Sudden death
Definition
. Sudden cardiac death (SCD) is defined as: “natural death due to cardiac causes, characterized by sudden loss of consciousness within one hour of the onset of symptoms; the presence of heart disease may be known, but the timing and mechanism of death is unpredictable.” The key concepts guiding the definition of sudden death are that the cause is non-traumatic and that the onset of death is immediate and unpredictable. When considering the problem of sudden death within heart diseases, the word “cardiac” was introduced into the term.
Healthy foods for the heart
Proper nutrition is the key to health and longevity; support your body with heart-healthy foods.
- Red grape juice.
- Low-fat milk.
- Fresh vegetables and fruits (legumes, bananas, carrots, pumpkin, beets, etc.).
- Sea fish.
- Lean meat (chicken, turkey, rabbit).
- Nuts.
- Vegetable oils.
A healthy lifestyle is the answer to the question, how to avoid sudden death?
There are many diets designed to strengthen and maintain good heart condition. Regular exercise will strengthen the body and make you feel more confident and healthier.
Active lifestyle and physical culture
Regular dosed physical activity with an emphasis on “cardio training”:
- Running in the fresh air.
- Bicycle rides.
- Swimming.
- Cross-country skiing and skating.
- Yoga class.
- Morning exercises.
Causes
Epidemiology
. One of the leading causes of death in the adult population of developed countries is SCD due to coronary heart disease. In patients with sudden cardiovascular collapse, the rhythm of ventricular fibrillation is most often determined on the ECG (in 75-80% of cases), while bradyarrhythmias are the cause of SCD in a minimal number of patients. In 5-10% of cases of sudden cardiac death, patients do not have coronary heart disease or congestive heart failure. According to statistical data obtained annually in Western countries, the incidence of SCD varies from 0.6 – 1.28 per 1000 people per year. These studies only include data on those killed or resuscitated by emergency medical services; thus, official data are lower than the actual number of SCD cases in the general population.
Prevention of sudden cardiac death: general population and high-risk group. Among the adult population, the incidence of SCD is 1 in 1000 per year. Prophylactic interventions to reduce the risk of sudden cardiac death in this population appear to be neither practical nor cost-effective, since the costs include the remaining 999 per 1000 people per year who are not at risk for SCD. Thus, general principles of a healthy lifestyle are recommended in the general population.
Subgroups in which the annual risk of sudden cardiac death progressively increases are relatively few. It follows from this that promoting a healthy lifestyle among the population will naturally lead to a decrease in the number of patients with coronary heart disease, which in turn will reduce the number of cases of sudden cardiac death.
Additional examinations
The medical examination schedule for adolescents is determined by the state and provides for detailed examinations by at least six specialists of children in grades 1, 5, 7 and 9. Adolescent medical examination, especially that carried out during puberty, includes additional studies. So, a teenager must definitely visit a pediatrician, undergo basic tests, go to an ENT specialist, an ophthalmologist, an orthopedist, a dentist, a psychologist, and an endocrinologist. For the most part, pathological conditions in this area can significantly worsen the child’s health, forcing other organs and systems, incl. and cardiovascular, work literally to the limit.
Of course, as a preventative measure, you should review the child’s schedule and make it, where possible, less busy. It is also necessary to take care of the teenager’s nutrition. After all, as he grows up, he needs the right food, healthy and balanced, more than ever. It is imperative to choose vitamin therapy to compensate for the lack of useful microelements, which is quite common today. So, doctors say that many teenagers around the age of 14 experience anemia. And this is fatigue, lack of composure, and inattention, which are followed by bad grades at school, conflicts with teachers and parents. Teenagers are still children who also need attention and care.
Risk factors for sudden cardiac death in the population
| Non-modifiable risk factors | Modifiable risk factors |
| Age | Smoking |
| Male | Hypertension |
| Family history of coronary heart disease | Elevated LDL levels |
| Genetic factors | Diabetes |
| Obesity |
What to do if your baby stops breathing?
It is necessary to stimulate the respiratory center. To do this, take the child in your arms and shake him, then gently massage his arms, feet, earlobes and vigorously run your fingers along the spine. As a rule, such actions are enough for the child to wake up.
If this does not happen, start giving the baby artificial respiration, and if there is no pulse, then chest compressions. However, in order to carry out all actions correctly, it is advisable that you acquire the necessary skills for this during pregnancy or earlier, when you were planning to become a mother.
In addition, as soon as you begin to help your baby, one of your relatives should call an ambulance so that the doctors can arrive on time.
Prevention of SCD: recommendations of the European Society of Cardiology
The European Society of Cardiology Specialist Group on Sudden Cardiac Death presents recommendations aimed at reducing the incidence of SCD. The recommendations are presented in tables and distributed as follows:
Class I:
Reliable evidence and/or consensus among experts that a given procedure or treatment is appropriate, beneficial and effective.
