Chronic cerebrovascular accident (cerebral vascular insufficiency) is characterized by a decrease in blood supply to the brain. This condition is very common among older people in developed countries due to the high prevalence of atherosclerosis. In most cases, the carotid artery is damaged. A pair of carotid arteries, one on each side of the neck, running parallel to the jugular vein, are the main arteries that supply blood to the brain.
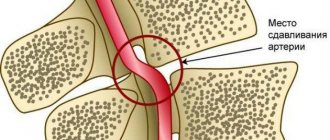
As a rule, cerebral vascular insufficiency develops in the area of the bifurcation of the carotid artery - the splitting of the carotid artery into internal and external branches. This splitting is similar to a stream that has split into two streams. In bifurcation, as well as during bifurcation in a water flow, accumulation of slag occurs. Severe symptoms begin to appear in most cases only when the artery blockage reaches 90 percent. This situation is similar to what happens with coronary heart disease.
Symptoms of chronic cerebrovascular accident are caused by decreased blood flow and oxygen supply to the brain. Stopping the flow of blood and oxygen leads to a stroke. The official definition of stroke is "loss of nerve function for at least 24 hours due to lack of oxygen." Some strokes are mild; others result in paralysis, coma, or speech impairment, depending on what part of the brain is involved. Mini-strokes, or transient ischemic attacks, can result in loss of nerve function for an hour or more, but less than 24 hours. TIAs can lead to transient symptoms of cerebral vascular insufficiency: dizziness, ringing in the ears, blurred vision, confusion, and so on.
Atherosclerosis is one of the main causes of cerebrovascular insufficiency. As this process progresses, high cholesterol levels combined with inflammation in the walls of the arteries in the brain can cause cholesterol to accumulate on the vessel wall in the form of a thick, waxy plaque. This plaque can restrict or completely prevent blood flow to the brain, causing stroke, transient ischemic attacks, or dementia, which can lead to a variety of other health complications.
The most common forms of cerebrovascular disease of the brain are thrombosis (40% of cases) and cerebral embolism (30%), followed by cerebral hemorrhages (20%).
Another form of cerebrovascular disease includes aneurysms. In women with defective collagen, weak key arterial branch points result in ridges with a very thin endothelial covering that can easily rupture with minimal increase in blood pressure. It can also occur with poor capillaries caused by cholesterol deposition in tissues, especially in hypertensive patients with or without dyslipidemia. If bleeding occurs, the result is a hemorrhagic stroke in the form of subarachnoid hemorrhage, intracerebral hemorrhage, or both.
A drop in blood pressure during sleep can lead to a marked decrease in blood flow in narrowed blood vessels, causing ischemic stroke in the morning. Conversely, a sharp increase in blood pressure due to daytime agitation can lead to rupture of blood vessels, resulting in intracranial hemorrhage. Cerebrovascular disease primarily affects people who are elderly or have a history of diabetes, smoking, or coronary heart disease.
What is a stroke
The essence of a stroke is the cessation of blood supply and functioning of a part of the brain as a result of damage to a vessel.
The larger the affected area, the more severe the stroke. Necrosis of a portion of the brain substance is called an infarction [3]. There is a high risk of death in the first few hours, and then in the period up to 28 days after a vascular accident. The annual mortality rate from stroke in the Russian Federation is 374 cases per 100,000 [10]. In 2018, 35% of patients died in the acute period of stroke; by the end of the first year, this figure increases by 15%, and in general, in the first 5 years, the mortality rate of strokes is 44% [11]. The mortality rate from stroke was 92.9 per 100,000 population, and the hospital mortality rate was 19.1% [5].
Long-term disability is most likely for patients who have suffered a stroke. The prevalence of primary disability due to stroke in 2018 was 3.2 per 10 thousand population [2]. Of these, 31% need constant care, 20% have severe mobility limitations, and only 8% return to work [3]. The prevalence of recurrent strokes in 2014 was 0.79%, of which ischemic
strokes account for 87.5% [9].
Causes of stroke
Depending on the cause of cerebrovascular accident, ischemic and hemorrhagic strokes are distinguished.
Ischemic stroke occurs as a result of blockage of cerebral vessels by a blood clot, when gradually less and less blood flows to an area of the brain. Hemorrhagic stroke develops as a result of rupture of a vessel and hemorrhage in the brain tissue, as a result of which the blood supply to its area abruptly stops. Hemorrhage can be into the subarachnoid space (SAS) or directly into the cerebral substance (ICH). The ratio of ischemic and hemorrhagic strokes is 4-5:1 [4].
