Relevance
Patients with residual invasive breast cancer (BC) after neoadjuvant therapy are at increased risk of recurrence.
The rate of complete response to therapy among patients with HER2-negative primary breast cancer reaches 13-22%. However, in patients who do not achieve a complete response after neoadjuvant therapy (taxane and anthracycline), the relapse rate may be 20-30%. Capecitabine, a fluoropyrimidine carbamate derivative, has demonstrated efficacy as an adjuvant therapy for gastrointestinal cancer. However, the effectiveness of the drug in patients with breast cancer is not known.
Clinical perspectives of capecitabine
About the article
15248
0
Regular issues of "RMZh" No. 14 dated 07/06/2006 p. 1016
Category: General articles
Authors: Markovich A.A. , Gorbunova V.A.
For quotation:
Markovich A.A., Gorbunova V.A. Clinical perspectives of capecitabine. RMJ. 2006;14:1016.
The antitumor activity of drugs from the antimetabolite group is inextricably linked with DNA synthesis, so they are most active in fast-growing cells. A characteristic feature of pyrimidine analogues is the need to undergo “lethal synthesis” under the action of enzymes in order to turn into biologically active nucleotides, enzyme inhibitors. Drugs in this group include 5-fluorouracil (5-FU) and other fluorine derivatives. The effectiveness of 5-fluorouracil was first shown in the early 60s of the last century, and since then this drug has remained one of the main drugs in the treatment of many solid tumors, especially tumors of the gastrointestinal tract. 5-fluorouracil has shown its high activity in advanced colorectal cancer, both in monotherapy and in combinations with other cytostatics, as well as in adjuvant treatment.
Over the past time, many drug administration regimens have been proposed and tested (bolus, daily infusions, long-term continuous infusions, chronomodulated regimens, etc.), and the use of biomodulators that increased the effectiveness of 5-fluorouracil (methotrexate, interferons, levamisole, leucovorin) was justified ). To date, the best results have been obtained with long-term intravenous administration of high doses of 5-fluorouracil. The main side effects of treatment are mucositis, diarrhea, myelodepression and, with infusion administration, palmar-plantar syndrome, which is characterized by numbness, paresthesia, tingling, swelling, redness, peeling, blistering, desquamation and severe pain; The cardio- and neurotoxic effects of fluoropyrimidines have also been described. The use of daily infusions of 5-FU requires permanent central venous access and is associated with a high risk of complications associated with the installation of a central catheter. This regime disrupts the patient’s usual rhythm of life, as it implies the patient’s stay in the hospital, which, in turn, requires large expenses on the part of the medical staff. The use of 5-FU in bolus mode has one advantage - the possibility of use in an outpatient setting. However, its low efficiency and unpredictable, poorly controlled toxicity, especially in DPD syndrome (unexpectedly severe toxicities in the form of stomatitis, diarrhea, neutropenia and neurotoxicity due to insufficient activity of dihydropyrimidine dehydrogenase, the enzyme responsible for the catabolism of 5-FU), limits its widespread use in clinical practice. The obvious inconvenience of using such regimens and the difficulties of outpatient treatment encourage researchers to search for more effective, safe and easy-to-use forms of fluoropyrimidines. Xeloda (capecitabine) is a good example of the development of a highly effective and safe oral fluoropyrimidine. Xeloda is a non-toxic metabolite that is converted by thymidine phosphorylase (TF) to 5-fluorouracil directly in the tumor (selective activation). TF is one of the enzymes of DNA synthesis in a tumor, identical in structure and function to tumor-associated angiogenesis factor and platelet-derived endothelial growth factor; is highly active in most human solid tumors and directly correlates with rapid tumor growth and aggressive invasion. In addition, TF prevents the apoptosis of cancer cells. It has been proven that overexpression of TF leads to increased angiogenesis and is associated with an unfavorable prognosis in breast cancer, colorectal cancer, gastric, bladder, ovarian, and kidney cancer (Fig. 1). Thus, due to the high expression of TF, the concentration of active 5-fluorouracil in the tumor after taking Xeloda is 127 times higher than its concentration in plasma. At the same time, after the introduction of 5-fluorouracil, these ratios do not change. This explains the high efficiency and relatively low toxicity of Xeloda (Table 1). Oral Xeloda therapy, designed to mimic long-term infusions of 5-FU, offers a number of benefits for both patients and clinicians. The dominant adverse events associated with taking the drug are skin reactions (hand-foot syndrome), reactions from the gastrointestinal tract (nausea, mucositis, diarrhea) and weakness. Cases of myelosuppression occur quite rarely, and manifestations of alopecia are minimal. All types of toxicity can be controlled quite well by modifying drug doses or by temporarily interrupting treatment. A wide spectrum of antitumor activity, low toxic profile, the ability to control adverse events and ease of use make Xeloda an optimal drug for use in outpatient practice. The favorable safety profile opens up prospects for the use of Xeloda in the second and subsequent lines of chemotherapy, for the treatment of elderly patients and debilitated patients. In an experiment with transplantation of human breast and colon cancer cells into mice, it was shown that drugs such as cyclophosphamide, mitomycin C, docetaxel, paclitaxel, and gemcitabine can increase the activity of TF in the tumor. This provided the basis for studying the use of Xeloda in combination with potentially synergistic drugs in various localizations. Radiation therapy has the same effect. Currently, capecitabine is widely used to treat breast and colorectal cancer. The XELOX (Xeloda 1000 mg/m2 2 times a day 1–14 days + oxaliplatin 130 mg/m2 on the 1st day IV, cycle 3 weeks) and XELIRI (irinotecan 200 mg/m2 30–min.) regimens have been shown to be highly effective. IV infusion on day 1 + Xeloda 1000 mg/m2 2 times a day from the evening of day 1 to the morning of day 15, cycle 21 days) in the first line of treatment of metastatic colorectal cancer. The X-AST study has also been completed, according to the results of which Xeloda is recommended for adjuvant therapy of colon cancer. The use of capecitabine for pancreatic, ovarian, and cervical cancer is practiced. Its study has begun in combination with platinum drugs for solid tumors of the head and neck and non-small cell lung cancer. Research is being conducted on its use in patients with disseminated gastric cancer. The range of antitumor drugs active in gastric cancer is quite narrow; the most studied standard of monochemotherapy is 5-fluorouracil, the effectiveness of which in disseminated gastric cancer does not exceed 21%, therefore studies of the effectiveness of Xeloda in this pathology, both in monotherapy and in combination, are quite justified . Analysis of the pharmacokinetics of the drug showed its good absorption in patients who had previously undergone gastrectomy, which allows capecitabine to be successfully used in this category of patients (Table 2). The effectiveness of Xeloda monotherapy ranges from 19–34%. Currently, capecitabine is being actively studied in various combinations, presented in Table 3, as 1st line of treatment. Based on the results of the phase II Korean study of Xeloda in combination with cisplatin [13], the following dosage regimens are recommended: Xeloda 1000 mg/m2x2 r/day. on days 1–14 + cisplatin 60–80 mg/m2 on day 1 (cycle 21 days). Currently, a randomized phase III study has been organized comparing this regimen with the standard regimen: cisplatin 80 mg/m2 on day 1 + 5-FU 800 mg/m2/day x 24 hours on days 1–5. In the studies by Evans [6] and Shin [10], capecitabine was used in the ECF regimen instead of infusional 5-FU. A dose of capecitabine 2000 mg/m2/day, given daily on days 1–14 followed by 1 week of rest along with two other drugs administered intravenously every 3 weeks, was determined to be active and well tolerated. Currently, the phase III REAL2 study is being conducted to compare the effectiveness and tolerability of four combinations: 1) epirubicin 50 mg/m2 daily + cisplatin 60 mg/m2 daily every 3 weeks + 5-FU continuous infusion 200 mg/m2/day; 2) epirubicin 50 mg/m2 every day + oxaliplatin 130 mg/m2 every day every 3 weeks + 5-FU continuous infusion 200 mg/m2/day; 3) epirubicin 50 mg/m2 every day + cisplatin 60 mg/m2 every day every 3 weeks + capecitabine 1000 mg/m2/day. days 1–21; 4) epirubicin 50 mg/m2 per day + oxaliplatin 130 mg/m2 per day every 3 weeks + capecitabine 1000 mg/m2/day. Days 1–21. The planned duration of treatment is 24 weeks. According to preliminary results, the effectiveness of combinations of epirubicin with platinum derivatives and 5-FU was 35%, and with capecitabine – 41% [14]. Currently, the departments of chemotherapy and outpatient methods of diagnosis and treatment of the State Institution Russian Cancer Research Center named after. N.N. Blokhin Russian Academy of Medical Sciences is conducting a study of two chemotherapy regimens, including Xeloda. Regime A – cisplatin 80 IV drips on day 1 + capecitabine 1000 mg/m2 2 times a day from the evening of day 