Alcohol and antibiotics are a combination that doctors do not recommend using. Harm to health and danger to life are guaranteed. In some situations, you cannot do without medication. Diseases always appear at the wrong time - on the eve of a holiday or celebration, symptoms suddenly appear, indicating an infectious disease.
In this situation, people prefer to isolate themselves from the crowd by refusing a sip of wine or beer. Others forget about taking medications for the evening, thinking that one evening does not solve anything. If you miss at least one dose, the entire result of treatment comes to naught, since the pathogen receives fertile soil for development. To defeat the bacteria, you will have to use stronger combinations, which harms the body, weakens it, making it vulnerable.
During antibacterial treatment, you are allowed to drink a glass of opinion. According to the results of laboratory studies, alcohol does not affect the use of antibiotic compounds. You should not expect any unpleasant side effects. Maintain boundaries without overusing them. Mixing treatment with alcohol is associated with the following consequences:
- Development of an allergic reaction to components containing alcohol.
- Redness of the skin, rash, increased sweating. A feeling of heat and temperature appears.
- Intoxication of the whole body. Symptoms include vomiting, convulsions, severe headache and dizziness.
- Liver dysfunction. Metabolism slows down. Recycling products cease to be excreted. The exchange is slow and atypical. This inhibits the work and function of systems, accumulates toxins and products, which affects well-being.
- Blood pressure surges.
Everyone's reaction is different based on the combination. The mechanism of action is different, so it is difficult to give a definite answer. Call a doctor at home for a consultation. Please call our 24-hour service contact number. The operator will answer, ask questions and dispatch a team that will arrive within thirty minutes within the city. After examining the patient, the doctor will describe the picture, prescribe treatment, and help get out of intoxication. Some restrictions are imposed on the patient’s usual life and diet in order to get rid of unfavorable manifestations and return to the working rhythm.
Compound
The main active ingredient of the drug is norfloxacin .
The auxiliary components of Norbactin are as follows: MCC , sodium lauryl sulfate , colloidal silicon dioxide , purified talc , croscarmellose sodium , corn starch , magnesium stearate .
The shell contains the following substances: hypromellose , purified talc, purified water, macrogol 400, titanium dioxide.
Pharmacodynamics and pharmacokinetics
Once in the body, the drug affects the bacterial enzyme DNA gyrase. It destabilizes the DNA chain, which leads to the death of bacteria. The bactericidal effect occurs quite quickly. The development of plasmid-mediated resistance is minimal.
The drug affects most aerobic gram-negative microorganisms, as well as some gram-positive ones. This is a potent antipseudomonal agent .
The medicine is well absorbed from the gastrointestinal tract. However, you should not take it with food as this will reduce its effectiveness. For better absorption, it should be consumed on an empty stomach.
The maximum concentration of the drug is 1-2 hours after administration. The degree of protein binding is 14%. Widely distributed in tissues, but does not penetrate bones and the central nervous system. Bioavailability is about 40%, half-life is 3.5-6.5 hours, but high concentrations are found in tissues for longer.
The drug is partially processed in the liver. Some amounts are excreted in bile, but mainly in urine and feces.
Side effects of the drug Norbactin
from the gastrointestinal tract: anorexia, bitterness in the mouth, nausea, vomiting, abdominal pain, diarrhea, pseudomembranous enterocolitis (with prolonged use), hepatitis, increased activity of liver transaminases, moderate gastralgia, heartburn, pancreatitis, jaundice; from the urinary system: crystalluria, glomerulonephritis, interstitial nephritis, dysuria, polyuria, albuminuria, urethral bleeding, hypercreatininemia; from the central nervous system: headache, dizziness, drowsiness, hallucinations, fatigue, mood changes, paresthesia, dissomnia, depression, anxiety, irritability, euphoria, disorientation, restlessness, polyneuropathy, including Guillain-Barré syndrome, epileptiform seizures; from the cardiovascular system: tachycardia, arrhythmia, decreased blood pressure, fainting, vasculitis; allergic reactions: skin itching, urticaria, swelling, exanthema, anaphylaxis, petechiae, hemorrhagic bullae and papules with crust formation as a manifestation of vascular involvement (vasculitis), angioedema; in isolated cases - exfoliative dermatitis, Stevens-Johnson syndrome, Lyell's syndrome, exudative polymorphic erythema, photosensitivity; from the musculoskeletal system: arthralgia, tendonitis, tendovaginitis, tendon ruptures, myalgia, arthritis; from the blood system: leukopenia, eosinophilia, decreased hematocrit, hemolytic anemia, thrombocytopenia; from laboratory parameters: neutropenia, increased levels of glutamate-oxaloacetate transaminase, glutamate-pyruvate transaminase and alkaline phosphatase in the blood plasma; others: vaginal candidiasis, dysopia, lacrimation, ringing in the ears. When using drugs based on norfloxacin, several cases of inflammation of the Achilles tendon were observed, which can lead to its rupture. Pseudomembranous colitis . Depending on the indications, the issue of discontinuing norfloxacin therapy is decided and appropriate treatment of the adverse reaction is immediately started (use of appropriate antibiotics/chemotherapeutic drugs, the effectiveness of which has been clinically proven). In this case, you should not use drugs that suppress peristalsis. Severe hypersensitivity reactions (anaphylaxis) . If such reactions occur, treatment with norfloxacin is immediately stopped and appropriate emergency measures are taken (administration of antihistamines, corticosteroids, sympathomimetics, and, if necessary, mechanical ventilation). Epileptiform seizures. Appropriate emergency measures are taken (restoration and maintenance of airway patency, administration of anticonvulsants - diazepam or barbiturates).
