The phenomenon of aminophenylbutyric acid
Perhaps the most interesting of all drugs currently existing in our country is aminophenylbutyric acid (ABA), known under such trade names as Anvifen [1], Phenibut [2], Noofen [3]. ROS is considered as a nootropic, tranquilizing, psychostimulant, antiplatelet and antioxidant agent [4, 5]. Some domestic experts believe that ROS improves the functional state of the brain by normalizing tissue metabolism [4]. Accordingly, in adult patients the drug is recommended for the treatment of TFR (neurotic) [6], asthenic conditions [7], including in patients with schizophrenia [8]. But ROS has a particularly wide range of indications in childhood. The drug is recommended for TFR [9], asthenic conditions [10], mild tic disorders and stuttering [11, 12], sensorineural hearing loss [4], ADHD [13]. Finally, the possibilities of using ROS in addiction medicine are discussed. Thus, some foreign publications report the advisability of prescribing the drug to patients with alcoholism [14]. It is indicated that ROS contributes to the relief of withdrawal syndrome, as well as the reduction of pathological craving for alcohol. Is it possible to imagine a drug that is both a tranquilizer and a psychostimulant? More than half a century ago, a natural inhibitory neurotransmitter, γ-aminobutyric acid (GABA), was discovered in the central nervous system. Its study under experimental conditions (for example, when administered directly into the brain of experimental animals) helped to clarify how the processes of natural (physiological) inhibition occur (Table 1).
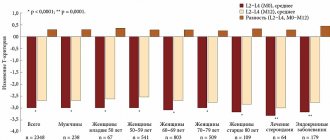
It turned out that GABA acts on several types of GABA receptors, the most important of which are GABAA and GABAB (Table 1). The main function of the former is to transmit a signal from one GABA neuron to another (Fig. 1, 2). Moreover, GABAA receptors are a channel through which, after exposure to the natural neurotransmitter GABA, negatively charged chlorine ions (ionotropic receptor) quickly penetrate. At the same time, the “charge” of GABA neurons changes, and they lose the ability to perceive stimulating electrical signals. This is why GABA demonstrates an anticonvulsant effect in animal experiments [15].
At the same time, GABA neurons, into which chloride ions have penetrated, become activated themselves and begin to release a significant amount of “new” GABA (Fig. 1). This neurotransmitter acts on GABAA receptors on other GABA neurons. In this case, the inhibition spreads further. It also passes to other neurons: histamine (HI), acetylcholine (AC), norepinephrine (NA), glutamate (GLU), domaphine (DA) [17, 18]. To do this, GABA already affects the GABAB receptors located on these nerve cells (Fig. 1). Unlike GABAA receptors, they are a protein molecule, part of which is located outside the neuron, and part is inside it. Once GABA acts on the “outer” part of the protein, a chain of successive chemical reactions is initiated that allows the signal to pass through the membrane. Subsequently, enzymes located inside the neuron enter into reactions, and its metabolism changes (metabotropic receptor). In this case, nerve cells stop releasing their neurotransmitters (histamine, acetylcholine, norepinephrine, glutamate), i.e., they inhibit their main activity (Table 1). However, the effect of GABA on dopamine neurons is not so clear (Table 1). To begin with, GABA neurons also have GABAB receptors (Fig. 1, 2). The latter are necessary for self-regulation of physiological inhibition [17, 18]. If GABA affects these GABAB receptors, then the GABA neurons are inhibited. On the one hand, this mechanism prevents hypersedation, but on the other hand, it contributes to the fact that GABA can not only reduce, but also increase the activity of dopamine neurons [19]. It is believed that this is due to a significant difference in the sensitivity of GABAB receptors. Those located on GABA neurons are very sensitive to GABA. These GABAB receptors respond even to small amounts of “their” neurotransmitter (Fig. 2). In contrast, those receptors located on dopamine neurons are less sensitive to GABA. They react only to a significant amount of “foreign” neurotransmitter. That is why if there is little GABA, then the activity of GABA neurons, which inhibit dopamine cells, initially decreases (Fig. 2). And they, on the contrary, increase their activity. And only when the amount of GABA increases does this neurotransmitter finally reach the GABAB receptors on dopamine neurons, and they stop releasing dopamine. Finally, in addition to the processes of physiological inhibition, GABA is involved in the regulation of the endocrine system [20]. It is assumed that GABA affects “its” neurons located in the hypothalamus and pituitary gland. At the same time, the neurotransmitter has multidirectional effects on the secretion of growth hormone (somatotropic hormone (GH)), which has an anabolic effect, manifested in enhancing protein