Gonorrhea is a disease of men and women, transmitted mainly through sexual contact. The forms of the disease can be different. Basically, the symptoms are erased, that is, unclear, so the disease is not treated in time. Lack of treatment is known to lead to complications. In addition, while a person is sick, he infects everyone around him with whom he has unprotected sexual intercourse.
- Epidemiology
- Classification
- Symptoms
- Chronic gonorrhea
- Complications of gonorrhea
- Diagnostics
- Prevention
- Treatment
It is necessary and mandatory to treat gonorrhea in women. Because its main and saddest result can be infertility - the inability to conceive a child.
What is gonorrhea?
Gonorrhea is an infectious disease that is sexually transmitted.
Popularly called gonorrhea or “hussar runny nose,” men with gonorrhea often experience characteristic discharge from the penis. The disease affects men more often, but also occurs in women and newborns. The main signs of gonorrhea are pain and burning when urinating, unusual green-yellow purulent discharge from the genital tract, and redness of the genitals. But the disease can occur without symptoms.
Causes of occurrence, causative agent
Gonorrhea is caused by the bacterium Neisseria gonorrhoeae (gonococcus). It primarily affects the urethra (causing urethritis) and the cervix (causing cervicitis), less often the rectum, mucous membrane of the throat and eyes, causing inflammation.
The causative agent of infection
Gonorrhea occurs when Neisseria gonorrhoeae invades the mucous membranes of the genital organs.
These are gram-negative diplococci that multiply in environments with access to oxygen. Due to their protective properties, gonococci can survive in neutrophils and change their properties under the influence of external factors. The main form of modification under adverse influences is the transformation of surface proteins. It is these protective properties that explain the resistance of gonococci to some antimicrobial drugs. After entering the body, gonococci enter the submucosa, where they are quickly absorbed by neutrophils. Special surface structures and enzymes of the bacterium prevent phagocytosis and allow gonococci to survive inside cells. Often, invasion of Neisseria gonorrhoeae causes secondary infections caused by chlamydia, trichomonas and other pathogenic microorganisms.
Routes of infection
Gonorrhea is a sexually transmitted disease; it is transmitted from person to person through unprotected sexual intercourse: through contact with areas affected by the bacterium (genitals, anus, mouth).
Important! The bacterium is not found in seminal or vaginal fluids, but directly on the surface of the genitals. Interrupted sexual intercourse does not reduce or eliminate the risk of contracting gonorrhea.
The infection can enter the rectum during anal intercourse, and into the throat during oral intercourse. Through the oral cavity of a person with gonorrhea, the bacteria can be transmitted to his healthy partner.
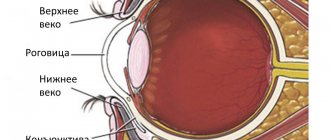
In newborns, gonorrhea is detected if the bacterium was in the mother's body during childbirth. Infection occurs when a child comes into contact with the fallopian tubes and uterus. Moreover, the bacterium most often affects the eyes of newborns, causing gonorrheal conjunctivitis (blennorrhea).
Since the bacterium is not able to exist outside the human body (that is, outside the host cell), it is impossible to become infected with gonorrhea in public places, swimming pools and toilets. Gonorrhea is also not airborne.
Is gonorrhea transmitted through towels or dishes?
It is very rare for bacteria to be transmitted through a towel. To do this, an infected person must use a towel on the mucous membrane affected by the bacterium. Then a healthy person must transfer the secretions from the towel to his own mucous membrane. Considering that the bacterium quickly dies outside the human body, this must be done quickly. It turns out that you can get infected through a towel only if you do it on purpose. Therefore, doctors say that infection does not occur through towels, dishes and cutlery.
Who is at risk?
At risk of contracting gonorrhea are people who have unprotected sex (without using a condom):
- sex workers and their clients;
- people who have same-sex unprotected sex (men who have sex with men and women who have sex with women);
- people who frequently change sexual partners.
You can get gonorrhea again if you have contact with a sick person. The risk of infection increases in the presence of other sexually transmitted diseases (chlamydia, syphilis, etc.).
What determines the risk of infection?
The main risk factors are associated with intimacy without the use of barrier contraception, as well as oral sex with an infected partner. At a young age from 18 to 25 years, the risk of getting sick increases due to a surge in hormonal activity and riskiness during sexual intercourse.
The following can lead to infection with gonorrhoea:
- diagnosis of the disease in the anamnesis;
- having promiscuous sex life;
- intimacy with a new sexual partner;
- infection of a woman's birth canal.
A child can become infected due to an attempted violent action on the part of an adult who is a carrier of the infection.
