Eglonil
Eglonil (sulpiride) is a neuroleptic antipsychotic used for the treatment of psychosomatic disorders (anorexia nervosa, hallucinosis, bulimia, amentia, alcoholism, involutional hysteria, depression of various origins, etc.). Eglonil has been widely used in the treatment of psychosomatic disorders for more than two decades. It is distinguished from other antipsychotic drugs by its low incidence of unwanted side reactions, as well as its stimulating effect on the central nervous system: the drug invigorates, improves mood, and improves the overall psycho-emotional background. The main effects of the drug are antiasthenic, anxiolytic, antidepressant, and antihypochondriacal. It should be noted that the severity of the antidepressant and anxiolytic effects of Eglonil is comparable to those of classical antidepressants and anxiolytics. Clinical studies of Eglonil have proven its effectiveness as an adjuvant in the treatment of diseases of the cardiological, pulmonological, dermatological, neurological, and gastroenterological profiles. The safety and good tolerability of the drug are determined by such characteristics as lack of addiction, lack of suppressive effect on daytime work ability, and lack of liver and kidney toxicity. Undesirable side effects (mainly extrapyramidal disorders) when taking the drug are relatively rare and disappear immediately after stopping drug therapy.
In most cases, they develop when taking submaximal and maximum doses. Patients who already have extrapyramidal disorders (parkinsonism), as well as elderly people, should take Eglonil with extreme caution and under medical supervision. In patients suffering from severe renal failure, the dose should be halved (a possible alternative is an intermittent course of medication). One of the properties of Eglonil is a decrease in the threshold of convulsive readiness, which should be taken into account when prescribing the drug to people suffering from epilepsy. Eglonil is incompatible with ethanol, so alcohol consumption should be avoided during treatment. While taking Eglonil, it is recommended to exclude activities associated with increased attention and concentration (driving a car, working with potentially dangerous mechanisms). The inhibitory effect of the drug on the central nervous system is enhanced when taken together with opioids, tranquilizers, clonidine, sleeping pills and central antitussives. Eglonil potentiates the effect of antihypertensive drugs when used together and increases the risk of orthostatic hypotension. Levodopa reduces the effectiveness of Eglonil. Lithium carbonate and fluoxetine, when used together with Eglonil, increase the risk of developing extrapyramidal reactions.
Eglonil (in gastroenterology)
Eglonil
(eng.
Eglonil
) - an antipsychotic, a dopamine receptor blocker, used in gastroenterology as a prokinetic agent.
Dosage forms and composition of Eglonil
Eglonil is (was) approved in Russia in the form of the following dosage forms:
- tablets containing 200 mg of active substance - sulpiride
- capsules containing 50 mg sulpiride
- solution for intramuscular administration, in the form of ampoules containing 100 mg of sulpiride each
- oral solution in 200 ml glass bottles containing 1 mg of sulpiride (5 mg of sulpiride in 1 ml of solution)
In addition, Eglonil tablets contain excipients: potato starch, magnesium stearate, talc, lactose monohydrate, colloidal silicon dioxide, hypromellose.
Indications for use of Eglonil
In psychiatry and neurology:
- all forms of schizophrenia
- acute delirious states
- depression and neuroses
In psychiatry and neurology (50 mg capsules):
- children over 6 years of age: severe behavioral disorders (agitation, self-harm, stereotypy), especially in combination with autism syndromes
In gastroenterology (only as an additional remedy):
- psychosomatic symptoms in peptic ulcers of the stomach and duodenum, hemorrhagic rectocolitis and other diseases.
Method of use of Eglonil and dose in the treatment of the digestive system
In the treatment of gastroenterological diseases, Eglonil is used only as part of complex therapy. Eglonil in the treatment of GERD
. One of the main reasons leading to an increase in spontaneous relaxations of the lower esophageal sphincter is an increase in the level of neuroticism in patients suffering from GERD; testing is relevant to assess the personality profile and correct the identified disorders. To assess the personality profile of patients with pathological gastroesophageal reflux identified by pH-metry, psychological testing is carried out, on the basis of which the dependence of the nature and severity of gastroesophageal reflux on individual personality characteristics is revealed and, along with standard therapy, patients with a depressive personality type are prescribed Eglonil 50 mg 3 times a day, which improves the prognosis of the disease (Maev I.V. et al.). In the presence of psychoform disorders in the form of anxiety, fear, irritability, masked and overt depression, Eglonil 50 mg 2-3 times a day for 3-4 weeks is widely used for GERD. Eglonil is an atypical analeptic; it has a prokinetic effect on the motility of the esophagus of the stomach and intestines due to the blockade of dopaminergic receptors, which explains its antiemetic effect. In addition, eglonil has axiolytic (anti-anxiety) and antidepressant effects (Degtyareva I.I.).
Egonil in the treatment of duodenostasis in combination with hypomotor dyskinesia of the gallbladder
. For compensated and subcompensated duodenostasis, the prokinetic agents metoclopramide or domperidone are prescribed, in addition to which it is possible, especially in the presence of depressive states, to use Eglonil 50 mg 2-3 times a day or 2 ml of a 5% solution intramuscularly 1-2 times a day (Maev I .V., Samsonov A.A.).
