Antiepileptic drugs are medications used for epilepsy to prevent or treat epileptic seizures. In addition, these drugs are used to prevent or treat seizures that occur due to other diseases. Therefore, they are also called anticonvulsants.
Epilepsy is a common chronic disease of the nervous system, which usually manifests itself as repeated seizures - convulsions. Epileptic seizures are generalized (spread to both hemispheres of the brain) and partial (occur in a strictly defined area of the brain).
The development of seizures is preceded by an aura - nausea, weakness, dizziness, speech impairment, numbness of the lips, tongue, loss of consciousness. Next, convulsions occur directly: tonic (the body and limbs are stretched in a state of tension, the jaws are clenched, and breathing is held) and clonic (contraction of the muscles of the limbs, neck, and torso).
Sometimes convulsions are manifested by individual muscle twitching without loss of consciousness (myoclonus), sudden short-term freezing, lack of reaction (absence).
Epilepsy usually occurs in childhood and most often the cause cannot be determined. Heredity, intrauterine oxygen deprivation of the fetus during pregnancy, and birth injuries play a certain role in the development of epilepsy.
Seizures can also be a symptom of other diseases or conditions that occur at any age. Thus, seizures can occur with head injuries, hemorrhage in the brain, intracranial tumors, pregnancy, oxygen starvation, metabolic disorders, overdose of substances that affect the nervous system (including alcohol).
Indications for use
All antiepileptic drugs are used to treat epilepsy, as well as symptomatic seizures in other diseases of the nervous system.
Certain drugs (carbamazepine, gabapentin, pregabalin) are also used to treat neuralgia and neurogenic pain (associated with nerve damage).
Lamotrigine, carbamazepine, oxcarbazepine, and valproic acid are additionally used to normalize mood in patients with bipolar affective disorder, which is characterized by alternating periods of manic agitation and depression.
pharmachologic effect
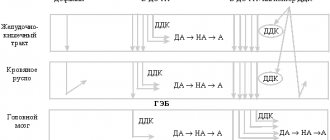
Convulsions occur when the balance between excitation and inhibition in the brain is disturbed in the direction of excitation. Mediators (signal transmitters between neurons) are responsible for this balance:
- inhibitory – gamma-aminobutyric acid (GABA), glycine;
- stimulating – amino acids glutamate, aspartate.
In addition, sodium and calcium channels of neurons play a huge role in the generalization (spread) of excitation. Antiepileptic drugs affect one or more mechanisms maintaining the balance of excitation and inhibition in the brain.
Approaches to taking anticonvulsants
If previously the main goal of treating epilepsy and taking anticonvulsants was to prevent new seizures, today an integrated approach takes first place, taking into account the patient’s quality of life and maintaining his ability to work during treatment
Finding effective therapy can be difficult. This is influenced by factors such as compliance with medication regimen and side effects. Changing drugs by trade name, but with the same active ingredient, can also lead to worsening problems.
Typically, one drug is used at the beginning of treatment for epilepsy, but the dosage and medication may vary. If the desired result is not achieved, only then connect a second remedy and use various combinations.
Finding effective therapy can sometimes be difficult.
Anticonvulsants
There are 3 main mechanisms used to treat epilepsy:
- Stabilization of the membrane potential of nerve cells due to the influence on ion channels. Due to this, K+ ions remain in the cell, and Na+ ions outside. The effect can also be exerted through Ca2+ channels. This maintains “rest” on the membrane of nerve cells.
- Suppression of processes involved in excitation.
- Strengthening braking mechanisms.
Many drugs act on several mechanisms at once and it will not be possible to divide them into groups on this basis.
Medicines:
Depakine Chronosphere , Convulex , Encorat chrono . Valproic acid preparations. They have a muscle relaxant effect and enhance inhibitory processes in the brain. Absorption of the drug may slow down when taken with food. Side effects include : weight gain, hair loss, gastrointestinal problems, tremors.
Finlepsin retard , Tegretol CR , Carbatol. They belong to carbamazepine drugs and are used for grand mal seizures and mixed forms of epilepsy. Contraindications: absence and myoclonic seizures. Side effects: dizziness, drowsiness, headache, but stopping treatment often causes a skin rash.