Class II:
Conflicting evidence and/or differences in expert opinion about the benefit/effectiveness of a procedure or treatment.
Class IIa:
evidence and/or expert opinion for benefit/effectiveness predominates.
Class IIb
: Benefit/effectiveness is not well supported by evidence and/or expert opinion.
In these guidelines, the terms “primary” and “secondary” prevention are used primarily in the context of ventricular arrhythmia. Therapy prescribed to prevent the development of sustained ventricular arrhythmias in patients without a history of episodes of life-threatening ventricular arrhythmias, but classified as at high risk for their development, refers to “primary” prevention. The therapy recommended for patients with cardiac arrest and syncope/hypotension secondary to paroxysmal ventricular tachycardia is “secondary” prevention.
Negative effects of drugs
Medicines that cause cardiac arrest are used for treatment. In rare cases, deliberate overdose causes death. This must be proven to the judicial and investigative authorities. When prescribing medications, the doctor takes into account the patient’s age, weight, diagnosis, and warns about a possible reaction and the need to see a doctor again or call an ambulance.
Overdose occurs when:
- non-compliance with the regime (taking pills and alcohol);
- deliberately increasing the dose (“I forgot to drink this morning, so I’ll take two at once”);
- combination with traditional methods of treatment (St. John's wort, shepherd's ears, self-prepared tinctures of lily of the valley, foxglove, adonis);
- carrying out general anesthesia against the background of continuous medication use.
The use of St. John's wort herb should be very limited; its potency is comparable to antitumor cytostatics
The most common causes of cardiac arrest are:
- sleeping pills from the group of barbiturates;
- narcotic drugs for pain relief;
- groups of β-blockers for hypertension;
- medicines from the group of phenothiazines prescribed by a psychiatrist as a sedative;
- tablets or drops of cardiac glycosides, which are used to treat arrhythmias and decompensated heart failure.
It is estimated that 2% of asystole cases are drug related.
Only a specialist can determine which medications have the most optimal indications and have the least accumulation and addiction properties. You should not do this on the advice of friends or on your own.
I. Myocardial infarction and heart failure
A. Risk stratification
Both non-invasive and invasive tests are used to determine the risk of SCD in patients with a history of myocardial infarction.
Risk stratification in patients who have had myocardial infarction
with/without development of HF
| Class | I | IIa | IIb |
| Demographic variability LVEF HR or BR sensitivity LV volume | ES unstable VT resting heart rate | Late potentials EPI Dynamics h. T Patency of the infarct-dependent artery |
LVEF – left ventricular ejection fraction; HR – rhythm variability
BR – baroreflex; ES – extrasystole; VT – ventricular tachycardia
HR – heart rate; h. T – T wave
B. Primary and secondary prevention of SCD in patients with a history of MI
Sudden cardiac death occurs most often among patients who have had a myocardial infarction. In this group, primary prevention includes drug treatment with beta blockers, aspirin, ACE inhibitors and cholesterol-lowering drugs. In patients with documented sustained VT or VF, the alternative is an implantable cardioverter-defibrillator (ICD) or amiodarone, and in selected cases, ablation or surgery. In patients with a history of myocardial infarction, a decrease in LVEF less than or equal to 40% (less than or equal to 5%) and clinically symptomatic paroxysms of non-sustained VT, or induced sustained or non-sustained VT by programmed electrical stimulation (EPS), the recommended treatment is CD implantation. For secondary prevention of SCD, the use of CD is recommended for those resuscitated after VF and patients with hemodynamically symptomatic VT paroxysms.
Primary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| History of MI | Beta blockers ACE inhibitors Cholesterol-lowering drugs Aspirin | Polyunsaturated fatty acids Amiodarone | |
| MI + LV dysfunction | Beta blockers ACE inhibitors Aldosterone receptor blockers | Amiodarone | |
| Hemodynamically asymptomatic VTs | Amiodarone Beta blockers | CD Ablation Surgical treatment | |
| LVEF less than or equal to 40% + paroxysms of non-sustained VT + inducible sustained VT with EPI | KD |
Secondary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| VF | KD | ||
| Hemodynamically symptomatic sustained VT | KD | Amiodarone Beta blockers |
What are the consequences of cardiac arrest?
The consequences of circulatory arrest depend on the speed and correctness of emergency care. Long-term oxygen deficiency of organs causes:
- irreversible foci of ischemia in the brain;
- affects the kidneys and liver;
- With vigorous massage in elderly people and children, fractures of the ribs, sternum, and the development of pneumothorax are possible.
