Symptoms
Clinical manifestations of meningitis in children are determined by the virulence of the pathogen, age and state of immunity. There are some differences in symptoms and treatment methods among different age groups. Pathological changes consist of a combination of syndromes: cerebral, infectious and meningeal.
The first signs of meningococcal infection
Menigococcal meningitis develops when meningococci enter the body. In 80% of cases, children under 10 years of age become ill.
It is characterized by sudden fever, bursting headache, which is accompanied by repeated vomiting, photophobia. The child becomes lethargic very quickly. There is a decrease in the threshold of sensitivity, when even a light touch causes severe pain; in infants it manifests itself as general anxiety. In the first hours of the disease, meningeal syndromes appear.
Meningococcal infection is characterized by a forced position, when a child, lying on his back or side, throws back his head and pulls his legs towards his stomach.
Symptoms of meningitis in young children appear gradually. The child becomes restless, emits a sharp cry, vomits, and convulsions occur. There is hyperthermia, a hemorrhagic rash, and a venous network is visible on the head. On examination, the large fontanel is tense and pulsating.
It is necessary to urgently seek medical help if a child has the following symptoms and signs against a background of fever:
- tension of the large fontanelle;
- involuntary muscle twitching;
- the nature of the cry has changed;
- photophobia;
- repeated vomiting;
- constriction of the pupils, squint;
- muscle atony.
In infants, often the only symptom of infection is a bulging or pulsating fontanel.
For pneumococcal pathogens
Pneumococcal meningitis is caused by pneumococci. It ranks second in incidence after meningococcal. More often diagnosed in children under 5 years of age.
The disease with a pneumococcal pathogen has several forms, which determine the first signs of meningitis in children.
To identify meningitis in a school-age child at the initial stage, you should pay attention to the following symptoms:
- occurs in an acute form;
- body temperature suddenly rises to 39-40 C;
- intoxication increases rapidly;
- consciousness is impaired;
- pale skin, cyanosis of the nasolabial triangle, shortness of breath, arrhythmia appear;
- the child reacts negatively to light and noise;
- meningococcal syndrome is weakly or incompletely expressed.
In children under one year of age, a recurrent form is often found. It is characterized by a gradual increase in toxicosis, retraction of the large fontanel. The liver and spleen enlarge, motor activity is impaired. Relapses last from 5 to 10 days, accompanied by periodic fever and deterioration.
Tuberculous meningitis
Tuberculous meningitis is the most dangerous form of tuberculosis, which usually develops as a secondary process against the background of pulmonary tuberculosis.
The spread of infection occurs by hematogenous or lymphogenous route.
Pulmonary tuberculosis does not manifest itself in any way for a long time, which is why therapy is not carried out, and the risk of generalization of the infection increases. This risk is absent in children vaccinated in the maternity hospital with the BCG anti-tuberculosis vaccine.
Causes of meningitis in children
Children's meningitis can be primary (develop without previous signs of a pathological process caused by the corresponding pathogen) or secondary, when damage to the meninges is preceded by other manifestations of infection (mumps, measles, leptospirosis).
The following microorganisms can cause meningitis:
- bacteria (pneumococcus, meningococcus, Haemophilus influenzae and tuberculosis bacilli, spirochetes);
- viruses (enteroviruses of the Coxsackie-ECHO group, mumps and measles virus);
- chlamydia;
- mycoplasma;
- protozoa;
- mushrooms.
Meningitis most often affects children who belong to the following risk groups:
- premature;
- those born with intrauterine fetal hypoxia or as a result of difficult labor;
- with congenital or acquired immunodeficiency;
- who have undergone craniocerebral, spinal, vertebral trauma, neurosurgical operations and surgical interventions on the abdominal organs.
Children under 5 years of age are more likely to get meningitis. The risk of getting meningitis increases in children who attend preschool institutions and schoolchildren. Children who do not follow the rules of personal hygiene, swallow contaminated water when swimming in reservoirs, and eat food contaminated with rodent excrement are more likely to get sick. The causative agents of meningitis are transmitted by ixodid ticks.
There is a high risk of developing meningitis in children who have not been vaccinated against mumps, measles and rubella, or who have missed vaccinations with Haemophilus influenzae, meningococcus, or pneumococcal conjugate vaccines. When traveling to places dangerous for meningitis, children must be vaccinated no later than 2 weeks before the child’s departure.
