- Daclatasvir is an inhibitor of NS5A, an enzyme that is needed to assemble the virus from amino acids and RNA. The product prevents germs from spreading through the bloodstream, inhibits the development of infection, preventing infection of healthy cells. It reduces the likelihood of relapses. It has virtually no negative effects; the patient can maintain his usual lifestyle.
- Sofosbuvir is an inhibitor of NS5B, a key HVC enzyme. It prevents the multiplication of the virus and can be used for infections of all genotypes. It is characterized by good tolerability and a low probability of developing viral resistance. It is prescribed for decompensated liver function, fibrosis, and cirrhosis.
The combination of Daclatasvir and Sofosbuvir is used to treat hepatitis C of four genotypes. It has proven effective in treating hepatitis types 2 and 3, for the treatment of which in Russia previously only dual therapy was used, combining pegylated interferon and ribavierin. Sofosbuvir and Daclatasvir have virtually no side effects and allow you to cope with the virus in 12-24 weeks.
These are medications with direct antiviral action. They directly affect the functional proteins of the HVC virus. It cannot reproduce and dies. The result of the drugs ranges from 95-97%.
How and where to order Daclatasvir with Sofosbuvir
The cost of treatment with American drugs starts from $17,000. An alternative is patented medicines produced in India and Egypt. Their composition and formula are 100% identical to the original ones, and the price of the course starts from $900.
Sofosbuvir is not used in monotherapy. In therapeutic regimens it is combined with Daclatasvir or Ledipasvir. The cost of therapy and the treatment regimen depend on the combination of medications the doctor prescribes.
- Contact your doctor. Let them know you plan to use this combination. Before treatment, you need to take two tests: to determine the infectious load and to determine the HVC genotype.
- After determining the initial parameters, the doctor will prescribe a dosage regimen, timing, and write a prescription for medications. Sofosbuvir and Daclatasvir are taken in two different tablets, and with Ledipasvir - in one tablet.
- The minimum course is 3 months. You need to get tested every two weeks. After the course, a control blood test is carried out, and if necessary, the dosage regimen is adjusted.
- The presence of HVC virus in the blood should be monitored 2-3 months and six months after treatment.
Direct antiviral drugs for the treatment of chronic viral hepatitis C
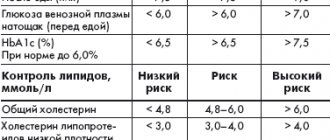
To prescribe a course of treatment, an examination is necessary, and during treatment, monitoring the effectiveness and safety of treatment in accordance with the recommendations of the European Association for the Study of the Liver.
According to the mechanism of action, all drugs are inhibitors of various viral proteases: NS3, NS4, NS5A, NS5B. Different combinations of drugs allow recovery, with a probability of up to 100% in some cases. Among the drugs there are pangenotypic, that is, effective for all genotypes, and drugs that act only on certain genotypes of the virus (1a, 1b, 2a/b, 3a/c).
SOFOSBUVIR, an NS5B inhibitor, should be taken at a dose of 400 mg (1 tablet) once a day. It is used only in combination with other DAA drugs or with ribavirin and interferon.
Sofosbuvir is excreted mainly (60%) by the kidneys in the urine, so its administration requires caution in patients with kidney disease.
Sofosbuvir enters into drug-drug interactions with many drugs, so you should be careful about concomitant diseases and adjust the intake of drugs prescribed for the treatment of these diseases.
LEDIPASVIR , an NS5B inhibitor, is available in combination with sofosbuvir (400 mg sofosbuvir and 90 mg ledipasvir). Dose: 1 tablet per day, regardless of meals.
Because ledipasvir interacts with other drugs, precautions should be taken with frequent monitoring of renal function. In addition, it is important to consider whether patients are taking statins and medications in their antiretroviral (HIV) therapy regimen.
DACLATASVIR is an NS5A inhibitor - 1 tablet of 60 mg per day is used in combination with other DAA drugs, including sofosbuvir, or ribavirin with interferon. Numerous drug interactions with daclatasvir require careful attention when prescribing it and appropriate monitoring when using it.
VIKEIRA PACK is a complex drug that includes 4 active ingredients (ritonavir, which enhances the effect of paritaprevir, ombitasvir and dasabuvir). The recommended dose is 2 tablets of ritonavir/paritaprevir/omnitasvir once a day with meals, as well as dasabuvir 2 times a day. When prescribing, numerous drug interactions should be taken into account, as well as the class of cirrhosis.
VELPATASVIR – NS5A inhibitor, 100 mg once a day. Effective for all genotypes of the virus. The drug is used in combination with sofosbuvir and voxilaprevir - VOSEVY . Its effectiveness has been shown in the retreatment of patients with unsuccessful therapy and the formation of mutations.