synthesis, inhibiting its breakdown, as well as reducing subcutaneous fat deposits and accelerating its combustion. In particular, acting on GABA neurons in the hypothalamus region, GABA promotes the release of GH, and in the pituitary gland - a decrease in its secretion. The presented properties of GABA (the natural nature of inhibition, its self-regulation, anticonvulsant effect, lack of hypersedation) could not but seem encouraging. The idea immediately arose to use this substance to treat pathological processes accompanied by excessive excitation of neurons, for example, epilepsy [21]. Soon, GABA was synthesized in the laboratory, and this drug was supplied to medical institutions under various trade names [22, 23]. GABA began to be prescribed to patients with epilepsy. And the first experience of such treatment seemed quite successful [21]. Later it turned out that there was a positive placebo effect. GABA, being a non-lipophilic substance, practically does not penetrate the BBB [24], and therefore, the effect on patients was not so much the drug itself as the doctors’ belief in its impressive pharmacological properties [21]. As soon as this became known, scientists around the world turned to the search for new GABAergic drugs that can cause inhibition of neurons. As a result, the first benzodiazepines were synthesized quite quickly, capable of easily crossing the BBB (Table 1) [25]. These drugs, by their chemical nature, were in no way similar to GABA and subsequently even received the special name “positive allosteric modulators of the GABAA receptor” [16, 25]. Such a complex, at first glance, term means only that: 1) benzodiazepines are attached to GABAA receptors on the opposite side from the place where GABA interacts with it (allosteric - from the Greek άλλος - other and στερεός - spatial), 2 ) at the same time, they sharply increase the ability of GABA to influence the activity of the receptor (positive modulator). It seems, however, that these drugs are even better described as a catalyst for the physiological inhibition caused by GABA. The fact is that benzodiazepines by themselves are not active and, in the absence of GABA, are not capable of causing any effect at all [16]. But their addition to GABA leads to a sharp increase in inhibition, which, in contrast to the usual - physiological - can be designated as “generalized”. Indeed, benzodiazepines dramatically increase the ability of GABA neurons to resist stimulating electrical signals (Fig. 3). As a result, all of these GABAergic drugs are, to one degree or another, endowed with an anticonvulsant effect (Table 1). In addition, benzodiazepines cause GABA neurons to release large amounts of GABA, sufficient to rapidly inhibit various neurons (including dopamine neurons) and cause hypersedation [26]. Finally, it has been found that benzodiazepines can suppress the activity of the endocrine system and, in particular, help reduce the secretion of GH [27].
The high efficiency of the mechanism of action of benzodiazepines, along with the above-mentioned ability to penetrate the BBB, predetermined their widespread use in clinical practice [25]. However, there have always been groups of patients (outpatients, drivers, students, the elderly, etc.) in whom these GABAergic drugs could not be used due to serious problems associated with the pronounced nature of inhibition. That is why the search for new drugs with a different mechanism of action continued. At the same time, a completely understandable idea arose - to return to GABA. After all, if it is nevertheless “dragged” through the BBB, then it will be possible to take advantage of the “physiological” inhibition of neurons. Then, on the initiative of Professor I.P. Lapin from the Institute. V.M. Bekhterev at the Department of Organic Chemistry of the Pedagogical Institute named after. A.I. Herzen synthesized a new GABAergic drug – AOS [15]. It was obtained by attaching a phenyl ring to GABA, which adds lipophilic properties to the molecule. As a result, ROS easily penetrates the BBB (Table 1). However, due to a change in the structure of the molecule, ROS has its own mechanism of inhibition, which is neither physiological nor generalized (Table 1, Fig. 4). And this new option, perhaps, can be described as “selective”. Indeed, unlike benzodiazepines, ROS does not enhance the effects of GABA, but itself plays its role. Moreover, ROS has only one of the two GABA mechanisms. Thus, ROS can influence GABAB receptors (GABA receptor agonist, from the Greek ἀγωνιστής - enemy fighter), located on various neurons. In addition, this effect is less pronounced than that of GABA itself [15]. As a result, selective inhibition is of a moderate nature, inferior in strength to physiological and even more generalized. This is why ROS does not have an anticonvulsant effect and does not cause hypersedation. There is also no scientific data indicating the effect of ROS on the endocrine system and, in particular, the release of GH.