Indications for use of Norbactin
Norbaktin is used for cystitis , pyelonephritis , urethritis , as well as for bacterial infections of the gastrointestinal tract, genital organs and uncomplicated gonorrhea :
- prostatitis;
- endometritis;
- cervicitis;
- salmonellosis;
- shigellosis.
Indications for use of Norbactin also include its use by patients with granulocytopenia and travelers' diarrhea as a prophylactic agent.
Emergency care for acute pyelonephritis and hematuria
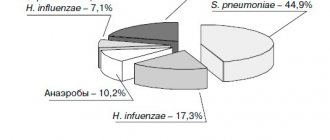
Acute pyelonephritis is a nonspecific infectious inflammation of the pyelocaliceal system and renal parenchyma. ARF is caused by Escherichia coli, Klebsiella, Proteus, Pseudomonas.
Routes of entry of an infectious agent into the kidney:
- ascending - foci of chronic inflammation are located in the female genital organs, lower urinary tract and less commonly in the colon;
- hematogenous - the source is an acute or subacute inflammatory process outside the urinary tract (mastitis, boil or carbuncle, etc.).
Predisposing factors for the development of acute pyelonephritis are hemodynamic or urodynamic disorders in the kidney or upper urinary tract. Acute pyelonephritis is more often observed in women.
The infection, once in the kidney, receives favorable conditions for its development in zones of hypoxia, where the inflammatory process occurs. An infected thrombus or embolus in the terminal vessels of the renal cortex causes an infarction followed by suppuration. The occurrence of multiple small suppurating infarctions in the cortex is classified as apostematous nephritis. The development of an extensive infarction with subsequent suppuration leads to the formation of a renal carbuncle.
With regard to the pathogenesis of the disease, primary and secondary pyelonephritis are distinguished (Fig. 1). Secondary pyelonephritis is based on organic or functional changes in the kidneys and urinary tract.
Depending on the passage of urine through the upper urinary tract, i.e. from the kidney to the pelvis and further along the ureter, acute pyelonephritis is distinguished between non-obstructive (if it is preserved) and obstructive (if it is disturbed).
Manifestations of acute pyelonephritis:
- chills;
- high fever (38–39°C and above);
- pain in the lower back (side);
- often nausea and vomiting;
- general intoxication.
Often acute pyelonephritis is preceded by frequent, painful urination at the end (clinical picture of acute cystitis).
Non-obstructive acute pyelonephritis can begin with dysuria and on the same day or 1-2 days later lead to high body temperature, chills and pain in the affected kidney. Chills may be replaced by heavy sweat with a short-term decrease in body temperature; pain in the lumbar region in some cases appears during urination and precedes chills and fever (vesicoureteral reflux!), and after them does not recur (rupture of the fornix of one or more calyces and resorption of urine - fornical reflux!).
Obstructive acute pyelonephritis (occlusion of the ureter by a stone, products of chronic inflammation of the kidney, external compression - retroperitoneal fibrosis, cancer of the internal genital organs, enlarged lymph nodes, etc.) begins with gradually increasing or acute pain in the lower back on the affected side, followed by chills and increased body temperature.
Complications of obstructive acute pyelonephritis:
- development of a purulent process;
- severe impairment of renal function;
- bacteriotoxic shock;
- urosepsis;
- toxic hepatitis;
- paranephritis;
- pyonephrosis.
Diagnostics
When collecting anamnesis, pay attention to:
- for recent hypothermia;
- chronic pyelonephritis;
- urolithiasis;
- diseases of the female genitalia, prostate gland;
- previous operations on the kidneys and urinary tract, etc.
They check that the pulse rate corresponds to body temperature, detect pain in the hypochondrium during palpation of the abdomen and a positive symptom of tapping on the lower back (Pasternatsky’s symptom) from the affected kidney.