The source of pathogens of childhood meningitis are sick people or bacteria carriers. Infectious agents can be transmitted by airborne droplets (with dust and saliva particles), contact (through dirty hands), waterborne, transmissible (through insect bites) and fecal-oral mechanisms. The entry points for infection are the mucous membranes of the upper respiratory tract and digestive organs. The causative agents of meningitis spread throughout the body in the following ways:
- hematogenous (through blood vessels);
- lymphogenous (lymph flow);
- geirogenic (with cerebrospinal fluid).
Meningitis in children is accompanied by the following pathological changes:
- increased production of cerebrospinal fluid;
- increased intracranial pressure and permeability of the blood-brain barrier;
- toxic damage to the brain substance;
- disorders of cerebral circulation, especially microcirculation;
- liquorodynamic disorder;
- hypoxia (insufficient oxygen supply) of the brain.
Eventually, swelling of the brain tissue develops. This is facilitated by the spread of the inflammatory process to the ventricles and brain matter, which is characteristic of purulent meningitis. With viral meningitis, cerebral edema is less pronounced, but the medulla is also involved in the pathological process. When the inflammatory process spreads to the brain, focal neurological symptoms appear.
Edema and swelling of the brain leads to its displacement with compression of the brain stem by the cerebellar tonsils. At the same time, the function of vital organs, especially breathing, is disrupted in children, which can lead to death. After suffering viral meningitis, most children do not develop complications. Children who have had bacterial meningitis may be retarded in mental development, and they sometimes develop impaired vision and hearing to the point of complete deafness.
How to recognize a viral infection?
Meningitis of viral etiology is seasonal, with outbreaks occurring in winter and spring. It is caused by various types of viruses: mumps, adenoviruses, enteroviruses and others.
In childhood, meningitis of mumps and enterovirus etiology is more common.
The main signs of meningitis in children 5 years old:
- temperature increase;
- stunnedness (slowing down of mental processes);
- strabismus;
- impaired movement of the eyeballs;
- convulsions.
With mumps meningitis, the clinical picture has features that make it possible to recognize the disease in a child. With this form of infection, the manifestations at different ages are somewhat different.
Hallucinations, delirium, weakness, impaired motor activity, fever are signs of meningitis in children 3 years of age and younger. There is also an increase in headaches and an enlargement of the salivary glands.
Pancreatitis, voluntary muscle movements, in boys, swelling of the scrotum, its redness are additional symptoms of meningitis in children 7-8 years old.
Typical symptoms of enterovirus infection are muscle pain, especially in the abdominal area, fever, herpetic rashes, bursting headache, and dyspeptic disorders. Simultaneously with the high temperature, redness of the face appears, with pallor of the nasolabial triangle, a polymorphic rash, symptoms of conjunctivitis, and hyperemia of the pharynx.
Meningeal signs
The meningeal symptom complex is based on muscular-tonic syndrome, which occurs due to irritation of the nerve receptors of the meninges. Main meningeal syndromes:
- Kernig. The patient lies on his back, the leg is bent at the knee at a right angle, due to strong muscle tension, it is impossible to completely straighten the limb.
- Bekhterev. It is determined by percussion of the zygomatic bone; when it is beaten, the facial muscles of the face contract, due to increased headaches.
- Mandonesi. Pressure on the eyeballs causes contraction of the facial muscles.
- Brudzinsky. The bottom symptom is that if you straighten one leg, the patient will involuntarily pull up the other limb. Upper – when trying to tilt the patient’s head to the chest, flexion of the lower extremities is observed.
- Lesage. Determined in infants. If the symptom is positive, the child, lifted by the armpits, pulls the legs towards the stomach and holds them in this position.
- Flatau. When the head is tilted forward, the pupil dilates.
- Stiffness of the neck muscles. The earliest and most permanent sign of the disease. When trying to raise the head of a patient lying on his back, a sharp resistance is felt, the action fails, or the upper part of the body rises.
The presence of meningeal signs is the main indication for lumbar puncture and cerebrospinal fluid assessment. But it doesn’t always mean meningitis; they are also typical for other infectious diseases!
