Professions - risk groups
This disease mainly affects medical workers, mechanics, builders, hairdressers, cosmetologists, makeup artists, cleaners, gardeners, agricultural workers, as well as people who work with food (waiters, cooks, etc.).
- The most common irritating agents are solvents, bleaches, medical alcohol, soaps, deodorants, cosmetics, sawdust, oils, and detergents.
- If you have to wash your hands regularly or the work itself involves the fact that they are often in a humid environment, then this is also a risk factor for the development of contact dermatitis.
- Allergic contact dermatitis can be caused by metals, formaldehyde (found in glue, solvents), plants, cosmetics, etc.
Reasons why contact dermatitis occurs
Contact dermatitis always develops “in the presence” of some chemical, biological or physical environmental irritant. All unfavorable factors that cause a skin reaction in the form of inflammation are conventionally divided into two large groups - obligate and facultative.
To obligate
include factors that irritate the skin of absolutely any person:
- alkaline and acidic compounds;
- poisonous plants, animals, insects;
- ionizing radiation;
- temperatures too low or too high.
Optional
These are the factors that provoke inflammation of the skin only when there is increased sensitivity in a particular person:
- turpentine;
- metal salts;
- some local drugs;
- cleaning and detergents;
- cosmetics;
- synthetic underwear;
- wool clothing;
- formalin;
- machine oil and others.
In addition to the obligatory contact skin irritant, relapses can be caused by the following factors:
- decreased immunity;
- increased sweating;
- intestinal dysbiosis;
- hormonal disorders;
- frequent trauma to the skin;
- chronic skin diseases.
For example, a woman experiences dry and tight skin after using a detergent. But she doesn’t pay attention to this and continues to wash the dishes without household gloves. And one day, dryness and tightness quickly turn into inflammation with itching.
Most likely, in such cases, in addition to an external contact irritant, something else turns on - spring has come, immunity has decreased due to vitamin deficiency, or the day before you cut your finger.
The following point of view is also widespread among specialists: the cause of contact dermatitis should be sought in a violation of autoimmune processes. Due to an autoimmune failure, the body begins to produce antibodies to its own cells. And then any aggressive substance provokes an inflammatory reaction.
Manifestations and types of contact dermatitis
For irritant contact dermatitis to occur, a single exposure to the agent may be sufficient. Then the disease is called acute , redness of the skin occurs, often swelling, blisters, and the affected area becomes moist. All this is accompanied by burning, pain and often itching.
Chronic is more common - when there is prolonged contact with a substance that has a mild irritant effect. Then the skin becomes dry, red, flaky, thicker and cracks.
With irritant contact dermatitis, problems most often occur on the back of the hand and the skin between the fingers. But sometimes even areas covered by clothing, such as the genitals, are affected.
With allergic contact dermatitis, the boundaries of redness can be blurred, several areas are affected at once: eyelids, lips, etc. Pain and burning occur infrequently, but there is almost always itching. Visually, allergic and irritant contact dermatitis are quite similar.
If you suspect contact dermatitis, your doctor will first ask you about the specifics of your work (especially if you are undergoing a medical examination), as well as when your symptoms began and what you attribute to their worsening. Therefore, it is better to prepare and try to answer these questions for yourself before visiting the doctor. The doctor will also be interested in whether you have already had dermatitis and allergic diseases.
Allergic contact dermatitis: basic approaches to diagnosis, treatment and prevention
Allergic contact dermatitis is a classic form of delayed-type hypersensitivity reaction mediated by sensitized lymphocytes. According to a number of authors, this pathology affects 1% to 2% of the population in various regions. The prevalence of the disease is higher in industrialized countries. It is increasing as more and more new chemical substances are introduced into use in medicines, cosmetic products, medical implants, household chemicals, and industrial reagents.
Unlike simple contact dermatitis, in which an irritant causes inflammation in all people when exposed to the skin, allergic dermatitis occurs only in sensitized individuals, that is, in people who have immune cells specific to this substance - T-lymphocytes. Contact dermatitis is often caused by harmless chemicals that, under normal conditions, do not cause any clinical symptoms in healthy people. But allergic dermatitis is also known when in contact with aggressive agents - components of hair dyes, hair growth products, dyes for fabrics, fur and leather, detergents, medications, juice of poisonous plants.
A classic example of allergic contact dermatitis is dermatitis caused by plants of the genus sumac (in particular, poisonous sumac - Rhus toxicodendron), in which the rashes often have a linear shape and are located on exposed areas of the body.