In the treatment of peptic ulcer with symptoms of vegetative neurosis in children
Eglonil 0.005 mg per kg of the child’s weight in 2 doses, morning and afternoon, gives a good effect (Shabalov N.P.).
Comparison of Eglonil with other drugs regarding the effect on the electrical activity of the upper gastrointestinal tract
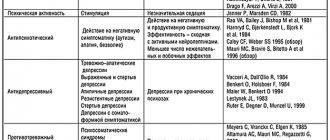
Using the Gastroscan-GEM gastroenteric monitor, a comparative study of the effect of Eglonil, the “classical” prokinetic agent Motilium and the myotropic antispasmodic Duspatalin on the electrical activity of the upper gastrointestinal tract was carried out. The data obtained is shown in the table below:
| A drug | Group affiliation | Pi/Ps | Kritm | Ai/As | Pi/Pi+1 | |||
| stomach | DPK | stomach | DPK | stomach | DPK | stomach/duodenal | ||
| Eglonil | antipsychotic | pad | pad | pad | pad | pad | pad | No |
| Motilium | prokinetic | height | pad | height | height | height | height | norm |
| Duspatalin | myotropic antispasmodic | pad | pad | No | No | No | No | No |
Abbreviations: growth
- the indicator of peripheral electrogastrography increases after taking the drug,
decline
- decreases,
no
- the drug does not affect the indicator,
normal
- taking the drug normalizes the indicator. For indicators of electrical activity—peripheral electrogastrography indicators Pi/Ps, Kritm, Ai/As and Pi/Pi+1, see “Electrogastroenterography: study of the electrical activity of the stomach and intestines.” Duodenum - duodenum.
Eglonil reduces the electrical activity Pi/Ps, the rhythmicity of Kritm and the amplitude of contractions Ai/As of both the stomach and duodenum. Prokinetic Motilium increases the electrical activity of the stomach Pi/Ps and reduces the electrical activity of the duodenum, increases the rhythmicity of Kritm contractions of the upper gastrointestinal tract and normalizes the coordination of contractions of the stomach and duodenum Pi/Pi+1. The myotropic antispasmodic Duspatolin reduces the electrical activity of the stomach and duodenum Pi/Ps and does not affect the rhythm of Kritm and the coordination of contractions Pi/Pi+1 of the upper gastrointestinal tract (Smirnova G.O.).
Eglonil, like other prokinetics, have a predominantly stimulating effect on the smooth muscles of the gastrointestinal tract. In particular, it increases the tone and contractile activity of the stomach and duodenum, improves antroduodenal coordination, accelerates the evacuation of gastric contents and small intestinal transit (Avdeev V.G.):
Rice.
The effect of Eglonil on the motor function of the duodenum (Avdeev V.G.) a - motility on an empty stomach, b - motility after administration of Eglonil; 1 — manometry in the upper horizontal part of the duodenum; 2 — pH-metry in the upper horizontal part of the duodenum; 3 — pH-metry in the distal part of the duodenum. On the website gastroscan.ru in the literature catalog there is a section “Prokinetics”, containing medical articles concerning the treatment of diseases of the gastrointestinal tract with various prokinetics, including Eglonil.
general information
According to the pharmacological index, Eglonil belongs to the group “Neuroleptics”.
According to ATC, Eglonil is included in the group “N05A Antipsychotic drugs” and has the code “N05AL01 Sulpiride”. Eglonil is available from pharmacies with a prescription.
Other drugs containing the active ingredient sulpiride
The following drugs with the active substance sulpiride are (have been) registered in Russia: Betamax, Vero-Sulpiride, Prosulpin, Sulpiride, Sulpiride Belupo, Eglek.
In the USA, Canada and Australia, sulpiride is not approved for use. In many countries of the European Union, Latin America and Southeast Asia it is sold under the trade name Dogmatil. In the UK - Dolmatil, Sulpiride and Sulpor. In Japan - Abilit, Betamac T, Dogmatyl, Keityl, Margenol, Miradol, Pyrikappl, Skanozen, Sulpiride Choseido, Sulpiride Kyowa Yakuhin, Sulpiride Taisho, Sulpiride Taiyo, Sulpiride Towa Yakuhin, Youmathyle, as well as under many other trade names in various countries around the world .
Eglonil has contraindications, side effects and application features; consultation with a specialist is necessary.
Back to section
Instructions for use EGLONIL
Sedatives
It should be taken into account that many drugs and substances can have additive effects on the central nervous system and contribute to decreased alertness. These drugs include morphine derivatives (analgesics, antitussives and replacement therapies), antipsychotics, barbiturates, benzodiazepines, non-benzodiazepine anxiolytics (such as meprobamate), hypnotics, sedative antidepressants (amitriptyline, doxepin, mianserin, mirtazapine, trimipramine), sedatives H1 -antihistamines, centrally acting antihypertensives, baclofen and thalidomide.