The risk group for gonorrhea includes prostitutes and their clientele, tourists, and people leading an immoral lifestyle.
Types of disease, classification
Gonorrhea can affect more than just the genitourinary system, although urogenital infection is the most common. There are:
- Urogenital infection: in men, inflammation occurs in the penis, scrotum, prostate, in women - in the cervix, vagina and pelvic organs (Fig. 1).
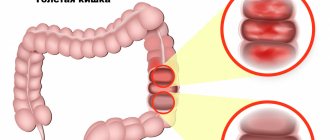
- Rectal gonorrhea: bacteria enter the body during anal sex. Symptoms include itching, bleeding, bowel movements (constipation, diarrhea).
- Gonococcal infections of the pharynx (gonococcal pharyngitis): the cause is oral sex. There may be no symptoms, but infection can lead to a sore throat.
- Disseminated gonorrheal infection (arthritis-dermatitis syndrome): The infection affects the skin and joints. Red spots appear on the skin, joints swell. One type of infection is gonorrheal septic arthritis.
- Gonorrheal conjunctivitis (blennorrhea): occurs when fluid contaminated with bacteria gets into the eyes. The result is swelling and redness.
- Fitz-Hugh-Curtis syndrome (venereal perihepatitis): inflammation of the pelvic region and liver, accompanied by pain in the right upper abdomen with nausea, vomiting and fever.
Figure 1. Common development of urogenital infection in gonorrhea. A - urethritis, inflammation of the urethra in men. B - cervicitis, inflammation of the uterus in women. Source: CC0 Public Domain
How is the bacterium transmitted?
Gonococci are spread mainly through sexual contact. This can be oral, anal or vaginal sex. Due to its asymptomatic course and high degree of contagiousness, the bacterium can be transmitted to the patient’s sexual partners for a long time. At the same time, the previous disease does not determine acquired immunity - a person can become infected with gonorrhea again. Because of these properties, gonococcal infection is one of the most common sexually transmitted diseases.
Other methods of infection:
- Household transmission of infection through the use of contaminated personal hygiene items.
- Transfer of bacteria into the child's body during pregnancy or childbirth. This method of infection often causes eye damage in infants.
- Self-infection is the transfer of infectious agents from the mucous membrane of the genital organs to other parts of the body.
In the external environment, gonococci die quickly, so household transmission is rarely recorded. Possible risk factors that increase the likelihood of infection include promiscuity, unsafe sex, and a history of gonococcal infection in the past. Also, the risk of infection increases significantly if one of the sexual partners has HIV infection.
Get tested for gonorrhea
Gonorrhea symptoms
The course of the disease may be completely invisible to the infected person.
The first signs of the disease
The first symptoms of gonorrhea may appear only 2 weeks or several months after unprotected sex with an infected partner. Sometimes signs of the disease appear earlier - on the third or fifth day after infection. Typically, the genitals become red, there is a burning sensation and discomfort that increases with urination.
Further symptoms vary depending on the type of gonorrhea.
Symptoms in women
In women, symptoms appear within 10–14 days:
- burning, pain when urinating;
- unusual vaginal discharge: it may have a denser structure than usual, be purulent or watery, with a green or yellowish tint;
- spotting before or after menstruation;
- more rarely: pain in the lower abdomen, blood after sex, menstruation may be more severe (heavier discharge).
It should be remembered that in half of women with gonorrhea, the disease is asymptomatic.
Symptoms in men
In men, symptoms manifest themselves 2–14 days after unprotected intercourse (Fig. 2):
- urination disorders: pain, burning, discomfort, incontinence, frequent urge;
- unusual discharge from the glans penis, often purulent, green or yellowish;
- redness and swelling of the glans penis;
- more rarely: pain in the scrotum, swelling.
Every tenth man infected with gonorrhea does not show any symptoms.
Figure 2. Common symptoms of urogenital infection when infected with gonorrhea in men and women. Source: Verywell
Symptoms of infection of the skin, eyes, rectum
Gonorrhea on the skin (arthritis-dermatitis syndrome) manifests itself in the form of red pus-filled dots. They are accompanied by fever and severe joint pain. The joints are swollen and the skin around the ankles, wrists or knees is red.
For rectal gonorrhea, symptoms include itching, bleeding, constipation, or diarrhea.
Gonorrhea of the throat mucosa may not manifest itself in any way, but in the future it can cause gonorrheal sore throat.
Gonorrheal conjunctivitis (blennorrhea) is expressed in redness and swelling of the eyes.
Gonorrhea on the skin. Photo: PHIL CDC
Symptoms in newborns
During childbirth, gonorrhea can be passed on to the baby. In newborns, signs of the disease include red and swollen eyes with purulent discharge.