Pathologically, a stroke can be cardioembolic, lacunar, atherothrombotic, or another, including unknown, etiology (TOAST classification) [10].
Predisposing factors:
- men from 45 to 59 years old;
- age 70 years and older (for both sexes) [4];
- arterial hypertension;
- atrial fibrillation;
- atherosclerosis of cerebral vessels;
- coagulopathy, thrombophilia, anemia;
- arteriovenous malformations;
- osteochondrosis with damage to the vertebral artery;
- brain tumors;
- dyslipoproteinemia;
- obesity;
- diabetes;
- intermittent claudication;
- mechanical prostheses of heart valves and blood vessels;
- IHD, myocardial infarction less than 6 months before the stroke;
- other cardiac diseases;
- smoking, alcoholism;
- family history of stroke;
- sedentary lifestyle;
- stress [1, 3].
Cerebrovascular accident
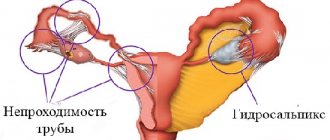
Cerebral circulation is blood circulation in the vascular system of the brain and spinal cord. In a pathological process that causes cerebral circulatory disorders, the main and cerebral arteries (aorta, brachiocephalic trunk, as well as common, internal and external carotid, vertebral, subclavian, spinal, basilar, radicular arteries and their branches), cerebral and jugular veins may be affected , venous sinuses. The nature of the pathology of cerebral vessels can be different: thrombosis, embolism, kinks and looping, narrowing of the lumen, aneurysms of the vessels of the brain and spinal cord.
Morphological changes in the brain tissue of patients with cerebrovascular accidents, according to the severity and location, are determined in accordance with the underlying disease, the mechanisms of development of the circulatory disorder, the blood supply pool of the affected vessel, age, and individual characteristics of the patient.
Signs of cerebrovascular accident
Morphological signs of cerebrovascular accident are divided into focal and diffuse. Focal signs include hemorrhagic stroke, cerebral infarction, intrathecal hemorrhage; diffuse signs include multiple small-focal changes in the brain substance of varying nature and varying degrees of age, small fresh and organizing foci of necrosis of brain tissue, small hemorrhages, gliomesodermal scars, small cysts.
At the time of cerebrovascular accident, subjective sensations without objective neurological symptoms, such as dizziness, headache, paresthesia, etc., may be clinically present; organic microsymptoms without clear symptoms of loss of central nervous system function; focal disorders of the higher functions of the cerebral cortex - agraphia, aphasia, alexia, etc., dysfunction of the sensory organs; focal symptoms: motor disorders - coordination disorders, paresis or paralysis, hyperkinesis, extrapyramidal disorders, sensitivity disorders, pain; changes in memory, intelligence, emotional-volitional sphere; psychopathological symptoms, epileptic seizures.
Disturbances of cerebral circulation by nature can be divided into initial manifestations of insufficiency of blood supply to the brain, acute disorders of cerebral circulation (stroke, transient disorders, intrathecal hemorrhages) and slowly progressive chronic disorders of cerebral and spinal circulation (dyscirculatory myelopathy and encephalopathy).
Symptoms of cerebrovascular accident
Clinical symptoms of initial manifestations of insufficient blood supply to the brain include symptoms that appear after intense mental and physical work and after being in a stuffy room: dizziness, headache, decreased performance, noise in the head, sleep disturbance. As a rule, such patients do not have focal neurological symptoms or are represented by scattered microsymptoms. Diagnosis of the initial manifestations of insufficient blood supply to the brain consists of identifying objective signs of atherosclerosis, vasomotor dystonia, arterial hypertension and excluding other somatic pathologies, as well as neurosis.
Acute cerebrovascular accidents include strokes and circulatory disorders in the brain that are transient in nature.
Such transient disorders of cerebral circulation manifest themselves in the form of focal and/or cerebral symptoms that last less than a day. Most often, these symptoms are observed in hypertension, cerebral atherosclerosis, and arterial hypertension. A distinction is made between hypertensive cerebral crises and transient ischemic attacks.
Transient ischemic attacks are characterized by the appearance of focal neurological symptoms against a background of mild symptoms (static disturbances, difficulty speaking, weakness and numbness of the limbs, diplopia, etc.)
Hypertensive cerebral crises, on the contrary, are characterized by a predominance of general cerebral symptoms over focal ones, such as dizziness, headache, nausea or vomiting. In some cases, these symptoms may be absent. A case of acute cerebrovascular accident with persistence of focal neurological symptoms for more than a day is considered a stroke.