But the selective version of inhibition is associated not only with a decrease in neuronal activity, but also with a more noticeable (in comparison with GABA) revival of dopamine nerve cells (Table 1). This is due to the already mentioned differences in the sensitivity of GABAB receptors, as well as the weaker (in comparison with GABA) influence of ROS on them. As a result, this drug is able to inhibit dopamine neurons only in very significant doses that go beyond therapeutic limits. Thus, ROS has two main components of the mechanism of action that are important for the clinical use of the drug: inhibitory (↓GLU, ↓NA, ↓ACCh, ↓GI)1 and activating (↑DA) (Table 1). The first of them (inhibitory - ↓GLU, ↓NA, ↓ACCh, ↓HI) can be required in numerous pathological conditions, whose pathogenesis is associated with an increase in the activity of glutamate, norepinephrine, acetylcholine and histamine neurons (Table 2). These disorders have never been studied by a single medical specialty. On the contrary, their study involved psychiatrists, neurologists, cardiologists, pulmonologists, etc. That is why a large number of medical terms from different classes of the ICD 10th revision have to be used to designate the disorders in question [28]. Benzodiazepines are often used in clinical practice to treat these disorders. And this tactic seems completely justified taking into account the mechanism of action of these drugs (Table 1). However, it was already mentioned above that there are numerous groups of patients in whom generalized inhibition, often associated with hypersedation, will create certain problems during pharmacotherapy. In this situation, it seems preferable to use a moderate inhibitory component of the ROS mechanism of action. Better tolerability of therapy will also be facilitated by the fact that ROS (unlike benzodiazepines) has an activating component of the mechanism of action (↑DA). Meanwhile, dopamine activity is necessary for the implementation of the functions of the intellectual and motor spheres of both adults and children [16]. It is dopamine neurons that are responsible for the development of motivation, the reinforcement system, and, consequently, goal-directed behavior in the process of learning any new skills. Additionally, dopamine neurons are extremely important for switching from one task to another. Finally, they are also responsible for emotions, the organization of precise movements and their smoothness, and also regulate the endocrine system. That is why indications for prescribing ROS may be various disorders associated with increased activity of glutamate, norepinephrine, acetylcholine and histamine neurons (Table 2) in “problem” groups of patients. These groups include patients: 1) children or the elderly; 2) receiving treatment on an outpatient basis, 3) engaged in study or work involving intellectual and/or motor activity.
It is obvious that all the presented indications are by no means new and only clarify those available in reference books [1]. In addition, they are widely discussed in the literature. But there are other pathological conditions in which it is advisable to resort to prescribing the drug. Unfortunately, these disorders are practically not reflected in the testimony; they are much less often mentioned in publications. Perhaps this is explained by the complex pathogenesis of such pathological conditions that arise due to a decrease in the activity of some neurons (dopamine) and an increase in others (norepinephrine and/or acetylcholine) (Table 3).
