Anesthesia (anesthetics, general anesthetics) are medications that cause anesthesia - a temporary loss of consciousness and all types of sensitivity, primarily pain. In large doses, anesthetics inhibit reflexes and cause deep muscle relaxation.
Another name for anesthesia is general anesthesia.
It is important not to confuse general anesthesia with local anesthesia. With local anesthesia, the loss of pain sensation is limited to a small area of the body around the injection site of the local anesthetic. In addition, with local anesthesia, the patient is conscious, unlike general anesthesia.
Any anesthesia occurs in four stages:
- The stage of pain relief (analgesia) is the loss of pain sensitivity, but the patient is still conscious.
- Excitation stage – speech and motor excitation; a very short stage, practically absent with modern anesthetics.
- The stage of anesthesia is loss of consciousness, decreased muscle tone, suppressed reflexes. Depending on the depth of general anesthesia, superficial, light, deep and ultra-deep anesthesia are distinguished.
- The stage of recovery from anesthesia is awakening. In case of an overdose of anesthesia, the exit stage is replaced by the agonal stage with respiratory depression and cardiac arrest.
All anesthetic drugs have a rapid effect, causing the patient to black out within a few seconds of the start of administration.
Indications for use
Anesthesia is used for various surgical interventions (operations), including for pain relief for short-term operations in dentistry, gynecology, childbirth anesthesia, traumatology (fusion of dislocations, fractures).
Certain anesthetic drugs are used to eliminate severe pain and prevent pain shock in myocardial infarction, acute pancreatitis, multiple injuries (for example, car accidents, falls from a height), severe and extensive burns.
Anesthesia can also be used to relieve (eliminate) status epilepticus, a severe complication of epilepsy in which the patient’s seizures follow one another without stopping.
Anesthesia[edit | edit code]
A. Application of anesthesia
by anesthesia
is called a reversible drug blocking of the functions of the nervous system in order to turn off the patient’s consciousness, anesthetize, immobilize and reduce autonomic reflexes during surgery.
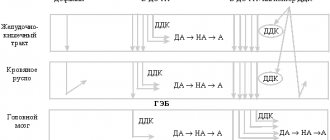
The required depth of anesthesia depends on the intensity of pain, i.e., on the degree of nociceptive stimulation. The anesthesiologist administers anesthesia dynamically in accordance with the actions of the surgeon. Initially, anesthesia was performed with one drug. In Boston in 1846, Morton first demonstrated the possibility of using diethyl ether for anesthesia. With such mononarcosis, in order to immobilize the patient, higher doses of the drug were needed than to turn off consciousness. In this case, it is possible to turn off the vital functions of the body (breathing, regulation of blood circulation). With modern anesthesia, thanks to the combination of various pharmacological agents, all goals are achieved (combined anesthesia). The risk of anesthesia is reduced. In Fig. Examples of the use of anesthesia and possible combinations of drugs are presented. It must be recalled that “curarization” of the patient requires artificial respiration. The use of muscle relaxants has led to modern anesthesia being performed without risk. Before moving on to a description of anesthesia, let's introduce the different types of anesthesia. B. Previously - mononarcosis, today - combined anesthesia
Neuroleptanalgesia
(droperidol + fentanyl) and neuroanaesthesia (+ laughing gas, i.e. nitrous oxide N20) are now considered obsolete. Disadvantage: incomplete switching off of consciousness and extrapyramidal states.
Regional anesthesia (spinal anesthesia) is performed using a local anesthetic to stop the pain. Such anesthesia is not essentially anesthesia (consciousness is preserved).
B. Example of combined anesthesia
There are drugs for inhalation and non-inhalation anesthesia. They fall under the definition of anesthesia in the narrow sense.
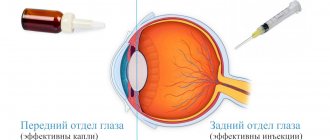
Inhalation anesthesia agents are administered along with inhaled air and are eliminated (to a greater or lesser extent) also through the respiratory tract. They are used primarily to maintain anesthesia.
Injection anesthetics are used to induce anesthesia. The intravenous route of administration and rapid effect are more favorable for the patient than inhaling narcotic gas. The duration of action of the intravenously administered anesthetic is several minutes. During this time, quick manipulations are carried out or the patient is prepared for inhalation anesthesia (intubation). It is necessary to maintain a balance between inhalational and intravenous anesthetic. For long-term anesthesia, anesthetics are now increasingly administered intravenously rather than by inhalation (eg, propofol; total intravenous anesthesia, abbreviated TVA).