Acute disorders of venous circulation in the brain also include venous hemorrhages, thrombosis of the venous sinuses and cerebral veins. Chronic disorders of cerebral circulation (myelopathy and discirculatory encephalopathy) appear as a result of progressive insufficiency of blood supply, which is caused by various vascular diseases.
Discirculatory encephalopathy usually manifests itself with diffuse organic symptoms, combined with headaches, memory impairment, irritability, non-systemic dizziness, etc. There are three stages of discirculatory encephalopathy.
The first stage, in addition to mildly expressed scattered persistent organic symptoms (asymmetry of cranial innervation, slight oral reflexes, inaccuracies in coordination, etc.), is characterized by the presence of a syndrome that is similar to the asthenic form of neurasthenia (absent-mindedness, fatigue, memory impairment, difficulty switching from one activity to another , non-systemic dizziness, dull headaches, poor sleep, depressed mood, irritability, tearfulness). At the same time, intelligence does not suffer.
The second stage is characterized by progressive memory deterioration (including in the professional sphere), decreased performance, decreased intelligence, personality changes, manifested in a narrowing of interests, apathy, the appearance of rigidity of thought, often verbosity, irritability, quarrelsomeness, etc.). Daytime sleepiness with poor sleep at night is typical. More distinct are organic symptoms, such as mild dysarthria, changes in muscle tone, tremor, coordination and sensory disorders, bradykinesia, reflexes of oral automatism and other pathological reflexes.
The third stage of discirculatory encephalopathy is characterized by both worsening mental disorders (to dementia) and the development of neurological syndromes that are associated with damage predominantly to a specific area of the brain. This may be parkinsonism, pseudobulbar palsy, pyramidal insufficiency, cerebellar ataxia. The condition often deteriorates, occurring in the form of a stroke. At the same time, new focal symptoms appear and the previously existing signs of cerebrovascular insufficiency intensify.
Discirculatory myelopathy is also characterized by a progressive course, in which three stages are conventionally distinguished.
The first (compensated) stage is manifested by moderately severe fatigue of the muscles of the limbs, and in more rare cases, weakness of the limbs. Further, in the second (subcompensated) stage, weakness in the limbs progressively increases, sensory impairment of the segmental and conduction type and changes in the reflex sphere appear. In the third stage of discirculatory myelopathy, paresis or paralysis, severe sensory disturbances, and pelvic disorders develop. Focal syndromes in nature depend on the localization of pathological foci along the diameter and length of the spinal cord. Possible clinical syndromes include poliomyelitis, pyramidal, syringomyelic, amyotrophic lateral sclerosis, posterior columnar, and transverse spinal cord lesions.
Chronic disorders of venous circulation include venous congestion, which causes venous encephalopathy and venous myelopathy. Venous stagnation occurs due to compression of extracranial veins in the neck, cardiac or pulmonary-heart failure, etc. There may be long-term compensation for the difficulty of venous outflow of blood from the cranial cavity and spinal canal; with decompensation, headaches, seizures, cerebellar symptoms, and dysfunction of the cranial nerves may occur. Venous encephalopathy is characterized by a variety of clinical manifestations. Hypertensive (pseudotumor) syndrome, asthenic syndrome, and syndrome of diffuse small-focal brain lesions may be present. Venous encephalopathy also includes bettolepsy (cough epilepsy), which develops in diseases that lead to venous stagnation in the brain. Venous myelopathy, being a particular variant of discirculatory myelopathy, is not clinically significantly different from the latter.
Causes of cerebrovascular accidents
The main cause of cerebral hemorrhage is high blood pressure. With a sharp rise in blood pressure, a vessel may rupture, causing blood to enter the brain, causing an intracerebral hematoma.
A more rare cause of hemorrhage is a ruptured aneurysm. As a rule, related to a congenital pathology, an arterial aneurysm is a protrusion in the form of a sac on the wall of a vessel. The walls of such a protrusion, unlike the walls of a normal vessel, do not have a sufficiently powerful muscular and elastic frame. Therefore, sometimes a relatively small increase in pressure, which can be observed during physical activity or emotional stress in completely healthy people, leads to rupture of the aneurysm wall.
Along with saccular aneurysms, other congenital anomalies of the vascular system may be present, which pose a risk of sudden hemorrhage. If the aneurysm is located in the walls of blood vessels that are on the surface of the brain, rupture of the aneurysm leads to the development of subarachnoid hemorrhage rather than intracerebral hemorrhage. Subarachnoid hemorrhage is located under the arachnoid membrane surrounding the brain. It does not directly lead to the development of focal neurological symptoms (speech disorders, paresis, etc.), but when it occurs, general cerebral symptoms are pronounced, such as a sharp (“dagger”) sudden headache, often accompanied by subsequent loss of consciousness.
