Antiparkinsonian drugs are medications that are used to treat Parkinson's disease. In addition, these drugs are used in the treatment of parkinsonism syndrome.
Parkinson's disease (shaking palsy) is a common chronic disease of the nervous system associated with damage to special areas of the brain responsible for muscle tone, maintaining posture and coordination of movements. Parkinson's disease has a genetic predisposition and manifests itself mainly in old age.
Parkinson's disease should be distinguished from parkinsonism syndrome, which occurs as a side effect when using certain groups of drugs, or due to infectious diseases of the brain (encephalitis), skull injuries, vascular diseases of the brain, syphilitic brain lesions, poisoning with alcohol and its surrogates, carbon monoxide gas, manganese salts, pesticides. Parkinsonism syndrome often develops in heroin addicts.
The manifestations of Parkinson's disease and parkinsonism syndrome are the same. These are stiffness of movements (bradykinesia), increased muscle tone (rididity), trembling (tremor) of the hands and head, and impaired posture. In patients, facial expressions decrease, the face becomes like a mask (hypomimia), and handwriting changes (micrography).
In addition, more than half of patients develop depression, memory (dementia) and intelligence decrease, mental activity slows down (bradyphrenia), sleep disturbances are observed, and the secretion of saliva and sweat increases.
pharmachologic effect
Parkinson's disease and parkinsonism syndrome are associated with disruption of the structure or function of dopaminergic neurons (nerve cells that use dopamine as an impulse transmitter) in certain areas of the brain - the substantia nigra, caudate nucleus and putamen. A decrease in the amount of dopamine leads to an increase in the influence of acetylcholine and glutamate, which are responsible for the development of characteristic symptoms of the disease.
Antiparkinsonian drugs can replenish dopamine deficiency in the brain, perform the functions of dopamine, or block the actions of acetylcholine and glutamate.
Development of addiction
The occasional use of cyclodol gradually changes to its systematic use up to 1-3 times a week. After 3-6 months, mental dependence syndrome develops.
Periodic mood swings occur that coincide with the rhythm of anesthesia, a feeling of mental discomfort, dissatisfaction, irritability, decreased mood in the absence of the drug and the impossibility of its immediate use. Thoughts about the need for intoxication become dominant and obsessive. Patients stop useful activities, leave work or study, and resort to various tricks in order to purchase cyclodol.
Tolerance gradually increases, the euphoric effect is achieved with increasingly higher doses, which can reach 60 mg per dose. A year or more after the onset of abuse of antiparkinsonian drugs, physical dependence develops. Autonomic disorders become permanent. Typical bright red cheeks against the background of general pallor of the skin of the face, bright red lips, isolated muscle twitching, dyspeptic disorders.
Up
Classification of antiparkinsonian drugs
According to the mechanism of action, antiparkinsonian drugs are classified into:
Drugs that stimulate the dopaminergic system of the brain
- Dopamine precursor – DOPA (levodopa): with DOPA decarboxylase inhibitor (levodopa + carbidopa, levodopa + benserazide)
- with DOPA decarboxylase inhibitor and catechol-O-methyltransferase inhibitor (levodopa + carbidopa + entacapone)
Drugs that inhibit the cholinergic system of the brain
- central anticholinergic agents (trihexyphenidyl, biperiden)
Parkinson's Disease Treatment Basics
Treatment of Parkinson's disease is mainly symptomatic. However, antiparkinsonian drugs cannot prevent the development of the disease.
The choice of drug depends on the stage of the disease, the prevailing symptoms, concomitant diseases in the patient, and tolerability of the drug.
Treatment begins with one drug (monotherapy) at a low dose. In the early stages of the disease, levodopa with a DOPA decarboxylase inhibitor is used, MAO type B inhibitors are drugs that stimulate dopamine receptors.
If treatment with one drug is ineffective, first gradually increase its dose. If it doesn’t help, use a drug from a different group. Another option is to use two drugs with different mechanisms of action. In elderly patients, drug metabolism slows down, so it is recommended to use all drugs in small doses.