MAVIRET is a combination of glecaprevir with pribrentasvir in patients with any genotype; it is also recommended for retreatment, since mutations do not affect the treatment outcome.
SIMEPREVIR is an NS3/4A inhibitor - one 150 mg capsule should be taken per day. Patients taking simeprivir should be treated with other drugs, in particular antiretrovirals, with caution.
ASUNAPREVIR is an NS3/4A protease inhibitor, used 100 mg 2 times a day. The drug is prescribed in combination with daclatasvir, as well as in regimens with ribavirin and interferon.
NARLAPREVIR – NS3 protease inhibitor (domestic drug), 200 mg, 1 tablet per day, used in combination with ribavirin and interferon, with the mandatory inclusion of ritonavir in the treatment regimen. There are a number of restrictions when used simultaneously with other medications. Contraindication is cirrhosis of the liver class B and C.
Why is Sofosbuvir prescribed with Daclatasvir?
The combination of these medications is used for antiviral treatment of infections of all genotypes. Sometimes ribavierin is added to them. PEG-IFN is not used in treatment. The therapeutic regimen was approved by the FDA in 2015-16.
The drugs enhance each other's effects, reduce the viral load and reduce liver damage. They cure hepatitis C in 97% of cases. To make therapy more effective, follow your doctor's recommendations. Stick to a diet, completely give up alcohol, smoking, and give your body some physical activity.
European Assistance employees provide advice on the use of antiviral drugs and organize hepatitis treatment in India.
Return to list
Sofosbuvir in the treatment of chronic HCV infection: hopes and facts
Only 20 years have passed since the discovery of the hepatitis C virus, and the problem of treating chronic HCV infection is acute throughout the world. There is a constant search for new drugs and new effective treatment regimens, so the therapeutic landscape is changing rapidly.
Until now, the standard treatment for chronic hepatitis C (CHC) has been a combination of peginterferon and ribavirin. A thorough understanding of the biology of hepatitis C virus (HCV) has led to the identification and isolation of specific proteins directly involved in the process of viral replication. Newly developed drugs, so-called. protease inhibitors and polymerase inhibitors target these proteins.
Two years ago, two new drugs from the group of protease inhibitors appeared in our field of vision - boceprevir and telaprevir. These pharmacological agents have improved patient response to treatment, but they also bring with them a number of limitations. Thus, protease inhibitors showed antiviral activity against only HCV genotype 1. Moreover, these drugs provoke the development of viral resistance to treatment, which can lead to therapeutic failures and have multiple pharmacokinetic interactions with other drugs. In addition, these drugs are used in combination with standard therapy with peginterferon and ribavirin, which has extensive and well-studied side effects, the aggravation of which is inevitable when adding telaprevir or boceprevir to therapy.
Of course, assessment and treatment of unwanted side effects is an integral part of the treatment of CHC. Both patients and doctors are awaiting the development and introduction into clinical practice of new therapeutic agents with less toxic properties.
Recently, 2 groups of researchers (Jacobson et al. and Lawitz et al.) published the results of their work[1,2]. This involved the use of sofosbuvir, a new polymerase inhibitor, in four clinical trials in patients with chronic hepatitis C. In three randomized trials - FISSION, POSITRON and FUSION - researchers focused on analyzing the effectiveness of the treatment in patients with genotypes 2 or 3 who had not received prior treatment. this other therapy, or who refused interferon therapy due to severe adverse reactions or did not respond to previous therapy. All studies had similar endpoints: sustained virological response at 12 weeks after the end of therapy (SVR12). And in the open-label NEUTRINO study, the authors studied the effectiveness of sofosbuvir in patients with genotypes 1, 4, 5 or 6.
Let us briefly consider the design and results of these works. The FISSION study evaluated the efficacy of sofosbuvir plus ribavirin for 12 weeks compared with standard peginterferon alfa-2a plus ribavirin for 24 weeks. Standard treatment was successful in 78% of patients with genotype 2 and 63% of patients with genotype 3 HCV, compared with success rates of 97% and 56%, respectively, in the sofosbuvir group.
The purpose of the POSITRON study was to analyze the effectiveness of sofosbuvir plus ribavirin compared with placebo in a population of patients who are not suitable for interferon-based therapy. Such reasons could be pre-existing mental disorders (57%) or autoimmune disorders (19%). In the placebo group, no patients reached the endpoint, while 93% of patients with genotype 2 and 61% with genotype 3 in the sofosbuvir group achieved a sustained virological response.
The FUSION study focused on patients without a sustained response to interferon-based therapy. Sofosbuvir and ribavirin treatment groups were compared for 12 weeks and 16 weeks. Four additional weeks of treatment had clinically significant success in increasing the SVR rate from 86% to 94% in those with genotype 2 and from 30% to 62% in those with genotype 3.