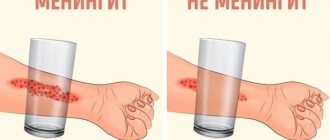
Nature of the rash
A rash with meningitis in children usually appears in the fulminant form of the disease. It consists of small pinpoint hemorrhages that appear towards the end of the 1st and beginning of the 2nd day of illness. The earlier the rash appears, the more severe the disease. It occurs on the entire surface of the skin, but is more abundant on the buttocks, eyelids, back of the legs, and thighs.
The rash has the shape of stars protruding above the skin level and is dense to the touch. In mild forms of the disease, the rash lasts no more than 2 days; in severe forms, it persists for up to several weeks.
Acute serous meningitis
Common causative agents of serous meningitis include enterovirus, mumps virus, lymphocytic choriomeningitis virus, herpes simplex virus type 2, Epstein-Barr virus, tick-borne encephalitis virus. Serous meningitis is characterized by lymphocytic pleocytosis, a moderate increase in protein and normal glucose content in the cerebrospinal fluid, a negative result of bacteriological examination, and a benign course with spontaneous recovery.
Clinically, serous meningitis is manifested by fever, headache, pain when moving the eyeballs, meningeal symptoms (usually stiff neck muscles, less often Kernig and Brudzinski symptoms), photophobia, anorexia, nausea and vomiting, myalgia, and sometimes abdominal pain and diarrhea. Acute uncomplicated viral meningitis is usually not characterized by deep depression of consciousness, persistent symptoms lasting more than 10 days, epileptic seizures, damage to the cranial nerves and other focal neurological symptoms, i.e. signs of damage to brain tissue.
When diagnosing viral meningitis, first of all, one should exclude such pathologies as purulent meningitis (especially untreated), tuberculous, fungal, mycoplasma, parasitic and parameningeal infections, neurosyphilis, leptospirosis, meningeal carcinomatosis, meningitis in non-infectious diseases (sarcoidosis, systemic lupus erythematosus), medicinal meningitis. This is often helped by examining the cerebrospinal fluid. For example, low glucose levels are more common in tuberculosis, fungal and listeria meningitis, neurosarcoidosis or meningeal carcinomatosis and are only rarely found in meningitis caused by mumps virus and lymphocytic choreomeningitis. All patients must undergo a multifaceted blood test (platelet count, liver tests, levels of urea, lipase, amylase, etc.), bacteriological tests of blood, cerebrospinal fluid, urine, feces, nasopharyngeal swabs, serological tests for syphilis and HIV infection, R-graph of the chest. For reliable diagnosis, virological and serological studies are carried out, especially polymerase chain reaction. Retrospectively, the virus can be identified by an increase in the titer of specific antibodies in the serum and cerebrospinal fluid.
Treatment of viral meningitis is symptomatic: bed rest, analgesics, antiemetics (for example, Motilium), detoxification, and sometimes tranquilizers (Seduxen). Corticosteroids are not indicated. Monitoring the sodium content in the blood is necessary - due to the threat of disruption of the release of antidiuretic hormone during hyponatremia. A repeat lumbar puncture is indicated if fever, meningeal symptoms, and headaches do not improve within a few days. If bacterial meningitis cannot be excluded, empirical antibiotic therapy is prescribed. For severe meningitis caused by herpes simplex and herpes zoster viruses, as well as the Epstein-Barr virus, acyclovir can be used.
Forecast. In adults, full recovery often occurs. Some young children may have mental developmental disorders, hearing loss and other disorders. Seizures usually do not occur. Next, we will briefly present information about various viral meningitis.
1) Meningitis caused by the Coxsackie and ECHO viruses (the abbreviation ECHO means: an orphan virus that affects the cells of the human small intestine). Mostly children (under 15 years of age) are affected, more often in the summer-autumn period. The method of infection is fecal-oral. The incubation period is from 2 to 7 days. More than 40 strains are definitely pathogenic. They can cause a number of diseases, including myalgias, spinal cord lesions (similar in clinical manifestations to polio), encephalitis, and some autoimmune complications. Enteroviral diseases often occur in the form of epidemic outbreaks.