A prerequisite for the treatment of parkinsonism syndrome is to eliminate the cause of the underlying disease.
MODERN PRINCIPLES OF TREATMENT OF PARKINSONISM
Parkinsonism is a syndrome involving the extrapyramidal system, whose pathogenesis is associated with progressive degeneration of nigrostriatal neurons, leading to reductions in the synthesis of dopamine and in the activity of dopamine systems and to a relative or absolute increase in the activity of cholinergic systems. Cholinolytic drugs, aminoadamantane derivatives, DOPA-containing agents, monoamine oxidase B inhibitors, catechol-o-methyl-transferase inhibitors, and dopamine receptor agonists are used as antiparkinsonian agents. Stereotoxic destructive surgery should be resorted to if only drug-resistant tremor and rigidity are prevalent and if drug therapy causes significant adverse reactions. Intracerebral grafting of dopamine neurons of the human embryonal mesencephalon provides certain prospects.
V.N.
Shtok, N.V. Fedorov Russian Medical Academy of Postgraduate Education, Center for Extrapyramidal Diseases of the Nervous System of the Ministry of Health of the Russian Federation, Clinical Hospital named after. S.P. Botkina VN Shtok, NV Fedorova Russian Medical Academy of Postgraduate Training, Center for Exprapyramidal Diseases of the Nervous System, Ministry of Health of the Russian Federation, SPBotkin Clinical Hospital
P
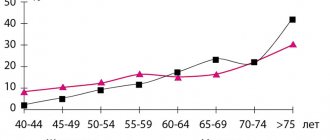
Arkinsonism is a syndrome of damage to the extrapyramidal nervous system, characterized by a combination of tremors, extrapyramidal muscle rigidity with the “cogwheel” symptom and akinesia. As the disease progresses, a fourth symptom appears – postural instability. There are Parkinson's disease, secondary parkinsonism (vascular, drug-induced, post-traumatic, post-encephalitic, etc.) and parkinsonism syndrome in degenerative and hereditary diseases of the central nervous system (strionigral degeneration, progressive supranuclear palsy, olivopontocerebellar atrophy, idiopathic orthostatic hypotension, Alzheimer's and Pick's diseases, hepatocerebral degeneration, Huntington's chorea, familial calcification of the basal ganglia, etc.). Despite the different etiologies of these diseases, the pathogenesis of clinical symptoms is similar and is associated with the progressive degeneration of nigrostriatal neurons, as a result of which the synthesis of dopamine and the activity of dopaminergic systems are reduced, while the activity of cholinergic systems is relatively or absolutely increased. All main approaches to pharmacotherapy for parkinsonism are aimed at correcting this imbalance of neurotransmitters that ensure the activity of the extrapyramidal nervous system.
Table 1. Anticholinergic drugs and aminoadamantane derivatives
| Anticholinergics | Content of active substance in 1 tablet, g | Aminoadamantane derivatives | Content of active substance in 1 tablet, g |
| Trihexyphenidyl | 0,001 – 0,002 – 0,005 | Amantadine hydrochloride | 0,1 |
| Biperiden | 0,002 | Midantan glucuronide | 0,2 |
| Triperiden | 0,002 | ||
| Benactizine | 0,002 | ||
| Arpenaium | 0,05 | ||
| Aprophenum | 0,025 | ||
Antiparkinsonian drugs (APDs)
For the pharmacotherapy of parkinsonism, anticholinergic drugs, aminoadamantane derivatives, DOPA-containing drugs (DCS), monoamine oxidase (MAO) type B inhibitors, catechol-O-methyltransferase inhibitors (COMT) and dopamine receptor agonists (DRA) are used. Individual sensitivity to PPS is variable. The threshold for the effect of PPS is determined by the minimum dose of one PPS that reduces the manifestations of parkinsonism. All PPPs can have side effects. The threshold for side effects is determined by the dose of the drug that causes the adverse reactions. The “gap” between these thresholds determines the boundaries of the pharmacotherapeutic window, or the optimal individual dose of each PPS.