1 to the morning of day 15 of each cycle, cycle – 21 days. Regime B – oxaliplatin 100–120 mg/m2 IV drip on day 1 + capecitabine 1000 mg/m2 2 times a day from the evening of day 1 to the morning of day 15 of each cycle, cycle – 21 days. The study included 74 patients with morphologically verified locally advanced or disseminated gastric cancer. Group A included 31 patients aged 29 to 73 years (median 55.6); 15 men and 16 women. Group B included 16 patients aged 46 to 76 years (median 59.9); 11 men and 5 women. All patients received 2 or more courses of chemotherapy. Total carried out: gr. A – 122 courses, gr. B – 69 courses. In group A, the complete effect was achieved in 3 patients, which was 9.7%, partial regression in 13 patients (41.9%); stabilization in 8 (25.5%). In group B - complete effect in 2 patients (12.5%), partial regression in 5 (31.25%) and stabilization in 8 (50%). The overall effectiveness of the cisplatin + Xeloda regimen was 51.6%, and the oxaliplatin + Xeloda regimen was 43.75%. Median survival has not been reached. Preliminary data indicate that two-component regimens are well tolerated (the severity of side effects generally does not exceed grade 1–2), which ensures safety and the possibility of long-term treatment in an outpatient setting. Many patients do not lose their usual activity and even continue their professional activities. The main types of toxicity were: leukopenia 3 tbsp. (in group A – 2 courses – 1.6%, in group B – 0); grade 3 granulocytopenia (group A – 4 courses – 3.3%, group B – 0), 4 tbsp. (group A – 1st course – 0.8%); hand-foot syndrome stage 3 was noted in one case in gr. A, treatment for this patient was stopped; anemia 3 degrees was observed over 7 courses in gr. A (5.7%). However, it should be taken into account that the study included patients with initially low hemoglobin levels, requiring intensive symptomatic therapy before the start of chemotherapy (use of iron supplements, erythropoietins, red blood cell transfusion). In such patients, in parallel with the implementation of the effect of specific treatment, the level of hemoglobin reached normal levels. Preliminary analysis indicates the effectiveness of two platinum-containing regimens, including capecitabine, but the oxaliplatin + Xeloda regimen is better tolerated. Capecitabine is being actively studied in other gastrointestinal malignancies. Modern treatment regimens for disseminated pancreatic cancer (in particular, the use of gemcitabine and high doses of 5-FU) have led to an increase in the objective effect, control of symptoms and an extension of the median survival of patients. Therefore, studies where 5-FU was replaced by capecitabine were logical. Xeloda 1250 mg/m2 2 times a day on days 1–14 in mono mode showed an objective effect in 10% of cases, stabilization in 40%, with a median survival of 6 months. The use of Xeloda 650–1000 mg/m2 2 times a day, days 1–21, in combination with weekly administration of gemcitabine 1000 mg/m2 was effective in 14–33% with stabilization in 35–58%. Median time to progression is 6 months, median survival is 8–10 months. Attempts are currently being made to study three-component combinations. Thus, Xeloda 1000–1500 mg/m2 2 times a day, days 1–14, in combination with gemcitabine 750 mg/m2 (days 4 and 11) and docetaxel 30 mg/m2 (days 4 and 11) showed an objective effect of 47 %, stabilization in 31% (n = 44). Xeloda 650 mg/m2 2 times a day (days 1–14) in combination with gemcitabine 800 mg/m2 (days 1 and cisplatin 60 mg/m2 (on day 1) showed an objective effect in 30% of cases, stabilization in 35%. Median time to progression - 5.1 months, median survival - 7.5 months (n = 40). The use of synergy between capecitabine and radiation therapy led to an increase in survival to 11-14 months, with one-year survival of 69% of patients Of interest are studies of the effectiveness of Xeloda in biliary tract cancer.At a dose of 650 mg/m2 2 times a day (days 1–14, cycle 21 days) in combination with gemcitabine 1000 mg/m2 (on days 1 and 8), the objective effect was 26 %, stabilization – 12%, time to progression – 6.8 months, survival – 10.3 months (n = 35) Xeloda 1000 mg/m2 2 times a day (days 1–14) with mitomycin C, 8 mg/m2 (on day 1), achieved an objective effect of 31–33%, stabilization in 13–34%, time to progression of 5.3–6.3 months, with overall survival of 9.3 months and one year survival rate 41–70% (n = 64). The research results give hope for improved results of treatment of cholangiocellular cancer compared to 1978–1989, when 20 to 29% of patients survived one year. Xeloda is also being studied for tumors of the female genital area. In particular, for ovarian cancer, in the second and subsequent lines of treatment, at a dose of 1250 mg/m2 2 times a day for 3 weeks, an objective effect was achieved - 10-19%, stabilization - 21-49%, median time to progression – 3–4 months with overall survival – 8 months. When using Xeloda 600 mg/m2 2 times a day on days 1–14 and gemcitabine 1000 mg/m2 on days 1 and 8, the objective effect is 60%, stabilization is 20%, the median time to progression is 3 months. Research on the use of Xeloda in cervical cancer is also important. Since at the moment the main methods of treating this pathology are surgery and radiation, the use of chemotherapy as a sensitizer for radiation therapy has good prospects. Currently, the standard treatment in combination with radiation therapy is cisplatin. However, everyone knows its severe side effects, in particular, nephrotoxicity and myelosuppression, which significantly limits the use of cytostatics in patients with medical history and in elderly patients. In combined treatment of patients with stage 2B–3B, using Xeloda at a dose of 825 mg/m2 2 times a day, 5 days a week, weekly, and radiation therapy 1.8 Gy per day, an objective effect was obtained in 87% of patients, median time before progression was 7.5 months. In patients who had previously received treatment, Xeloda at a dose of 1250 mg/m2 2 times a day every 3 weeks showed an objective effect in 13–17% of cases, stabilization in 42–53% of cases, with a median overall survival of 9.3 months. Xeloda (1000 mg/m2 2 times a day on days 1–14) in combination with cisplatin (50 mg/m2 1 time every 3 weeks) showed an objective effect of 57%, stabilization in 21%, with a median time to progression of 14 months . Xeloda's high selective efficacy, low toxic profile, and ease of use will allow it to occupy a leading position in modern chemotherapy for malignant neoplasms. References 1. Kondo K, Chin K, Sakamoto J, et al. Modified capecitabine regimen for advanced/metastatic gastric cancer: final results from multicenter phase II trial. Eur J Cancer 2003; 1(suppl.5):S69 (Abstr 221). 2. Koizumi W, Saigenji K, Ujiie S, et al. A pilot phase II study of capecitabine in advanced or recurrent gastric cancer. Oncology 2003; 64:232–6. 3. Hong YS, Song SY, Lee SI et al. A phase II trial of capecitabine in previously untreated patients with advanced or metastatic gastric cancer. Ann Oncol 2004; 15:1344–7. 4 Leon-Rodriguez E, Green D, Candelaria M, et al. Oral capecitabine in treatment of patients with advanced or metastatic gastric carcinoma. Ann Oncol 2002; 13(Suppl.5): 191 (Abstr 708P). 5 Kim TW, Kang YK, Ahn JH, et al. Phase II study of capecitabine plus cisplatin as first–line chemotherapy in advanced gastric cancer. Ann Oncol 2002; 13:1893–8. 6.Evans TR, Pentheroudakis G, Paul, et al. A phase I and pharmacokinetics study of capecitabine in combination with epirubicin and cisplatin in patients with inoperable oesophago–gastric adenocarcinoma. Ann Oncol 2002; 13: 1469–78. 7. Jackson DP, Smith D, Topham CA, et al. Fortnightly intravenous irinotecan plus oral capecitabine as treatment for gastroesophageal cancer – a phase 1 and 2 study. Eur J Cancer 2003; 1(Suppl.5): S64 (Abstr 206). 8. Petrovic Z, Tarabar D, Doder R, et al. Oxaliplatin (L–OHP) and capecitabine( X ) as second line chemotherapy in patients with advanced gastric cancer. Proc Am Soc Clin Oncol 2003;22:299 (Abstr 1199). 9. Yeon Hee P, Choi S–J, Ryoo B–Y, Kim H. A prospective phase II study of capecitabine and docetaxel combination chemotherapy in patients with advanced gastric cancer. Proc Am Soc Clin Oncol 2003;22:307 (Abstr 1232). 10. Shin DB, Cho EK, Lee W, et al A phase II trial of epirubicin (E), cisplatin © and capecitabine (X) combination chemotherapy for previously untreated advanced gastric cancer (AGC).. Proc Am Soc Clin Oncol 2003; 22:318 (Abstr 1318). 11. Kang HJ. A phase II study of paclitaxel and capecitabine combination chemotherapy in patients with advanced gastric cancer as a first–line therapy. Proc Am Soc Clin Oncol 2004;23 (Abstr 4051). 12. Kang Y–K, Kim TW, Chang HM, et al. A phase I/II study of docetaxel, capecitabine and cisplatin as a first line chemotherapy for advanced gastric cancer. Proc Am Soc Clin Oncol 2004;23 (Abstr 4066). 13.Kim TW, Kang YK, Ahn JH, et al. Phase II study of capecitabine plus cisplatin as first–line chemotherapy in advanced gastric cancer. Ann Oncol 2002; 13: 1893–8 14. Jin M, Shen L, Hu B. Capecitabine combined with cisplatin in patients with advanced gastric carcinoma (AGC) a Chinese phase II study.. Proc Am Soc Clin Oncol 2003;22:318 (Abstr 1279) . Sumpter K, Harper–Wynne C, Cunningham D, et al. Randomized multicenter phase III study comparing capecitabine with fluorouracil and oxaliplatin with cisplatin in patients with advanced oesophagogastric cancer: confirmation of dose escalation. Proc Am Soc Clin Oncol 2003;22:257 (Abstr 1031).