The pathogenesis of allergic contact dermatitis is based on a tuberculin-like delayed (cellular) hypersensitivity reaction, the inductive phase of which begins with local exposure to the skin of low molecular weight chemicals of organic or inorganic nature. Their sensitizing (allergenic) properties depend on their ability to penetrate the skin and form stable covalent bonds with the proteins of the host organism. Thus, dinitrochlorobenzene forms complexes in the epidermis with proteins containing a lot of lysine and cysteine. Skin lipids can also serve as an adjuvant.
In the formation of hypersensitivity, the leading role is played by professional macrophages of the epidermis - multi-processed Langerhans cells. The resulting delayed hypersensitivity is directed not only to the chemical itself, but also to the carrier protein.
Typically, at least 10–14 days pass from the moment of skin contact with the allergen until the development of the first clinical manifestations. The duration of the sensitization period is usually shorter for aggressive chemicals. Thus, according to our observations, drug allergens when applied to the skin can cause manifestations of contact dermatitis as early as 7–8 days. The most common allergenic medications are local forms of antibacterial drugs; contact allergic reactions to local anesthetics, antiseptics and latex are less common.
The location and configuration of the lesion is determined by the causative factor. The most common form of the disease is eczematous dermatitis. The disease is easy to diagnose and, as a rule, is characterized by a favorable course. The rash disappears when exposure to the pathogenic factor ceases. To accelerate the regression of clinical manifestations, local anti-inflammatory drugs, mainly topical glucocorticosteroids, can be used.
Etiology
According to our observations, the most common cause of allergic contact dermatitis is stainless metal alloys from which household products are made - kitchen utensils, jewelry, watches, denim rivets, zippers, keys, as well as medical supplies - dental crowns, braces , devices for focal and extrafocal osteosynthesis. Thus, having analyzed 208 cases of allergic contact dermatitis that we encountered in practice in the period from 1999 to 2009, we came to the conclusion that the metals nickel, cobalt and chromium, which are part of stainless alloys, were the cause of inflammation in 184 (88.5% ) patients.
A list of the most common, according to our data, causes of allergic contact dermatitis is given in
.
Pathogenesis
Allergic contact dermatitis is a delayed-type allergic reaction. An allergen that gets on the skin binds to tissue proteins, forming a compound that can cause an allergy - an antigen. Langerhans cells absorb antigen in the membrane molecules of the major histocompatibility complex class 2 by T lymphocytes. Activated T lymphocytes and Langerhans cells produce gamma interferon, interleukins 1 and 2, which enhance the immune response and inflammatory response. Activated T lymphocytes migrate through the lymphatic vessels to the paracortical zone of the regional lymph nodes. In the lymph nodes they undergo antigen-dependent proliferation and differentiation. Some of the “specialized” T-lymphocytes take part in the immune response, while the rest turn into memory cells. They cause the appearance of a rapid, pronounced response after repeated contact with the allergen. After the first contact with the allergen, T-lymphocytes recognizing it accumulate, which usually lasts 10–14 days. After this, T-lymphocytes leave the regional lymph nodes into the blood and populate all peripheral organs of the immune system. Upon repeated contact with the allergen, memory cells are activated and rapid accumulation of delayed-type allergic reaction effector cells—macrophages and lymphocytes—occurs.
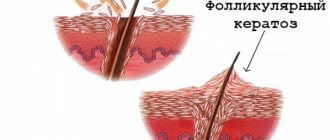
Histological picture
The histological picture of allergic contact dermatitis is characterized by infiltration of the dermis with mononuclear cells, primarily near blood vessels and sweat glands. The epidermis is hyperplastic and also infiltrated with mononuclear cells. Typically, the formation of vesicles in the epidermis combines with the formation of bullae. The serous fluid filling them contains granulocytes and mononuclear cells.
Clinical manifestations
The disease, according to our data, is more common in young and middle-aged people. However, exceptions are possible. Thus, of the people we examined, the youngest was a one-and-a-half-year-old girl with an allergy to cobalt, and the oldest patient was an eighty-year-old man, sensitized to chromium and nickel.
In the clinic, allergic contact dermatitis is distinguished into acute, subacute and chronic forms, as well as mild, moderate and severe.
The interval from the initial exposure to the allergen to the formation of skin hypersensitivity can vary: from relatively short (2–3 days when exposed to a strong sensitizer, for example, urushiol from the juice of plants of the genus sumac) to very long (several months or years in the case of a weak sensitizer, for example, chromic acid salts or chloromethylisothiazolinone). As a rule, in an already sensitized organism, the disease develops acutely 12–72 hours after exposure to the allergen and is manifested by itching, bright hyperemia and swelling of the skin at the site of contact, against which papules, small blisters or blisters are visible, opening and leaving weeping erosions (wetting) . Sometimes skin necrosis occurs.