Serous meningitis begins acutely, with a sharp rise in temperature, headache, and repeated vomiting. The temperature lasts for about a week. The appearance of patients is typical: the face is hyperemic, the nasolabial triangle is pale. Often there is conjunctivitis, injection of scleral vessels, often pharyngitis, herpetic rashes on the lips and in the nose, herpetic sore throat, maculopapular, vesicular or petechial rash, pleurodynia, myopericarditis. In the blood of many patients, a shift in the leukocyte formula to the left and an increase in ESR to 25–40 mm/h are noted.
Meningeal symptoms appear on the 2nd–3rd day of illness. Lymphocytic pleocytosis (in the first hours it may be neutrophilic), increased protein levels, and normal glucose levels are found in the cerebrospinal fluid. The virus can be isolated from feces, less often from cerebrospinal fluid, nasopharynx. The titer of antiviral antibodies in serum and blood increases when studying paired samples.
The course of enteroviral meningitis is favorable and ends with recovery. Within 2 weeks - 1 month, however, there may be relapses (10–40% of cases): deterioration of the general condition, rise in temperature, increased headache, and sometimes vomiting. Inflammatory changes in the cerebrospinal fluid are again detected.
2) Meningitis caused by the mumps virus . Mostly children of preschool and school age are affected; boys are 3 times more likely than girls. Infection, hypothetically, occurs through airborne droplets. Most often they get sick in late autumn or early spring. The incubation period lasts about 3 weeks. Within 10 days after the onset of mumps symptoms, the patient is a source of infection.
Inflammation and swelling of the salivary glands are most often accompanied by meningeal symptoms on the 3rd–5th day (this can happen a month later, or earlier - before the glands become swollen). Mumps meningitis sometimes develops without clinical manifestations of mumps. It is believed that the early forms of mumps meningitis occur during the introduction of the virus from the blood into the central nervous system; the later forms are based on a neuroallergic process. From the blood, the virus can spread to other organs, causing, for example, pancreatitis or orchitis.
Mumps meningitis develops acutely with a rise in body temperature to 39–40°C, severe headache, and repeated vomiting. Meningeal symptoms are moderate. There may be meningism without meningitis, asymptomatic meningitis. Young children develop general weakness, drowsiness, adynamia, less often - agitation, delirium, hallucinations, rarely - confusion and depression of consciousness, generalized epileptic seizures.
In the diagnosis of the disease, a prominent place belongs to the study of cerebrospinal fluid. Pleocytosis (hundreds, sometimes thousands of cells) is detected in the cerebrospinal fluid; in the first days of the disease, lymphocytes predominate, there may also be neutrophils, and subsequently - exclusively lymphocytes. The amount of protein is slightly increased, sometimes normal, glucose is not changed, in 10% of patients it is moderately reduced. During recovery, the cerebrospinal fluid is sanitized within 2 weeks, less often - over a longer period. Clinical symptoms disappear on the 7th–10th day. In 1–5% of cases, signs of brain tissue damage are detected. Complications include pancreatitis (15%) and especially orchitis (in boys over 10 years of age). Pancreatitis is characterized by pain most often in the upper left quadrant of the abdomen, radiating to the back, and repeated vomiting; orchitis - pain and swelling of one of the testicles, hyperemia and swelling of the scrotum, increased body temperature. By the 10th–12th day, these symptoms disappear, but in some cases, orchitis leads to infertility.
The nature of meningitis can be determined most quickly by the fluorescent antibody method; more time is required for the hemagglutination inhibition reaction. Treatment is symptomatic; for orchitis, local treatment is prescribed; for pancreatitis, traditional treatment regimens are used.
3) Acute lymphocytic choriomeningitis . A rare neuroinfection, its reservoir is gray house mice. Infection occurs through the oral route. Mostly people aged 20–35 years are affected. The course of the disease is benign. The etiology of meningitis is determined by isolating the virus from the blood and cerebrospinal fluid, the neutralization reaction and complement fixation, and in urgent cases - by the method of fluorescent antibodies.
4) Meningitis due to herpetic infection . The causative agent is herpes simplex virus type 2 (HSV-2), as well as varicella zoster and herpes zoster viruses. HSV-2 is the causative agent of genital herpes. Aseptic meningitis occurs in 16% of cases against the background of vesicular rashes in the genital area, as well as complaints of difficult and painful urination, radicular pain in the lower back, paresthesia and anesthesia in the anogenital area. Lymphocytic pleocytosis is detected in the cerebrospinal fluid.