To date, the best results have been obtained with long-term intravenous administration of high doses of 5-fluorouracil. The main side effects of treatment are mucositis, diarrhea, myelodepression and, with infusion administration, palmar-plantar syndrome, which is characterized by numbness, paresthesia, tingling, swelling, redness, peeling, blistering, desquamation and severe pain; The cardio- and neurotoxic effects of fluoropyrimidines have also been described. The use of daily infusions of 5-FU requires permanent central venous access and is associated with a high risk of complications associated with the installation of a central catheter. This regime disrupts the patient’s usual rhythm of life, as it implies the patient’s stay in the hospital, which, in turn, requires large expenses on the part of the medical staff. The use of 5-FU in bolus mode has one advantage - the possibility of use in an outpatient setting. However, its low efficiency and unpredictable, poorly controlled toxicity, especially in DPD syndrome (unexpectedly severe toxicities in the form of stomatitis, diarrhea, neutropenia and neurotoxicity due to insufficient activity of dihydropyrimidine dehydrogenase, the enzyme responsible for the catabolism of 5-FU), limits its widespread use in clinical practice. The obvious inconvenience of using such regimens and the difficulties of outpatient treatment encourage researchers to search for more effective, safe and easy-to-use forms of fluoropyrimidines. Xeloda (capecitabine) is a good example of the development of a highly effective and safe oral fluoropyrimidine. Xeloda is a non-toxic metabolite that is converted by thymidine phosphorylase (TF) to 5-fluorouracil directly in the tumor (selective activation). TF is one of the enzymes of DNA synthesis in a tumor, identical in structure and function to tumor-associated angiogenesis factor and platelet-derived endothelial growth factor; is highly active in most human solid tumors and directly correlates with rapid tumor growth and aggressive invasion. In addition, TF prevents the apoptosis of cancer cells. It has been proven that overexpression of TF leads to increased angiogenesis and is associated with an unfavorable prognosis in breast cancer, colorectal cancer, gastric, bladder, ovarian, and kidney cancer (Fig. 1). Thus, due to the high expression of TF, the concentration of active 5-fluorouracil in the tumor after taking Xeloda is 127 times higher than its concentration in plasma. At the same time, after the introduction of 5-fluorouracil, these ratios do not change. This explains the high efficiency and relatively low toxicity of Xeloda (Table 1). Oral Xeloda therapy, designed to mimic long-term infusions of 5-FU, offers a number of benefits for both patients and clinicians. The dominant adverse events associated with taking the drug are skin reactions (hand-foot syndrome), reactions from the gastrointestinal tract (nausea, mucositis, diarrhea) and weakness. Cases of myelosuppression occur quite rarely, and manifestations of alopecia are minimal. All types of toxicity can be controlled quite well by modifying drug doses or by temporarily interrupting treatment. A wide spectrum of antitumor activity, low toxic profile, the ability to control adverse events and ease of use make Xeloda an optimal drug for use in outpatient practice. The favorable safety profile opens up prospects for the use of Xeloda in the second and subsequent lines of chemotherapy, for the treatment of elderly patients and debilitated patients. In an experiment with transplantation of human breast and colon cancer cells into mice, it was shown that drugs such as cyclophosphamide, mitomycin C, docetaxel, paclitaxel, and gemcitabine can increase the activity of TF in the tumor. This provided the basis for studying the use of Xeloda in combination with potentially synergistic drugs in various localizations. Radiation therapy has the same effect. Currently, capecitabine is widely used to treat breast and colorectal cancer. The XELOX (Xeloda 1000 mg/m2 2 times a day 1–14 days + oxaliplatin 130 mg/m2 on the 1st day IV, cycle 3 weeks) and XELIRI (irinotecan 200 mg/m2 30–min.) regimens have been shown to be highly effective. IV infusion on day 1 + Xeloda 1000 mg/m2 2 times a day from the evening of day 1 to the morning of day 15, cycle 21 days) in the first line of treatment of metastatic colorectal cancer. The X-AST study has also been completed, according to the results of which Xeloda is recommended for adjuvant therapy of colon cancer. The use of capecitabine for pancreatic, ovarian, and cervical cancer is practiced. Its study has begun in combination with platinum drugs for solid tumors of the head and neck and non-small cell lung cancer. Research is being conducted on its use in patients with disseminated gastric cancer. The range of antitumor drugs active in gastric cancer is quite narrow; the most studied standard of monochemotherapy is 5-fluorouracil, the effectiveness of which in disseminated gastric cancer does not exceed 21%, therefore studies of the effectiveness of Xeloda in this pathology, both in monotherapy and in combination, are quite justified . Analysis of the pharmacokinetics of the drug showed its good absorption in patients who had previously undergone gastrectomy, which allows capecitabine to be successfully used in this category of patients (Table 2). The effectiveness of Xeloda monotherapy ranges from 19–34%. Currently, capecitabine is being actively studied in various combinations, presented in Table 3, as 1st line of treatment. Based on the results of the phase II Korean study of Xeloda in combination with cisplatin [13], the following dosage regimens are recommended: Xeloda 1000 mg/m2x2 r/day. on days 1–14 + cisplatin 60–80 mg/m2 on day 1 (cycle 21 days). Currently, a randomized phase III study has been organized comparing this regimen with the standard regimen: cisplatin 80 mg/m2 on day 1 + 5-FU 800 mg/m2/day x 24 hours on days 1–5. In the studies by Evans [6] and Shin [10], capecitabine was used in the ECF regimen instead of infusional 5-FU. A dose of capecitabine 2000 mg/m2/day, given daily on days 1–14 followed by 1 week of rest along with two other drugs administered intravenously every 3 weeks, was determined to be active and well tolerated. Currently, the phase III REAL2 study is being conducted to compare the effectiveness and tolerability of four combinations: 1) epirubicin 50 mg/m2 daily + cisplatin 60 mg/m2 daily every 3 weeks + 5-FU continuous infusion 200 mg/m2/day; 2) epirubicin 50 mg/m2 every day + oxaliplatin 130 mg/m2 every day every 3 weeks + 5-FU continuous infusion 200 mg/m2/day; 3) epirubicin 50 mg/m2 every day + cisplatin 60 mg/m2 every day every 3 weeks + capecitabine 1000 mg/m2/day. days 1–21; 4) epirubicin 50 mg/m2 per day + oxaliplatin 130 mg/m2 per day every 3 weeks + capecitabine 1000 mg/m2/day. Days 1–21. The planned duration of treatment is 24 weeks. According to preliminary results, the effectiveness of combinations of epirubicin with platinum derivatives and 5-FU was 35%, and with capecitabine – 41% [14]. Currently, the departments of chemotherapy and outpatient methods of diagnosis and treatment of the State Institution Russian Cancer Research Center named after. N.N. Blokhin Russian Academy of Medical Sciences is conducting a study of two chemotherapy regimens, including Xeloda. Regime A – cisplatin 80 IV drips on day 1 + capecitabine 1000 mg/m2 2 times a day from the evening of day 1 to the morning of day 15 of each cycle, cycle – 21 days. Regime B – oxaliplatin 100–120 mg/m2 IV drip on day 1 + capecitabine 1000 mg/m2 2 times a day from the evening of day 1 to the morning of day 15 of each cycle, cycle – 21 days. The study included 74 patients with morphologically verified locally advanced or disseminated gastric cancer. Group A included 31 patients aged 29 to 73 years (median 55.6); 15 men and 16 women. Group B included 16 patients aged 46 to 76 years (median 59.9); 11 men and 5 women. All patients received 2 or more courses of chemotherapy. Total carried out: gr. A – 122 courses, gr. B – 69 courses. In group A, the complete effect was achieved in 3 patients, which was 9.7%, partial regression in 13 patients (41.9%); stabilization in 8 (25.5%). In group B - complete effect in 2 patients (12.5%), partial regression in 5 (31.25%) and stabilization in 8 (50%). The overall effectiveness of the cisplatin + Xeloda regimen was 51.6%, and the oxaliplatin + Xeloda regimen was 43.75%. Median survival has not been reached. Preliminary data indicate that two-component regimens are well tolerated (the severity of side effects generally does not exceed grade 1–2), which ensures safety and the possibility of long-term treatment in an outpatient setting. Many patients do not lose their usual activity and even continue their professional activities. The main types of toxicity were: leukopenia 3 tbsp. (in group A – 2 courses – 1.6%, in group B – 0); grade 3 granulocytopenia (group A – 4 courses – 3.3%, group B – 0), 4 tbsp. (group A – 1st course – 0.8%); hand-foot syndrome stage 3 was noted in one case in gr. A, treatment for this patient was stopped; anemia 3 degrees was observed over 7 courses in gr. A (5.7%). However, it should be taken into account that the study included patients with initially low hemoglobin levels, requiring intensive symptomatic therapy before the start of chemotherapy (use of iron supplements, erythropoietins, red blood cell transfusion). In such patients, in parallel with the implementation of the effect of specific treatment, the level of hemoglobin reached normal levels. Preliminary analysis indicates the effectiveness of two platinum-containing regimens, including capecitabine, but the oxaliplatin + Xeloda regimen is better tolerated. Capecitabine is being actively studied in other gastrointestinal malignancies. Modern treatment regimens for disseminated pancreatic cancer (in particular, the use of gemcitabine and high doses of 5-FU) have led to an increase in the objective effect, control of symptoms and an extension of the median survival of patients. Therefore, studies where 5-FU was replaced by capecitabine were logical. Xeloda 1250 mg/m2 2 times a day on days 1–14 in mono mode showed an objective effect in 10% of cases, stabilization in 40%, with a median survival