Laboratory diagnostics. In a general urine test, leukocyturia is often noted, which may be absent in obstructive acute pyelonephritis, since urine from the affected kidney does not enter the bladder.
In a general blood test, leukocytosis is noted, often with a shift in the blood count to the left (the number of band neutrophils is 20% or higher).
In a biochemical blood test, an increase in urea and creatinine levels is possible, often in elderly and weakened patients, with chronic renal failure or damage to the only functioning kidney.
When culturing urine (carried out before antibacterial therapy), the causative agent of the disease is isolated and its sensitivity to antibacterial drugs is determined.
To clarify the diagnosis and form of acute pyelonephritis, the following is carried out:
- Ultrasound;
- X-ray examinations;
- computed tomography;
- magnetic resonance imaging.
Acute pyelonephritis is differentiated from the following conditions:
- infectious diseases that occur with fever and chills and are not accompanied by pain localized in the lumbar region;
- surgical pathology of the abdominal organs, in which severe pain is often observed, and a pronounced increase in temperature and dysuric phenomena are rare.
Main directions of therapy
The emergency care algorithm for acute pyelonephritis is presented in Figure 2.
- Normalization of urine passage from the kidney:
- installation of a ureteral catheter or stent;
- installation of a catheter in the bladder if vesicoureteral reflux is suspected (lower back pain during urination);
- nephrostomia.
- Antibacterial therapy for acute pyelonephritis is in most cases empirical and depends on the severity of the disease:
- mild - oral drugs from the fluoroquinolone group;
- moderate and severe - parenteral aminoglycosides in combination with or without ampicillin, fluoroquinolones, third and fourth generation cephalosporins in combination with or without aminoglycosides.
- Surgical treatment after further examination is prescribed:
- if antibacterial therapy is ineffective within 3 days;
- severe course of the disease;
- purulent pyelonephritis
Clinical pharmacology of individual drugs
Gentamicin is effective against infections caused by gram-positive and gram-negative microorganisms, bacteria of the intestinal group. The drug is rapidly absorbed when administered intramuscularly, the therapeutic concentration in the blood is reached after 1 hour and persists for 8–12 hours. A single dose is 80–160 mg, a daily dose is 160–320 mg. Side effects: nephro- and ototoxicity. Contraindications for use: decreased kidney function and decreased hearing.
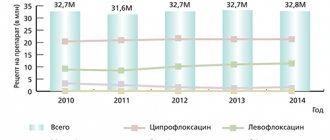
Fluoroquinolones (ciprofloxacin, norfloxacin, ofloxacin) are active against a large number of gram-positive and gram-negative bacteria and are available in forms for oral and parenteral administration. The drugs are well absorbed in the intestine and widely distributed in body fluids and tissues, secreted mainly by the kidneys. The half-life is 3–7 hours. The most widely used drugs for the treatment of acute pyelonephritis are ciprofloxacin (medociprin, siflox, ciprovin) - 500 mg 2 times a day, norfloxacin (nolicin, norbactin) - 400 mg 2 times a day and ofloxacin (zonocin, oflo , ofloxacin) - 200 mg 2 times a day. The use of fluoroquinolones is contraindicated in children under 14 years of age, pregnant women, as well as in case of individual intolerance.
Common therapy errors:
- conservative management of obstructive pyelonephritis;
- continuation of intensive antibacterial therapy without effect for more than 3 days without further examination;
- prescription of antibacterial drugs from the group of semisynthetic penicillins (ampicillin, oxacillin);
- the use of drugs from the group of uroseptics (nitroxoline, palin, negram, etc.).
Indications for hospitalization are most cases of acute pyelonephritis, especially if there is a suspicion of an obstructive nature of the lesion.
Analysis of clinical cases
Patient S., 18 years old. Complaints of pain in the left lumbar region, increased body temperature to 38°C, accompanied by chills, nausea, increased frequency and painful urination. History: 3 days ago there was hypothermia, after which urination became more frequent and painful, the temperature increased and pain appeared. I took nitroxoline without effect. On examination: pain on palpation in the left lateral parts of the abdomen, Pasternatsky’s sign is sharply positive on the left. Diagnosis: acute non-obstructive pyelonephritis on the left. The patient was hospitalized in the urological hospital. Treatment: antibacterial therapy with gentamicin (80 mg 2 times a day IM).