There are four great vessels: the right and left internal carotid arteries, which supply blood to most of the brain; the right and left vertebral arteries, which merge into the main artery and supply blood to the brain stem, occipital lobes of the cerebral hemispheres and the cerebellum.
There may be various reasons for blockage of the main and cerebral arteries. An inflammatory process on the heart valves, in which infiltrates or a parietal thrombus is formed in the heart, can lead to the fact that broken pieces of a thrombus or infiltrate can travel through the bloodstream to a brain vessel whose caliber is smaller than the size of the piece (embolus), as a result of which they clog vessel. Emboli can also be particles of a disintegrating atherosclerotic plaque located on the walls of the main artery of the head. This is an embolic mechanism for the development of cerebral infarction.
Another, thrombotic mechanism for the development of a heart attack is the gradual development of a thrombus (blood clot) in the place where the atherosclerotic plaque is located on the vessel wall. An atherosclerotic plaque fills the lumen of the vessel. This leads to slower blood flow and promotes the development of a blood clot. Thanks to the uneven surface of the plaque, the adhesion (aggregation) in this place of platelets with other blood elements improves, which is the main framework of the resulting thrombus. For a blood clot to form, local factors alone are usually not enough. In addition, the development of thrombosis occurs as a result of a slowdown in blood flow (for this reason, thrombosis of cerebral vessels, unlike embolisms and hemorrhages, usually develop at night, during sleep), an increase in the aggregation properties of platelets and red blood cells, and an increase in blood clotting.
Everyone knows from experience what blood clotting is. If you accidentally cut your finger, blood will flow from it. But the bleeding will stop due to the fact that a blood clot (thrombus) appears at the site of the cut.
Blood clotting is a biological factor that contributes to human survival. However, both increased and decreased blood clotting is a threat to our health and even life.
With increased blood clotting, thrombosis may develop; with decreased blood clotting, bleeding may occur due to the slightest cuts or bruises. Hemophilia, a disease accompanied by reduced blood clotting and having a hereditary nature, was inherent in many members of the ruling families of Europe, including Tsarevich Alexei, the son of the last Russian emperor.
Disruption of normal blood flow can occur due to spasm (strong compression) of the vessel, which occurs due to a sharp contraction of the muscle layer of the vascular wall. In the development of cerebral circulatory disorders, great importance was attached to spasm several decades ago. Currently, cerebral vasospasm is mainly associated with cerebral infarction, which can develop several days after the occurrence of subarachnoid hemorrhage.
With frequent increases in blood pressure, changes can occur in the walls of small vessels that feed the deep structures of the brain. The changes that occur lead to narrowing and often to the closure of these vessels. Sometimes a sharp rise in blood pressure (hypertensive crisis) develops into a small infarction in the circulatory system of a vessel (in the scientific literature this phenomenon is called a “lacunar” infarction).
In some cases, cerebral infarction develops without complete blockage of the vessel, called a hemodynamic stroke. You can imagine this process with a clear example. You are watering your garden with a hose that is clogged with silt. But the power of the electric motor of the pump lowered into the pond is sufficient to obtain a normal stream of water and high-quality watering of your garden. However, if the hose is slightly bent or the motor performance deteriorates, the powerful stream is replaced by a thin stream, which is clearly not enough to water the soil well.
The same situation under certain conditions is observed with blood flow in the brain. In the presence of two factors: a sharp bend in the lumen of a main or cerebral vessel or its narrowing due to a filling atherosclerotic plaque, plus a decrease in blood pressure, which occurs due to a deterioration (often temporary) in the functioning of the heart.
The mechanism of transient cerebrovascular accidents (in other words, transient ischemic attacks) is in many ways similar to the mechanism of development of cerebral infarction. But with transient disturbances of cerebral circulation, compensatory mechanisms work quickly, and within a few minutes (hours) the developed symptoms disappear. However, one should not hope that compensation mechanisms will cope with the violation that has arisen with the same success. Therefore, understanding the causes of cerebrovascular accidents is so important. This allows us to develop methods to prevent repeated disasters.
Factors contributing to the formation of strokes
- diabetes mellitus, smoking, use of contraceptives;
- high blood pressure, ischemia of the heart muscle, pathology of blood parameters, a history of strokes;
- disturbance of blood flow, microcirculation of peripheral arteries (increasing the risk of ischemic stroke by 2 times);
- high weight in the presence of atherosclerosis;
- lipid metabolism disorder;
- alcohol abuse;
- sedentary lifestyle;
- stressful condition.