Phenobarbital , Benzonal , Maysolin . They belong to the group of barbiturates. Can be used for any type of epilepsy attack. Often used in infants. There is a marked slowdown in mental processes. Children have the opposite reaction and develop hyperreactivity. They reduce motor activity and can cause drowsiness. The anticonvulsant effect is realized by preventing the occurrence and propagation of an impulse from the source of activity. The absence form of idiopathic epilepsy will be a contraindication for use.
Frisium , Relanium , Merlit. They belong to the group of benzodiazepines. They are especially often used for progressive myoclonic epilepsy. But over time, the effect may decrease and addiction may develop .
Lamictal , Pamolen. The active ingredient is lamotrigine. It is effective for all types of seizures, but it is recommended to avoid it for myoclonus. The main side effect is a rash, the severity of which increases sharply when combined with valproate and carbamazepine.
Topamax (topiramate). Acts on different mechanisms in preventing attacks, effective in adults and children. Start taking with minimal doses and increase slowly. Use with caution in children with speech disorders, as well as sleep problems. One of the side effects is weight loss, so it should not be used in “thin” patients.
Keppra , Levetinol . The active ingredient is levetiracetam. Optimal action for epileptic myoclonus, does not interact with other drugs. Should not be used in patients prone to agitation and sleep disturbances.
Suxilep. Previously it was the drug of choice for the treatment of absence seizures, but has now given way to valproic acid. Contraindicated for mental problems. Side effects: headache, drowsiness, gastrointestinal symptoms.
Tebantin , Neurontin , Gabapentin . Structurally similar to GABA, they are not transformed in the liver, so they can be used with many other drugs and for liver diseases. Side effects: weakness, dizziness, weight gain.
Since the treatment of epilepsy in many cases involves lifelong use of drugs, the balance between their effectiveness and toxicity is important. Drug metabolism pathways (in the liver) and interactions with other drugs in concomitant diseases also play a role. The selection of anticonvulsant drug therapy is a joint effort between the doctor and the patient.
Classification of antiepileptic drugs
There are several classifications of antiepileptic drugs: according to the characteristics of use in different forms of epilepsy - types of paroxysms, according to the mechanism of action, as well as the chemical structure of the drugs.
According to the mechanism of action, the following groups of antiepileptic drugs are distinguished:
Sodium channel blockers
- Hydantoin derivatives (phenytoin)
- Carboxamide derivatives (carbamazepine, oxcarbazepine, eslicarbazepine acetate)
- Others (lamotrigine, lacosamide)
Calcium channel blockers
- Succinimide derivatives (ethosuximide)
- Others (pregabalin)
Agents that enhance the inhibitory effects of GABA
- Barbiturates (phenobarbital, benzobarbital)
- Benzodiazepines (diazepam, clonazepam, lorazepam)
- Others (vigabatrin, gabapentin, tiagabine)
Agents that inhibit the action of excitatory amino acids
- Felbamate
Combination agents
- Fatty acid derivatives (valproic acid and its salts - valproates)
- Others (topiramate)
According to the characteristics of their use in different forms of epilepsy, antiepileptic drugs are divided into:
- Drugs used for partial seizures: valproate, carbamazepine, lamotrigine, vigabatrin, gabapentin, phenobarbital, clonazepam, phenytoin.
- Drugs used for generalized seizures:
- for grand mal seizures - valproate, carbamazepine, phenobarbital, phenytoin, lamotrigine;
- for small convulsive seizures (absences) - ethosuximide, valproate.
In addition to the drugs listed in the classification, seizures can be eliminated or prevented by magnesium preparations (magnesium sulfate) when administered intravenously, anesthetics (sodium hydroxybutyrate, sodium thiopental).
Institute of Child Neurology and Epilepsy
Even in the second half of the last, 20th century, epilepsy was considered an incurable disease. The development of neuropharmacology in recent decades, the synthesis of new highly effective antiepileptic drugs (AEDs), a radical revision of many principles of its treatment - all this has now made it possible to classify epilepsy as a disease that can be treated. AEDs are chosen depending on the form of epilepsy and the nature of the attacks.