The mass of the brain and spinal cord together constitutes only about 3% of the total body mass. And for their full functioning, up to 15% of the total cardiac output is required. Good compensatory capabilities make it possible to preserve the functions of nerve centers when the level of blood circulation decreases to 25% of normal. However, even chest compressions can only maintain 5% of normal blood flow.
Read about the rules of resuscitation measures and possible options in this article.
Consequences from the brain can be:
- partial or complete memory impairment (the patient forgets about the injury itself, but remembers what happened before it);
- blindness is accompanied by irreversible changes in the visual nuclei, vision is rarely restored;
- paroxysmal spasms in the arms and legs, chewing movements;
- different types of hallucinations (auditory, visual).
Statistics show actual revival in 1/3 of cases, but complete restoration of brain and other organ functions occurs only in 3.5% of cases of successful resuscitation
This is due to the delay in assistance in cases of clinical death.
II. Cardiomyopathies
Hypertrophic cardiomyopathy (HCM)
HCM is a relatively common cardiac disorder (incidence in adults approximately 1:500) in which sudden cardiac death is the most likely outcome at any age, but is most common in young, often asymptomatic patients. Implantation of a CD for the prevention of sudden cardiac death is strongly justified in patients who survive cardiac arrest (secondary prevention). Prophylactic use of KD is also possible in patients with two or more risk factors.
Hypertrophic cardiomyopathy
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Family history of SCD Syncope LV hypertrophy (VSD greater than cm) Unsustained VT Hypotension during exercise stress test | High risk of mutations |
| Primary prevention | KD | Amiodarone | |
| Secondary prevention | KD |
VSD – thickness of the interventricular septum
Arrhythmogenic right ventricular dysplasia (ARVD)
ARVD is one of the main causes of sudden cardiac death in the “pre-coronary” age group. Although the predisposing factors for SCD have not yet been sufficiently studied in large prospective studies, sudden cardiac death occurs more often in patients with significant changes in the right ventricle, as well as in those with LV involvement. In those resuscitated after SCD (secondary prevention), in patients with sustained VT and ineffective antiarrhythmic therapy, and in high-risk patients with documented paroxysms of VT, the most adequate treatment is CD implantation.
Arrhythmogenic right ventricular dysplasia
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT/VF Dilation of the RV RV dysfunction Inducible VT/VF with EPI | Family history of SCD Late potentials + LV dysfunction VT Inducible VT/VF with EPS | |
| Primary prevention | KD | Antiarrhythmic drugs | |
| Secondary prevention | KD |
RV – right ventricle; EPI – electrophysiological study
Dilated cardiomyopathy (DCM)
SCD is one of the most common mechanisms of death in DCM, especially in the early stages of the disease. Ejection fraction (EF) has been shown to be the most accurate predictor of outcome for both sudden cardiac death and death in advanced HF. The frequency of syncopal episodes is also considered one of the reliable risk factors for sudden cardiac death.
General therapeutic strategies aimed at reducing the risk of SCD in patients with DCM include the use of ACE inhibitors, beta blockers and aldosterone receptor antagonists, while amiodarone and CD implantation are used in individual cases. Several studies examining the role of antiarrhythmic drugs in patients with DCM have provided evidence (not statistically proven) that drug treatment recommended for patients who have had an MI with development of HF is equally effective in patients with DCM. The use of CDs for secondary prevention is considered acceptable; implantation of CDs is also recommended in high-risk patients for the primary prevention of sudden cardiac death.
Dilated cardiomyopathy
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Syncopations | Decreased EF Unsustained VT |
| Primary prevention | ACE inhibitors Beta blockers | KD Aldosterone receptor blockers | Amiodarone |
| Secondary prevention | KD ACE inhibitors Beta blockers | Aldosterone receptor blockers | Amiodarone |
Weak children
Modern children have a special way of life compared to past generations. On the one hand, they have more opportunities, because... they have access to global sources of information, more clubs and hobbies, but on the other hand, they go out less, communicate less often with peers, and eat poorly.
In addition, medical progress also contributes to the deterioration of children’s health. Indeed, today, young mothers often give birth at very early stages. Doctors have learned how to care for such babies: they can even grow babies born weighing 1 kg! Over time, these kids catch up with their peers, but they still remain quite fragile, and they need to be approached with special attention: they should be examined by doctors more often, and not ignore even seemingly harmless health problems. Naturally, you shouldn’t overload them. Also, various infections pose a separate danger to the fragile bodies of modern teenagers. Due to the mutation of viruses and widespread parental self-medication, even common colds can be much more difficult for children to tolerate. Doctors are especially concerned about infections when the symptoms include only fever and nothing more. All this, naturally, greatly weakens the immune forces of the child’s body.
And we shouldn’t forget about the period of hormonal changes, which has shifted today, and children begin growing up earlier. And this also becomes a serious test for a fragile organism.