Consequences of a stroke
One of the main dangers of a stroke is that as a result of this disease there is a high probability for the patient to become disabled. About 30% of people who have suffered a stroke cannot cope without the help of other people and their care within a year. Throughout the world, stroke has been assigned the status of a disease that most often leads to disability. Particularly sad is the fact that stroke is the second most common cause of dementia. Stroke also leads to deterioration of cognitive abilities (attention, memory), reduces performance, learning, and thinking abilities.
Considering the above, if you detect the first signs of cerebrovascular accident, you should contact a neurologist.
Prevention of cerebral blood supply disorders
Measures to prevent cerebral blood supply disorders are quite simple. But that is precisely why they are most often neglected.
Below are the basic principles to follow.
- Move more
- No smoking
- Don't use drugs
- Control and maintain normal body weight
- Reduce the amount of salt you consume
- Monitor glucose levels, as well as triglycerides and lipoproteins in the blood
- Treat existing cardiovascular diseases
Signs of an incipient stroke
The onset of a hemorrhagic stroke is characterized by the following symptoms:
- severe headache;
- increased blood pressure;
- vomit;
- dizziness;
- loss of consciousness;
- weakness in the limbs;
- visual impairment;
- seizures [1].
The onset of ischemic stroke is gradual; within an hour, some of the following symptoms appear:
- facial asymmetry, numbness;
- difficulty speaking – incoherent, impaired understanding;
- double vision, visual disturbances;
- headache;
- numbness, limited mobility in the limbs, often on one side;
- dizziness, imbalance, staggering, staggering gait;
- confusion with disorientation, subsequently there may be loss of consciousness [3].
If one or more of these signs appear, you should:
- Sit the patient down, providing access to fresh air.
- Call emergency medical help immediately.
- If the patient is conscious and able to chew and swallow, give him one aspirin tablet.
The patient must be hospitalized in a neurological or neurosurgical department, where stroke treatment will be carried out. The sooner the patient is in the hospital, the more effective the therapy.
Symptoms of a stroke
Stroke leads to various brain injuries, depending on the location of the lesion and the pathological type of cerebrovascular accident:
- disturbances of movement in the limbs: from restrictions (paresis) to complete paralysis. When the lesion is localized on the right, the left limbs suffer; with a left-sided lesion, right hemiparesis is formed; in some cases, movements in all limbs may stop (tetraparesis or double hemiparesis);
- sensory disturbances on one or both sides;
- speech disorders (dysarthria - poor articulation; aphasia - inability to pronounce and understand words, write and read);
- ataxia (impaired coordination of movements, “overshooting”, unsteadiness, imbalance, tremor);
- visual impairment: from blindness to double vision and gaze paresis;
- hearing impairment and dizziness;
- violation of mental functions (consciousness, thinking, attention, memory, will, behavior);
- paresis of the soft palate and pharynx, swallowing disorders;
- disorders of urination and defecation;
- depression of respiration and vascular tone;
- increased intracranial pressure;
- patients complain of headaches, vomiting, hiccups, yawning, shoulder pain;
- consciousness is gradually depressed to the point of coma [1, 3].
Causes of death may include cerebral edema, pneumonia, heart failure, and recurrent stroke. In severe cases, “locked-in syndrome” may develop: the patient is conscious, but cannot move, swallow or speak [3].
Diagnosis of the disease
When the first signs of cerebrovascular accident appear, you must call an ambulance or go to the hospital yourself (if your condition allows). The doctor will perform an examination and collect anamnesis (description of the patient’s condition and related data). The doctor must be provided with the following information:
- main complaints (headache, disturbance in the functioning of the sensory organs, nausea, etc.);
- when the condition worsened;
- under what conditions;
- the presence of risk factors for stroke (smoking, alcoholism, chronic diseases, taking medications).
A simple test can detect the development of stroke or stroke (provided that the patient is conscious):
- It is necessary to ask the patient to smile (with stroke, the smile will be skewed);
- It is necessary to ask the patient to stretch his arms forward and then raise them up (with a stroke he will not be able to do this or will only raise one arm);
- Ask the patient to repeat any simple sentence (with stroke, this will cause difficulties);
- Ask the patient to stick out his tongue (with stroke, the tongue will be clearly displaced from the center).