of 6 months. The use of Xeloda 650–1000 mg/m2 2 times a day, days 1–21, in combination with weekly administration of gemcitabine 1000 mg/m2 was effective in 14–33% with stabilization in 35–58%. Median time to progression is 6 months, median survival is 8–10 months. Attempts are currently being made to study three-component combinations. Thus, Xeloda 1000–1500 mg/m2 2 times a day, days 1–14, in combination with gemcitabine 750 mg/m2 (days 4 and 11) and docetaxel 30 mg/m2 (days 4 and 11) showed an objective effect of 47 %, stabilization in 31% (n = 44). Xeloda 650 mg/m2 2 times a day (days 1–14) in combination with gemcitabine 800 mg/m2 (days 1 and cisplatin 60 mg/m2 (on day 1) showed an objective effect in 30% of cases, stabilization in 35%. Median time to progression - 5.1 months, median survival - 7.5 months (n = 40). The use of synergy between capecitabine and radiation therapy led to an increase in survival to 11-14 months, with one-year survival of 69% of patients Of interest are studies of the effectiveness of Xeloda in biliary tract cancer.At a dose of 650 mg/m2 2 times a day (days 1–14, cycle 21 days) in combination with gemcitabine 1000 mg/m2 (on days 1 and 8), the objective effect was 26 %, stabilization – 12%, time to progression – 6.8 months, survival – 10.3 months (n = 35) Xeloda 1000 mg/m2 2 times a day (days 1–14) with mitomycin C, 8 mg/m2 (on day 1), achieved an objective effect of 31–33%, stabilization in 13–34%, time to progression of 5.3–6.3 months, with overall survival of 9.3 months and one year survival rate 41–70% (n = 64). The research results give hope for improved results of treatment of cholangiocellular cancer compared to 1978–1989, when 20 to 29% of patients survived one year. Xeloda is also being studied for tumors of the female genital area. In particular, for ovarian cancer, in the second and subsequent lines of treatment, at a dose of 1250 mg/m2 2 times a day for 3 weeks, an objective effect was achieved - 10-19%, stabilization - 21-49%, median time to progression – 3–4 months with overall survival – 8 months. When using Xeloda 600 mg/m2 2 times a day on days 1–14 and gemcitabine 1000 mg/m2 on days 1 and 8, the objective effect is 60%, stabilization is 20%, the median time to progression is 3 months. Research on the use of Xeloda in cervical cancer is also important. Since at the moment the main methods of treating this pathology are surgery and radiation, the use of chemotherapy as a sensitizer for radiation therapy has good prospects. Currently, the standard treatment in combination with radiation therapy is cisplatin. However, everyone knows its severe side effects, in particular, nephrotoxicity and myelosuppression, which significantly limits the use of cytostatics in patients with medical history and in elderly patients. In combined treatment of patients with stage 2B–3B, using Xeloda at a dose of 825 mg/m2 2 times a day, 5 days a week, weekly, and radiation therapy 1.8 Gy per day, an objective effect was obtained in 87% of patients, median time before progression was 7.5 months. In patients who had previously received treatment, Xeloda at a dose of 1250 mg/m2 2 times a day every 3 weeks showed an objective effect in 13–17% of cases, stabilization in 42–53% of cases, with a median overall survival of 9.3 months. Xeloda (1000 mg/m2 2 times a day on days 1–14) in combination with cisplatin (50 mg/m2 1 time every 3 weeks) showed an objective effect of 57%, stabilization in 21%, with a median time to progression of 14 months . Xeloda's high selective efficacy, low toxic profile, and ease of use will allow it to occupy a leading position in modern chemotherapy for malignant neoplasms. References 1. Kondo K, Chin K, Sakamoto J, et al. Modified capecitabine regimen for advanced/metastatic gastric cancer: final results from multicenter phase II trial. Eur J Cancer 2003; 1(suppl.5):S69 (Abstr 221). 2. Koizumi W, Saigenji K, Ujiie S, et al. A pilot phase II study of capecitabine in advanced or recurrent gastric cancer. Oncology 2003; 64:232–6. 3. Hong YS, Song SY, Lee SI et al. A phase II trial of capecitabine in previously untreated patients with advanced or metastatic gastric cancer. Ann Oncol 2004; 15:1344–7. 4 Leon-Rodriguez E, Green D, Candelaria M, et al. Oral capecitabine in treatment of patients with advanced or metastatic gastric carcinoma. Ann Oncol 2002; 13(Suppl.5): 191 (Abstr 708P). 5 Kim TW, Kang YK, Ahn JH, et al. Phase II study of capecitabine plus cisplatin as first–line chemotherapy in advanced gastric cancer. Ann Oncol 2002; 13:1893–8. 6.Evans TR, Pentheroudakis G, Paul, et al. A phase I and pharmacokinetics study of capecitabine in combination with epirubicin and cisplatin in patients with inoperable oesophago–gastric adenocarcinoma. Ann Oncol 2002; 13: 1469–78. 7. Jackson DP, Smith D, Topham CA, et al. Fortnightly intravenous irinotecan plus oral capecitabine as treatment for gastroesophageal cancer – a phase 1 and 2 study. Eur J Cancer 2003; 1(Suppl.5): S64 (Abstr 206). 8. Petrovic Z, Tarabar D, Doder R, et al. Oxaliplatin (L–OHP) and capecitabine( X ) as second line chemotherapy in patients with advanced gastric cancer. Proc Am Soc Clin Oncol 2003;22:299 (Abstr 1199). 9. Yeon Hee P, Choi S–J, Ryoo B–Y, Kim H. A prospective phase II study of capecitabine and docetaxel combination chemotherapy in patients with advanced gastric cancer. Proc Am Soc Clin Oncol 2003;22:307 (Abstr 1232). 10. Shin DB, Cho EK, Lee W, et al A phase II trial of epirubicin (E), cisplatin © and capecitabine (X) combination chemotherapy for previously untreated advanced gastric cancer (AGC).. Proc Am Soc Clin Oncol 2003; 22:318 (Abstr 1318). 11. Kang HJ. A phase II study of paclitaxel and capecitabine combination chemotherapy in patients with advanced gastric cancer as a first–line therapy. Proc Am Soc Clin Oncol 2004;23 (Abstr 4051). 12. Kang Y–K, Kim TW, Chang HM, et al. A phase I/II study of docetaxel, capecitabine and cisplatin as a first line chemotherapy for advanced gastric cancer. Proc Am Soc Clin Oncol 2004;23 (Abstr 4066). 13.Kim TW, Kang YK, Ahn JH, et al. Phase II study of capecitabine plus cisplatin as first–line chemotherapy in advanced gastric cancer. Ann Oncol 2002; 13: 1893–8 14. Jin M, Shen L, Hu B. Capecitabine combined with cisplatin in patients with advanced gastric carcinoma (AGC) a Chinese phase II study.. Proc Am Soc Clin Oncol 2003;22:318 (Abstr 1279) . Sumpter K, Harper–Wynne C, Cunningham D, et al. Randomized multicenter phase III study comparing capecitabine with fluorouracil and oxaliplatin with cisplatin in patients with advanced oesophagogastric cancer: confirmation of dose escalation. Proc Am Soc Clin Oncol 2003;22:257 (Abstr 1031).
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Methods
The CREATE-X UMIN trial enrolled 910 patients with HER2-negative residual breast cancer following neoadjuvant chemotherapy (anthracycline, taxane, or both).
Patients received standard postsurgical treatment with or without capecitabine.
The primary efficacy endpoint was tumor-free survival and the secondary endpoint was overall survival.
Patient reviews
Free consultation
Information is published with the consent of patients. The names of the patients have been changed.
International treatment protocol - Scope of surgery!
Zarema, 53 years old, Bashkortostan
2 years ago I was diagnosed with stage 2 ovarian cancer, tumor aggressiveness G2. The chances of recovery are therefore good. All examinations in Ufa were done quickly, surgery was performed and chemotherapy was prescribed. But already six months after chemotherapy, a relapse began. I was told that this happens. They started giving me different chemicals. My husband found information that you can get a consultation in absentia in Germany and receive a chemotherapy regimen. We sent all the documents and it was clear from the operation protocol that the scope of the operation was incomplete. My lymph nodes and other tissues were not cut out. It turns out that the treatment protocol includes not only the correct chemotherapy regimen, but also the scope of the operation! Only if the operation was completed in full can we talk about the chances of recovery. Therefore, the first thing that the chief doctor of the German clinic recommended to me was to remove the remains of the tumor, and then carry out a course of chemotherapy. The chief doctor himself also prescribed the regimen. They refused to do an operation of this magnitude in Russia; they said there was no need. I read on the Internet that operations of this magnitude cannot be performed in Russia due to poor funding and lack of specialists. Such operations take longer, surgeons must have appropriate experience, the risk of complications is high and patients stay in the hospital longer, so they perform smaller operations. I decided to have the operation in Germany and take the chemotherapy drugs with me. I will not save on the operation, I really hope that the situation can still be corrected.
Consultation on histology
Anna, 35 years old, Leningrad region.
In September, I was diagnosed with breast cancer and underwent surgery in a hospital in St. Petersburg. Histology, of course, was done on site. With such a serious diagnosis, I want to believe that everything was done correctly and the treatment prescribed was effective. I would not have been able to pay for the operation in Germany, but I decided to learn more about treatment and consultations from a German doctor in a large public hospital. A public hospital is cheaper than private clinics and has world-famous specialists. I don't want to overpay. I found the opportunity to send blocks for repeat histology through Interbasis. Moreover, I received not only reliable research results, but also a consultation with an oncologist. The head doctor of the clinic himself gave recommendations for treatment and prescribed a chemotherapy regimen. It all took a little time, I had all the conclusions within 12 days. The main thing is that I managed to get a consultation before my appointment with an oncologist at our oncology center. This played a big role in prescribing treatment and gave me confidence that the therapy would produce results. Interbasis also assured me that if I have any questions or need to monitor my treatment, I can always contact my doctor for help. Thank you very much!