As a preventative measure, the doctor may prescribe antibiotics to the mother before the baby is born. After birth, the baby is given an antibiotic intravenously and the eyes are washed with saline.
How to cure itching and burning of the vulva? Is it always gonorrhea?
How to cure itching and burning of the vulva
Disease, infection or maybe a common allergy? Before you begin to treat itching or burning of the vulva on your own, make sure that you do not suffer from, for example, vaginal mycosis or sexually transmitted diseases. In this case, it is necessary to consult a doctor as soon as possible.
Itching and burning in the intimate area is a common female ailment. This is not always due to a bacterial infection or poor hygiene. Although these symptoms are usually relatively harmless, they are a warning sign - be sure to find out the causes of this unpleasant condition before starting any treatment on your own.
Before you decide to get rid of vulvar itching and burning with home remedies, you need to make sure that the unpleasant symptoms are not associated with a bacterial infection or disease. The most common infection is athlete's foot, estimated to affect up to 75% of women. It is caused by yeast-type fungi, and, in addition to itching and burning, its characteristic symptoms are white or yellowish discharge with a curd-like consistency.
However, mycosis is not the only disease of the intimate organs. If, in addition to itching and burning of the vulva, you notice symptoms such as: vaginal discharge of an unusual appearance or odor, vaginal dryness, burning of the urethra, painful urge to urinate, rashes or erythema spots, contact your gynecologist. As soon as possible. These could be signs of a sexually transmitted disease such as gonorrhea or trichomoniasis, as well as psoriasis, diabetes and even vulvar cancer.
Diagnosis of gonorrhea
Diagnosis and treatment of gonorrhea should be taken seriously. Even if gonorrhea does not manifest itself in any way, a person is still a carrier of the infection.
When the first symptoms appear, as well as in the absence of confidence in your partner or after unprotected sexual intercourse, you should immediately visit a venereologist (dermatovenerologist).
What tests are needed?
To determine gonorrhea, the doctor takes a smear from the mucous membrane of the penis or urethra in a man and, accordingly, from the mucous membrane of the cervix in women.
Then the doctor sends the smear for examination. To identify the pathogen, use:
- PCR method (polymerase chain reaction, bacterial DNA is detected in the sample);
- cultural method (bacteriological seeding);
- Gram staining method.
Since gonorrhea promotes infection with other sexually transmitted infections, doctors advise testing for mycoplasma, trichomonas and chlamydia.
Each method for diagnosing gonorrhea has its pros and cons.
PCR method
The most sensitive and widely used approach is the PCR method. Used to analyze a smear from the genitals, throat, rectum, as well as to examine a urine sample.
In addition to gonococci, mycoplasma and chlamydia are detected by PCR. You can get the result the very next day.
Gram staining method
The second method, Gram staining, is quite simple and quick. The sample taken is exposed to dyes and then the result is studied under a microscope (Fig. 3).
Figure 3. Diagnosis of gonorrhea, Gram stain. The preparation is sequentially stained with dyes. As a result, the bacteria Neisseria gonorrhoeae acquire an orange-red color against the background of the purple color of the cellular elements.
This method is used to diagnose gonorrhea in men with damage to the urethra. It is not effective for infections of the throat, cervix and rectum, since its result in this case is often unreliable.
The Gram stain method also does not detect the presence of other pathogens - mycoplasma and chlamydia.
Culture method
The culture method involves placing a sample in a special vessel and culturing it. Bacteria form colonies. The isolated pure bacterial colony is identified by microscopy using Gram stain.
The main advantage of this method is that it allows you to identify bacteria to various antibiotics. Among the disadvantages are the duration of the study (about 3 days) and strict adherence to the rules for taking samples and transporting the material. At the slightest disturbance of the environment in which the bacteria are placed, the analysis may give a false result.
The culture method is used to analyze samples from the throat, rectum and in arthritis-dermatitis syndrome, when fluid from the joints is sent to the laboratory.
Important! To obtain a reliable result, you must follow the rules for preparing for the study. Stop taking any antibiotics 2 weeks in advance, as they may affect the results. Tests are not taken during menstruation (the ideal time is 5 days before or 5 days after menstruation).
What is a provocative test?
After the patient has undergone treatment and repeated tests are negative, doctors may resort to a provocative test.
This test involves irritating the bacteria so that it manifests itself again.
After all, not fully cured gonorrhea can penetrate deep into the body, and it will no longer be possible to detect it on the mucous membranes using a smear.