Patient K., 29 years old. Complaints of sharp pain in the right lumbar region, radiating to the perineum, increased body temperature to 39°C with tremendous chills, nausea, and repeated vomiting. Medical history: he has been suffering from urolithiasis for a long time; previously, small stones passed on their own several times. Two days ago, sharp pain appeared in the right lumbar region, she took Baralgin and No-shpa with a temporary effect. A day after the onset of pain, she noted a rise in temperature with chills, nausea and vomiting. On examination: the patient groans in pain. The tongue is dry, heart rate 90 beats/min. The abdomen is soft, sharply painful on palpation in the right lateral regions, Pasternatsky's symptom is sharply positive on the right. Diagnosis: right-sided renal colic. Acute obstructive pyelonephritis on the right. The patient was hospitalized in the urological hospital. Treatment: catheterization of the right ureter; if this is impossible, nephrostomy on the right. Intensive detoxification and antibacterial therapy.
Patient Sh., 67 years old. Complaints of chills, increased body temperature to 39.5°C, lower back pain on the right. History: 3 months ago, a radical cystoprostatectomy was performed for bladder cancer, plastic surgery of the bladder with an intestinal flap according to Studer. Preoperative examination revealed aplasia of the left kidney in the patient. A month after the operation, constant nagging pain appeared in the right lumbar region; he did not consult a doctor. Over the past week, the amount of urine excreted has decreased and swelling of the legs has appeared. Three days ago he noticed an increase in temperature against the background of increased pain in the right lumbar region, the temperature progressively increased, reached 39.5°C and was accompanied by chills, the volume of urine per day did not exceed 200 ml. On examination: the patient is pale, asthenic in build, and there is swelling of the lower extremities. Palpation reveals severe pain in the right lateral parts of the abdomen, Pasternatsky's symptom is sharply positive on the right. Diagnosis: acute obstructive pyelonephritis on the right. Stricture of the right ureteroneocystanastomosis. Oliguria. The patient was hospitalized in the urological hospital. Treatment: emergency nephrostomy on the right.
Hematuria is a pathological symptom characterized by blood in the urine.
The main causes of renal bleeding are presented in Table 1.
Essential hematuria (Table 2) combines a number of conditions in which the etiology and pathogenesis are unknown, and clinical, radiological and morphological studies do not allow us to accurately indicate the cause of bleeding.
Hematuria can be caused by taking non-narcotic analgesics, anticoagulants, cyclophosphamide, oral contraceptives, vincristine.
With kidney tumors, when the tumor grows in the pelvis or calyces, the integrity of the vascular wall is disrupted. If the tumor does not communicate with the pyelocaliceal system, the venous outflow from the area of the kidney with the tumor node is disrupted, the fornical veins dilate and rupture.
With prostate cancer, the tumor grows into the walls of the bladder or prostatic urethra, the veins of the bladder in its cervical section are compressed by the tumor, and venous stasis occurs. Free-floating villous tumors of the bladder, located near its neck, during urination are carried away by the flow of urine into the urethra, clog its lumen and, when pinched, swell, burst and begin to bleed.
With cystitis and prostatitis, the mucous neck of the bladder becomes inflamed, injured and bleeds easily when it comes into contact with other walls at the end of urination.
When renal hemo- and urodynamics are disturbed, the venous plexuses of the fornix, with impaired venous outflow or a significant increase in intrapelvic pressure, become overfilled with blood, the veins encircling the vaults of the calyces in a ring form expand and their integrity is disrupted, which leads to hematuria from the upper urinary tract.
With necrosis of the renal papillae, the blood supply to the papilla, and sometimes to the entire Malpighian pyramid, is disrupted, necrotic tissue is rejected, and bleeding occurs.
With benign prostatic hyperplasia, venous congestion occurs in the pelvic organs, and the integrity of the vessels is disrupted.
There are two types of hematuria:
- microscopic - the presence of red blood cells in the urine (more than three in the field of view) is determined only by microscopic examination of urine sediment;
- macroscopic - blood in the urine is determined visually; if only in the first portion of urine - initial (initial), in the last portion of urine - terminal (final), in all portions of urine - total.
Clinical picture
The appearance of red blood cells in the urine gives it a cloudy appearance and a pink, brown-red or reddish-black color, depending on the degree of hematuria. Hematuria can occur suddenly, be one-time or repeated. Its cessation is deceptive, since the cause of hematuria, as a rule, is not eliminated, and examination in case of repeated bleeding with a great delay often reveals an already advanced tumor.
With a kidney tumor, hematuria may be the first and for a long time the only symptom of the disease. In most cases, it is painless, but with profuse bleeding with the formation of clots in the renal pelvis and their passage through the ureters, dull, less often colicky pain occurs in the lumbar region. With papillary tumors of the bladder, hematuria is usually painless and profuse without the formation of clots. With villous tumors of the bladder located near its neck, the urine stream may be interrupted during urination.
With tuberculous kidney damage, total hematuria is observed in the very early stages of the process, which may be accompanied by persistent pyuria.