November 2017
Suspicion of cancer.
Ildar, 52 years old, Kazan
In Russia they could not give me an accurate diagnosis using PET CT, but there was no doubt that it was cancer. I was told that the tumor in the liver could be both a metastasis and a primary tumor, so other examinations were necessary. They would take weeks, and then I would have to look for a specialist who could perform this operation on me. I was given the date for the start of examinations and surgery in Germany for the next week. Within a week I prepared my departure and received a visa. All examinations took 2 days. The professor performed the operation, urgent histology did not show cancer. A week later I was already at home. I consider myself a happy person. I fully realized it at the airport when I was met by my wife and children. The clinic refunded me a large amount because it turned out to be not oncology. I am very grateful to my friend, who treated my mother in Germany, for convincing me to come, and to the company’s professionalism and sensitivity.
August 2017
Oncology. Correspondence consultation with an oncologist
Elena, 45 years old, Moscow
Let me tell you right away that I was asked to write this review. Instead of describing the history of the disease in detail, I decided to write what I went through and what the consultation gave me. Let me just say that we are talking about oncology. We have no problems with diagnostics and consultations with an oncologist. Difficulties arise when you need to undergo treatment in a hospital. As a rule, the necessary medications are not immediately available. To receive them you need to fill out a form and wait. Sometimes you have to wait a very long time. If you look for a solution to the problem on the Internet, there are many forums where they really advise where to go with a complaint, what can be done if you have to wait a very long time for medicines. But we must not forget that while a person with cancer seeks the truth, time passes. It costs him his life. I'm not even talking about the fact that doubts arise about the diagnosis and that I will be treated correctly, because while searching for information on the Internet, you come across stories of patients who were given an erroneous diagnosis. In this case, there can be no talk of any treatment; the patient simply takes the prescribed medications, and the disease progresses. Doubts arise about the attending physician. I saw a solution to this problem in searching for a doctor at a private clinic, hoping that the qualifications of doctors there should be higher. Again, to find a trustworthy clinic, you need to read a ton of information and reviews. The quality of service in a private clinic is, of course, better, but it all comes down to trust, which gradually disappears during consultations. In fact, public and private clinics differ only in equipment and attitude towards you, but the qualifications of doctors are the same. Treatment with the necessary medications can be started immediately in the clinic. Prices, however, as well as doctors' recommendations and prescribed medications, can vary greatly. Once again, you are faced with a choice that you simply cannot make, because you cannot judge the correctness of the treatment, much less whether the medications are counterfeit. By luck, I was given the opportunity to contact a German oncologist. Here, the very fact that this is a professor from Germany outweighs all doubts about the correctness of the decision. The correspondence consultation gave me clarity and a clear action plan. Nobody persuaded me to undergo treatment or examinations in Germany, i.e. they definitely didn’t make much money from me. The consultation itself cost 265 euros + 100 went for translations. And I decided to order the medicines myself in Germany. If I was waiting in line for a hospital, I would not be writing a review now. Now I am doing diagnostics at my own place, but I am getting advice from a German professor. There are probably good doctors in Russia, but the system itself is destructive. Since then I have recommended consultation to all my friends. One converted, all the rest, about 10 people, are already in the next world.
September 2016
Oncology. Medicines.
Samara
My wife has breast cancer. We undergo treatment with Herceptin and Capecitabine at home, but it turned out that Kadcyla is more effective, so this is the third time I’ve come to Germany for medicines. I buy Kadcyla and painkillers, and have learned a lot during this time. We found out where to buy Kadcyla and how much it costs. It turns out that medicines from Germany are always only in German, and not in English, like many “pharmacies” on the Internet. Prices are different for everyone, but in Germany the price is always the same. In any case, ordering on the Internet is more expensive and without a guarantee that it is not counterfeit. You can fly in and buy it locally, it’s cheaper and most importantly reliable. I am bringing medicines for my wife with accompanying documents and receive Tax Free.
August 2016
Oncology. Prostate cancer.
Patient, 67 years old, Irkutsk
My grandfather was diagnosed with stage 4 prostate cancer without metastases T4n0m0. I was very scared by the degree. They removed the testicles and did histology, there were no cancer cells. The oncologist prescribed him 20 radiation therapy sessions. Of course, we looked for information on the Internet, advice on forums. One can only say that they got confused and lost confidence in doctors. Therefore, we decided to get a paid consultation with an oncologist in Moscow. He prescribed chemotherapy. We were very confused by this, we started looking for help on forums where doctors give answers. Opinions there were also divided, and time passed. Then we found the opportunity to take a correspondence consultation with a German oncologist professor. It turned out to be easier than we thought. We received an answer quickly, from two specialists at once - an oncologist and a radiotherapist. We even decided to come for treatment; it turned out that we could handle it financially. They even gave a good prognosis. We had to do this right away, not waste time and not sit on forums, which only increased fears and uncertainty. Thank you for the fast and competent help and organization!
Patient, 67 years old, August 2016
Patient, 57 years old, St. Petersburg
Oncology. Stomach cancer.
I consider myself very lucky. I was diagnosed with stomach cancer in a St. Petersburg clinic. The stage, however, was not determined. A doctor once operated on my father for the same diagnosis, who died six months later. Of course, I have a predisposition to the disease. Well, a certain way of life, like everyone else... Friends advised me to go for a consultation with an oncologist professor in Germany. We decided that treatment was expensive, but it made sense to go for a consultation. After talking with the professor, I underwent additional examinations. It became clear that we had to hurry. Friends and relatives collected money for the operation. I really didn’t want to have surgery in the same place as my father. The oncologist surgeon showed and explained in great detail how the operation would take place. The operation was successful and after 5 days I was already walking. After that there was chemistry, I took 1 course in Germany, the rest - at home with German medicines. This is the fourth year that I have been flying to the clinic for examination.
I am very grateful to the professor and doctors that I can enjoy life and raise my grandchildren.
Evgeniy, 57 years old, St. Petersburg, July 2016
Patient, 52 years old, Perm
Oncology. Thyroid cancer
I am very grateful to the professor and all the medical staff of the clinic. I never thought that an attitude could be so sincere. My daughter helped me come here; it was she who convinced me not to do this at home. At first I didn’t know what to do at all. I still wanted to save money. Now I understand that they don’t save money on this. Until you walk this path yourself, it’s difficult to understand. Thyroid cancer is easily detected at an early stage. There was no need to wait, an operation was immediately scheduled and the operation was performed the next day. After the operation, I stayed in the clinic for only 3 days. There was no need to do chemistry. We immediately flew home. Every six months I fly to my professor for examination. Just blood and an ultrasound, but it’s important to me that he does it. How everything was on time! Thank you!
Ekaterina, 52 years old, Perm, August 2016
Patient, 63 years old, Saratov
Oncology. Oncologist consultation
Unfortunately, I arrived too late. Since September I had severe pain in the stomach area that radiated to my back. I went through many examinations in my city and went to other clinics in Moscow. Nothing significant was found, only suspicion of various diseases. A professor in a German clinic, after undergoing an MRI and biopsy, identified a stage 3 pancreatic tumor. It was too late for the operation, even with the CyberKnife system. Now I am on palliative treatment (chemotherapy with gemcitabine and pain relief with morphine) and I very much regret that I did not come earlier.
Thank you for organizing the visit and the professor.
Nadezhda, Saratov, March 2021.
Patient, 52 years old, Chelyabinsk
Orthopedics. Spine surgery.
I am 52 years old and have had back pain for 12 years. In the last year the pain has become very intense, especially in the sacral area. Physiotherapy and pain relief did not help. I had spinal surgery in country X. We went there to see a Russian-speaking doctor because we didn’t need to apply for a visa. Surgery under general anesthesia, decompression laminectomy with fixation with cages. It seems to be a simple operation that is performed everywhere, even here in Russia. Of course, they were right after the operation, so I went through rehabilitation, first in the same clinic, then with us. Six months later, the pain not only did not go away, but even intensified and began to radiate to my legs. I turned to a German neurosurgeon for a correspondence consultation. I sent the clinic disks with MRI and X-rays and a description of the history, as the doctor asked. His conclusion shocked me. From the photographs, he concluded that the screws were already positioned incorrectly during the operation! I was operated on by a German professor orthopedic neurosurgeon. This is a surgeon from God! My deepest bow! I immediately felt much better, although it is clear that it will take time to recover. Now I am undergoing rehabilitation in a specialized center, here in Germany. It was very difficult for me to decide on this. Thank you very much for the organization, help and support!
Olga S, Chelyabinsk. June, 2016
Patient, 26 years old, Kirov
ENT. Correspondence consultation. Surgery to remove sinus adenoma
Six months ago, I was diagnosed with a paranasal sinus adenoma, which grew quite quickly. On the Internet I found a lot of information and suggestions for tumor removal. The price range was wide, and all clinics, of course, promised quality. On the advice of friends, I turned to a German clinic to find out the professor’s opinion in absentia and to make sure that they did not want to operate on me just like that. The diagnosis of cancer was confirmed and I, in principle, could choose a clinic here, they even recommended a good one. But, judging by the way they answered all my questions at the German clinic, what they offered, what results were guaranteed, I already had a good impression of her and the professor. Whatever the operation, complex or routine for the doctor, the patient has to pay for mistakes and failures. The decision to come to Germany was made quickly, but the operation was possible in the same week, so I did not lose time. The operation was successful and I was very pleased with the result! The main thing is that I did not regret the decision, as often happens when everything goes well and you think that everything would have gone just as well in our clinic. The result was worth all the extra expenses and the flight. I think that trust in the doctor and confidence in the result influenced the decision.