Drugs likely to cause torsade de pointes
This serious heart rhythm disorder can be caused by a number of medications, both antiarrhythmic and non-antiarrhythmic. Hypokalemia is a contributing factor, as is bradycardia or pre-existing or acquired QT prolongation.
This includes, in particular, antiarrhythmic drugs of classes Ia and III.
As for erythromycin, spiramycin and vincamycin, this interaction concerns only dosage forms for intravenous administration.
The simultaneous use of two drugs that can cause torsades de pointes is generally contraindicated.
However, methadone, as well as some subclasses, are an exception:
- antiparasitic drugs (halofantrine, lumefantrine, pentamidine) are not recommended only in combination with other drugs that can cause ventricular tachycardia “torsades de pointes”;
- neuroleptics that can cause torsades de pointes are also not recommended, but are not contraindicated in combination with other drugs that can cause torsades de pointes.
Contraindicated combinations
Non-antiparkinsonian dopaminergic receptor agonists (cabergoline and kinagolide)
There is mutual antagonism between dopaminergic receptor agonists and antipsychotics.
Levodopa:
- mutual antagonism of the effects of levodopa and antipsychotics.
Combinations not recommended
Antiparasitics that can cause torsade de pointes (halofantrine, lumefantrine, pentamidine)
Increased risk of ventricular arrhythmias, in particular torsade de pointes. If possible, treatment with the azole antifungal agent should be interrupted. If its use is unavoidable, check the QT interval and perform ECG monitoring before treatment.
Antiparkinsonian dopamine agonists (amantadine, apomorphine, bromocriptine, entacapone, lisuride, pergolide, piribedil, pramipexole, ropinirole, selegiline)
There is mutual antagonism between dopaminergic receptor agonists and antipsychotics. If possible, interrupt treatment with azole antifungals. The above drugs may cause or worsen psychosis. If treatment with an antipsychotic is necessary for a patient suffering from Parkinson's disease and receiving a dopaminergic antagonist, the dose of the latter should be gradually reduced until discontinuation (abrupt withdrawal of dopaminergic agonists can lead to the development of neuroleptic malignant syndrome).
Other drugs that can cause torsade de pointes: class Ia (quinidine, hydroquinidine, disopyramide) and class III antiarrhythmics (amiodarone, sotalol, dofetilide, ibutilide) and other drugs such as bepridil, cisapride, difemanil, i.v. in erythromycin, mizolastine, IV vincamine, moxifloxacin, IV spiramycin
Increased risk of ventricular arrhythmias, in particular torsade de pointes.
Other antipsychotics that can cause torsade de pointes (amisulpride, chlorpromazine, cyamemazine, droperidol, haloperidol, levomepromazine, pimozide, pipothiazine, sertindole, sulpiride, sultopride, tiapride, veraliprid)
Increased risk of ventricular arrhythmias, in particular torsade de pointes.
Alcohol
Alcohol enhances the sedative effect of neuroleptics. Impaired attention creates a danger for driving vehicles and working on machines. The consumption of alcoholic beverages and the use of medications containing alcohol should be avoided.
Levodopa
Mutual antagonism between levodopa and antipsychotics.
Patients suffering from Parkinson's disease should be prescribed the minimum effective dose of both drugs.
Methadone
Increased risk of ventricular arrhythmias.
Combinations requiring precautions during use
Beta blockers for heart failure (bisoprolol, carvediol, metoprolol, nebivolol)
Increased risk of ventricular arrhythmias. Clinical monitoring and ECG control are required.
Drugs that cause bradycardia (especially class Ia antiarrhythmics, beta blockers, some class III antiarrhythmics, some calcium channel blockers, digitalis glycosides, pilocarpine, anticholinesterases)
Increased risk of ventricular arrhythmias. Clinical monitoring and ECG control are required.
Drugs that reduce potassium levels in the blood (potassium-sparing diuretics, alone or in combination, stimulant laxatives, glucocorticoids, tetracosactide and IV amphotericin B)
Increased risk of ventricular arrhythmias.
Before prescribing, any hypokalemia should be corrected and clinical monitoring, as well as electrolytes and ECG, should be performed.
Sucralfate
Gastrointestinal absorption of sucralfate and sulpiride is reduced.
Intervals between the use of sucralfate and sulpiride should be observed (more than 2 hours, if possible).
Topicals for gastrointestinal use, antacids and charcoal
Gastrointestinal absorption of sulpiride is reduced.
Intervals between the use of these agents and charcoal should be observed (more than 2 hours, if possible).
Combinations to Consider
Antihypertensive drugs
Strengthening the hypotensive effect and increasing the possibility of postural hypotension (additive effect).
Beta blockers (except esmolol and sotalol and beta blockers used for heart failure)
Vasodilator effect and risk of hypotension, especially postural (additive effect).
Nitrates, nitrites and related products
Increased risk of hypotension, particularly postural.
CNS depressants,
including narcotics, analgesics, sedative H1-antihistamines, barbiturates, benzodiazepines and other anxiolytics, clonidine and its derivatives.