The general rule when prescribing any PPS is to start treatment with a subeffective dose and then increase it very slowly (on average over 1 - 1.5 months) to select a dose that gives the minimum effect (effect threshold dose). The need for this approach is explained by the fact that as the disease progresses, the dose threshold for the effect increases, and the threshold dose causing adverse reactions decreases, that is, the boundaries of the pharmacotherapeutic window narrow.
Table 2. DOPA-containing drugs
| I. Preparations containing only levodopa | |||||||||
| Levodopa | 1 tablet/capsule – 0.25 or 0.5 g | Maximum daily dose – 3.0 g | |||||||
| II. Preparations containing levodopa in combination with a peripheral DDC inhibitor | |||||||||
| A drug | Levodopa content, mg | Inhibitor content, mg | Levodopa/DDC inhibitor | Maximum daily dose, mg (tablets) | |||||
| Pills: | |||||||||
| sinemet nakom | 250 | 25 | 10 : 1 | 750 (3) | |||||
| Capsules: | |||||||||
| madopar-125 | 100 | 25 | 4 : 1 | 7 capsules | |||||
| madopar-250 | 200 | 50 | 4 : 1 | 3 capsules | |||||
| Pills: | |||||||||
| Tidomet LS | 100 | 10 | 10 : 1 | 700 (7) | |||||
| Tidomet Plus | 100 | 25 | 1 : 1 | 700 (7) | |||||
| Tidomet Forte | 250 | 25 | 10 : 1 | 750 (3) | |||||
| III. Long-acting preparations containing levodopa and a DDC inhibitor | |||||||||
| Capsules: | |||||||||
| Madopar HBS | 100 | 25 | 4 : 1900 (9) | ||||||
| Pills: | |||||||||
| sinemet CR | 200 | 50 | 4 : 1900 (4, 5) | ||||||
| com R | 200 | 50 | 4 : 1900 (4, 5) | ||||||
Treatment with anticholinergic drugs
Anticholinergic drugs for parkinsonism stop the relative or absolute increase in the activity of cholinergic systems. Despite the fact that various drugs in this group are analogues (Table 1), in practice there is often a predominant individual sensitivity of patients to one of them. In order to identify individual sensitivity at the beginning of treatment, every 3 to 4 months one anticholinergic drug is replaced by another. In the future, the most effective drug is prescribed for continuous use, replacing it 1-2 times a year for a period of 1 month with another anticholinergic drug to avoid possible addiction. If doubts arise about the effectiveness of the anticholinergic drug, it is canceled. Worsening of parkinsonian symptoms after sudden discontinuation indicates that the prescribed treatment was effective, and then the drugs are resumed. Anticholinergic drugs are contraindicated in glaucoma and prostate adenoma. Side effects such as dry mouth and blurred vision indicate an individual overdose and require adjustment of the single and daily dose. Due to the unfavorable effect on cognitive functions, treatment with anticholinergic drugs is not started in the elderly and senile, as well as in patients with dementia.
Table 3. MAO type B inhibitors and COMT inhibitors
| Drugs | Dose, mg/day | |
| regular | maximum | |
| MAO type B inhibitors: | ||
| Selegiline (5 mg tablets) | 10 – 15 | 40 |
| COMT inhibitors: | ||
| Tolcapon | 100 – 200 | 400 |
| Entacapon | 200 – 800 | 2000 |
Table 4. Dopamine receptor agonists
| Drugs | Active substance content, mg | Daily dose, mg |
| Bromocriptin: | ||
| pills | 2,5 | 15 – 25 |
| capsules | 5 or 10 | |
| Pinbedil, tablets | 0,025 | 2,5 |
| Lisuride, tablets | 0,025 | 2,5 |
| Pergolide, tablets | 0,05, 0,25, 1 | 0,75 – 5 |
Treatment with aminoadamantane derivatives
Drugs of this class have anticholinergic properties and improve the circulation of dopamine in dopaminergic synapses. Analogs of amantadine hydrochloride (see Table 1) are prescribed 2–3 times a day, 1 tablet (0.1 g). More often, these drugs are added to anticholinergic drugs or DSS when their effect decreases, but they can also be used as a means of initial therapy. As a rule, a half dose (0.05 g) is first prescribed 2–3 times a day, and then gradually over 3–4 weeks it is increased to the average daily dose (0.3 g). Side effects during treatment with amantadine include anxiety, non-systemic dizziness, the appearance of a “marbled” coloration of the skin of the distal extremities, swelling of the legs, and visual illusions. Midantan glucuronide - gludantan (0.2 g) is inferior in pharmacotherapeutic activity to amantadine hydrochloride, but is less likely to cause side effects.