Means for inhalation anesthesia[edit | edit code]
A. Lipophilicity and activity.
Removal of nitrous oxide N20 and halothane The mechanism of action of these substances is not fully known. Due to the fact that the substances used for such anesthesia (inert gas xenon, hydrocarbons, alkane halides) are very different in their chemical nature, it is difficult to explain what in these substances is the “cause” of the narcotic effect. There is a certain correlation between the effectiveness of the anesthetic and its lipophilic properties (A). On the hydrophobic side of cell membranes, there appear to be special areas that can be associated with neuronal dysfunction. It is assumed that interactions with lipophilic domains of membrane proteins, in particular proteins of ligand-gated ion channels, play a particularly important role in the mechanism of narcotic action.
The effectiveness of anesthetic agents is expressed in MAC values (minimum alveolar concentration). At this concentration, 50% of patients do not respond to painful stimulation (skin cuts). Nitrous oxide N20, which exhibits low lipophilicity, should be used in higher concentrations than, for example, halothane, which has pronounced lipophilicity.
The rate of onset of anesthesia and recovery from it depends mainly on the lipophilicity of the drug. Nitrous oxide is quickly eliminated from the body as soon as the patient begins to inhale clean air. This is due to certain reasons: due to the high partial pressure of N20 in the blood, the driving force for its transfer into exhaled air is large and, in addition, nitrous oxide does not accumulate in the tissues. On the contrary, the partial pressure of halothane in the blood is very low and it accumulates in the tissues. Therefore, halothane is eliminated from the body much more slowly.
Nitrous oxide, or laughing gas, cannot create anesthesia of sufficient depth even at a concentration of 80 vol.% (20 vol.% oxygen is the required minimum!).
Nitrous oxide has a pronounced analgesic effect, which is used when combining this gas with other anesthetics. Nitrous oxide is excreted unchanged by the lungs (B).
B. Routes of elimination of inhalation anesthesia
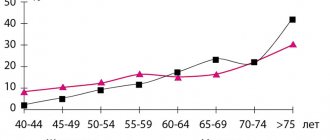
Halothane (bp 50 °C), enflurane (bp 56 °C), isoflurane (bp 48 °C) and new substances of this group, desflurane and sevoflurane, are used using special evaporators. Part of the halothane in the body (up to 20%) can be converted into toxic metabolites (reversible liver dysfunction) (B). In rare cases, halothane causes severe liver damage. With an increase in the number of anesthesia and a reduction in the intervals between them, the risk of hepatotoxicity of halothane increases (liver damage occurs in one case per 35,000 anesthesia).
During anesthesia with enflurane or isoflurane, 0.2-2% of these substances undergo biotransformation. Metabolic products have virtually no effect on the body.
Halothane significantly lowers blood pressure (vasodilation and negative inotropic effect). Enflurane and isoflurane have less effect on blood circulation. Halothane sensitizes the myocardium to the action of catecholamines. This effect is less pronounced with isoflurane and enflurane. They, unlike halothane, have a muscle relaxant effect, which is added to the action of non-depolarizing muscle relaxants.
Desflurane, metabolized by 0.2%, is structurally similar to isoflurane, but less lipophilic. Thanks to these properties, entry and exit from anesthesia occur faster and the controllability of anesthesia is very good. The newest drug in this group, sevoflurane, also acts quickly and the anesthesia is well controlled, but about 3% of this substance undergoes biotransformation.
Means for injection anesthesia[edit | edit code]
A. Redistribution of the drug in the body
Injection anesthetics include compounds of various chemical classes that, when administered intravenously, cause loss of consciousness (A). Unlike inhalational anesthetics, they do not have an analgesic effect (exception: ketamine). The action of anesthesia appears to be based on interaction with ligand-gated ion channels. Receptors active during excitation are blocked (NMDA receptor, see below), the functions of inhibitory receptors are regulated allosterically (GABA receptor; glycine receptor).
Most drugs are short-acting. The rapid cessation of action is explained by the distribution of the drug after injection in the well-supplied brain, where a high concentration of the drug is created and its action begins. Over time, the substance is redistributed evenly throughout the body: its concentration increases in the periphery, and in the brain decreases (the end of the narcotic effect, A). Thus, the effect ends before the drug leaves the body. Repeated administration of the drug while the body is saturated can have unpredictable consequences. Only etomidate and propofol can be administered to maintain anesthesia for a long time. If inhalational anesthetics are not additionally used, then we talk about total intravenous anesthesia (TIA).
Thiopental and methohexitape are classified as barbiturates. They turn off consciousness, but lower the threshold of pain sensitivity and depress the respiratory center. Barbiturates are often used for anesthesia.