The following methods are used for this:
- chemical (use a silver solution for the urethra or Lugol's solution for the rectum);
- thermal (warming up tissues using electrotherapy);
- nutritional (when the patient eats spicy and salty foods to irritate the bacteria);
- physiological (check to see if the bacteria will manifest itself during a hormonal surge in women before and during menstruation);
- biological (the doctor administers the gonococcal vaccine and pyrogenal).
Publications in the media
Gonorrhea is an infectious disease caused by gonococci of the genus Neisseria and transmitted sexually. Frequency. The incidence in Russia in 2001 was 108.7 per 100,000 population. The predominant age is 15–35 years.
Etiology. The causative agents are Neisseria gonorrhoeae - gram-negative diplococci 1.25–1.6 µm long and 0.7–0.8 µm in diameter. Currently, from 60 to 100 strains of gonococcus are identified. Can form L-forms. Certain strains of gonococci produce b-lactamase (an enzyme that destroys penicillin).
Genetic aspects. In patients with congenital deficiency of late components of the complement system (C7, C8, C9), the frequency of generalization of local forms of gonococcal infection is increased.
Risk factors • Promiscuous sex life • Rare use of barrier methods of contraception (condoms) • Newborns - infection of the mother's birth canal • Children - attempts at sexual violence by an infected person • The presence of a focus of gonococcal infection in the body - autoinoculation (for example, bringing the infection into the eye with your hands) • For inflammatory diseases of the pelvic organs - use of an IUD.
Risk groups: prostitutes and their clients, businessmen, tourists, drug addicts, etc.
Pathogenesis. Routes of infection: more often sexual, less often household (through personal hygiene items). Newborns become infected when passing through the birth canal of a sick mother. The incubation period is from 1 day to 1 month (on average 2–5 days). The infection affects the genitourinary organs, lined with columnar and transitional epithelium; urethra, cervix, lower third of the rectum, conjunctiva. Mucous membranes lined with stratified squamous epithelium (vagina, pharynx) are involved in the pathological process only under special conditions (trauma, hormonal changes, immune disorders). Gonococci are able to penetrate the blood, causing transient bacteremia, but only in exceptional cases can they disseminate with the formation of gonococcal metastases in various organs or with the development of sepsis.
Pathomorphology • Exudate is typical, including polymorphonuclear leukocytes • In inflammatory diseases of the pelvic organs - desquamation of the ciliated epithelium of the fallopian tubes. The fallopian tubes, pelvic peritoneum and ovaries may be connected to each other by dense fibrous adhesions or a formed abscess.
Classification • By localization •• Gonorrhea of the lower parts of the genitourinary tract without complications •• Gonorrhea of the lower parts of the genitourinary tract with complications •• Gonorrhea of the upper parts of the genitourinary tract and pelvic organs •• Gonorrhea of other organs • Along the course •• Fresh gonorrhea (disease duration - up to 2 months): acute, subacute, torpid •• Chronic gonorrhea (disease duration is more than 2 months), from the very beginning it proceeds torpidly, exacerbating under the influence of provoking factors.
Clinical picture. Gonococcal infection does not have characteristic clinical features that distinguish it from other urogenital infections and is very often combined with chlamydia (in 30–60% of cases), trichomonas, ureaplasma and other infections.
• Gonorrhea in men occurs in the form of anterior and total urethritis. For diagnosis, the Tampson test is used: the patient releases urine in 2 glasses successively; cloudiness, purulent threads and flakes only in the first glass indicate the presence of anterior urethritis; with total or posterior urethritis, the urine becomes cloudy from pus in both portions •• Anterior acute (fresh) urethritis: pain during urination, profuse purulent discharge, hyperemia and swelling of the urethral sponges •• Subacute urethritis: pain during urination decreases, small serous-mucosal lesions are noted predominantly morning discharge, less severe hyperemia of the urethral sponges •• Torpid urethritis is asymptomatic; they notice scanty discharge or sticking of the urethral sponges in the morning, often not noticed by patients at all; when the process spreads to the posterior part of the urethra, frequent urge to urinate and increased pain occur •• Chronic gonorrheal urethritis occurs torpidly or asymptomatically. It is characterized by local focal lesions of the urethra caused by metaplasia of the cylindrical epithelium (soft and hard infiltrates of the urethra), as well as inflammation of the mucous glands of the urethra, Morgagni lacunae, and colliculi, which are identified by the urethroscopic method. Complications often occur: balanoposthitis, cooperitis, prostatitis, vesiculitis, epididymitis •• Gonorrheal cooperitis - inflammation of the bulbourethral (Cooper's) glands. There is a feeling of heaviness and aching pain in the perineum. In the acute stage: increased body temperature, pain, dysuric phenomena. The diagnosis is made by rectal examination •• Gonorrheal prostatitis (catarrhal, parenchymal, follicular) is often chronic, less often acute. A feeling of heaviness in the perineum, weakening of erection, and premature ejaculation are noted. In the acute stage - fever, dysuric phenomena. Palpation determines the enlargement and tenderness of the prostate gland •• Gonorrheal vesiculitis (inflammation of the seminal vesicles in combination with prostatitis and epididymitis). The course is often asymptomatic. The diagnosis is made on the basis of palpation of the seminal vesicles and examination of their contents. •• Gonorrheal epididymitis (inflammation of the epididymis) is manifested by high body temperature, swelling and severe pain of the affected epididymis, redness and swelling of the scrotum.