In addition, the treatment of these disorders often requires both activating (↑DA) and inhibitory (↓GLU, ↓NA, ↓ACH, ↓GI) components of the ROS action mechanism. As an example, let us take ADHD, the pathogenesis of which is associated with a decrease in the activity of dopamine neurons and an increase in norepinephrine neurons. Traditional approaches to the treatment of this syndrome, unfortunately, are far from rational. In particular, in our country, when treating ADHD, they hope to “activate” certain “reserves” of the central nervous system [29] through piracetam, vinpocetine and even polypeptides extracted from the “cerebral cortex of cattle, as well as pigs” [30]. Meanwhile, it is not entirely clear how these very different drugs affect the exchange of dopamine and norepinephrine. On the contrary, the activating component of the ROS action mechanism directly involves an increase in the activity of dopamine neurons, and the inhibitory component – a decrease in norepinephrine neurons (Table 1). The pathogenesis of complications of pharmacotherapy for schizophrenia is also quite complex (Table 3), which in our country are aggravated by long-term prescription of high-potency neuroleptics (for example, haloperidol) [31]. Meanwhile, these drugs inhibit various dopamine neurons, which in some cases is accompanied by a reciprocal increase in the activity of other nerve cells: acetylcholine and norepinephrine (Table 3). As a result, patients experience a variety of disorders associated with emotions, motor skills and the endocrine system. To combat these complications, it is usually recommended to discontinue medications, replace one drug with another, more tolerable one, and also prescribe correctors (anticholinergics) for a short time [32]. Unfortunately, in our country, this modification of neuroleptic therapy is preferred to the constant (usually long-term) use of a powerful anticholinergic – trihexyphenidyl. Meanwhile, this leads to the development of even more severe and intractable side effects, such as tardive dyskinesia [33]. The possibility of at least partially improving the described situation is associated with the fairly common practice of prescribing tranquilizers for schizophrenia [32] - as a rule, these are benzodiazepines used to treat psychopathic and neurosis-like symptoms. It seems, however, that the administration of AFC in the cases under consideration will contribute not only to the implementation of these “tactical” goals of therapy, but also to the prevention of tardive dyskinesia. Indeed, unlike benzodiazepines, the mechanism of action of ROS (Table 1) allows one to increase the activity of dopamine neurons (the activating component) and reduce it in acetylcholine and norepinephrine neurons (the inhibitory component). As a result, ROS will help relieve the side effects of antipsychotics. At the same time, it will be possible to reduce the dose of trihexyphenidyl, and therefore the risk of developing tardive dyskinesia (Table 3). Thus, some disorders associated with a decrease in the activity of dopamine neurons and an increase in norepinephrine and acetylcholine neurons may also be indications for the administration of ROS (Table 3). Moreover, for ADHD, this drug can be used as monotherapy. As for the various side effects of neuroleptics, it is advisable to use ROS as an additional medication. Interestingly, however, the inherent selective inhibition of ROS largely precludes its non-medical use. Indeed, based on the mechanism of action presented above, the drug is able to activate dopamine neurons, but only in therapeutic doses [15]. It is under these conditions that ROS will act on the GABA receptors of GABA neurons, which inhibit dopamine nerve cells. But if the dose of the drug increases, it will “reach” the GABAB receptors located on dopamine neurons. As a result, they will slow down and stop releasing dopamine. Meanwhile, one of the most important mechanisms for the formation of dependence is the possibility of increasing the dose of a substance in order to overcome tolerance to it or addiction to its effects. Obviously, an attempt to increase the dosage of ROS will inevitably lead not to an increase in the activity of dopamine neurons, but to their inhibition. That is why, according to foreign researchers, people who use this drug for non-medical reasons actually cannot go beyond the therapeutic range [34]. In turn, this leads to the fact that ROS, even in the complete absence of any medical supervision, remains a safe drug. Cases of serious complications (hypersedation, withdrawal syndrome) when using ROS for non-medical reasons are quite rare, and deaths do not occur at all [34–40]. The presented data on the mechanism of action of ROS also allow us to express some thoughts regarding the advantages and disadvantages of various drugs containing the active substance in question. Thus, the advantages of selective inhibition make it possible to use ROS in patients of all ages (including children over 3 years old), as well as in a large number of pathological conditions. This is why it seems very convenient to use tablets that contain different amounts of ROS. In this case, optimal opportunities are created for individual selection of doses. The drug Anvifen meets exactly these requirements [1]. It is available in doses of 50 and 250 mg. At the same time, other drugs containing ROS as an active substance are available only in the highest of the listed dosages (250 mg). Concluding this review of the literature, it is advisable to emphasize that in the context of the coexistence of many opinions regarding the clinical use of a drug, one can always resort to an analysis of its mechanisms of action. Comparison of the pharmacological properties of a drug with modern data on the pathogenesis of disorders allows us to judge with a high degree of confidence the validity of certain indications for prescribing a drug.
Gamma-amino-beta-phenylbutyrate hydrochloride
International name of the medicinal substance:
Gamma-amino-beta-phenylbutyrate hydrochloride The list of drugs containing the active substance Gamma-amino-beta-phenylbutyrate hydrochloride is given after the description.
Pharmacological action:
Nootropic agent, facilitates GABA-mediated transmission of nerve impulses to the central nervous system (direct effect on GABA receptors), also has an anxiolytic, psychostimulating, antiplatelet and antioxidant effect.