With benign prostatic hyperplasia, hematuria occurs for no apparent reason or during catheterization of the bladder due to a violation of the integrity of the loosened mucous membrane of the posterior urethra.
In acute cystitis and prostatitis, terminal hematuria is noted against the background of severe dysuria.
With urolithiasis, hematuria usually develops following an attack of renal colic; the urine stream may suddenly stop during urination.
Possible complications: with massive bleeding with the formation of shapeless clots, acute urinary retention is possible due to tamponade of the bladder with these clots. Rarely, shock may develop due to blood loss and pain.
Diagnostics
During the survey you need to find out:
- conditions for the occurrence of hematuria;
- degree, nature and duration of hematuria: - initial hematuria - a pathological process in the urethra (tumor, inflammation, foreign body, burn, etc.); – terminal hematuria - a pathological process in the neck of the bladder (acute cystitis, prostatitis, stones and bladder tumors); – total hematuria is a pathological process in the kidney, ureter or bladder (tumors, benign prostatic hyperplasia, renal tuberculosis, pyelonephritis, necrosis of the renal papillae, nephroptosis, etc.);
- the presence of blood clots in the urine, their shape: – worm-shaped – bleeding from the upper urinary tract and the formation of clots in the ureter; – shapeless clots – bleeding from the bladder;
- the presence of pain and its connection with changes in the color of urine: – pain in the lumbar region on the affected side – disruption of the passage of urine from the kidney due to blood clots, urolithiasis; – painless hematuria with subsequent development of renal colic (normal-colored urine) – tumor of the kidney or upper urinary tract;
- presence or absence of dysuric phenomena;
- whether there were injuries to the kidneys, bladder, urethra (in case of injury, blood is released from the urethra outside the act of urination).
Visual assessment of urine:
- scarlet blood - bleeding continues;
- brown urine - bleeding has stopped;
- brick shade - intense uraturia.
The color of urine may change when taking medications and foods:
- pink - when taking pyramidon;
- saffron yellow - nitroxoline;
- brown - rhubarb and hay;
- raspberry - purgena;
- red - phenolphthalein and beets;
- red-brown - madder dye.
With the syndrome of prolonged compression and crushing of tissues, myoglobin from the muscles enters the blood and penetrates into the urine, which gives it a red-brown color.
To determine the nature and source of bleeding in a hospital setting, the following is carried out:
- cystoscopy - in all cases of gross hematuria, with the exception of inflammatory diseases (acute urethritis, cystitis, prostatitis);
- digital rectal examination;
- Ultrasound of the bladder kidneys, prostate, transrectal ultrasound;
- excretory urography, retrograde reno- and urethrocystography, computed tomography, osteoscintigraphy according to indications in a hospital setting.
Laboratory diagnostics include:
- clinical analysis of blood, urine;
- blood chemistry;
- microscopic examination of urine sediment;
- urine culture for sterility;
- determination of the level of prostate-specific blood antigen.
With hemoglobinuria, the color of urine does not change even after standing for a long time, and with hematuria, red blood cells settle to the bottom of the vessel and the upper layers of urine become yellowish.
Hematuria in women should be differentiated from bleeding from the genitals. To do this, examine the average portion of urine during spontaneous urination or urine obtained from the bladder by catheterization.
Main directions of therapy
The emergency care algorithm for hematuria is presented in Figure 3.
| Figure 3. Emergency care algorithm for hematuria |
With the development of hypovolemia and arterial hypotension, restoration of bcc: crystalloid and colloid solutions intravenously.
If acute cystitis is suspected, after collecting urine for culture to ensure sterility, a broad-spectrum antibiotic is prescribed.
Therapy with hemostatic drugs should be carried out in a urological hospital, after diagnosis, under the control of blood clotting.
Clinical pharmacology of individual drugs
Etamsylate (dicinone) activates the formation of thromboplastin, the formation of blood coagulation factor III, and normalizes platelet adhesion. The drug does not affect the thrombotic time, does not have hypercoagulable properties, and does not contribute to the formation of blood clots. Etamsylate is administered in 2–4 ml (0.25–0.5 g) intravenously at once or drip, adding to conventional solutions for infusion.
The hemostatic effect develops:
- for intravenous administration - after 5–15 minutes; maximum effect - after 1–2 hours; the effect lasts 4–6 hours or more;
- when administered intramuscularly, the effect occurs somewhat more slowly;
- When taken orally, the maximum effect occurs after 3 hours.
Etamsylate should not be used for hemorrhages caused by anticoagulants.
Aminocaproic acid inhibits fibrinolysis by blocking plasminogen activators and partially inhibiting the effect of plasmin, and has a specific hemostatic effect in bleeding associated with increased fibrinolysis. To quickly achieve an effect, under the control of a coagulogram, a sterile 5% solution of the drug in saline is administered intravenously, up to 100 ml.