• Gonorrhea in women is characterized by multifocality and in 75–85% of cases asymptomatic course. Taking into account the structural features of the genitourinary organs in women, gonorrhea of the lower section is distinguished (urethritis, bartholinitis, vestibulitis, cervicitis and endocervicitis) and ascending gonorrhea (endometritis, metroendometritis, salpingitis, salpingoophoritis, pelvioperitonitis) •• Gonorrhea of the lower section ••• Urethritis is detected in 90% cases. It often occurs torpidly, less often acutely and subacutely. In the acute stage, patients complain of pain when urinating, in the chronic stage there are no complaints ••• Bartholinitis is inflammation of the large glands of the vestibule of the vagina, often bilateral. It begins with the excretory duct. When a secondary infection occurs, a true or pseudo-abscess of the Bartholin gland develops. ••• Endocervicitis is inflammation of the cervix, the most common manifestation of gonorrhea. During an acute process, patients complain of pain; the vaginal part of the cervix is swollen, hyperemic, discharge is observed from the cervical canal, and bright red erosion is observed around the pharynx. In the chronic process, follicular erosion is detected, cysts of the cervical glands are visible, the discharge is less abundant •• Ascending gonorrhea is characterized by the involvement of the internal genital organs in the process, often develops in the postpartum period and after abortion ••• Gonorrheal endometritis. Both the basal and functional layers of the endometrium are involved in the inflammatory process. Characterized by hyperpolymenorrhea. In the acute stage - pain in the lower abdomen, increased body temperature ••• Gonorrheal salpingoophoritis is often bilateral. I am worried about pain in the lower abdomen and menstrual irregularities. In the acute stage - increased body temperature, pain on palpation. Symptoms of pelvic peritonitis may join ••• Gonorrheal pelvioperitonitis is the result of the transfer of infection from the uterine appendages to the pelvic peritoneum, and has a pronounced tendency to be delineated (spread peritonitis is an exception). More often it occurs acutely: abdominal pain, increased body temperature, symptoms of peritoneal irritation in the lower abdomen. During vaginal examination, signs of bilateral salpingoophoritis, bulging of the posterior vaginal vault, and severe pain on palpation are determined.
• Gonorrhea in children •• Gonoblenorrhea - gonococci enter the conjunctiva of the eyes when passing through the birth canal of a sick mother •• Gonorrheal vulvovaginitis in girls occurs when passing through the birth canal of a sick mother or using common hygiene items. At an older age, infection often occurs as a result of depraved acts of adults.
• Extragenital gonorrhea is often combined with gonorrhea of the genitourinary organs •• Gonorrheal proctitis - damage to the lower third of the rectum; observed in women and girls with gonorrhea, as well as in homosexual men. Subjective sensations are often absent, only sometimes itching, burning, and slight pain during bowel movements are noted. During rectoscopy, swelling and hyperemia of the mucous membrane, purulent discharge are determined •• Oropharyngeal gonorrhea is manifested by damage to the tonsils and pharynx: hyperemia and edema, sometimes purulent plaque appears on the tonsils •• Eye gonorrhea in adults is recorded due to poor personal hygiene: swelling of the eyelids, conjunctival hyperemia, suppuration , photophobia.
