since early maturation of the placenta, as we have already noted, does not threaten the life and health of the expectant mother and child. But remember that further examination is indicated (ultrasound with Doppler, CTG), if everything is within normal limits, then there is no reason to worry.
In this case it is recommended:
- to walk outside;
- treatment of chronic and infectious diseases;
- eat properly and rationally;
- avoid stress;
- exclude serious physical activity;
- to refuse from bad habits.
If fetal hypoxia is determined by the results of ultrasound with Doppler and CTG, careful monitoring and treatment of the cause is required, and sometimes emergency delivery is necessary. There are no medications that can slow down the aging of the placenta. The drugs that are most often prescribed for premature ripening of the placenta (Actovegin, Chimes, multivitamins and other drugs) do not have a clear evidence base.
How to prevent early aging of the placenta?
To prevent such manifestations, a woman must be very careful in planning her pregnancy and in her lifestyle while carrying a baby. It is important to practice the following preventive measures:
- plan pregnancy;
- do not drink alcohol or smoke;
- practice moderate physical activity;
- to walk outside;
- carry out screenings, CTG, Doppler ultrasound in a timely manner;
- take Folic acid ;
- for anemia, take iron supplements;
- try to avoid crowds of people to prevent infection with infectious diseases.
If a woman is worried about certain indicators obtained during the examination, she should definitely seek additional advice from a doctor. Perhaps he will order additional examinations.