Rice. 2. The effect of ADR on presynaptic defamine and postsynaptic receptors.
EDA-endogenous dopamine; DA from LD-dopamine from taken levodopa; 1-postsynaptic dopamine receptor; 2-presynaptic dopamine receptor.
Treatment with “pure” levodopa
Since dopamine, like other catecholamines, does not pass through the blood-brain barrier (BBB), the metabolic precursor of dopamine, levodopa (L-dioxyphenylalanine), is used for replacement therapy, which passes through the BBB and is converted in dopaminergic neurons under the influence of cerebral DOPA decarboxylase (DDC). into dopamine. The metabolism of levodopa under the influence of DDC and the catabolism of dopamine under the influence of MAO type B and COMT are presented in the diagram (Fig. 3). Preparations of “pure” levodopa (Table 2) contain 0.25 or 0.5 g of active substance. Treatment with levodopa can serve as an addition to combination therapy with anticholinergic drugs, amantadine or ADR, or used as monotherapy at the beginning of treatment of parkinsonism. Treatment begins with a subthreshold dose (125 mg of levodopa) and gradually, over 1.5–2 months, increases the dose until the effect occurs. With a rapid increase in the individual dose, the risk of early onset of side effects from the gastrointestinal tract and cardiovascular system increases. This is due to the fact that “premature” decarboxylation of levodopa occurs in the gastrointestinal tract and bloodstream with the formation of not only dopamine, but also norepinephrine and adrenaline. In 50–60% of cases, this leads to nausea, vomiting, intestinal dyskinesia, heart rhythm disturbances, angina pectoris and fluctuations in blood pressure. Therefore, the administration of “pure” levodopa is undesirable for diseases of the gastrointestinal tract, coronary heart disease with rhythm disturbances, and angina pectoris.
The daily dose of levodopa should not exceed 3 g, but even with long-term treatment this dose causes adverse reactions. Up to 80% of ingested levodopa undergoes “premature” decarboxylation, and only 1/5 of the ingested dose reaches the brain and is metabolized by the cerebral DDC to form dopamine, as well as norepinephrine and adrenaline. If the level of catecholamines formed in the brain exceeds the threshold of side effects, then neurological (dystonia and dyskinesia) and mental (hallucinations, agitation, delirium, confusion) adverse reactions appear. These manifestations require dose reduction and sometimes drug discontinuation.