Article on the topic
Evgeniy Yamburg: There are almost no healthy children left
III. Genetic pathology of ion channels
QT prolongation
Long QT syndrome is associated with a high risk of sudden cardiac death. Risk stratification is mainly based on the presence of syncope, Torsades de Pointe (VT) and a history of cardiac arrest. Primary prevention of SCD is generally based on treatment with beta blockers. CD implantation is recommended for secondary prevention, as well as in patients with VT/VF with a history of adequate treatment with beta blockers.
QT prolongation
| Class | I | IIa | IIb |
| Risk stratification | Torsade de pointes/VF/cardiac arrest Syncope Jervell–Lange-Nielsen syndrome QT prolongation | QT greater than 600 ms Development of VT/VF in childhood Prolongation of QT + AV block Macroscopically dynamic T waves Female gender Postpartum period | Family history of SCD Increased QT interval dispersion |
| Primary prevention | Avoid drugs that prolong the QT interval Beta blockers Avoid strenuous exercise | Sympathetic denervation of the LV pacemaker | |
| Secondary prevention | KD + beta blockers + avoid drugs that prolong the QT interval Avoid intense exercise |
ECS - electrical pacemaker
Brugada syndrome
Diagnosis of Brugada syndrome (BS) is based on the presence of spontaneous or inducible ST segment elevation in leads V1-V with or without right bundle branch block (RBBB). Risk stratification is still poorly defined, and the role of EPS in identifying patients with high-risk factors is debated. In survivors of cardiac arrest, CD implantation is recommended. Prophylactic use of KD in high-risk populations is strongly recommended, but this approach is limited by the lack of clearly defined risk criteria.
Brugada syndrome
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Syncope Family history of SCD | Inducible VT/VF during EPI |
| Primary prevention | CD in patients with syncope/VT | KD in asymptomatic patients with VT induced by EPI | |
| Secondary prevention | KD |
Catecholaminergic polymorphic ventricular tachycardia
To date, there is no precise definition of catecholaminergic polymorphic ventricular tachycardia (CPVT), since large-scale studies are not possible. This disease is associated with a high risk of sudden cardiac death at a young age, but criteria for stratification are lacking. Prevention of sudden cardiac death is based on the use of beta blockers; KDs are recommended for secondary prevention, since the significance of KDs for primary prevention has not been determined.
Catecholaminergic polymorphic ventricular tachycardia
| Class | I | IIa | IIb |
| Risk stratification | VF | Family history of SCD Unsustained VT/syncope in childhood | Syncopations |
| Primary prevention | Beta blockers | KD | |
| Secondary prevention | KD + beta blockers | Beta blockers |
Diagnostic signs of cardiac arrest
Cardiac arrest syndrome includes early signs of clinical death. Since this phase is considered reversible with effective resuscitation measures, every adult should know the symptoms, since a few seconds are allotted for reflection:
- Complete loss of consciousness - the victim does not respond to shouting or braking. It is believed that the brain dies 7 minutes after cardiac arrest. This is an average figure, but the time can vary from two to eleven minutes. The brain is the first to suffer from oxygen deficiency; the cessation of metabolism causes cell death. Therefore, there is no time to speculate on how long the victim’s brain will live. The earlier resuscitation is started, the greater the chance of survival.
- Inability to detect pulsation in the carotid artery - this diagnostic sign depends on the practical experience of others. If it is absent, you can try to listen to heartbeats by placing your ear to your bare chest.
- Impaired breathing - accompanied by rare noisy breaths and intervals of up to two minutes.
- “Before our eyes” there is an increase in the change in skin color from pallor to blueness.
- The pupils dilate after 2 minutes of cessation of blood flow, there is no reaction to light (constriction from a bright beam).
- Manifestation of cramps in individual muscle groups.
If an ambulance arrives at the scene of the incident, then asystole can be confirmed by an electrocardiogram.
IV. Valve pathology
Aortic stenosis
Among patients whose cause of death is aortic stenosis (AS), about 20% are sudden cardiac death. In the absence of symptoms, the survival rate of patients with AS is high even without valve replacement. The prognostic value of various hemodynamic and electrophysiological studies is limited. Asymptomatic patients with hemodynamically severe aortic stenosis should be under constant observation and, if symptoms develop, undergo immediate surgery. In patients with documented sustained ventricular tachycardia, cardiac implantation should be considered.
Aortic stenosis
| Class | I | IIa | IIb |
| Risk stratification | Syncope Angina | VT, including those induced by EPS Decreased exercise tolerance | Significant stenosis |
| Primary prevention | Surgery | Amiodarone | |
| Secondary prevention | KD |
Mitral valve prolapse
Mitral valve prolapse (MVP) generally has a favorable prognosis; There are suggestions about the risk of sudden cardiac death, but there is no evidence. Most cases of SCD are described in patients who have previously suffered syncope or cardiac arrest, a family history of SCD at a young age, with severe prolapse or myxomatous changes in the mitral valve leaflets. For patients surviving cardiac arrest, CD implantation is recommended.