Protamine sulfate has an antihemorrhagic effect in bleeding caused by heparin during its overdose, after operations using extracorporeal circulation and the use of heparin. Apply 1 ml of a 1% solution intravenously in a slow stream over 2 minutes or drip; 1 mg of protamine sulfate neutralizes approximately 85 units of heparin. Contraindicated in hypotension, adrenal insufficiency, thrombocytopenia.
Common treatment errors: prescribing hemostatic drugs before identifying the source of hematuria.
Gross hematuria is an indication for emergency hospitalization in a urological hospital.
Analysis of clinical cases
Patient M., 30 years old. Complaints of cramping pain in the lumbar region on the left, aggravated by movement, after physical activity, blood in the urine, increased body temperature to 38.2°C. The disease began with dysuria in the form of frequent, painful urination, a day later pain appeared in the lumbar region, and blood in the urine. History: 7 years ago, a diagnosis was made of stage I nephroptosis on the left. The disease manifested itself as periodic attacks of pyelonephritis. On examination: the patient is restless. The kidney area is visually unchanged, painless on palpation, the effleurage symptom is weakly positive on the left, there is no pain along the ureters, the bladder is empty by percussion. Diagnosis: acute ascending left-sided pyelonephritis. Nephroptosis on the left. The patient was hospitalized in the urology hospital.
Patient J., 77 years old. Calling an emergency room due to intense blood in the urine and the release of blood clots during urination. History: no urological diseases. On examination: the patient is asthenic, the skin is pale. The kidney area is not visually changed; bimanual palpation of the right kidney reveals a mass formation in the lower segment; the effleurage symptom is negative on both sides. A digital rectal examination reveals that the prostate is enlarged 1.5–2 times, has a tight-elastic consistency, the median groove is smoothed, the rectal mucosa above the gland is mobile, palpation is painless. Diagnosis: tumor of the right kidney. The patient was hospitalized in the urology department.
Patient Ch., 24 years old. Complaints of constant bleeding through the urethra. History: About an hour ago I fell and hit my crotch on a pipe. On examination: bruising in the perineal area, discharge of scarlet unchanged blood from the urethra, outside the act of urination. A digital rectal examination reveals that the prostate gland is of normal size, has a tight-elastic consistency, the median groove is pronounced, the rectal mucosa above the gland is mobile, palpation is painless. Diagnosis: urethral injury. The patient is indicated for hospitalization in a hospital for examination and determination of treatment tactics.
Thus, the success of treatment of patients with pyelonephritis and hematuria is largely determined by the adoption of adequate measures in the provision of emergency medical care.
E. B. Mazo , Doctor of Medical Sciences, Professor, Corresponding Member of the Russian Academy of Medical Sciences, Russian State Medical University, Moscow
Table 1. Causes of renal bleeding
| Causes of hematuria | Pathological changes in the kidney, blood diseases, etc. |
| Congenital anomalies | Cystic diseases of the pyramids, papillary hypertrophy, nephroptosis, etc. |
| Mechanical | Trauma, stones, hydronephrosis |
| Hemodynamic | Disorders of the blood supply to the kidney (venous hypertension, infarction, thrombosis, phlebitis, aneurysms), nephroptosis |
| Hematological | Blood coagulation disorders, hemophilia, sickle cell anemia, etc. |
| Reflex | Vasoconstrictor disorders, shock |
| Allergic | Glomerulonephritis, arteritis, purpura |
| Toxic | Medicinal, infectious |
| Inflammatory | Glomerulonephritis (diffuse, focal), pyelonephritis |
| Tumor | Benign neoplasms, malignant neoplasms |
| Essential | (See Table 2) |
Table 2. Causes of essential renal hematuria
| Nature of the process | Immediate cause |
| Pathological processes | Pyelovenous reflux, calyceal venous channel, |
| in the papillary-fornical zone | venous varicose veins |
| kidneys (fornical bleeding) | |
| Diseases of the papillae and pelvis | Cystic processes in the papilla, “spongy kidney”, necrosis of the papillae, endometriosis, varicose veins |
| Pathological kidney mobility | Nephroptosis |
| Renal sinus diseases | Adhesions around the main renal vessels, sinus lipomatosis, aneurysms, varicose veins |
| Diseases of the renal interstitium | Microfibromatosis, interstitial hyperplasia with arterio- |
| Infectious and inflammatory | Pyelonephritis, necrotizing papillitis, hepatitis |
| processes | (hepatorenal syndrome) |
| Renal vascular damage | Infarction, venous thrombosis, compression of the main renal vein, varicose veins of the intrarenal veins, intraparenchymal aneurysms, angiomatous formations in Fornix |
| Blood diseases, dyscrasia | Sickle cell anemia, hemophilia, erythremia, |
| The harmful effects of drugs that disrupt the function of the blood coagulation system | Anticoagulant therapy, cytostatics |
Instructions for use of Norbactin
If the patient is prescribed Norbactin, the instructions for use provide for different dosages, which depend on what the tablets are used for. 400 mg of the drug 2 times a day is taken for:
- urinary tract infections - within 7-10 days;
- recurring or chronic urinary tract infections with exacerbations - for a month, and then, if necessary, use 400 mg per day for up to 12 weeks;
- chemoprophylaxis before and after urological operations;
- intestinal infections - within 5 days;
- acute uncomplicated cystitis - within 3 days.