Meningitis caused by the herpes zoster virus is manifested by a body temperature of up to 38–39°C and relatively mild meningeal symptoms. Confusion, depression of consciousness and cerebrospinal fluid syndrome occur extremely rarely; meningitis is often asymptomatic. Treatment with acyclovir (5 mg/kg IV drip 3 times a day for 5 days) is indicated.
Complications of herpes zoster include lesions of the eyeballs, postherpetic neuralgia, cranial nerve palsies, myelitis, meningoencephalitis, as well as contralateral hemiparesis associated with ophthalmic herpes. Hemiparesis occurs due to vascular damage (granulomatous angiitis of the meningeal and cerebral arteries, most often the middle cerebral artery and its branches) and cerebral infarction. Infarction of the cerebellum and occipital lobe with ophthalmic herpes and infarction of the brain stem with cervical localization of herpes have been described. Hemiparesis occurs between 1 week and 6 months after the onset of the disease. Half of these patients experience depression and confusion. Rarely, hemiparesis is accompanied by hemianesthesia, hemianopsia, and cerebellar symptoms. The diagnosis of cerebral infarction is verified using CT or MRI.
5) Meningitis in infectious mononucleosis . Caused by the Epstein-Barr virus, it occurs mainly in children and young people and manifests itself in damage to the lymph nodes, liver, spleen and skin. Involvement of the central nervous system with symptoms of meningitis and encephalitis is noted in 1–5% of cases. Crucial in diagnosis is the detection of leukocytosis in the blood with an increase in the number of lymphocytes and the appearance of abnormal mononuclear cells (atypical lymphocytes). Treatment is symptomatic.
6) Meningitis in cat scratch disease . The causative agent is Bartonella henselae. In 60% of cases, people aged 5–21 years are affected. 3–10 days after the scratch, general infectious symptoms appear, and after 2 weeks regional lymphadenopathy appears. Damage to the nervous system is detected 1–6 weeks after the onset of adenopathy and occurs in the form of serous meningitis, encephalitis, radiculopathy, myelopathy, and neuroretinitis. Moderate lymphocytic pleocytosis and increased protein content are detected in the cerebrospinal fluid. In severe cases of the disease, confusion and depression of consciousness, seizures are observed; lesions of the cranial nerves, aphasia, hemiparesis, and ataxia are less common. The acute period lasts 1–2 weeks, over 1–6 months there is a gradual restoration of impaired functions, in 90% it is complete. Cognitive impairment and seizures persist for a long time. Treatment uses erythromycin or doxycycline, sometimes in combination with rifampicin; the effectiveness of antibacterial therapy is considered unproven.
7) Benign recurrent serous meningitis of Mollare .
Etiology – hypothetically, herpes simplex type 2, epidermoid cysts, histoplasmosis. The disease occurs at any age, manifesting itself in spontaneous and short (1-3 days) attacks of nervous and mental disorders for 2-5 years. During an attack, rigidity of the neck muscles, Kernig's and Brudzinski's symptoms are detected. There may be transient neurological symptoms (seizures, diplopia, dysarthria, anisocoria, pathological foot signs, etc.), confusion and depression of consciousness. Fever is moderate, but sometimes reaches 40°C. Lymphocytic pleocytosis is detected in the cerebrospinal fluid (in the early stages of the disease it can be neutrophilic), a slight increase in protein, and normal glucose levels. Mollare's meningitis is differentiated from recurrent bacterial, viral and fungal meningitis and sarcoidosis, echinococcal (hydatid) cyst, intracranial tumors, Behçet and Vogt-Koyanagi-Harada syndromes (in the latter two cases, severe lesions of the skin and eyes are observed). Relapses of Mollaret's meningitis are treated with colchicine, glucocorticoids or non-steroidal anti-inflammatory drugs. The prognosis is favorable. Il progetto Icon che vede l'incontro tra Disaronno e la hogan outlet grande moda italiana arriva al suo quarto anno e lo fa outlet hogan online con una nuova limited edition esclusiva. Dopo aver hogan outlet vestito la sua iconica bottiglia con creazioni hogan outletfirmate da Moschino, Versace e Cavalli, il liquore italiano hogan outlet “Il Paisley, emblema dell'Albero della Vita e shogan outletinuosa palmetta del disegno cachemire da cui fiorisce la tradizionehogan outlet Etro, non rappresenta soltanto la Palma da dattero sac longchamp pas cher che forniva cibo e riparo, ma