Mitral valve prolapse
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Family history of SCD Severe prolapse or myxomatous changes in the leaflets | QT prolongation Frequent/group ES Inducible VT/VF with EPS Mitral valve regurgitation Late potentials |
| Primary prevention | |||
| Secondary prevention | KD |
Diet to prevent sudden death syndrome
Mom's diet while breastfeeding
- Efficacy: no data
- Timing: entire breastfeeding period
- Cost of products: 1400-1500 rubles per week
Sudden infant death often occurs in premature babies in families with low responsibility and material income, when the mother, due to circumstances, does not provide decent care for the baby, has various types of addictions and cannot find a permanent partner for life. Therefore, for the well-being of the child, it is necessary to exclude all of the above factors, take care of his sleep hygiene and establish a healthy life schedule - with walks and good nutrition for both mother and child, which can provide all nutrients, vitamins and minerals. Often, due to the mother’s lack of breast milk, it is necessary to resort to artificial feeding, the main thing is that it is of high quality and meets the needs of the child.
V. Pathology of the coronary arteries
Anomalous origin of the coronary arteries
SCD most often occurs in patients with an anomalous origin of the trunk of the left coronary artery from the right or non-coronary sinus of Valsalva. Therefore, special attention should be paid to young patients with chest pain similar in description to angina. Surgery is the most appropriate treatment option for patients at high risk of sudden cardiac death.
Anomalous origin of the coronary arteries
| Class | I | IIa | IIb |
| Risk stratification | VF | Young patients with angina or a positive stress test | |
| Primary prevention | Surgery | ||
| Secondary prevention | Surgery |
Myocardial bridges
The long-term prognosis for patients with the presence of myocardial bridges seems favorable, but in some cases this pathology can cause the development of tachyarrhythmias or sudden cardiac death. In symptomatic patients, quantitative coronary angiography, Doppler, and intravascular ultrasound are used to diagnose myocardial bridges. Drug treatment with beta blockers, surgery, angioplasty and coronary artery stenting are alternative treatments.
Myocardial bridges
| Class | I | IIa | IIb |
| Risk stratification | Symptomatic VT VF | Myocardial ischemia | |
| Primary prevention | Surgical treatment in patients with myocardial ischemia | Beta blockers | |
| Secondary prevention | Surgical treatment in patients with myocardial ischemia |
Is it painful to die or not - feelings at the moment of death
Every person at a conscious age thinks about death. What awaits us after death? Does the other world exist? Are we purely biological beings, or does each of us still have a certain soul that, after death, goes to another world? One of the many questions that arises in the mind is the unknown of the sensations that a person experiences just before death. Does a person experience torment, pain, or, on the contrary, do all sensations become dull before leaving for another world? The issues discussed have worried people since their inception and still do. Scientists continue to study this mysterious phenomenon, but only a few questions can be answered. Feelings of Dying People The physical sensations of a dying person will depend primarily on what led him to death. He can experience both severe pain and pleasant sensations. As for psychological perception, at the moment of dying, most people instinctively feel fear, panic and horror, and try to “resist” death. According to biology, after the heart muscle stops contracting and the heart stops, the brain continues to function for about five minutes. It is believed that in these last minutes, a person’s mind reflects on his life, vivid memories emerge, and the person, as it were, “sums up” his existence. Classification of death Biologists divide death into two categories: Natural; Unnatural. Natural death occurs according to the laws of normal physiology and occurs due to the natural aging of the body or in the case of underdevelopment of the fetus in the womb. Unnatural death can occur for the following reasons: Due to various serious and fatal diseases (oncological, cardiovascular, etc.); Mechanical effects: suffocation, electric shock; Chemical exposure: overdose of drugs, medicinal substances or alcohol overdose; Unspecified - a seemingly healthy person dies suddenly from a latent disease or a sudden, acute form of the disease. From a legal point of view, death is divided into: Non-violent; Violent. Nonviolent death occurs in old age, long-term illness, and in other similar cases. Violent deaths include murder and suicide. Stages of Death To better understand what a person may experience during death, we can consider the stages of the process identified from a medical point of view: Preagonal stage. At this moment, a malfunction occurs in the blood circulation and breathing systems, causing hypoxia to develop in the tissues. This period lasts from several hours to several days; Terminal pause. At this moment, the person stops breathing, the functioning of the myocardium malfunctions; Agonal stage. The body is trying to return to life. At this stage, a person periodically stops breathing, the heart works increasingly weaker, which causes malfunctions in the functioning of all organ systems; Clinical death. Breathing and blood circulation stop. This stage lasts about five minutes, and it is at this moment that the person can be brought back to life with the help of resuscitation measures; Biological death - a person finally dies. Important! Only people who have experienced clinical death are