Research methods • Gram staining of exudate of infected mucous membranes (in men, smears are taken from the urethra and rectum, in women - from the urethra, cervical canal and rectum) - freely lying accumulations of gram-negative diplococci, accumulations of neutrophils in the cytoplasm •• In men with clinical manifestations when staining urethral smears, gonococcus is detected in 95% of cases •• In infected women, when staining smears from the cervix, gonococcus is detected in 60–70% of cases • Sowing the exudate on selective media (Thayer-Martin or Martin-Lewis) containing antibiotics that inhibit growth of other microorganisms. Culture is mandatory in women due to the low frequency of detection of gonococci when staining smears and in children with suspected sexual abuse • When the infection is generalized, blood culture is positive in 50% of cases • When culture of synovial fluid in septic arthritis, gonococcus is detected in 50% of cases • Gram staining of the material , taken from skin elements during a generalized infection, sometimes reveals gonococci • If the results of bacteriological examination are negative, in case of suspected gonorrheal infection, provocative tests are necessary (lead to a temporary weakening of the local immune defense and the active proliferation of gonococci) •• Chemical provocation method - lubrication of the mucous membrane cervical canal 2–5% solution or urethra 1–2% solution of silver nitrate •• Biological method of provocation - intramuscular injection of 500 million microbial bodies of gonovaccine or 20 mcg of pyrogenal •• Thermal method - daily diathermy or inductothermy of the genitals in for 3 days •• Physiological method - smears are taken during menstruation •• Nutritional method - eating spicy and salty foods •• Physical method - urethral massage • Immunofluorescence and coagglutination reactions with mono- and polyclonal antibodies • ELISA • PCR • Antibiotics even in small doses affect the research results.
Special studies • Antibiotic sensitivity tests. Currently, the production of b-lactamase by bacteria and chromosomally determined resistance to penicillin and/or tetracycline are becoming increasingly common • Analysis of the phenotypic characteristics of the isolated culture - the use of standard enzymatic tests and DNA tests. This stage is important during forensic medical examination in cases of rape and sexual offenses against children, because other Neisseria (normal flora of the mucous membranes) may look like gonococci • Ultrasound or CT of the pelvic region - thickening of the walls and widening of the lumen of the fallopian tubes or abscess formation • Culdocentesis - free purulent exudate in the pouch of Douglas.
Differential diagnosis • Trichomoniasis • Chlamydia • Ureaplasmosis • Bacterial vaginosis.
TREATMENT
Management tactics • Hospitalization •• If generalization of infection is suspected •• with pneumonia or eye infection in newborns •• Women with inflammatory diseases of the pelvic organs • Serological testing of all patients for the presence of syphilis and HIV infection is mandatory • Examination and treatment of sexual partners • Patients , in which the source of infection has not been identified, are subject to clinical and serological control for 3 months.
Surgery. Patients with pelvioperitonitis due to purulent salpingitis are treated conservatively. If there is no effect from the therapy within 24–48 hours, laparoscopic diagnosis is used to exclude rupture of the ovarian-tubal abscess. For diffuse peritonitis not limited to the pelvic cavity, emergency surgery is indicated.
Drug therapy
• For uncomplicated gonococcal infection of the lower genitourinary tract, pharynx and rectum •• Ceftriaxone - 250 mg IM once (or amoxicillin 3 g orally once, or benzylpenicillin IM if the pathogen is sensitive) •• Alternative drugs: azithromycin 1 g once orally, spectinomycin 2 g IM, norfloxacin 800 mg orally, ciprofloxacin 500 mg, combination of cefuroxime 1 g, cefotaxime 1 g IM •• Due to the fact that gonococcal infection is often combined with chlamydia, one of the above drugs is prescribed simultaneously with doxycycline 100 mg orally 2 times a day for 7 days (for pregnant women - with erythromycin 500 mg orally 4 times a day for 7 days).
• For complicated gonorrhea of the lower genitourinary tract, for gonorrhea of the upper genitourinary tract and pelvic organs, for gonococcal proctitis, pharyngitis and disseminated gonococcal infection •• Ceftriaxone 1 g IM or IV 1 r / day (or benzylpenicillin [sodium salt] if the pathogen is sensitive) or •• cefotaxime 1 g IV every 8 hours, or •• spectinomycin 2 g IM every 12 hours, or •• kanamycin 1 million units IM every 12 hours, or •• ciprofloxacin 500 mg IV every 12 hours, or •• ampicillin 1 g orally every 6 hours (if the pathogen is sensitive) •• Pregnant women - erythromycin, benzylpenicillin (sodium salt) or some cephalosporins •• Chemotherapy is stopped no earlier than 24–48 hours after the disappearance of clinical symptoms •• In case of joint damage, NSAIDs are additionally prescribed.
• For conjunctivitis •• Ceftriaxone 125-250 mg IM once or •• Locally every 2 hours - gentamicin (0.3%) or tetracycline (1%).
• For infection in newborns •• Ceftriaxone 25–50 mg/kg IV or IM every 12 hours for 7 days •• For eye infection - ceftriaxone 125 mg IM once •• For the prevention of gonoblennorrhea in newborns, drops into the eyes 30% sulfacetamide solution.
• For infection in children - ceftriaxone 125 mg IM (with body weight 45 kg and above).