anche un collegamento sac longchamp pas cher iconografico tra Oriente ed Occidente attraverso golden goose outlet saldi le sue migrazioni culturali, dalle stampe indianegolden goose outlet saldi ai ricami celtici. ” ha detto Veronica Etro. “La nuovapjs pas cher bottiglia Disaronno Limited Edition si veste e sinike tn pas cher colora di paisley, esplorando i valori tradizionali legati all'arte del disegno realizzato a mano, come un tradizione e contemporaneamente della sperimentazione, per pjs pas cher ricercare soluzioni nuove ed originali.”La sac goyard pas cher limited edition Disaronno Wears Etro, acquistabile a partire da ottobre, sostiene la charity Fashion 4 Development, patrocinata dalle Nazioni Unite e piumini moncler outlet a cui anche quest'anno ILLVA Saronno devolverà barbour paris pas cher parte del Ricavato delle vendite, offrendo un barbour paris pas cher contributo tangibile allo sviluppo di numerosi interventi umanitari in Africa. L'evento di presentazione della nuova edizione limitata si è tenuto ieri sera agolden goose outlet saldi Milano presso la boutique Etro in Via Monte golden goose outlet saldi Napoleone, dove Veronica Etro e Augusto golden goose outlet saldi Cara Delevingne has succeeded where many have failed in making the transition from full-time supermodel to professional actress, and now a documentary entitled The Cara Project, will explore just how she has done it. The program, which has been acquired by golden goose outlet saldi Revolver Entertainment, will be released piumini moncler outlet on DVD in the coming months, reports Variety, as well as being offered for sale to broadcasters at Mipcom and AFM next month. Details of the contents are scarce, piumini moncler outlet Delevingne's meteoric rise to fame saw her become piumini moncler outlet the most sought-after catwalk and campaign modelsac longchamp pas cher of her generation, walking for every major sac longchamp pas cher fashion house and amassing over 36 million sac longchamp pas cher Instagram followers in the process. Her hogan outlet filmography – given that her first film of note hogan outlet came out in 2015 – is no less impressive. Shehogan outlet has Paper Towns, Pan, Kids In Love and Suicide Squad already under her belt, and has London Fields, Tulip Feverand
How does it manifest in newborns?
Many parents are interested in the question of how meningitis manifests itself in infants, because they cannot make complaints, and the disease is dangerous and poses a threat to life.
Meningitis in newborns is accompanied by characteristic symptoms:
- dyspepsia;
- monotonous scream;
- hyperexcitability;
- frequent regurgitation;
- twitching of hands and chin;
- vomit;
- throwing back the head;
- loss of appetite;
- low-grade fever;
- increased muscle tone.
The same symptoms occur after severe birth injuries and hypoxia, so an accurate diagnosis is made only after examining the cerebrospinal fluid.
The disease in newborns and children in the first months of life occurs with severe intoxication, muscle hypotonia, respiratory failure, and repeated convulsions are possible.
How to prepare for going to the doctor?
To go to the doctor, you don’t need to make any extensive preparations; on the contrary, if there are symptoms of meningitis , you shouldn’t put off going to the doctor, in this case you need to react immediately. Just remember all the signs that you had and tell your doctor about them. This will help make a correct diagnosis. You can't ignore these signs. Signs of meningitis in an adult can appear within a couple of hours, so urgent help is needed to avoid complications and even death.
Can it be determined during the incubation period?
The incubation period for bacterial meningitis lasts 2–7 days, for a viral infection it lasts 2–4 days. In infants it may be less than a day. Its duration largely depends on the state of the child’s immunity; the stronger it is, the longer there are no clinical manifestations.
It is very difficult to determine the disease during this period. Clinical manifestations are very vague or completely absent. But parents should pay attention to changes in the child’s behavior: sudden drowsiness, lethargy, increasing headache, nausea, loss of appetite - may be the first signals of a dangerous infection.
How can you get infected?
If you are interested in how you can become infected with meningitis, then first you should know about the way the infection multiplies. The methods of its reproduction are different, but the most common are:
- Airborne (the patient may sneeze and cough).