the only ones who can accurately report what sensations are possible in a dying person. Morbidity in various deaths Cause Time of dying Pain Overdose of prescription drugs 129 minutes 8.5 Fall from height 5 minutes 17.78 Drowning 18 minutes 79 Shot in the head with a pistol 3 minutes 13 Fire 1 hour 91 Is it painful to die from cancer Cancer is one of the the most common causes of death. Unfortunately, a cure for malignant carcinoma has not yet been discovered, and cancer at stages 3 and 4 is an incurable disease. All that doctors can do in this situation is to reduce the patient’s pain with the help of special analgesics and slightly prolong the person’s life. A person with a cancer tumor does not always experience pain when dying. In some situations, before the death of a cancer patient, he begins to sleep a lot and ultimately plunges into a comatose state, after which he dies without feeling any physical illness, that is, directly in his sleep. In another situation, the stages of dying of a cancer patient are as follows: Before death, the patient may experience migraines, see hallucinations and lose memory, which is why he does not recognize his loved ones; Speech disturbances occur, it is more difficult for the patient to say connected sentences, he may utter awkward phrases; The person may experience blindness and/or deafness; As a result, the motor functions of the body are impaired. However, this is only a general average picture of how a person with cancer feels before death. If we look directly at specific types of cancer tumors, then the localization of carcinoma in the liver makes a person die in agony due to multiple bleedings. Death from lung cancer also causes significant pain due to the fact that the patient begins to choke, vomit blood, after which an epileptic attack occurs and the patient dies. In the case of intestinal cancer, the patient also feels excruciating pain in the abdomen, in addition to this, he is tormented by a headache. Laryngeal cancer patients also feel pain before they die. With this localization, the person also experiences severe pain in the corresponding area. Important! Do not forget that the described symptoms are eliminated by doctors with the help of special analgesics, and before death - narcotic drugs, so in some cases it is possible to achieve an almost complete reduction in pain until it disappears. Thus, the question “is it painful to die from cancer” can most likely be answered in the negative, since modern medicine has all the means to help reduce the patient’s pain. Is it painful to die of old age? According to medical research, people in old age experience a feeling of relief when they die. Only 1/10 of those surveyed feel fear before death. Just before death, old people feel discomfort, pain and complete apathy towards everything. When dying, people begin to see hallucinations and can “talk” to the dead. As for physical sensations, dying is painful only due to difficulty breathing. Most old people can die in their sleep, and this death is not associated with severe pain and physical suffering. Does it hurt to die from a pill overdose? The physical sensations of a person dying due to taking an excessive amount of a drug depend primarily on the type of medication and the individual characteristics of the body. In fact, death occurs due to the development of severe intoxication of the body, and before death a person may experience pain due to pain in the abdomen. In addition, he experiences dizziness, nausea and vomiting. An exceptional case would be a person who has taken an excessive dose of a potent sedative, since the consequences of such an act will be the onset of a deep coma and the shutdown of all instinctive defense mechanisms. In view of this, a person passes into another world directly in a dream and does not feel pain. Is it painful to die from a stroke? Because a stroke can occur in different areas of the brain, a person's experience of death may vary. If the motor center has been affected, weakness or paralysis may occur in a particular limb. The general picture of a person’s feelings about death is usually the following: He hears incomprehensible voices or sounds; Sleepy; Confused mind; Strong headache; General weakness. Some stroke patients may also die in their sleep or go into a deep coma. Is it painful to die from a heart attack? During a heart attack, sudden changes in pressure occur due to a failure in blood circulation, which is felt by a person as severe pain in the area behind the sternum. In addition, the blood supply to all organs is disrupted, which also causes pain - in particular, blood stagnates in the lungs and swelling of the latter occurs. The patient experiences difficulty breathing and general weakness of the body. In the first minutes, when blood stops flowing to the brain and hypoxia begins, the person will also experience a severe headache. However, as a rule, during such an attack, a person may lose consciousness almost immediately, since the organs are not supplied with blood in the normal manner. Without medical assistance, a person in this condition can live no more than 5 minutes without feeling pain. Does it hurt to die from a bullet? It all depends primarily on the place where the bullet hit and its caliber. If a bullet pierces the brain, then very often death occurs almost instantly, and the organ shuts down faster than the person has time to feel anything. In other situations, as a rule, first a person feels a sharp jolt, then a certain warmth in the body, and only then severe pain. After a few minutes, a painful shock occurs, when pain is no longer felt due to the body’s defense mechanisms being turned on, and the person loses consciousness. If medical care is not provided, he dies from blood