Treatment should begin with the drug of first choice for this form of epilepsy. The drug is usually prescribed in a small initial dose with a gradual increase until an optimal clinical effect occurs or initial signs of overdose occur. If the drug is ineffective, it is gradually discontinued and the next one is prescribed; however, you cannot immediately switch to a combination of drugs without using all the reserves of monotherapy.
Valproic acid preparations (Convulsofin, Depakine, etc.) are one of the most effective groups of AEDs.
Convulsofin is the calcium salt of valproic acid. This is a modern drug with a wide spectrum of action; it is highly effective in almost all forms of epilepsy and types of epileptic seizures. Currently, more than 20 years of experience in the use of valproates indicates that they are the drugs of absolute choice in the treatment of most forms of generalized and idiopathic partial epilepsy. It has now been proven that Convulsofin has a wide range of antiepileptic activity, both in relation to primary generalized seizures (generalized convulsive, myoclonic, absence seizures), and partial (simple and complex) and secondary generalized paroxysms. At the same time, Convulsofin is used as a basic drug as monotherapy and in combination with other AEDs in children and adults of all ages.
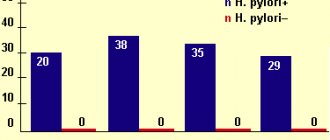
Dosages of Convulsofin are selected individually and vary over a wide range. The average dose can be 600-1500 mg/day (20-40 mg/kg/day). If necessary and in severe forms, significantly higher doses are used. Among the side effects (AE) of valproate, the most significant are the following: increased appetite and weight (rarely refusal to eat), heartburn, nausea, abdominal pain, mild hair loss, hand tremors. It is necessary to monitor the level of platelets in the blood (they may decrease). If PE occurs, you should consult your doctor; however, it is not always necessary to discontinue the drug.
Drugs of the carbamazepine group (Finlepsin, Finlepsin - retard, Tegretol) are also modern, highly effective AEDs. Finlepsin is the drug of choice in the treatment of symptomatic partial forms of epilepsy; with partial, primary and secondary generalized seizures. It is used both in monotherapy and as an additive drug. It should be remembered that carbamazepine drugs are contraindicated for absence seizures and myoclonic seizures. The average daily dose is 400-800 mg (about 20 mg/kg/day). Preference in treatment is given to prolonged forms, such as Finlepsin retard. Main adverse events: double vision, drowsiness, skin rash, headache, decreased level of leukocytes in the blood.
Ethosuximide (Suxilep). Suxilep is a narrow-spectrum drug. It is highly effective in absence and myoclonic seizures, both in monotherapy and in combination with valproate (Convulsofin). In some forms of epilepsy, for example, Lennox-Gastaut syndrome, Suxilep can only be used in combination with other AEDs. Average doses: 500-750 mg/day (about 20 mg/kg/day). PE: nausea, intestinal disorders, drowsiness. It is noteworthy that the drug passes into breast milk in large quantities. Women taking suxilep during lactation should avoid breastfeeding.
Topiramate (Topamax) is a broad-spectrum drug. Effective for all types of partial seizures, as well as generalized convulsive ones. It is used in the treatment of partial and generalized forms of epilepsy with the presence of convulsive attacks. Average doses: 5-7 mg/kg/day (200-400 mg/day). It is necessary to slowly increase the dose when administering the drug (usually over 6-10 weeks). AEs depend mainly on the dose of topiramate and are associated with dysfunction of the central nervous system: dizziness, fatigue, drowsiness, irritability, decreased concentration. These manifestations usually disappear soon after the next dose increase. Paresthesia (a crawling sensation) may also occur. To prevent the occurrence of kidney stones, patients should increase their daily fluid intake (alkaline mineral waters). The drug is contraindicated in patients with impaired renal function and kidney stone disease.
Benzodiazepines (clonazepam, antelepsin, clobazam, seduxen, radedorm, lorafen, etc.). Benzodiazepines are used only as adjunctive AEDs for resistant forms of epilepsy. Particularly effective for myoclonic and photosensitivity forms of epilepsy. Also prescribed for serial increases in attacks, as first aid medications. They have a wide range of adverse effects, primarily in relation to the central nervous system: pronounced sedation, impaired concentration, depression or agitation, unsteadiness, speech disorder, drooling, breathing problems in young children. It is strictly forbidden to abruptly discontinue benzodiazepines in patients with epilepsy - there is a threat of increased frequency of attacks and the development of epistatus.