Means for injection anesthesia
Ketamine acts as an analgesic regardless of loss of consciousness within 1 hour after injection. The duration of the unconscious state is about 15 minutes. After awakening, the patient may experience a state of dual consciousness (dissociative anesthesia). Many patients do not remember the awakening stage, but some complain of painful dreams. This condition can be prevented by the administration of benzodiazepines (eg, midazolam). The central effects of ketamine are due to its influence on the glutamate receptors responsible for excitation. Ketamine blocks the cation pores of the ionotropic glutamate receptor, the so-called NMDA receptor (NMDA - N-methyl-O-aspartate, an agonist of this receptor). Ketamine increases the release of catecholamines and thereby increases heart rate and blood pressure.
Propofol has a surprisingly simple chemical structure, reminiscent of the structure of phenol-based disinfectants. This compound is not soluble in water, so it is administered in the form of a suspension with the addition of soybean oil, phosphatide and glycerin. The action comes quickly and ends just as quickly, which is very beneficial for the patient. Anesthesia is well manageable with prolonged administration. Adverse reactions may include decreased blood pressure and respiratory depression.
The effect of (+)-etomidate, due to its redistribution in the body, ends after a few minutes. It can cause muscle cramps, which are prevented by premedication with a benzodiazepine or an opioid. Since it causes slight vegetative reactions, it is indicated for administration under combined anesthesia. Etomidate blocks the synthesis of cortisol. In case of increased adrenal function (Cushing's disease), this effect of etomidate can be used by prescribing it for a long time in a sub-narcotic dose.
Midazolam is a benzodiazepine that disintegrates quickly and is therefore used for anesthesia.
Basics of anesthesia treatment
Anesthetics are drugs that are subject to particularly strict accounting and control of circulation. You cannot buy them at the pharmacy even with a prescription. All anesthetic drugs are dispensed from pharmacies directly to clinics and hospitals using special documents - invoice requirements.
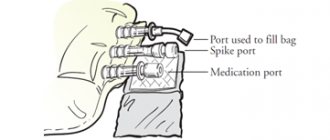
For anesthesia, the accuracy of their dosage is vital. To administer drugs for inhalation anesthesia, special anesthesia machines are used, which allow very precise dosing of substances delivered into the respiratory tract. Vapors of anesthetic drugs enter the lungs through an endotracheal tube, which is first introduced through the mouth and pharynx deep into the trachea. Non-inhalation anesthesia agents are administered intravenously.
For short-term operations, only inhalation anesthesia drugs are usually used. For long-term heavy operations, a combined anesthesia is usually used - both inhalation and induction - to ensure optimal general anesthesia.
The task of choosing anesthesia, calculating the dosage of drugs for a particular patient and constantly monitoring the course of general anesthesia during surgery (respiratory and cardiac indicators), as well as ensuring the patient’s recovery from anesthesia lies with the anesthesiologist.
The best anesthesia. Choice of anesthesia.
Patients often ask: “Which anesthesia is better!? Make it for me!” The answer is - anesthesia, which your personal anesthesiologist is fluent in, the main thing is that it is safe for health and life!
And, of course, each type and method of pain relief, like surgery, has its own specific indications and contraindications. And this is dictated, of course, by the volume and severity of the surgical intervention, and the somatic status of the patient:
- His health or any pathology, chronic diseases and the degree of compensation for these diseases and conditions. This also includes allergic reactions, age, and weight.
- Many other medical indicators based on the patient’s medical history, his tests and special research methods (if required).
This is, on the one hand, and on the other hand, the qualifications and experience of your anesthesiologist-resuscitator and medical staff in general, the equipment of the clinic, the availability of appropriate medications, etc. All this taken together influences the choice of the type and method of anesthesia (anesthesia) for a particular patient. In this case, the patient can express his wishes, and the doctor will make the final decision.
Under general anesthesia, for example, under ETN (deep endotracheal anesthesia), any operation can be performed in principle, but for blepharoplasty, combined anesthesia (local anesthesia with IV sedation) is quite sufficient, i.e. “There is no need to shoot sparrows from a cannon.” In other words, blepharoplasty is possible under ETN, but the method of choice is combined anesthesia.
Some, even colleagues, say: “What are you writing about “understaffed clinics”, there are no such clinics now!” I'd like to believe it. But, despite the 21st century, almost the first 20 years, there are often “clinics” in which everything is fine on paper and on the website, but in reality they have semi-working equipment, decommissioned from city hospitals, there is no license for potent and narcotic substances, doctors coming, leaving, etc. and so on. And then we see and hear on the news about a patient who went for surgery and did not return.
I strongly recommend that you carefully choose doctors and clinics, check everything, starting with licenses, but not only for surgical activities, but also for potent drugs and narcotic drugs. And then YOU will definitely have the “best anesthesia”!
Author:
Anesthesiologist-resuscitator M. V. Bakaushin