loss, but there is no physical suffering. Does it hurt to die from a fall? Death from falling from a great height occurs almost instantly - within a few seconds or minutes. The sensations largely depend on the position in which the person landed and on the surface on which he fell. If you land on your head, death occurs instantly, and the only thing that can be experienced in this case is psychological panic during the flight. Death due to a fall occurs due to multiple fractures, rupture of internal organs and large blood loss. In the first seconds after the fall, a person experiences severe pain from the impact, then weakness occurs due to developing hypoxia and loss of consciousness. Is it painful to die from blood loss? The time of death in this case depends on the caliber of the damaged vessels. In particular, if the walls of the aorta are destroyed, the person dies almost instantly, without experiencing pain. Losing a lot of blood, a person does not feel pain. When bleeding, he first experiences dizziness, heaviness in the body and weakness. Gradually, strong thirst is added to these feelings. Eventually, due to insufficient blood supply, the person may lose consciousness and die. Is it painful to die from cold? In severe frost conditions, a person can die for quite a long time, but will not experience pain. Being in the cold for a long time, a person first experiences severe trembling and body aches. Gradually, he also begins to lose his memory and the ability to recognize the faces of loved ones. Then severe weakness sets in and, as a rule, people simply fall into the snow. The slow speed of blood flow in the brain provokes hallucinations. Severely narrowed capillaries on the skin can suddenly expand their lumen to create a surge of heat, which is why people often try to take off their clothes at this moment due to the feeling of “hotness”. After this, the person loses consciousness and dies as if “in his sleep.” Is it painful to die from AIDS? Since death in this case does not arise from AIDS itself, but from a disease that the body cannot cope with, the sensations before death may vary. Most often this is cytomegalovirus, liver cirrhosis, tuberculosis, developing against the background of AIDS. However, death can also occur from ordinary bronchitis. Physical sensations will depend entirely on the disease that the body cannot overcome. It is painful for a person to die only if he is sick with serious diseases of the internal organs. For example, if death occurs from tuberculosis, the patient will experience severe pain in the chest, breathing and heartbeat may be impaired, and bloody vomiting may occur. In cases where death occurs due to cirrhosis of the liver, the patient may experience excruciating pain in the abdomen and right hypochondrium. Conclusion Summarizing the above, we can say that it is more painful for people to die psychologically. Only in some cases does a person experience severe pain before death. Most often, people find it difficult to accept the fact of dying.
VI. Wolff-Parkinson-White syndrome (WPW)
According to modern research, in patients with WPW syndrome, the incidence of sudden cardiac death is 0.15% per year. The main cause of SCD is the transition of atrial fibrillation with a rapid ventricular response to ventricular fibrillation. Survivors of resuscitation for sudden cardiac death are typically characterized by the absence of symptoms, shortened RR intervals (less than 250 ms) during paroxysmal atrial fibrillation, and the presence of multiple or posteroseptal accessory pathways. Electrophysiological study with atrial excitation and determination of RR intervals between preexcited QRS complexes has high sensitivity, but specificity and significance in determining a positive predictor are limited. In patients at high risk for SCD, catheter ablation is recommended, particularly in those resuscitated from ventricular fibrillation or in patients with symptomatic episodes of atrial fibrillation with a rapid ventricular response.
Wolff-Parkinson-White syndrome
| Class | I | IIa | IIb |
| Risk stratification | less than 250 ms cycle duration in AF less than 270 ms anterograde refractory period of additional pathways Multiple additional pathways | Cessation of pre-excitation during treatment with ajmaline | |
| Primary prevention | Ablation for atrial fibrillation and the presence of rapid conduction through accessory pathways | Ablation in asymptomatic patients with – family history of SCD – athletes | Amiodarone Antiarrhythmic drugs classes Ia and Ic |
| Secondary prevention | Ablation |
Pathogenesis
Children commonly have abnormalities in serotonin , which is thought to impair the ability to regulate arousal and breathing normally, particularly in potentially life-threatening situations such as sleep and turning the baby onto his or her stomach. In addition, changes in the polymorphism of anti-inflammatory cytokines and reduced mandibular size are determinants of death. Another chain of mechanisms that causes sudden cessation of breathing is associated with the process of accumulation of high concentrations of carbon dioxide and insufficient blood oxygenation.
In general, there are several theories of the development of thanatogenesis mechanisms - respiratory, cardiac and metabolic.
VII. Bradyarrhythmias
It has been established that bradyarrhythmias are the cause of sudden cardiac death in 15-20% of cases. Risk factors for bradyarrhythmic death include high-degree AV block with intraventricular conduction disturbances, but in the presence of structural changes in the heart, these factors may predispose to the development of tachyarrhythmias. Pacing is the treatment of choice in high-risk patients with bradyarrhythmia: it relieves symptoms and may reduce mortality.