“Old” AEDs: barbiturates (phenobarbital, hexamidine, benzonal) and hydantoins (difenin, phenytoin, difantoin). Effective in the treatment of generalized convulsive and partial seizures. Phenobarbital is used in a dose of 100-300 mg/day (2-5 mg/kg/day), and Diphenin - in a dose of 100-400 mg/day (3-8 mg/kg/day). In 1998, the European Commission on Antiepileptic Drugs recommended that doctors significantly narrow the indications for the use of these drugs in patients with epilepsy. The reason for this is the negative impact of these drugs on the central nervous system: lethargy, drowsiness, difficulty concentrating, hyperactivity, decreased learning ability, etc. Difenin is a teratogenic drug that often causes developmental defects in newborns. It is contraindicated for use during pregnancy.
New antiepileptic drugs include topiramate, lamotrigine, tiagabine, vigabatrin, felbamate, and levetiracetam.
It should be remembered that there are no universal drugs that would be highly effective in all cases, would not produce side effects (SE) and would be inexpensive. Prescribing a specific drug, selecting dosages, adding or removing AEDs should only be done by the attending physician. Failure to comply with recommendations and independent manipulation of medications can lead to serious consequences for patients, including the development of status epilepticus.
Epilepsy Treatment Basics
Antiepileptic drugs are prescribed only by a specialized specialist - a neurologist or psychiatrist - after a complete neurological examination of the patient. In this case, the type of epileptic seizures must be taken into account.
Antiepileptic drugs are usually prescribed after the second attack. The earlier treatment begins, the better and easier it is to control seizures.
Therapy is usually started with one drug (monotherapy). The effectiveness of treatment is assessed over 3 months. Ideally, the drug completely prevents seizures. In case of ineffectiveness, the drug is changed or a combination of two (less often three) drugs is used.
Epilepsy
Epileptic seizures that occur without any apparent reason two or more times can be considered epilepsy. An epileptic seizure is an abnormal or excessive discharge of neurons in the brain with visible manifestations. Visible manifestations are not always convulsions and loss of consciousness, they can be:
- only changes in consciousness;
- mental manifestations;
- motor changes;
- vegetative manifestations.
For a particular person, these symptoms can be in the form of ringing in the ears, flashes of light or flame, redness of the face, short-term disturbances in speech, memory and many others. It depends on where the nerve impulse went out of control and activated a particular area of the brain. Moreover, these changes may be first noticed by another person, and not by the patient himself. This can happen, for example, with episodes of freezing for a few seconds. If these symptoms have a clear cause, such as a head injury or a brain tumor, it is not epilepsy.
There are many forms of epilepsy depending on the type of epileptic seizures, types of epilepsy and status epilepticus (an epileptic seizure lasting more than 30 minutes at once or a series of seizures without full recovery of consciousness).
If the symptoms have a clear cause, then it is not epilepsy.
Features of epilepsy treatment
Epilepsy is a chronic disease that requires long-term, often lifelong, treatment. If epilepsy is not treated, the patient experiences behavioral disturbances, emotional disorders, and memory loss (epileptic dementia).
During treatment, patients are recommended to adhere to a normal sleep and rest schedule, a special diet high in fat and low in proteins and carbohydrates (ketogenic diet), and exclude alcohol, coffee, energy drinks and tobacco products from the diet.
Epilepsy drugs
Epileptic seizures occur when potassium leaves nerve cells at the same time calcium and sodium enter it. An impulse failure occurs, which provokes the release of neurotransmitters. Some activate the attack (glutamate), others inhibit it (GABA). Antiepileptic drugs are necessary in order to properly influence neurotransmitters and normalize the functioning of neurons.
AEDs are classified into different groups based on their mechanism of action:
- sodium and calcium blockers;
- glutamate blockers;
- GABA receptor stimulants;
- multiple action drugs.
There are also the following groups of drugs against epileptic seizures:
- anticonvulsants (anticonvulsants);
- sedatives (calming);
- vitamin complexes.