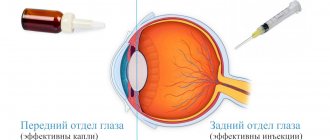
Treatment with levodopa in combination with peripheral DDC inhibitors
Preparations containing levodopa with a peripheral DDC inhibitor, carbidopa or benserazide, are presented in Table. 2. Peripheral DDC inhibitors inhibit the premature decarboxylation of levodopa in the gastrointestinal tract and bloodstream (Fig. 1). The ratio of the amount of levodopa and DDC inhibitor in different drugs is different (see Table 2). The higher the inhibitor content, the lower the risk of side effects from the gastrointestinal tract and cardiovascular system. When taking levodopa drugs with a DDC inhibitor, the incidence of cardiovascular and gastroenterological complications is reduced to 4–6%. At the same time, inhibition of “premature” decarboxylation increases the delivery of the administered dose of levodopa through the BBB into the brain by 5 times. Therefore, when replacing “pure” levodopa with drugs with a DDC inhibitor, a 5 times smaller dose of levodopa is prescribed (in terms of “pure” levodopa. For example, if the patient took 3 g of “pure” levodopa per day, then the amount of levodopa per day in the composition of drugs with peripheral DDC inhibitor should be 5 times less (3000 mg: 5 = 600 mg) and will be approximately 2.5 tablets of Nakoma or Sinemet (625 mg levodopa), or 6 capsules of Madopar-125, or 3 capsules of Madopar-250 (600 mg levodopa).If levodopa preparations with an inhibitor are prescribed as initial therapy, then treatment begins with subthreshold doses (for example, 1/4 tablet of Sinemet or Nakoma 2 times a day) with a gradual increase in dose over 3 to 5 weeks. Since the inhibitor of peripheral DDC does not pass through the BBB and does not affect the formation of dopamine, norepinephrine and adrenaline in the brain, the risk of neurological and mental side symptoms remains the same as when taking “pure" levodopa. Therefore, the daily dose of the drug with a DDC inhibitor in most cases should not exceed 750 mg levodopa. The use of vitamin B6 in combination with “pure” levodopa is inappropriate, while at the same time, when treating with levodopa preparations containing a DDC inhibitor, the administration of vitamin B6 is possible.
Clinical pathomorphosis of parkinsonism during long-term course of the disease and treatment of DSS
With rational selection of the optimal individual dose, the pronounced pharmacotherapeutic effect of DSS without the appearance of adverse reactions usually persists for 4–7 years, after which, even when taking the usual optimal dose, various adverse reactions and changes in the typical clinical picture of parkinsonism (clinical pathomorphosis) with the appearance of a number of phenomena are noted. The phenomenon of attrition of the effect of a single dose is due to a shortening of the duration of action of drugs. The effect of the drugs is significantly reduced and even disappears after short periods of time after taking levodopa (for example, after 2 - 3 hours), resulting in the resumption of symptoms of the disease. Such changes in motor activity are usually clearly related to the timing of drug administration and are defined as simple motor fluctuations. The “on-off” phenomenon is that the effect of the next single dose of levodopa after a certain time after taking the medication (30-60 minutes) occurs very quickly - within 5-15 minutes (“on”) lasts 1-1.5 hours and disappears just as quickly (“turning off”). When turned on quickly, the state can change from almost complete immobility to almost complete relaxation. Significant fluctuations in physical activity throughout the day do not necessarily occur suddenly and are not always clearly related to medication use. The effect of a single dose becomes insufficient, delayed in time, and sometimes the next dose may not give a therapeutic effect at all. Such unpredictable fluctuations in motor activity are called “complex motor fluctuations.” The phenomenon of “freezing” is manifested by a state of sudden paroxysmal akinesia. There are akinesia of the onset of movement (starting difficulties in movement), “akinesia of turning”, “akinesia of the threshold”. Akinesia is often accompanied by tramping or postural instability.
Pharmacological approaches to correcting the manifestations of motor fluctuations
If manifestations of clinical pathomorphosis occur at a certain time after taking DSS, then their reduction can be achieved by changing the frequency of administration, the size of any single dose in the morning, afternoon or evening. However, the possibilities of this approach are limited. Pharmacological correction using long-acting DSS, MAO type B inhibitors, and dopamine receptor agonists turned out to be more effective.
Long-acting DSS (DSPD)
The manufacturing technology of DSSPD ensures gradual release and, consequently, absorption of levodopa and DDC inhibitor from an orally taken tablet (sinemet CR, nacom R) or capsule (madopar HBS; see Table 2). When taking these drugs, a more stable level of drug concentration in the blood and a more uniform synthesis of dopamine from drugs in the brain makes it possible to reduce the severity of simple and complex motor fluctuations, reduces the frequency and degree of drug dyskinesias that occur when taking non-extended-release DSS. The bioavailability of sinemet CR and madopar HBS is less than the bioavailability of traditional drugs (sinemet and madopar). Therefore, in the case of replacing traditional DSS with long-acting drugs, the dose of levodopa to obtain the same antiparkinsonian effect can be increased by 20–30%. When taking DSSPD, the frequency of administration during the day can be reduced. If these drugs are used at the beginning of treatment of patients with parkinsonism (at the initial stage), a uniform pharmacotherapeutic effect can sometimes be obtained by taking the drugs 1 - 2 times a day.