400 mg once a day is prescribed if the indications for use of Norbactin are as follows:
- prevention of traveler's diarrhea ;
- renal failure.
For acute uncomplicated gonococcal infection, the instructions for use of Norbactin include taking 800 mg once.
Overdose of Norbactin, symptoms and treatment
Symptoms: increased body temperature up to febrile levels, shortness of breath, leukopenia, thrombocytopenia, acute hemolytic anemia, allergic reactions, gastrointestinal disorders, renal failure. Treatment: in case of acute overdose, calcium-containing solutions are taken orally to convert norfloxacin into a complex with calcium, which is absorbed in a very small amount into the gastrointestinal tract. The patient is carefully examined and, if necessary, symptomatic treatment is prescribed; ensure sufficient fluid intake, perform hemodialysis and peritoneal dialysis.
Overdose
In case of an overdose of the drug , dizziness , vomiting cold sweat , nausea , drowsiness , as well as a puffy facial expression without changes in the main hemodynamic parameters .
Treatment includes gastric lavage and adequate hydration therapy with forced diuresis . In addition, examination and hospitalization under the supervision of specialists for several days is necessary.
How soon can you drink alcohol after taking antibiotics?
There is a list of drugs that are allowed to be drunk with alcoholic cocktails. Among them are:
- Antifungal components. They do not enter into synthesis and do not retain harmful poisons.
- Penicillins are a broad-spectrum medicine that fights all unpleasant manifestations.
- Heliomycin - used against infectious dermatitis.
Joint use does not cause harm. We should not forget about the characteristics of each person. Do not drink alcohol for three days after completing the course. The instructions provide more detailed recommendations for each mixture.
According to doctors and scientists, the active agent remains in the blood for three days. For some, the decay period reaches two weeks. Consult your doctor first to avoid any side effects. Read the instructions carefully. It contains the following information:
- Duration of therapeutic action.
- Compatible with others.
- The time during which it is better to abstain from drinks.
If the described values are missing, intoxication can be avoided. The body is weakened during illness. He does not accept therapy if it is approached incorrectly. He is not strong enough to fight the toxins. Hops neutralizes the pharmacological effect. As a result, therapy and recovery will not bear fruit.
It is recommended to wait a day to start a course of antibiotics after drinking alcohol. It is advisable to maintain a longer interval to achieve a restorative result. If there was a long binge, you will have to wait a longer period. Contact your doctor for advice, prescription, course recommendations.
Antibiotics are useful for many diseases because they help fight bacteria and infections. Therapy is influenced by various factors, such as alcohol intake. During the recovery period, it is better to give up alcohol in order to quickly return to normal and nourish the body with useful substances.
Author of the article: Yakovlev Evgeniy Anatolyevich
Narcologist, Candidate of Medical Sciences.
Interaction
The absorption of Norbactin is made difficult by the use of antacids that contain aluminum and magnesium, as well as preparations with iron, sucralfate and zinc. There should be a break of at least 4 hours between their use.
In addition, this drug reduces the clearance of theophylline and the effect of nitrofurans , and also increases the content of indirect anticoagulants and cyclosporine in the blood serum.
The drug should be taken with caution in combination with drugs that reduce the seizure threshold, otherwise it may cause epileptiform seizures .
The simultaneous use of Norbactin and drugs that lower blood pressure can cause a sharp decrease in blood pressure. So the heart rate and ECG readings must be carefully monitored.
Norbactin analogues
Level 4 ATX code matches:
Siflox
Hyleflox
Leflobakt
Lefoccin
Gatifloxacin
Ofloxacin
Faktiv
Tigeron
Lebel
Zanotsin
Lomefloxacin
Eleflox
Lomflox
Pefloxacin
Tsiprobay
Sparflo
Tariwid
Zoflox
Abaktal
Moxifloxacin
The following analogues of Norbactin can be obtained in pharmacies:
- Nolitsin;
- Norfloxacin;
- Normax.