The doctor assesses the general and local status of stroke. General status represents the general condition of the patient, clinical manifestations of cerebrovascular accident. Local status is described in the presence of head trauma. The collected data gives the doctor an idea of the patient’s condition, on the basis of which he prescribes examinations to obtain a complete picture of what is happening.
Diagnosis of stroke is carried out using visualization of nerve tissue using CT and MRI. These are the most informative diagnostic methods that allow you to identify the lesion. To provide timely assistance in case of acute stroke, the examination is carried out urgently. In some cases, the patient will need emergency surgery.
At the Yusupov Hospital you can undergo examinations of any complexity for acute stroke and stroke. The hospital is equipped with the latest technology, which allows for a quick and high-quality examination of the patient. High-precision technology will help establish an accurate diagnosis and the extent of brain damage.
Consequences of a stroke
There are transient ischemic attack (less than a day), minor stroke (from 1 day to 3 weeks) and stroke with persistent residual effects. The consequences of a stroke are expressed mainly in motor and sensory disorders, the formation of muscle contractures (pronounced constant restriction of movements in the joints), speech and swallowing disorders. General symptoms may also remain, including confusion, disturbances in thinking, will, and emotional regulation. Complications can develop: from epilepsy to bedsores, encephalopathy and anxiety-depressive syndrome [1, 3].
Consequences
The consequences of stroke and stroke can be very severe, even death. Residual effects of stroke may be present throughout life, even after the end of the main therapy. Therefore, it is very important to undergo a rehabilitation course and, if necessary, repeat it over time. A person after a stroke needs willpower, as well as the support of loved ones to restore lost functions. Regular implementation of rehabilitation measures allows you to achieve good results in eliminating the consequences of stroke. Professionals at the Yusupov Hospital, using specialized techniques, will help you get the best effect in this difficult work.
The consequences of stroke will depend on the area of brain damage and the extent of the disorders. The degree of their severity can vary greatly: from imperceptible changes in behavior to complete paralysis. The consequences of stroke and stroke include:
- Complete or partial paralysis;
- Speech impairment;
- Impaired coordination of movements;
- Visual and hearing impairment;
- Impaired perception of space and time.
It is difficult for a person to move around, do the same job, or take care of himself. In severe cases, a person remains bedridden after a stroke. After a moderate stroke, the patient's speech is impaired; he cannot speak clearly or control the timbre and volume of his voice. Communication usually occurs through gestures and facial expressions. Memory impairment and the development of dementia are often noted. Another serious consequence of a stroke is depression. This condition should be taken seriously as a positive mental attitude is important for a person's continued recovery.
After a stroke, it is very important to undergo rehabilitation. With its help, you can recover after a stroke, albeit not completely, but significantly. The brain also needs training, like the rest of our body. A damaged brain requires special training under the supervision of professionals. The sooner rehabilitation measures are started, the greater the chances of maximum recovery after a stroke.
Diagnosis of strokes
First of all, it is necessary to conduct a detailed neurological examination. Instrumental diagnostic studies and laboratory tests are also prescribed. In case of a stroke, in the first hours, an MRI or CT scan of the brain is performed, if necessary, CT or MR angiography, color Doppler mapping of blood flow, ECG or Holter monitoring, echocardiography as indicated, monitoring of blood pressure, saturation, assessment of the risk of developing bedsores, assessment of swallowing function [ 1, 3, 6].
Tests for stroke
- Complete clinical blood test, including erythrocyte sedimentation rate (ESR).
- Biochemical blood test with determination of C-reactive protein and homocysteine, glucose level, platelet count, activated partial thromboplastin time, INR.
- Interleukin 10.
- Extended coagulogram.
- Determination of acid-base status.
- General urine analysis.
To prepare for neurosurgical intervention, a blood test is additionally performed for hepatitis, syphilis, HIV, blood group and Rh factor determination.
Stroke treatment
Treatment of stroke is regulated by relevant clinical guidelines and the Procedure for providing medical care to patients with acute cerebrovascular accident. In the first hours, thrombolytic therapy is carried out and subsequently - prevention of thrombus formation. For hemorrhagic stroke, neurosurgery may be performed. They normalize blood pressure, water-electrolyte balance, glucose levels in peripheral blood and urine, support the basic vital functions of the body and prevent complications. Drug therapy is also aimed at improving the affected functions of the nervous system [1, 3, 6].
Prevention of stroke
Prevention of pre-stroke and stroke conditions are measures to improve overall health and reduce the negative impact on the circulatory system. First of all, you need to quit smoking. Statistics for smokers are not favorable, and smoking negatively affects not only blood vessels, but also the condition of the lungs, heart muscle, liver, and skin.