Improves the functional state of the brain by normalizing tissue metabolism and influencing cerebral circulation (increases the volumetric and linear velocity of cerebral blood flow, reduces cerebral vascular tone, improves microcirculation, and has an antiplatelet effect). Helps reduce or eliminate feelings of anxiety, tension, restlessness and fear, normalizes sleep, and has some anticonvulsant effect. Does not affect cholinergic and adrenergic receptors. Extends the latent period and shortens the duration and severity of nystagmus. Reduces manifestations of asthenia and vasovegetative symptoms (including headache, feeling of heaviness in the head, sleep disturbances, irritability, emotional lability), increases mental performance. Improves psychological indicators (attention, memory, speed and accuracy of sensory-motor reactions). When taken as a course, it increases physical and mental performance, improves memory, and normalizes sleep; improves the condition of patients with motor and speech disorders. Patients with asthenia feel better from the first days of therapy; increases interest and initiative (motivation of activity) without sedation or agitation. When prescribed after severe TBI, it increases the number of mitochondria in the perifocal areas and improves the course of bioenergetic processes in the brain. In case of neurogenic lesions of the heart and stomach, it normalizes the processes of lipid peroxidation. In older people it does not cause workload and excessive lethargy; the relaxing aftereffect is most often absent. Improves microcirculation in the tissues of the eye, reduces the inhibitory effect of ethanol on the central nervous system. The drug is low toxic. Pharmacokinetics:
Absorption is high, penetrates well into all tissues of the body and through the blood-brain barrier (about 0.1% of the administered dose of the drug penetrates into brain tissue, and in young and elderly people to a much greater extent). Evenly distributed in the liver and kidneys. Metabolized in the liver - 80-95%, metabolites are pharmacologically inactive. Does not accumulate. After 3 hours it begins to be excreted by the kidneys, while the concentration in the brain tissue does not decrease and it is detected in the brain for another 6 hours. About 5% is excreted unchanged by the kidneys, partially with bile.
Indications:
Asthenic and anxious-neurotic conditions, anxiety, fear, obsessive-compulsive neurosis, psychopathy.
Stuttering and tics in children, enuresis, urinary retention due to myelodysplasia. Insomnia and nightmares in the elderly. Prevention of anxiety states that arise before surgical interventions and painful diagnostic tests (premedication). Meniere's disease, dizziness associated with dysfunctions of the vestibular analyzer of various origins (including otogenic labyrinthitis, vascular and traumatic disorders); prevention of motion sickness during kinetosis. Primary open-angle glaucoma (as part of combination therapy). As an auxiliary drug in the treatment of alcoholism (for the relief of psychopathological and somatovegetative disorders during withdrawal syndrome). In combination with generally accepted detoxification drugs, the drug can be used to treat predelirious and delirious conditions in alcoholism. Contraindications:
Hypersensitivity. Caution.
Erosive and ulcerative lesions of the gastrointestinal tract, liver failure, pregnancy, lactation. Side effects:
Increased irritability, agitation, anxiety, dizziness, headache, drowsiness, nausea (at first doses), allergic reactions (skin rash, itching). Overdose.
Symptoms: severe drowsiness, nausea, vomiting, fatty liver (ingestion of more than 7 g), eosinophilia, decreased blood pressure, impaired renal function. Treatment: gastric lavage, activated carbon, symptomatic therapy. Interaction:
Prolongs and enhances the effect of hypnotics, narcotic analgesics, antiepileptic, antipsychotic and antiparkinsonian drugs.
Special instructions:
With long-term use, it is necessary to monitor liver function indicators and peripheral blood patterns.
It is necessary to refrain from potentially hazardous activities that require increased attention. Ineffective for severe motion sickness (“uncontrollable” vomiting, dizziness, etc.). Preparations containing the active substance Gamma-amino-beta-phenylbutyric acid hydrochloride:
Phenibut-ANVI, Phenibut-LekT
The information provided in this section is intended for medical and pharmaceutical professionals and should not be used for self-medication. The information is provided for informational purposes only and cannot be considered official.
Phenibut tablets 250 mg 30 pcs
Registration Certificate Holder
SORBENT (Russia)
Dosage form
Medicine - Phenybut
Description
Pills
white or white with a slightly yellowish tint, round, biconvex, scored.