Their prices may vary. Norfloxacin is considered the cheapest drug . The price of Norbactin, however, is also very affordable.
Reviews about Norbactin
Numerous reviews of Norbactin indicate that the medicine in most cases is truly effective. On the forums, many people ask whether this is an antibiotic or not, since taking such drugs is contraindicated for some. However, those who have already tried this drug note its speed.
Reviews of Norbactin report virtually no side effects. There is evidence of minor heartburn and other gastrointestinal problems, but the symptoms quickly disappear when the dosage is reduced. Reviews from doctors about this product are also mostly positive.
Is it possible to drink alcohol with antibiotics?
Drinking alcohol is not recommended in large quantities. Causes:
- This is a poison that poisons the body. It interferes with recovery and therapy. The situation worsens, leading to disorders. Poisoning and others contribute to organ deterioration.
- Depriving the body of something useful. The person does not receive nutritional components. Cell absorption deteriorates. They lose oxygen, blocking the distribution of drugs in the blood.
When alcohol interacts with antibiotics, the concentration of substances decreases. The disposal of poisons and waste is slowed down. This leads to poisoning. It is difficult to cure at home. There are following recommendations for combination:
- Co-administration promotes unintended consequences. It is recommended to wait three days before consuming alcoholic compounds. Then all harmful products will be removed from the body, which reduces reactions.
- Tablets or injections are used with wine according to medical research. Scientists do not exclude negative manifestations from abuse. Requires resource allocation internally.
- Some elements are allowed to be consumed. Some are better to avoid. Please read the instructions before starting the course. It describes the pharmacological effects.
Studies conducted on volunteers and animals have made it possible to establish what will happen if the drugs are taken together with alcohol. The result depends on the group and elements. For example, Ceftriaxone, Azalide and others block the action, enhance the effect of toxins, increasing the effect on internal organs. This causes more poisoning and decreased immunity.
The issue of compatibility arose in the 60s of the last century. In those days, they began to use antibiotics. Then we noticed the first reactions of patients:
- nausea, vomiting;
- diarrhea;
- rapid heartbeat, pressure changes;
- drowsiness;
- dizziness, pain;
- confusion of consciousness up to its loss;
- redness, allergic reactions;
- sweating
The clinical picture was similar to that suffered by people working in rubber manufacturing plants. Disulfiram was used during the work. After the shift, the workers relaxed with alcohol and went out of order, showing similar signs. After laboratory studies, scientists began to use a remedy to eliminate alcoholism. Patients developed intolerance, so they quit.
Through research, it was revealed that it is prohibited to combine vodka, beer and other things with such chemicals:
- Metronidazole. Manufacturers recommend not to use it for two days after completing the course. Then the toxic poisons are completely removed. During this time, it is prohibited to use alcohol-containing cough medicines, gargles, etc. Consequences are being observed in patients in clinics.
- Tinidazole. Used to eliminate infections, stomach upsets, or to remove pathogens. It acts according to a principle similar to metronidazole.
- Cephalosporins. They interact poorly with alcoholic drinks. Complications have been observed in people when administered intravenously using a drip in the hospital. It is recommended to avoid such combinations.
- Linezolid. Interacts only with fermented drinks: beer, sherry, wine. Increases blood pressure. Not recommended for people with hypersensitivity.
- Doxycycline. Side effects occur in chronic alcoholics who have high blood alcohol levels. It is not recommended for use by those who have liver problems.
Most antibiotic components have an adverse effect. There is a group of antibiotics that have no contraindications. These include amoxil, cephalexin, zithromax and some others. The instructions do not provide any comments regarding the interaction of the elements. Anti-cold alcohol-containing tinctures are used for therapy.
Studies confirming the danger of the combination have not been conducted. There are only observations and conclusions of doctors who deliberately did not investigate. Remember that together they damage the liver. The organ wears out faster and loses its function to utilize decay products. This causes serious side reactions that lead to complex disorders and deterioration of well-being. Some allergies can be fatal in severe cases.
Norbactin price
The price of Norbactin is about 90 rubles. This is an inexpensive and accessible remedy, which, according to reviews, is quite effective.
- Online pharmacies in RussiaRussia
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Norbactin tablets p.p.o.
400 mg 20 pcs. Sun Pharmaceutical Industries Ltd./Ranbaxy Laboratories Limited RUR 386 order - Norbactin tablets p.p.o. 400 mg 10 pcs. SUN Pharmaceutikal Industries Ltd.
RUB 222 order
Pharmacy Dialogue
- Norbactin (tab.p.pl/vol. 400 mg No. 10)Ranbaxy
RUB 222 order
- Norbactin (tab.p.pl/vol. 400 mg No. 20)Ranbaxy
350 rub. order
show more