You need to reconsider your diet. Eat more fruits and vegetables, foods with fiber (oatmeal, bran, beans, lentils). Reduce the amount of salt and salty foods you consume (salted fish, pickles, ready-made frozen meals, instant foods). Limit consumption of fatty foods (fatty meats, poultry skin, rendered pork and lamb fat, heavy cream and butter).
An effective way to prevent cerebrovascular accidents is moderate physical activity. Physical education should be done for at least 30 minutes three times a week. The intensity of exercise should correspond to the level of physical fitness and increase gradually, without overdoing it.
At the clinic you can get advice on individual methods of preventing strokes and strokes. Here they not only perform treatment, but also talk about measures to prevent pathology. You can make an appointment with a neurologist, cardiologist, or rehabilitation specialist by calling the Yusupov Hospital.
Stroke rehabilitation
Stroke is a disease in which rehabilitation and care are of the utmost importance.
Recovery from a stroke begins in intensive care, from the moment vital functions are stabilized. A multidisciplinary rehabilitation team works with the patient, which includes a rehabilitation doctor, physical therapist or exercise therapy instructor, speech therapist, massage nurse, physiotherapist and physical therapy nurse, psychologist, occupational therapist, guard and rehabilitation nurse. Diagnosis is carried out using special scales that reflect the degree of dysfunction and limitations in the patient’s activity, the influence of environmental factors on the rehabilitation potential. The rehabilitation process continues throughout the entire period of hospitalization. At the second stage, patients with serious disabilities who are unable to move independently are sent to rehabilitation departments or specialized hospitals. Those who can walk independently or with support are rehabilitated in outpatient centers based in clinics and sanatoriums.
The rehabilitation process should not be interrupted, so classes must be continued at home. Of course, there are no high-tech robotic complexes or physiotherapeutic equipment at home, but exercise therapy, massage, and work with a psychologist, speech therapist and occupational therapist are possible. For this purpose, telemedicine technologies are used and visits to rehabilitation specialists are organized.
The individual rehabilitation program includes not only a referral for rehabilitation treatment, but also technical means of rehabilitation. However, usually relatives also have to devote significant physical and financial resources to achieve the best effect [7].
Rehabilitation after stroke
In rehabilitation after stroke, the Yusupov Hospital uses an integrated approach to ensure the best recovery for patients. Physiotherapists, speech therapists, massage therapists, exercise therapy instructors, and occupational therapists work with the patient. Physiotherapy and exercise therapy can help restore motor functions. The massage therapist eliminates muscle spasms and normalizes their tone. The speech therapist's task is to restore speech and swallowing. An ergotherapist helps to adapt to new living conditions and teaches everyday skills.
The human brain has a unique property - neuroplasticity - the ability to regenerate. New connections between neurons are formed in the brain, due to which lost functions are restored. Neuroplasticity can be stimulated, which is what happens during the rehabilitation process. Regular exercises, which are selected individually depending on what function is to be restored, must be performed constantly, every day until the desired effect is obtained. Regularity is a key factor in achieving your goal; without it, it is impossible to achieve any results.
During the rehabilitation process, various elements of breathing exercises and intellectual exercises are used. All this helps the brain work better and better. Also in rehabilitation, various simulators can be used to help learn how to walk again or perform any action (for example, alternately bending and straightening fingers), provoking its implementation.
An important part of rehabilitation is moral and psychological support. The development of post-stroke depression significantly worsens the patient's condition. This condition can be caused by social isolation, lack of desired results in treatment, and certain medications.
Prevention of strokes
Hereditary predisposition to stroke, the presence of cardiac diseases, pathology of blood vessels and blood composition, age over 40 years, obesity and diabetes require a number of preventive measures:
- Maintaining normal blood pressure, taking antihypertensive drugs as prescribed by a doctor, monitoring blood pressure.
- Maintaining a normal level of physical activity, exercise, walking 30-40 minutes a day (for example, walking the dog).
- Conducting preventive examinations, including a standard set of laboratory parameters. During a preventive examination, the following tests are additionally required: gene diagnosis of CADASIL syndrome using the PCR method, plasma factors of the blood coagulation system, antibodies to prothrombin of the IgG and IgM classes to determine the risk of thrombosis, determination of polymorphisms associated with the risk of arterial hypertension, diabetes mellitus, lipid disorders exchange, in order to identify a predisposition to diseases that increase the risk of stroke, von Willebrand factor (a glycoprotein that ensures the formation of blood clots), complex laboratory tests for preclinical diagnosis of cardiovascular diseases are offered (“ELI-ANKOR-Test-12”, “Cardiorisk”).