In addition, data from the NEUTRINO study on the overall antiviral effects of sofosbuvir against all genotypes of hepatitis C virus were obtained. The results of this study indicate the achievement of a cumulative SVR of 90% of cases in patients with genotype 1 (89%), genotype 4 (9%) and genotype 5 or 6 (2%) received a combination of sofosbuvir, peginterferon, or ribavirin for 12 weeks.
The speed of development of drugs to treat chronic HCV infection is unprecedented. Publications of data from clinical studies using sofosbuvir appeared 3 years after publications regarding the discovery of the chemical formula of the active substance. Although the results of the studies highlighted in the review are very encouraging, there are some issues with the study design.
In accordance with the principles of evidence-based medicine, the results of randomized clinical trials are qualitatively superior to those of open-label studies. However, of the studies discussed here, only three were randomized and only one was placebo-controlled. In addition, the results of these studies are somewhat inferior to the previous study by Gane et al.[3], in which the SVR rate was 100%. One reason for this difference may be the less rigorous study design of Gane et al. And using a different endpoint. The FDA has only recently approved the clinical trial endpoint of SVR after 12 weeks of therapy (previously SVR after 24 weeks of therapy was used).
Modern therapy for CHC revolves around the development of side effects from interferon therapy with intensive monitoring of patients. With the advent of an alternative to interferon, we expect a new leap in the treatment of this pathology. The results of studies using sofosbuvir suggest rapid changes in clinical practice. However, note that ribavirin is still the most effective drug when using interferon-free regimens. Thus, data from Gane et al. indicate that the effects of sofosbuvir are compromised when ribavirin is excluded from therapy. The use of ribavirin in this category of patients also requires close attention, because associated with the development of hemolytic anemia. In this regard, the results of Jacobson et al. are interesting. and Lawitz et al. on the safety of the combination of sofosbuvir and ribavirin, which showed a low level of anemia and leukopenia in patients compared to the standard treatment regimen. On the other hand, we understand that there have been no long-term studies involving large patient populations, and with widespread use of a new drug, new adverse events may be discovered.
What conclusion can be drawn based on the evidence base currently available to us on the use of sofosbuvir? Low incidence of side effects, relatively short treatment period, high rate of achievement of SVR in individuals with different HCV genotypes when using the sofosbuvir-ribavirin regimen and, possibly, less effort spent by both doctors and patients in the treatment of CHC. Perhaps the next step in this area is to analyze combinations of sofosbuvir with other agents that directly target the virus in order to potentiate the effects. Whether interferon will remain in its therapeutic niche or whether other drugs will take its place is still unknown. But we can confidently say that we are on the threshold of transformation.
Source: Joost PH Drenth, HCV Treatment - No More Room for Interferonologists?N Engl J Med 2013; 368:1931-1932, 2013, DOI: 10.1056/NEJMe1303818
Literature
- Jacobson IM, Gordon SC, Kowdley KV, et al. Sofosbuvir for hepatitis C genotype 2 or 3 in patients without treatment options. N Engl J Med 2013;368:1867-1877
- Lawitz E, Mangia A, Wyles D, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med 2013;368:1878-1887
- Gane EJ, Stedman CA, Hyland RH, et al. Nucleotide polymerase inhibitor sofosbuvir plus ribavirin for hepatitis C. N Engl J Med 2013;368:34-44
Treatment regimens for chronic viral hepatitis with direct antiviral drugs
The choice of the most effective regimen for the patient is carried out by a hepatologist, taking into account the degree of liver damage (there are restrictions in the case of a high class of cirrhosis), the genotype of the virus and concomitant chronic diseases, since most drugs have pronounced drug-drug interactions. Sometimes it is necessary to take into account the experience of previous unsuccessful treatment with interferon drugs, as this increases the likelihood of initial drug resistance mutations in the virus, which reduces the possibility of recovery.
The duration of therapy depends on the degree of liver damage and the presence of compensated or decompensated cirrhosis. The standard course is 12 weeks, for cirrhosis it can be increased to 24 weeks.
It is possible to prescribe ribavirin in addition to the treatment regimen in patients with cirrhosis and with negative prognostic factors for response to treatment.
For the treatment of patients with genotype 1 (1a and 1b), there are 4 recommended regimens of direct antiviral drugs:
Sofosbuvir+Ledipasvir
Sofosbuvir+Simeprevir
Sofosbuvir + Daclatasvir
Sofosbuvir+Velpatasvir
Vikeira Pak (genotype 1b – 12 weeks, genotype 1a – 24 weeks).
Daclatosvir + Aunaprevir – 24 weeks
For the treatment of patients with genotypes 2 and 3, there are two interferon-free regimens that can also be used for other genotypes - pangenotypic regimens.
Sofosbuvir+daclatasvir
Sofosbuvir + velpatasvir
New, increasingly effective and safe drugs with direct antiviral action are constantly being introduced into clinical practice. Information about them regularly appears on our website.