Risk stratification for cardiac conduction disorders
| Class | I | IIa | IIb |
| Profound AV block | AV block III degree AV block II degree, type II Syncope Combination of heart disease with CHF | ||
| Congenital AV block of the third degree | Syncope QT prolongation Congenital heart disease | ||
| Chronic two- or three-fascicle blockade | Combination of heart disease with CHF | Syncope Conduction from the Hiss bundle to the ventricles 100 ms (HV interval 100 ms) Intraventricular blocks Blocks induced during EPI |
Main types of cessation of cardiac activity and mechanisms of their development
The causes of cardiac arrest according to the developmental mechanism are hidden in a sharp violation of its functional abilities, especially excitability, automatism and conductivity. The types of cardiac arrest depend on them. Cardiac activity can stop in two ways:
- asystole (in 5% of patients);
- fibrillation (in 90% of cases).
Asystole is a complete cessation of ventricular contraction in the diastole phase (during relaxation), rarely in systole. An “order” to stop can come to the heart from other organs reflexively, for example, during operations on the gall bladder, stomach, and intestines.
With reflex asystole, the myocardium is not damaged and has fairly good tone.
In this case, the role of the vagus and trigeminal nerves was proven.
Another option is asystole in the background:
- general oxygen deficiency (hypoxia);
- increased carbon dioxide content in the blood;
- shift of acid-base balance towards acidosis;
- altered electrolyte balance (increase in extracellular potassium, decrease in calcium).
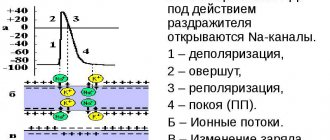
These processes taken together negatively affect the properties of the myocardium. The process of depolarization, which is the basis of myocardial contractility, becomes impossible, even if conductivity is not impaired. Myocardial cells lose active myosin, which is necessary to obtain energy in the form of ATP.
With asystole, hypercalcemia is observed in the systole phase.
Cardiac fibrillation is an impaired communication between cardiomyocytes in coordinated actions to ensure overall myocardial contraction. Instead of synchronous work causing systolic contraction and diastole, many separate areas appear that contract on their own.
The contraction frequency reaches 600 per minute and above
In this case, the ejection of blood from the ventricles is affected.
Energy expenditure is significantly higher than normal, and effective reduction does not occur.
If fibrillation affects only the atria, then individual impulses reach the ventricles and blood circulation is maintained at a sufficient level. Attacks of short-term fibrillation can end on their own. But such ventricular tension cannot provide hemodynamics for a long time, energy reserves are depleted and cardiac arrest occurs.
Out-of-hospital resuscitation
Survival after cardiac arrest varies from 5% to 60% depending on the characteristics of the cardiac arrest (ie, cardiac etiology or not; verified or not; ventricular fibrillation or not). The outcome of cardiopulmonary resuscitation (CPR) is influenced not only by the success of its implementation, but also by the patient’s condition before the start of CPR.
It is now generally accepted that time to electrical defibrillation is the single most significant determinant of survival after cardiac arrest.
The instructions for the automatic external defibrillator allow defibrillation in cases of out-of-hospital ventricular fibrillation or ventricular tachycardia to people of non-medical professions, often many minutes before the arrival of the ambulance team. This strategy is known in the West as “first responder defibrillation,” based on the principle of mutual aid.
Cardiac ischemia
Coronary heart disease is an extremely common disease in the human population and is the main cause of death and disability in the developed countries of the world. This is a syndrome that develops in the cardiac form of atherosclerosis and hypertension, which lead to absolute or relative failure of cardiac activity.
The term IHD was first coined in 1957 and defined the discrepancy between the need and blood supply of the heart. This discrepancy is due to blockage of the lumen of blood vessels by atherosclerosis, high blood pressure and spasm of the vascular wall.
As a result of insufficient blood circulation, heart attacks or local limited death of the muscle fibers of the heart develop. IHD has two main forms:
- The chronic form (angina) is periodic attacks of pain in the heart caused by relative transient ischemia.
- Acute form (acute cardiac infarction) is acute ischemia with the development of a local focus of myocardial necrosis.
Acute myocardial necrosis (infarction) is a form of ischemic heart disease that most often leads to death. There are several signs by which acute necrosis of the heart muscle is classified. Depending on the extent of the lesion, there are:
- large-focal myocardial infarction;
- small focal myocardial infarction.
According to the time interval from the onset of symptoms to death:
- The first two hours from the onset of necrosis (the most acute period);
- From the time of onset of the disease to 10 days (acute period);
- from 10 days to 4-8 weeks (subacute period);
- from 4-8 weeks to 6 months (scarring period).
The likelihood of death is very high in the acute period and with extensive damage.