1 tab.
aminophenylbutyric acid hydrochloride (phenibut) 250 mg
Excipients
: lactose monohydrate - 180 mg, potato starch - 56 mg, povidone K30 - 9 mg, calcium stearate monohydrate - 5 mg.
10 pieces. — cellular contour packages (1) — cardboard packs. 10 pieces. — cellular contour packages (2) — cardboard packs. 10 pieces. — cellular contour packages (3) — cardboard packs. 10 pieces. — contour cell packaging (5) — cardboard packs.
Indications
Asthenic and anxious-neurotic states, anxiety, fear, obsessive-compulsive neurosis, psychopathy. Stuttering and tics in children, enuresis. Urinary retention due to myelodysplasia. Insomnia and nightmares in the elderly. Prevention of anxiety states that arise before surgical interventions and painful diagnostic tests (premedication).
Meniere's disease, dizziness associated with dysfunctions of the vestibular analyzer of various origins (including otogenic labyrinthitis, vascular and traumatic disorders); prevention of motion sickness during kinetosis.
Primary open-angle glaucoma (as part of combination therapy).
As an auxiliary therapy in the treatment of alcoholism (for the relief of psychopathological and somatovegetative disorders during withdrawal syndrome).
Treatment of predelirious and delirious states in alcoholism (in combination with conventional detoxification agents).
Contraindications for use
Hypersensitivity to phenibut.
pharmachologic effect
The nootropic agent is gamma-amino-beta-phenylbutyric acid hydrochloride. Facilitates GABA-mediated transmission of nerve impulses to the central nervous system (direct effect on GABA receptors), and also has an anxiolytic, psychostimulating, antiplatelet and antioxidant effect.
Improves the functional state of the brain by normalizing tissue metabolism and influencing cerebral circulation (increases the volumetric and linear velocity of cerebral blood flow, reduces cerebral vascular tone, improves microcirculation, and has an antiplatelet effect). Helps reduce or eliminate feelings of anxiety, tension, restlessness and fear, normalizes sleep, and has some anticonvulsant effect.
Does not affect cholinergic and adrenergic receptors.
Extends the latent period and shortens the duration and severity of nystagmus.
Reduces manifestations of asthenia and vasovegetative symptoms (including headache, feeling of heaviness in the head, sleep disturbances, irritability, emotional lability), increases mental performance.
Improves psychological indicators (attention, memory, speed and accuracy of sensory-motor reactions).
When taken as a course, it increases physical and mental performance, improves memory, and normalizes sleep; improves the condition of patients with motor and speech disorders. Patients with asthenia feel better from the first days of therapy; increases interest and initiative (motivation of activity) without sedation and excitement. When used after severe TBI, it increases the number of mitochondria in the perifocal areas and improves the course of bioenergetic processes in the brain.
In case of neurogenic lesions of the heart and stomach, it normalizes the processes of lipid peroxidation. In older people it does not cause workload and excessive lethargy; the relaxing aftereffect is most often absent. Improves microcirculation in the tissues of the eye, reduces the inhibitory effect of ethanol on the central nervous system. Low toxic.
Drug interactions
Extends and enhances the effect of sleeping pills, narcotic analgesics, antiepileptic, antipsychotic and antiparkinsonian drugs.
Dosage regimen
Inside, regardless of food intake. The dose, frequency of administration and duration of treatment depend on the indications, age of the patient, and tolerability. A single dose for adults varies from 20 mg to 750 mg, for children - from 20 mg to 250 mg.
Side effect
From the side of the central nervous system:
increased irritability, agitation, anxiety, dizziness, headache, drowsiness.
From the digestive system:
nausea (at first doses).
Allergic reactions:
skin rash, itching.
special instructions
Use with caution in case of erosive and ulcerative lesions of the gastrointestinal tract, liver failure.
With long-term use, it is necessary to monitor liver function indicators and peripheral blood patterns.
Ineffective for severe symptoms of motion sickness (including uncontrollable vomiting, dizziness).
Impact on the ability to drive vehicles and operate machinery
During the treatment period, it is necessary to refrain from potentially hazardous activities that require increased attention and high speed of psychomotor reactions.
Use during pregnancy and breastfeeding
Restrictions during pregnancy - With caution. Restrictions when breastfeeding - With caution. Use with caution during pregnancy and lactation.
Use for liver dysfunction
Restrictions for liver dysfunction - With caution.
Use with caution in case of liver failure.