• Local treatment •• For men - urethral lavage with potassium permanganate solution (1:10,000), nitrofural (1:5,000), instillation of 0.25–0.5% silver nitrate solution, Vashkevich tamponade, bougienage • • Women: for urethritis - instillation of 0.25–0.5% silver nitrate solution; for cervicitis - vaginal baths, lubrication of the cervical canal with 1% Lugol's solution with glycerin, 2% silver nitrate solution; for vulvitis - sitz baths with potassium permanganate solution (1:8,000), chamomile infusion.
• 7–10 days after the end of treatment, a combined provocation is carried out and after 24–48–72 hours, material is taken for bacteriological and bacterioscopic studies. Provocation and clinical examination are repeated after 1 month.
Complications • Men: urethral strictures • Women: tubal infertility, tubal pregnancy.
The prognosis with early treatment is favorable.
Synonyms • Tripper • Fracture
ICD-10 • A54 Gonococcal infection
Treatment of gonorrhea
Gonorrhea can only be treated with antibacterial drugs, which are strictly prescribed by a doctor.
Photo: kuprevich / freepik.com
Treatment with drugs
The main drugs for the treatment of gonorrhea: a combination of antibiotics of two groups - cephalosporins and macrolides.
If a patient is allergic to macrolides, he is prescribed a drug from the tetracycline group (contraindicated during pregnancy).
Pregnant women are also prescribed a course of antibiotics. It is important to treat gonorrhea before your baby is born to reduce the risk of infection during childbirth.
Improvement occurs after the first day of treatment, but therapy must be completed to the end. If the course of antibiotics is not completed, bacteria may develop resistance to the drugs used. In this case, it will be very difficult to get rid of the infection. It can become chronic and incurable.
7 days after completing the course of treatment, you must visit your doctor to take control samples.
It should be remembered that during therapy it is necessary to abstain from sexual intercourse. Sexual intercourse can trigger a new infection. In addition, you can infect your partner. You can return to sexual activity after receiving negative test test results.
Important! Both partners must undergo treatment for gonorrhea. It is possible to get gonorrhea again if you have been treated and your partner has not.
Immunotherapy
As an auxiliary treatment for gonorrhea, the doctor may prescribe anti-inflammatory drugs and agents to strengthen the immune system. Immunotherapy cannot be the basis of therapy, since it is not sufficiently effective.
Treatment of other sexually transmitted infections associated with gonorrhea
Patients with gonorrhea due to unprotected sexual intercourse and due to weakened immunity can be infected with other sexually transmitted infections (chlamydia, syphilis, HIV).
Before starting treatment, the doctor examines the patient for other sexually transmitted infections, in case complex therapy is required against several pathogenic microorganisms at once.
Alternative therapy for gonorrhea in women
No traditional medicine can cure gonorrhea.
Translate into a chronic, latent form - yes.
But never destroy pathogens.
However, treating gonorrhea at home is possible.
First, a woman needs to be examined and consult a qualified venereologist.
Especially if you are planning a pregnancy.
Medicinal herbs can be used at the final stage of drug therapy, when antibiotics have already dealt with gonococci.
This can be douching with chamomile decoction, baths with sea buckthorn locally.
Inside - decoctions with juniper, dandelion, any other anti-inflammatory or immune-stimulating preparations.
And also with the knowledge and consent of the doctor.
Possible complications of gonorrhea
Gonococcal infection, like any other untreated infection, can lead to complications.
In women, gonorrhea, if left untreated, can cause inflammation of the cervix (cervicitis) and pelvic inflammatory disease (PID). And those, in turn, can lead to infertility and ectopic pregnancy. Another consequence of untreated gonorrhea is chronic pelvic pain.
In men, gonococcal infection can manifest as inflammation of the urethra (urethritis) or inflammation of the epididymis (epididymitis). If gonorrhea is left untreated, the infection will affect the prostate and seminal vesicles, which can lead to infertility and impotence.
Rare effects include inflammation of the endocardium (the inner wall of the heart) and inflammation of the brain or spinal cord (meningitis), as well as gonorrheal arthritis, in which the infection spreads to the skin and joints. And neglected blenorrhea can lead to blindness.
Gonorrhea weakens the immune system and can facilitate the transmission of other infections, including HIV.
Pathophysiology
The mechanism of disease development and the virulence of gonococcal strains depend on the specific antigenic properties of the bacteria. Some subtypes of Neisseria gonorrhoeae can successfully evade the immune response and rapidly cause systemic infection. It is noted that gonococci primarily affect the columnar and glandular epithelium of the genitourinary system. Moreover, some types of epithelial tissues are resistant to pathogenic microorganisms. Doctors note that gonococci rarely cause vaginitis if the vaginal mucosa is not susceptible to other pathological processes.