MAO type B inhibitors
MAO type B inhibitors (Table 3) prevent the metabolic degradation of available dopamine formed during endogenous synthesis from the drug levodopa. Thanks to this, a higher and more stable level of available dopamine is maintained, the manifestations of the phenomenon of dose depletion, on-off switching and other manifestations of motor fluctuations are smoothed out. In most cases, to achieve the indicated effect, which, however, is never significantly pronounced, it is enough to take selegiline 5 mg 2 - 3 times a day. Some authors consider a dose of 40 mg/day necessary.
COMT inhibitors
COMT naturally metabolizes L-DOPA into 3-0-methyldopa and dopamine into 3-0-methyldopamine. These products are not involved in the function of dopamine neurons. COMT inhibitors interfere with the metabolism of dopamine and its precursor. A COMT inhibitor that does not cross the BBB and therefore metabolizes levodopa in the “periphery” is entacapone, and an inhibitor that passes the BBB, i.e., acting both “in the periphery” and in the brain, is tolcapone (Table 3). The addition of tolcapone to DSS increases and prolongs steady-state plasma levodopa levels by 65%. The addition of COMT inhibitors increases pharmacotherapeutic efficacy and corrects motor fluctuations in 83% of cases more often than the addition of ADRs (69% of cases).
Dopamine receptor agonists
Unlike all the drugs mentioned above, ADRs (Table 4) are able to act directly on postsynaptic dopamine receptors, “bypassing” the degenerated dopaminergic neuron. The corrective effect of ADR on the manifestations of clinical pathomorphosis is based on a combination of a stimulating effect on postsynaptic receptors and a modulating effect on the function of the presynaptic dopaminergic neuron (Fig. 2). Piribedil (both D1 and D2 receptor agonist) was more effective than bromocriptine (D2 receptor agonist) when prescribed as monotherapy and when added to DSS.
The use of drugs that correct clinical pathomorphosis as initial therapy
In recent years, drugs that correct pathomorphosis have been proposed for the initial treatment of parkinsonism. The tactics for selecting the individual optimal dose are the same as for other PPPs. Experience shows that only DSSPD can be compared with traditional DSS in terms of efficiency. The drugs selegiline and ADR have a much lower potential for antiparkinsonian effect. One of the reasons for using MAO type B inhibitors as initial pharmacotherapy is the assumption that increased lipid peroxidation contributes to the degeneration of nigrostriatal neurons in parkinsonism. The multicenter study “Antioxidant Therapy with Deprenyl and Tocopherol in Parkinsonism” (DATATOR), which used selegiline (10 mg per day) and tocopherol (2000 IU per day), showed a slowdown in the progression of parkinsonism. However, the hypothesis about the effectiveness of antioxidants in the treatment of parkinsonism cannot be considered proven.
Neurosurgical treatment of parkinsonism
One of the methods for treating parkinsonism is neurosurgical operations: stereotactic methods (destruction or stimulation of certain structures of the basal ganglia) and intracerebral transplantation of embryonic tissue and human mesencephalon into subcortical structures. Indications for stereotactic destructive operations (ventrolateral thalamotomy, pallidotomy, thalamo-subthalamotomy, etc.) are clinical forms of parkinsonism with a significant one-sided predominance of tremor and rigidity (hemiparkinsonism), which are not amenable to pharmacotherapy, as well as the presence of adverse reactions when prescribing PPS. Stereotactic stimulation - chronic electrical stimulation of subcortical structures through implanted electrodes - is carried out to inhibit tremor and rigidity. It can be combined with ventrolateral thalamotomy. Intracerebral transplantation of dopaminergic neurons of the mesencephalon of a human embryo remains to this day a clinical experimental operation, the effectiveness of which continues to be studied. Implanted embryonic mesencephalon neurons either produce dopamine themselves or help increase the synthesis of the neurotransmitter from levodopa taken by the patient. Intracerebral transplantation does not lead to complete disappearance of the symptoms of the disease, but significantly improves the prospects for subsequent pharmacotherapy: in patients, the duration of action of a single dose of DSS increases, the severity of drug dyskinesias decreases, and in some cases it is possible to reduce the daily dose of PPS.