Anton, 26 years old, Kirov, July 2016
Patient, 40 years old, Togliatti
Oncology. Head and neck tumors
In January 2015, I was diagnosed with lower lip cancer. At the regional oncology center, all the examinations were carried out on me, and with very good equipment. Chemotherapy and radiation therapy were prescribed. I received all examinations, chemical preparations, radiation, and consultations free of charge. There was no such thing as an attending physician; you constantly come to see another doctor who looks at your medical history and prescribes treatment. The treatment did not produce results and it was not possible to talk about it with one doctor or ask questions. There was a feeling that no one was responsible for the treatment and its results. I began to have doubts not only about the correctness of the prescribed treatment, but also about the authenticity of the chemical preparations. I decided to go to a German clinic. Prices in private clinics in Moscow were not much lower, and I had more confidence in German doctors. A consultation was scheduled and I was seen by a surgeon-oncologist, a chemotherapist and a radiotherapist. Then treatment was already prescribed - chemotherapy and immunotherapy. My attending physician was a professor of oncology, to whom I could always turn with questions. I completed part of the therapy at the clinic. The control CT scan showed improvements and I could continue treatment at home. I bought all the drugs in Germany with a prescription, there were no problems at customs, although I had strong painkillers. Our doctors gave me several months, but I am still able to fly to a consultation with the professor.
Igor, Samara region, June 2016
Patient, 32 years old, Yekaterinburg
Rheumatology. Rheumatoid arthritis
I was diagnosed with rheumatoid arthritis at the age of 31. I have two small children and elderly parents. It would be possible to rely only on the husband if it were a question of material resources and raising children. But, of course, he cannot restore my health. The kids don't even go to school yet! The diagnosis was made by a rheumatologist at the clinic, and she prescribed medications and prescribed treatment. The pain only intensified. I spent a lot of time on forums and read specialized literature. At some point, I realized that the disease was so complex that an ordinary doctor at the clinic, although decent and conscientious, was unlikely to be able to help me. After going through the ordeal of our doctors, we decided to turn to German specialists. When I saw what tests were actually needed to make an accurate diagnosis and prescribe treatment that would actually bring something, I was horrified. They didn't even do half of this for me! There are various methods, medications, diets, but I was prescribed 2 medications and sent for exercise therapy. I decided that I would undergo all the examinations in Germany at a clinic that specializes in such diseases. They took me so seriously! It turned out that the disease is constantly being studied, so it is best to be treated at a university clinic or one affiliated with it. I immediately gained confidence in the doctors and staff of the clinic and really believed that they would help me. The examinations went quickly, we only had to wait for the laboratory results, they are very special. They prescribed me treatment, selected a diet and medications. The whole time in the clinic I didn’t even think about the fact that I had a serious illness. I felt much better and was confident that I was in good hands. 3 weeks in the clinic gave me not only the correct diagnosis and appropriate treatment, but also the opportunity to lead a normal life and enjoy my children!
Elena, 32 years old, Ekaterinburg, April 2016
Patient, 19 years old, Moscow. region
Neurology. Misdiagnosis
Last year, six months after entering the university and starting my studies, I started having very severe headaches and dizziness. There was even a loss of coordination and nausea. I had headaches day and night; painkillers didn’t help at all. A doctor at a Moscow clinic sent me for an MRI and I was immediately diagnosed with epilepsy and offered hormonal therapy. The whole family was very worried, my parents could not find a place for themselves. No one in our family had such diseases and we decided to seek a second opinion from a German epileptologist based on the images. One opinion is good, but two are better! I would be ready to undergo all the necessary examinations if the diagnosis was in question. A professor at the university clinic looked at my pictures and suggested that I undergo a full diagnosis as an inpatient, because the examination carried out at home was such that it did not provide grounds for making such a serious diagnosis. Don't get me wrong, I don't want to be inappropriate towards our doctors. I understand that there are so many people, so many cases, but mine just turned out to be unsuccessful. Therefore, I will be honest, the MRI diagnosis was done poorly. I flew to Germany on a Schengen tourist visa. I was very worried! At the clinic, in addition to MRI, I was given other examinations - EEG, ECG, ultrasound of cerebral vessels, special blood tests. The diagnosis was not confirmed!!! Headaches arose from overwork and prolonged stress. I didn't even imagine that this could happen. Hormonal therapy, especially the operation that was offered to me here in Moscow, was out of the question. I was prescribed medications and given recommendations on how to prevent headaches and vascular problems. All examinations and consultations with the professor took 2 days. Thanks to the entire team of doctors and company employees! I would like to express special gratitude to my curator-translator, I hoped that I would feel free with my English, but still I needed German.
Andrey, Moscow region, December 2015
Patient, 35 years old, Pavlovsk
Oncologist consultation. Mammary cancer
For 2 years, I periodically experienced pain and a pulling feeling in my chest. In 2014, I was diagnosed with stage 1 breast cancer. In St. Petersburg, this diagnosis was confirmed. The conversation was about surgery and further chemotherapy. We didn't know where to turn. After contacting a professor oncologist in Germany, after the initial examination, the diagnosis was removed. During the examination, a 3D biopsy was performed and a week later I received a discharge with a diagnosis of fibroadenoma, which did not require either medication or surgical treatment. What would have happened if surgery and chemotherapy had been performed... Thank you for the quick and efficient organization. After 3 days from the moment of treatment, I had a consultation at the clinic, at the Breast Treatment Center. Finally managed to make a reliable diagnosis! I was very impressed with the clinic itself! The attitude towards patients is amazing. These are professionals!
Valentina S, Leningrad region. February, 2015
Patient, 11 years old, Moscow
Neurology. Suspicion of a neoplasm
After school, my son started having severe headaches on the right side and signs of paralysis. After contacting a neurologist at the place of residence, an MRI was performed and a tumor was discovered in the right lobe of the brain. We contacted several clinics. Doctors could not tell whether it was benign or malignant and suggested opening the skull for a biopsy. They could not give a guarantee that after the diagnosis everything would be fine and the child would continue to develop normally. Within 1 day we received an offer of examination and an invitation from a German clinic and after 2 days we were already in Germany. At the clinic, events developed as follows. First there was a conversation with the professor, which lasted 3 hours. A detailed history was written and an examination plan was prescribed. Already during the consultation, the professor noted that the existing symptoms and the tumor cannot be related to each other, since with a tumor in the right lobe of the brain, paralysis will occur on the left side. An MRI, a special blood test, an EEG, and an ECG were performed. During all examinations and consultations, we had a medical translator-curator with us. After 3 days, the results of all examinations were ready and a final conversation with the professor took place. The resulting headaches and paralysis were explained by a family history of migraine and a blood clotting disorder. The professor gave recommendations and prescribed therapy that we could carry out at home. The neoplasm was a deposit of calcium salts in the brain, which, after treatment, would go away over time. We received prescriptions for medications, which we immediately bought in Germany. We would like to note that we ordered medications several times from Germany, since we have a connection with our curator and professor, this is always possible. We consider ourselves very lucky and our child was saved from wrong actions. It’s even scary to imagine what the outcome could be.
With gratitude, Irina K., Moscow. March, 2016
Patient, 40 years old, Ufa
Oncology. Breast cancer
In Russia I was diagnosed with breast cancer, stage 3, +++, treatment lasted more than a year, but did not bring results. In total, I underwent 12 courses of chemotherapy and radiotherapy, but I only got worse. A friend told me that you can get a paid consultation with a German oncologist. Before that, I found out everywhere where cancer is best treated. I decided to come to the German clinic after all. After an examination at the clinic, this diagnosis was not confirmed; it turned out that I had a different type of cancer. The histology done in Russia turned out to be erroneous. After that, there was no longer any trust in our medicine. Another treatment was prescribed. I felt better after a few days. Separately, I would like to talk about the doctors and the clinic. The professor himself and all the doctors at the clinic amaze with their sensitive attitude towards the patient and always listen carefully. They constantly monitor the patient’s condition and do not abandon him. You can feel the dynamics. This helps to cope with fears and undergo treatment with optimism. The nurses on the ward are kindness itself, they are always very responsive and come to the rescue in any situation. The clinic itself made a very big impression on me - clean, spacious, everyone is attentive and smiling. Since I was not only receiving counseling, but also undergoing chemotherapy, nutrition was especially important to me. It's really very good. All the medications prescribed to me were ordered and, which is very important, always on time, because we did the last chemo in Ufa. Our family decided that we would fly for diagnostics and a consultation with the professor, and to take medications with us.
Very quickly they set a date for the initial appointment with the professor and sent an invitation. We were given the first visa for 2 weeks, we got it very quickly. When we were in Germany, it turned out that the visa needed to be extended. The company did this for us within 1 day, we received a visa for several months.
Our financial situation is quite difficult, so we are forced to turn to funds. To do this, you need correctly executed invoices and other medical documents - epicrises, prescriptions. I never tire of saying thank you; not only I, but the whole family feel gratitude.