- Avoiding chronic and acute stress, maintaining mental hygiene.
- Normalization of weight (BMI <25 kg/m2).
- Healthy eating (for example, Mediterranean diet, limiting salt to 5 5 g/day).
- Quitting smoking and taking psychoactive substances.
- Treatment of diseases that are a risk factor for stroke [8, 11].
Causes of circulatory disorders in the brain
- Systolic pressure is less than 60 or more than 180 millimeters of mercury.
- Insufficient metabolic control, accompanied by unreasonable dilation of cerebral vessels.
- Atherosclerosis of cerebral vessels.
- Decreased blood oxygen saturation.
The compensatory capabilities of the brain are great. Vascular anastomoses allow blood to be distributed throughout the entire volume of the organ, even if the inflow through the left or right carotid artery is disrupted. However, these mechanisms do not work for long; after some time, oxygen starvation develops, and the first signs of the disease appear. This is why it is important to seek medical help immediately.
Most often, NMC develops against the background of:
- history of traumatic brain injury;
- chronic venous insufficiency;
- hypertension,
- atherosclerosis, ischemic heart disease,
- osteochondrosis,
- diabetes mellitus,
- hormonal imbalance,
- excess weight,
- stress, stress
- chronic fatigue,
- lipid metabolism failure,
- drinking alcohol,
- smoking.
Bibliography
- Hemorrhagic stroke in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021. Developers: Association of Neurosurgeons of Russia. - Electronic text. - URB: (access date 08/18/2020).
- Efremova M.D. Stroke as an urgent socio-psychological problem / M.D. Efremova – electronic text//Skif. Questions of student science.- 2021 - No. 2(24) URB: (date of access 08/17/2021) Access mode: Cyberleninka electronic library system. — Text: electronic.
- Ischemic stroke and transient ischemic attack in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021 developers: All-Russian Society of Neurologists, National Association against Stroke, Association of Neurosurgeons of Russia, Association of Neuroanesthesiologists and Neuroreanimatologists, Union of Rehabilitologists of Russia. - Electronic text. - URB: ( access date 08/18/2020).
- Machinsky P.A. Comparative characteristics of incidence rates of ischemic and hemorrhagic stroke in Russia / P.A. Machinsky, N.A. Plotnikova, V.E. Ulyankin [and others] – Direct text.// News of higher educational institutions. Volga region. Medical Sciences.- 2021.- “2(50)-P.112 – 132 DOI 10.21685/2072-3032-2019-2-11.
- Monitoring the implementation of the federal project “Combating Cardiovascular Diseases” - Presentation Department of Organization of Medical Care and Sanatorium Affairs of the Ministry of Health of the Russian Federation URB: (date of access 08/17/2021).
- Order of the Ministry of Health of the Russian Federation dated November 15, 2012 N 928n “On approval of the Procedure for providing medical care to patients with acute cerebrovascular accidents.” — URB: (access date 08/17/2021) Access mode: Electronic library system “Garant”. — Text: electronic.
- Order of the Ministry of Health of the Russian Federation dated July 31, 2021 No. 788n “On approval of the Procedure for organizing medical rehabilitation of adults.” – URB: (date of access 08.17.2021).- Access mode: Electronic library system “Garant”. — Text: electronic.
- Prevention of cerebrovascular accidents: textbook. manual / Compiled by: L.B. Novikova, A.P. Akopyan. – Ufa: Publishing house of the State Budgetary Educational Institution of Higher Professional Education BSMU of the Ministry of Health of Russia, 2015.-58 p.
- Stakhovskaya L.V. Analysis of epidemiological indicators of recurrent strokes in the regions of the Russian Federation (based on the results of the territorial-population register 2009-2014) / L.V. Stakhovskaya, O.A. Klochikhina, M.D., Bogatyreva, etc.]. CONSILIUM MEDICUM, 2021, vol. 5, no. 9, p. 8-11.
- Shamalov N. A. Analysis of the dynamics of the main types of stroke and pathogenetic variants of ischemic stroke / N. A Shamalov, L. V Stakhovskaya, O. A Klochikhina [and others]. Direct text. // Journal of Neurology and Psychiatry named after. S.S. Korsakov. Special issues. 2019;119(3-2):5-10. doi.org/10.17116/jnevro20191190325.
- 1RRE Electronic edition. Updated daily Stroke Day is celebrated on October 29, 2021 URB: (accessed 08/17/2021).
Author:
Pugonina Tatyana Alekseevna, Therapist