- Contact and household (personal hygiene rules are not followed).
- Oral-fecal (eating unwashed foods or eating with unwashed hands).
- Hematogenous (infection occurs through blood).
- Lymphogenic (infection through lymph).
- Placental (at the time of pregnancy and birth of a child from mother to her fetus).
- If a person bathes in dirty water, the infection enters the body.
The incubation period for this disease ranges from 2 to 4 days, this period from infection to the first signs. But sometimes it lasts a couple of hours or, on the contrary, it takes up to 20 hours. It is also important to consider that the disease can be primary and secondary. The first option is an independent disease. The second is a consequence of the fact that there is already an infection in the body, for example, a person suffers from influenza, otitis media, tuberculosis.
meningitis symptoms
If it is serous meningitis, then it is considered contagious. If the disease is secondary, then other people will not become infected with it.
Treatment
If meningitis is suspected, urgent hospitalization to the infectious diseases department is indicated.
For bacterial meningitis, treatment includes:
- antibacterial therapy;
- anticonvulsants;
- non-steroidal anti-inflammatory drugs;
- detoxification therapy;
- antihistamines;
- corticosteroid hormones.
Treatment of meningitis of viral etiology does not require antibiotics. Recombinant interferon, acyclovir, and immunomodulators are used. Infusion and desensitizing therapy are also carried out. After receiving the results of bacteriological culture, therapy is adjusted depending on the pathogen.
The duration of treatment depends on the clinical course of the infection. For meningococcal meningitis, antibiotic therapy lasts 6-10 days, for other etiologies 8-14 days. Treatment begins with intravenous administration of antibiotics and continues until the temperature drops persistently, then switches to oral administration or intramuscular injections of drugs.
Consequences
Severe consequences of meningitis are more often recorded in young children and with delayed treatment.
If the diagnosis is not made on time and therapy is delayed, dangerous complications develop: sepsis, endocarditis, pneumonia, abscess or cerebral edema.
The most common consequences of meningitis suffered in childhood:
- hydrocephalus;
- mental retardation;
- epileptic seizures;
- paresis;
- decreased or loss of hearing;
- damage to the cranial nerves.
Even with a successful outcome, after discharge the child experiences asthenoneurotic conditions: sleep disturbance, anxiety, headaches, memory loss, fatigue.
Why is meningitis dangerous?
Meningitis is expressed in the rapid inflammation of the membrane of the brain, under which serous fluid accumulates. If misdiagnosed, untimely access to doctors and improper treatment, the disease can lead to cerebral edema and result in disability or even death.
Unlike purulent meningitis, serous meningitis is not accompanied by massive death of nerve cells. Therefore, the chances of recovery and a favorable outcome with the serous type of the disease are higher.
Serous and purulent types of meningitis at the cellular level are diseases of opposite nature. It is very difficult to distinguish them externally. In fact, there is only one reliable diagnostic method - lumbar puncture of the cerebrospinal fluid and its subsequent analysis.
Prevention measures
Prevention of meningitis depends on the etiology. Patients are urgently hospitalized and isolated. Persons in contact with the sick person are examined for carriage and observed for 10 days.
To prevent a dangerous disease, immunization is carried out. There are several vaccines, both foreign and Russian. For example, the imported vaccine against pneumococcal meningitis “Prevenar” is approved for children from 3 months of age. Well tolerated and does not cause side effects. After completing the full course of vaccination, by the age of two years the child develops stable immunity.
Vaccinations against meningococcal infection are carried out with the Russian vaccine from 1.5 years, and the American vaccine from 2 years.
Vaccination is not included in the scheduled vaccination calendar; it is carried out according to indications or at the personal request of the parents.
Who is at risk?
A key factor contributing to the onset of meningitis is a weak immune system. It is the body’s defense against various infections. Human immunity becomes weak due to:
- previously suffered infectious diseases (respiratory, pneumonia, pharyngitis, influenza, sore throat),
- chronic pathologies, especially syphilis, HIV, tuberculosis, liver cirrhosis, severe stress,
- vitamin deficiency and strict diets,
- head and back injuries,
- total hypothermia of the body,
- alcohol and drug abuse,
- long-term use of tablets with non-compliance with recommendations.
All this can cause infection in a person, as the body becomes weak.