Alina, Ufa, May 2016
Patient, 45 years old, Moscow
Orthopedic rehabilitation
In July 2015, I had an accident, which resulted in a pelvic fracture, a comminuted fracture of the femur and a fracture of the 3rd-4th metatarsals. The operations had to be carried out here. There was no choice, since the condition was serious. Fortunately, the operation was successful. An acquaintance underwent rehabilitation in Germany and recommended a rehabilitation center, where they helped him quickly get back on his feet after spinal surgery. It was important to start rehabilitation on time, because if it is done too early or too late, the consequences can be fatal. From the time we sent the request and documents until the invitation from the center, 3 days passed. German doctors, after looking at the pictures and documents on treatment, set a date for arrival. So that I had time to recover and arrive at the center at the appointed time. The rehabilitation program impressed me right away. I used all the opportunities and time that I was in the clinic. In a short time, purposefully, they really put me on my feet and helped me avoid serious consequences. Moreover, they did not force me to undergo long-term rehabilitation and tried to achieve the maximum result as quickly as possible. I could undergo further treatment on an outpatient basis at my place. I was advised to maintain contact with the center’s doctors if questions arise. I really liked this because this way I could control what was offered here.
Victor, 45 years old, Moscow, January 2016
Patient, 38 years old, Nizhny Novgorod
Oncology. Surgical treatment of rectal cancer
In September in Russia I was diagnosed with rectal cancer. Since a friend of mine successfully underwent a similar operation in Germany several years ago, I did not waste time and immediately turned, on his advice, to a professor of oncology surgery. The diagnostics carried out in Russia were recognized; of the additional examinations, only an MRI of the liver was required, which was performed before the operation. The appointment date was set immediately, I didn’t need a visa, and 2 days later I was at the oncology clinic... The operation was successful, there were no complications. The professor examined me every day and controlled everything. I was amazed that the professor was at the department every day like an ordinary doctor, even on weekends! Since I did not hesitate and the surgery was done in a timely manner, I did not require further treatment such as chemotherapy or radiation. Already on the third day after the operation I could walk! and on the 7th day I was discharged. To say that the professor is impressive is to say nothing. The clinic staff is responsive and at the same time very tactful. The food for me was selected by a doctor. They took into account not only my underlying disease, but also all the characteristics of my body. All medications, even for other diseases, were included in the treatment. After discharge, the opportunity to contact the professor was very important for me, because I immediately returned to Russia. I couldn’t leave my business and family for a long time. Six weeks later I flew back for a follow-up examination and consultation, which took 2 days. Thank you very much to the doctors and organizers!!!
Sergey B., Nizhny Novgorod, December 2014
Patient, 23 years old, Kazan
Oncology. Breast cancer.
I didn’t think I could be diagnosed with cancer at 22 years old. The diagnosis of stage 1 breast cancer HER2- was confirmed in 2 clinics (in Moscow and St. Petersburg). It was difficult to decide which clinic to perform the operation in, because all the doctors were recommended to me by friends and acquaintances, and I needed to act quickly. What was important to me was not the doctors’ forecasts and promises, but the results, and, of course, the quality of treatment. Therefore, I turned to a German specialized center for the treatment of breast cancer at a university clinic and did not regret a single minute. Here in Kazan I was offered surgery and three chemotherapy treatments to choose from. This immediately struck me as very strange! As I was told in Germany, chemistry is prescribed according to medical indications - type, stage, and not at the patient’s choice, and this is done by the professor himself. The entire organization of the arrival took only 2 days. After being examined at the clinic, the next day the professor operated on me. The entire team of doctors and medical staff gave me great moral support. And the organizers of my arrival made sure that I felt at home; more comfortable conditions are difficult to imagine. After the operation, I had drainage for several days and had to wear special underwear, which was ordered for me by prescription along with the necessary medications, immediately to take with me to Kazan. A timely operation saved me from chemotherapy, not to mention it simply saved my life. I only took hormonal medications. Thank you very much from me and my entire family!
Aliya, Kazan, August 2015
- Organization of treatment in a German clinic
- Getting advice from a German doctor
- Making a request to the clinic
- Organization of stay in a German clinic
Free consultation
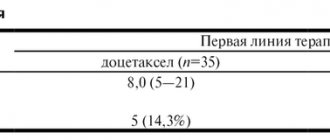
results
- The analysis demonstrated that the disease-free period was longer in the capecitabine group compared with the control group (74.1% vs. 67.6% of patients had no tumor recurrence or metastases over five years of follow-up; hazard ratio, 0.70; 95% confidence interval [CI ], 0.53 to 0.92; P=0.01).
- Overall survival was higher in the capecitabine group compared with the control group (89.2% vs. 83.6% of patients were alive at 5 years; hazard ratio for death, 0.59; 95% CI, 0.39 to 0.90; P=0.01).
- Among patients with a triple-negative tumor (absence of estrogen receptors and progesterone receptors and insensitivity to Herceptin), the frequency of a free period without a tumor was 69.8% in the study group and 56.1% in the control group (hazard ratio, 0.58; 95% CI, 0.39-0.87) , overall survival was 78.8% vs. 70.3% (hazard ratio, 0.52; 95% CI, 0.30–0.90).
- Palmar-plantar erythrodysesthesia, which is the most common side effect of capecitabine, was recorded in 73.4% of patients in the main group.
This report is based on the proceedings of the 2006 ASCO conference, which presented recent data on the role of capecitabine (Xeloda®) in the chemotherapy of a number of malignant tumors. The drug was developed and registered in Russia by F. Hoffmann–La Roche Ltd., Switzerland.
The unique mechanism of the antitumor effect of capecitabine is due primarily to the intratumoral activation of this drug, which, in addition to the pronounced therapeutic effect, determines its low systemic toxicity. Of the characteristic adverse reactions of capecitabine, the most common are hand-foot syndrome and diarrhea.
The basic chemotherapy drugs for most malignant tumors of the digestive tract are platinum drugs and fluorouracil derivatives. A study by Cunningham D. et al was devoted to determining the most optimal treatment combinations for cancer of the esophagus and stomach. In the 1st line of treatment, 1002 patients received one of a three-component regimen, including epirubicin 50 mg/m2 (E), cisplatin 60 mg/m2 (C) or oxaliplatin 130 mg/m2 (O) every three weeks and fluorouracil 200 mg/m2 (F) or capecitabine 1250 mg/m2 (X) daily; only eight cycles. The main purpose of the study is to assess survival. There were no significant differences between the regimens in the frequency of achieving a therapeutic effect (41–48%) and the development of grade III–IV non-hematological toxicity (33–45%). Grade III–IV neutropenia more often complicated treatment with cisplatin and fluorouracil, less often with oxaliplatin and capecitabine: ECF – 42%, EOF – 30% (p = 0.008), ECX – 51% (p = 0.043) and EOX – 28% (p = 0.001) respectively. The median one-year (40–47%) and overall survival (10–11 months) in the case of using these regimens did not differ significantly. The results obtained served as the basis for the conclusion that capecitabine is at least an adequate alternative to fluorouracil, and oxaliplatin to cisplatin [1].
These data were confirmed by the results of a study by Kang Y. et al. In advanced gastric cancer, capecitabine and cisplatin in the 1st line of therapy can adequately replace standard treatment with fluorouracil and cisplatin. An analysis of the treatment results of 316 patients (including data from our clinic) confirmed that the rate of achieving an objective effect was significantly higher in patients receiving capecitabine: 41 versus 29% (p = 0.03). At the same time, the median time to progression (5.6 and 5 months) and overall survival (10.5 and 9.3 months) were almost the same. Grade III–IV side effects occurred with comparable frequency in both groups: neutropenia – 16 and 19%; vomiting – 7 and 9%, stomatitis – 2 and 7%, diarrhea 5 and 5%, anemia – 5 and 3%, respectively. Thus, with similar rates of side effects and survival, treatment with capecitabine more often induced an objective effect, significantly reducing the need for hospitalization [2].
High therapeutic results in the 1st line of treatment for gastric cancer were achieved with the use of capecitabine at a dose of 2000 mg/m2/day from days 1 to 14 and cisplatin at a dose of 20 mg/m2 from days 1 to 5 each three-week cycle; only six courses. In 141 evaluated patients with gastric cancer, an objective effect was achieved in 36% of cases (13 complete and 38 partial regressions). The median time to progression was 9 months, overall survival was 12. Grade III side effects occurred in less than 5% of cases. Despite certain difficulties in the daily use of cisplatin, the minimal toxicity and high effectiveness of the regimen should attract the closest attention of practicing physicians [3].
In the 1st line of treatment, 54 patients with advanced gastric cancer received chemotherapy with capecitabine at a dose of 2000 mg/m2/day from days 1 to 14 and oxaliplatin at a dose of 130 mg/m2 on the 1st day of each three-week course; up to eight courses in total. Objective effect was achieved in 63% of cases, including 2 complete and 32 partial tumor regressions. The median time to progression was 5.8 months, overall survival was 11.9. The regimen had low toxicity; side effects of grade III–IV were observed in isolated cases. Taking into account the ease of implementation and the high frequency of achieving the effect, the regimen can be assessed as one of the best in the treatment of advanced gastric cancer [4].
In a similar situation, therapy with irinotecan 250 mg/m2 on day 1 (45 patients) or cisplatin 80 mg/m2 on day 1 (46 patients) in combination with capecitabine 2000 mg/m2/day from day 1 had similar effectiveness. on the 14th day of each three-week course. An objective effect was achieved in 39 and 42% of cases, drug control of the disease was achieved in 64 and 74% of patients, respectively. Grade III treatment side effects were: anemia (3 and 9%), neutropenia (17 and 19%), diarrhea (17 and 5%), nausea (14 and 21%), vomiting (3 and 14%) and palmoplantar syndrome (6 and 2%). The median time to progression and overall survival were similar and were 5.2 and 5 months, 8.9 and 9.4 months, respectively [5].