The main protective properties of bacteria are associated with genetic material. Typically, gonococcal plasmids contain genes responsible for resistance to antibiotics. Different strains of bacteria can freely exchange these genetic structures, resulting in a high risk of reinfection. In addition, the exchange of antibiotic resistance genes has meant that gonorrhea is rarely susceptible to beta-lactam antibiotics. In recent years, there has also been an increase in the incidence of gonorrhea resistant to fluoroquinolones.
The probability of developing disseminated gonococcal infection is approximately 1%. Patients experience symptoms of arthralgia, fever, migratory polyarthritis, tendonitis, endocarditis, or meningitis. These complications are associated with bacteria entering the bloodstream. The risk of such a negative consequence of gonorrhea depends on the characteristics of the patient’s immunity and the virulence of the particular strain of the bacterium. For example, changes in the acid-base properties of vaginal discharge during menstruation increase the likelihood of gonococcus entering the blood.
Prevention
Only sexual abstinence provides 100% protection against sexually transmitted diseases.
To reduce the risk of contracting gonorrhea, you need to:
- use condoms. For oral sex - condoms or latex wipes;
- be in a monogamous relationship;
- be screened for gonorrhea and other sexually transmitted diseases with your new partner before the first sexual intercourse;
- abstain from promiscuity;
- do not share the same sex toys with other people;
- undergo an annual examination by a gynecologist;
- undergo screening - urine test for nucleic acids. Its regular use is recommended for women under 25 years of age who are sexually active, men who have sex with other men, and people who are promiscuous.
Allergic reaction
If, in addition to itching and burning of the vulva, there are no other alarming symptoms, it may be an allergic reaction to washing powder, washing liquid, sanitary napkins or cosmetics.
To get rid of the problem:
- Use only intimate hygiene products with a neutral pH (about 5.2).
- Choose liquids that contain lactobacilli, as they protect intimate areas from attack by pathogenic bacteria.
- Avoid scented panty liners. Use them only when necessary - do not use them “prophylactically” for a month, because without them the skin breathes better.
- If your allergic reaction is caused by laundry detergent or softener, start using products designed for babies or allergy sufferers.
How is gonorrhea treated today according to international standards?
With the advent of the antibiotic penicillin, a real revolution came in the treatment of gonorrhea, and this disease ceased to be such a serious problem as it was in the pre-antibiotic era. Treatment for gonorrhea has become much more reliable, and the complications of this disease have become significantly less. However, it didn’t take long to celebrate the victory. Already in the late 60s and early 70s of the 20th century, more and more cases of gonococci resistance to penicillin began to be recorded. By the end of the 70s, by the beginning of the 80s of the last century, most strains of gonococci became completely insensitive to penicillin, as well as to tetracycline, and antibiotics of these groups, including semisynthetic penicillins, were removed from some national and international standards for the treatment of gonorrhea.
Today it has been established that, on average, 3 years after the appearance of a new antibiotic, antibiotic resistance begins to develop. Thus, more and more cases of resistance are being demonstrated to the most effective antigonorrhea antibiotic of the 80s, spectinomycin. There is an increasing number of cases of gonococcal resistance to ciprofloxacin, which is still included in the standard treatment of gonorrhea. Ciprofloxacin is not recommended for use if gonorrhea infection occurred in the Asia-Pacific region and Hawaii. According to L.S. Strachunsky et al. (2004) about 35% of gonococcal strains isolated in Moscow and Smolensk were not sensitive to ciprofloxacin. However, currently, according to the recommendations of the World Health Organization (WHO) and the US Center for Disease Control (CDC), the antibiotics of choice for the treatment of gonorrhea are: ceftriaxone, cefixime, ciprofloxacin, ofloxacin, levofloxacin, spectinomycin and azithromycin. Because about 30% of cases of gonorrhea are combined with chlamydia, the CDC recommends that after taking a single dose of an antigonorrhea drug, chlamydia should be treated with the antibiotics doxycycline or azithromycin.
If gonorrhea is detected in one of the partners, the other one must also be treated, even if gonorrhea has not been diagnosed. Treatment of chronic and complicated gonorrhea is carried out with higher doses of the same antibiotics, and the duration of treatment is 24 - 48 hours after the disappearance of symptoms of the disease (on average from 7 days to 1 month). Those suffering from gonorrhea should always remember to take into account all the features of the disease and determine The most effective drug, its dose and duration of treatment (taking into account known data on the antibiotic sensitivity of gonococci) can only be determined by a qualified doctor.