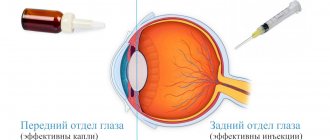
All medicines are produced in the form of tablets (capsules, granules), syrup (drops), powders for solution, injections. Each form of drugs has different bioavailability (rate of absorption into the blood):
- Solid (tablets, capsules). They can be slow or immediate. The former are used more often due to the absence of a sharp increase in the concentration of the active substance, which leads to its rapid decrease and reduction of the effect - this is how immediate-release tablets work. The delayed type is preferable due to the long-lasting effect, which allows you to minimize the number of medications taken.
- Soluble. The granules can be dissolved in water or yogurt - this method of consumption is well suited for small children or people with swallowing disorders.
- Liquid (drops, syrups). They are considered the most convenient for treating children and the elderly due to ease of use. Usually the packaging contains measuring devices (spoon, syringe).
- Injections. Indispensable in urgent situations due to its high bioavailability, when it is necessary to quickly relieve an acute attack. Most often used in hospitals or by emergency doctors.
Anticonvulsants
Anticonvulsants help prevent, reduce, or completely eliminate an epileptic seizure. Anticonvulsants block the excitation of nerve cells and activate GABA receptors, which inhibit excitation. Today doctors prescribe medications based on the following active ingredients:
- Sodium valproate. Increases the amount of GABA and stimulates its activity.
- Ethosuximide. Blocks calcium and sodium channels, weakens the effect of glutamate.
- Carbamazepine, phenytoin. Reduce the number of neurons in sodium channels, reduce the effects of amino acids and glutamate.
- Phenobarbital, primidone. Accelerate the activity of GABA receptors in calcium channels.
- Lamotrigine, oxcarbazepine, oxcarbazepine. They reduce the excitation of sodium neurons and inhibit glutamate activity.
- Levetiracetam, topiramate. They have multiple effects on nerve cells and neurotransmitters.
- Tiagabine. Blocks the attack of GABA by neurons, increases the concentration of beneficial neurotransmitters.
- Gabapentin. In addition to activating calming receptors, it relieves pain and tension.
Sedatives
Epileptics are often prescribed sedatives and sleeping pills - the active substances in tablets and injections help relieve stress, calm the nervous system and weaken the effect of impulses that provoke seizures. Usually prescribed:
- Valerian. Relaxes muscles, normalizes heart rate, suppresses attacks.
- Afobazol. It has a gentle effect on the nervous system and improves sleep.
- Relanium. Relieves anxiety, fears, overexcitement.
- Tenoten. Relieves psycho-emotional stress without atrophying muscles.
- Antidepressants. Prevents stress, panic and depression, which often cause seizures.
Other drugs
- Painkillers. An epileptic attack may be accompanied by pain in the head and muscles. Analgesics eliminate pain and additionally have an anti-inflammatory, vasodilating and calming effect.
- Hormonal. Most hormones in excess provoke an attack, but some of them (for example, dexamethasone) stop the transmission of impulses.
- Nootropic. They promote normal brain function while suppressing the activity of neurotransmitters.
Some doctors prescribe dietary supplements as a form of prevention and additional stimulation of the positive effect of drugs. It is not recommended to choose biological additives on your own - despite their plant origin, certain components can be harmful.
Vitamins and minerals for epilepsy
Vitamin and mineral complexes are especially necessary for young children or people following a ketogenic diet. With epilepsy, the patient has limited nutrition, which negatively affects physical and mental development. What vitamins and minerals restore the body’s functioning:
- B vitamins: For healthy metabolism and energy, the body needs folic acid, B6 and B12 - they eliminate drug resistance.
- Vitamin D. In epileptics, the liver actively produces enzymes that flush vitamin D from the body. Calcium deficiency threatens osteoporosis.
- Antioxidants. Taking medications reduces the amount of selenium, vitamins C and E, so the use of antioxidants is included in the medication course.
- Magnesium. Necessary for maintaining the balance of neurotransmitters, as well as for the inhibition of calcium channels.
- Melatonin. Inhibits excitatory receptors and glutamate, helps restore sleep and the biological rhythm of life, gives strength and energy.
- Omega-3. Fatty acids are essential for epilepsy due to their anticonvulsant effect. Large amounts of fat in the blood stimulate the production of ketones, which replace the stimulating glucose but are not harmful.