For locally advanced and/or metastatic gastric cancer, a first-line outpatient regimen is of undoubted practical interest, including capecitabine 2000 mg/m2/day from the 1st to the 14th day and docetaxel 75 mg/m2 on the 1st day of each three week course. According to preliminary data, in 70% of cases, patients experienced a significant regression of tumor symptoms (38 patients were assessed). Objective effect was achieved in 55.3% of cases, stabilization – in 36.8%. The median time to progression was 5.5 months, overall survival was 9.5. Of the grade III side effects, the most common were diarrhea (13%), asthenia (10%), stomatitis (10%), nausea (3%), and hand-foot syndrome (18%). Neutropenia of III and IV degrees was observed in 25 and 28% of patients, respectively, febrile neutropenia – in 10.3% [6].
The final results of chemotherapy with capecitabine 2000 mg/m2/day from days 1 to 14 and oxaliplatin 130 mg/m2 on day 1 of each three-week cycle for inoperable or metastatic biliary tract cancer are presented. The most significant side effect in the 65 patients assessed was grade III–IV peripheral sensory neuropathy, which complicated treatment in 13 cases (14% of courses). Other non-hematological complications of grade III–IV occurred in 1–2% of cases. Drug control of the disease in gallbladder cancer and cholangiocarcinoma was 72% (complete effect in 2 patients, partial effect in 11, stabilization in 21). Unfortunately, the authors do not provide data on survival, which, in our opinion, most accurately characterizes the results of treatment of this pathology [7].
The most effective regimens for disseminated colorectal cancer include oxaliplatin or irinotecan in combination with fluorouracil derivatives. It has now been proven that the inclusion of capecitabine in chemotherapy regimens is an adequate alternative to fluorouracil infusions. However, the results of large randomized trials have demonstrated a number of benefits of treatment with capecitabine. This area continues to be intensively studied.
The effect of capecitabine on the somatic status of patients with colorectal cancer was established in a retrospective analysis of 1210 case histories. In 42% of cases, during treatment, the status of patients ECOG ≥ 1 improved to ECOG 0. Depending on the initial status, pain syndrome significantly decreased (p Good preliminary results of 1st line chemotherapy were demonstrated with the use of irinotecan 80 mg/m2 in 1st and 8th days and capecitabine 2000 mg/m2/day from the 1st to the 14th day of each 21-day course. To date, 39 patients with colorectal cancer have been evaluated. An objective effect was achieved in 45% of patients, including 3 complete and 14 partial regressions, stabilization of the disease - in 8 (21%) patients. The duration of full effects exceeded 10 months at the time of publication. Side effects of III-IV degrees were acceptable: nausea and vomiting in 23% of cases, diarrhea - in 10%, leukopenia – in 5% [9].
Research continues on the inclusion of cyclooxygenase-2 inhibitors in capecitabine chemotherapy regimens. Judging by the data presented, the previously stated advantages of such combinations are ambiguous. In the 1st line, celecoxib 400 mg was added to treatment with irinotecan (70 mg/m2 on days 1 and 8) and capecitabine (2000 mg/m2/day from days 1 to 14 of each three-week course). 2 times a day every day. In a study of 51 colorectal cancer patients, objective response was achieved in 50% of cases with a median time to progression of 6.9 months and overall survival ≥ 19.4 months. Complications of grade IV were manifested by diarrhea in 2 (4%) patients; Grade III – diarrhea (33%), hand-foot syndrome (8%), nausea (13%), vomiting (8%) and neutropenia (12%) [10].
In a study by De Greve J. et al. compared the CAPIRI regimen (capecitabine 2000 mg/m2/day on days 1–14 and irinotecan 250 mg/m2 on the 1st day of each three-week course) with the FOLFIRI regimen (Douillard regimen; fluorouracil, leucovorin, irinotecan) ± celecoxib. After enrollment of 85 patients, enrollment was suspended until detailed analysis of eight deaths not related to disease progression. When using a combination of capecitabine with celecoxib, a therapeutic effect was achieved in 22% of cases, and if celecoxib was not used, then in 48%. Chemotherapy containing fluorouracil had a less significant difference (32 and 45%, respectively). When comparing the CAPIRI and FOLFIRI regimens, the treatment effect was almost the same: 15/44 (34%) and 16/41 (39%). Chemotherapy + celecoxib was less effective: 1¼2 (26%) in the celecoxib group and 20/43 (46%) in the placebo group. Diarrhea ≥ grade III complicated the following regimens: CAPIRI in 37% of cases (16/43), FOLFIRI in 13% (4/39). Median time to progression was 5.9 months (CAPIRI) versus 9.6 months (FOLFIRI); median overall survival was 14.8 and 19.9 months, respectively. Inclusion in celecoxib regimens did not significantly affect median time to progression and overall survival [11]. The data obtained force us to take a balanced approach to the recommendations for including cyclooxygenase-2 inhibitors in chemotherapy regimens.
It seems that recently oxaliplatin is gradually replacing irinotecan as a first-line chemotherapy regimen for colorectal cancer. The randomized study compared XELOX (capecitabine 2000 mg/m2/day on days 1–14 + oxaliplatin 130 mg/m2 on day 1 of each three-week course) and FUFOX (oxaliplatin 85 mg/m2 every 2 weeks + weekly 48-hour infusions of fluorouracil 2250 mg/m2). Each study group included 170 patients who had not previously received chemotherapy. The dose intensity in the XELOX regimen was 90% for capecitabine and 92% for oxaliplatin, in the FUFOX regimen - 78% for fluorouracil and 78% for oxaliplatin, which indirectly indicates the greater toxicity of the second regimen. Grade III–IV side effects of the XELOX and FUFOX regimens were represented by paresthesia (17.7 and 15.9%), asthenia (12.4 and 17.1%), diarrhea (14.1 and 23.6%), neutropenia ( 8.3 and 10.0%) and nausea (4.1 and 7.6%). The therapeutic effect when using the XELOX and FUFOX regimens was achieved equally often: in 37 and 43% of cases, respectively (p = 0.824). Median follow-up was 12.6 months in both groups, time to progression was 8.8 and 9.6 months, respectively (p = 0.130) [12]. Thus, both regimens did not have significant differences in therapeutic activity and toxicity profile. Nevertheless, the XELOX mode, in our opinion, is preferable as it is more convenient for the patient and less labor-intensive.
As was shown earlier, the so-called drugs. target group - cetuximab, which is a monoclonal antibody to the epidermal growth factor receptor (EGFR), and bevacizumab (Avastin®, F. Hoffmann-La Roche Ltd., Switzerland), which is a monoclonal antibody to vascular endothelial growth factor (VEGF), significantly increase efficiency and, most importantly, improve long-term results of chemotherapy for colorectal cancer.
As an example, we can present the results of a phase II study, where in the 1st line of therapy the XELOX regimen (oxaliplatin + capecitabine) was compared with a similar regimen including cetuximab (loading dose 400 mg/m2, then 250 mg/m2 weekly). Treatment was limited to six courses. In 67 patients evaluated, the inclusion of cetuximab in therapy increased the rate of achieving an objective effect from 33 to 53% while maintaining the rate of achieving drug control of the disease (objective effect + stabilization), which was 82% in both groups. Grade III–IV side effects were equally common, with the exception of skin toxicity characteristic of cetuximab (6 vs. 0%) [13].
In another study, 50 patients in the 1st line of therapy received oxaliplatin 85 mg/m2 on day 1, capecitabine 2000 mg/m2/day on days 1–5 and 8–12, and bevacizumab 10 mg/kg on the 1st day of each two-week course (XELOXA regimen). Subsequently, due to the development of grade II-III diarrhea in 56% of patients and hand-foot syndrome in 43% of patients, the dose of Xeloda was reduced to 1700 mg/m2/day, which led to a two- and three-fold decrease in the incidence of these complications, respectively. . Other grade III adverse reactions were minimal: neurotoxicity – 8%, nausea – 6%, neutropenia – 4%. 1 complete and 22 partial tumor regressions were achieved, the objective effect was 47%. Stabilization of the disease was recorded in 21 patients (43%). The median time to progression was 10.7 months (95% confidence interval, 8.6–13.6) [14].
In addition to the high therapeutic effect of the treatment regimen used, this work clearly shows that reducing the dose of capecitabine by 25% leads to a significant (two to three times) reduction in the incidence of dose-limiting toxicity.
Based on the known fact of potentiation of the antitumor effect of capecitabine when using radiation therapy, work devoted to chemoradiation treatment of rectal cancer, especially in the neoadjuvant mode, deserves undoubted interest.
In one study, 87 patients with locally advanced rectal cancer received radiation therapy (ROD - 1.8 Gy; SOD - 45 Gy, 5 fractions per week, 5 weeks), during the entire period of which they were prescribed capecitabine at a dose of 825 mg /m2/day and weekly administrations of oxaliplatin at a dose of 50 mg/m2. Six to eight weeks after completion of chemoradiotherapy, patients underwent surgical treatment (79 patients at the time of publication). In case of radical surgery, patients were additionally prescribed six courses of adjuvant chemotherapy with capecitabine and oxaliplatin. Resection R0–R1 was performed in 70 (82%) patients, of which R0 – in 57 (67%), while complete morphological remission was established in 13% of cases. The objective effect of chemoradiation treatment reached 70% (7% complete and 63% partial regressions). Complications of grade III preoperative therapy were rare: diarrhea – 16%, neuropathy – 1%, neutropenia – 1%, hand-foot syndrome – 1% [15].
Thus, based on the high therapeutic efficacy of capecitabine (Xeloda) demonstrated in clinical studies, we can conclude that this drug can be considered as one of the basic 1st-line drugs for chemotherapy of malignant tumors of the digestive tract.