Literature:
1. Hoehn M, Jahr MD. Parkinsonism: onset, progression and mortality. Neurology 1967;17(5):427–42. 2. Koller WC. Classification of Parkinsonism. Handbook of Parkinsons disease (Ed. by W. C. Koller). Marcel Dekker. New York-Basel 1987;99–126. 3. Marsden CD, Parkes JD, Quinn N. Fluctuation of disability in Parkinsons disease; clinical aspects. Movement disorders (Ed. C. D. Marsden, S. Fahn). London, Butterwoth 1982;96–119. 4. Mouradian MM. Control-release oral levodopa therapy for Parkinson's disease. Parkinsons disease review 1991;1–7. 5. Obeso JA, Granadas F, Vaamonde J, et al. Motor complications associated with chronic levodopa therapy in Parkinsons disease. Neurology 1989;39(11;Suppl.2):11–8. 6. Olanow CW. Protective therapy for Parkinson's disease. The scientific basis for the treatment of Parkinson's disease (Ed. by C. W. Olanow and A. N. Lieberman). The Parthenon Publishing Group 1992;225–56.
Features of the treatment of Parkinson's disease
Parkinson's disease is a chronic disease that requires lifelong treatment. When addiction develops (a decrease in the effect of the drug with prolonged use), the drug is changed to a drug with a different mechanism of action.
During treatment, patients are advised to maintain adequate physical activity and engage in physical therapy.
Concomitant depression in patients is treated with antidepressant drugs, memory disorders are treated with nootropics (drugs to improve memory and mental activity).
Acute intoxication with cyclodol (table)
There are four phases of cyclodol intoxication: euphoric, stunned or constricted consciousness, hallucinatory and the phase of recovery from the state of intoxication:
Phases of cyclodol intoxication (table)
| Phase | Main manifestations |
| First phase | Euphoric phase. Develops 20-25 minutes after taking the drug. It manifests itself as a feeling of warmth, especially in the limbs, a general pleasant feeling, and moments of ecstatic experience. Sounds are clear and colors are vibrant. Everyday troubles recede into the background, mood improves, and euphoria with a motor component is observed. The patient talks a lot and laughs. The phase lasts 30-40 minutes. |
| Second phase | Stun phase. Severe lethargy appears, a desire to take a reclining position and calmly feel pleasant warmth and at the same time cold, flight, weightlessness. At this time, the drug addict observes himself as if from the outside, in an unusual environment; objects in the surrounding world change shape and features. There is a feeling that the environment is constantly changing. Thoughts float sluggishly, words are difficult to find, and sometimes there are breaks in thinking. The duration of this phase can be 2-3 hours. |
| Third phase | Hallucinatory phase. Occurs when taking a sufficiently high dose of the drug. Deeper changes in consciousness occur. There is disorientation in time, environment, and self. At first, the drug addict feels elementary deceptions of perception - ringing, crackling, individual sounds, then hallucinatory images appear. They are dynamic and can be visual or auditory. When leaving this state, all experiences that are considered the most significant in the picture of intoxication are remembered. When describing hallucinatory experiences, a substance abuser differentiates them well from the real situation. The duration of the phase is 2-3 hours. |
| Fourth phase | The phase of recovery from intoxication. Characterized by distinct general asthenia. |
The presence of illusory and hallucinatory experiences does not cause gross disorientation in the environment. The experience of intoxication leaves drug addicts with pleasant memories and a desire to repeat intoxication.
Up