The subsiding inflammation leaves crusts and scales. In a chronic course, peeling and lichenification appear.
Acute allergic contact dermatitis is characterized by the following stages of development of rashes: erythema => papules => vesicles => erosions => crusts => peeling. For a chronic course: papules => desquamation => lichenification => excoriation.
In severe allergic contact dermatitis (for example, caused by sumac poison), the patient may experience symptoms of intoxication - headache, chills, weakness and fever.
The localization of dermatitis can be any and depends on the place of contact with the allergen. Thus, occupational allergens more often form foci of inflammation on the palmar and lateral surfaces of the hands and fingers, forearms, and metal allergens sensitize the skin and mucous membranes at points of contact with rings, bracelets, zippers, and denim rivets (“jean rivet disease”). , metal dental crowns.
Different areas of the skin are characterized by varying susceptibility to allergic dermatitis. Inflamed and infected tissues become sensitized more often. Friction, squeezing, maceration and increased sweating contribute to the formation of allergies. In this regard, the skin of the eyelids, neck, perineum, and anterior abdominal wall in the area of contact with fasteners and buckles is often sensitized. Often patients do not realize that they suffer from allergies, believing that they simply “rubbed” the skin in the area of inflammation.
Allergic contact dermatitis always begins at the site of exposure to the allergen. Therefore, at the beginning of the disease, the lesion is clearly demarcated, although it often extends beyond the area of skin in contact with the allergen. In sensitized patients, the lesion may spread to other areas of the body or become generalized.
With a single contact, the disease lasts several days or weeks. With frequent and regular contacts - months and years.
Diagnostics
Based on the location of skin lesions, as a rule, possible causative allergens can be assumed. In the future, their role in the pathological process is determined when performing skin patch tests. To conduct a patch test, the test material is applied to the skin for 48–72 hours, and then the size of the reaction caused by the allergen is assessed.
Since allergies are always a systemic process, the skin and mucous membranes of the entire body are sensitized. Consequently, inflammation develops when an allergen is applied to any area of the skin. However, it is technically more convenient to carry out patch skin tests in the interscapular region, the outer surface of the shoulder and the inner surface of the forearm, when fixing the material on which the patient feels most comfortable during the study.
The test materials are applied to dry skin treated with alcohol, covered with pieces of gauze and then attached with adhesive tape (that’s why the test is called “plaster”). It is convenient to use a standard test system with standardized allergens already applied to the adhesive base. Thus, the Allertest system for diagnosing allergic contact dermatitis to 24 reagents has been registered in Russia. It is sold in a pharmacy and allows you to diagnose contact allergies to nickel sulfate, lanolin, neomycin sulfate, potassium dichromate, a mixture of local anesthetics - caine derivatives, a mixture of flavoring substances, rosin, epoxy resin, a mixture of quinolines, Peruvian balsam, ethylenediamine dihydrochloride, cobalt chloride, p-tert-butylphenol formaldehyde, parabens, carbamate mixtures, black rubber mixtures, chloromethylisothiazolinone, quaternium 15, mercaptobenzothiazole, paraphenylenediamine, formaldehyde, mixtures of mercaptans, thiomersal and mixtures of thiuram derivatives. This is a simple and ready-to-use patch skin testing system. Allergens are included in a hydrophilic gel, from which the allergen is then released when soaked. "Allertest" contains two plates that are adhesive to the skin, each of which contains 12 allergens. All 24 antigens can be tested simultaneously, or the desired allergen can be cut from the plate with scissors and applied independently.
After 48–72 hours from the start of placement, the flaps are removed, wait 20–30 minutes for the nonspecific mechanical irritation to subside and take into account the severity of the reaction. Changes at the site of skin contact with the allergen are taken into account quantitatively. The gradation of a positive result is carried out as follows: (+) - erythema; (++) - erythema and papules; (+++) - erythema, papules, blisters; (++++) - erythema, papules, blisters and severe swelling.
A true allergic reaction lasts 3-7 days, while a reaction caused by skin irritation disappears within a few hours. Therefore, in doubtful cases, the severity of the reaction should be re-evaluated the next day.
H1 blockers do not affect the results of application tests. Topical use of corticosteroids on the skin area selected for testing should be discontinued at least one week before the test. Taking systemic corticosteroids in a daily dose exceeding 15 mg of prednisolone can suppress even sharply positive reactions, therefore skin patch tests are carried out no earlier than 7 days after the cessation of immunosuppressive therapy. In rare cases, skin tests are performed in patients chronically taking corticosteroids if the dose of prednisolone does not exceed 15 mg/day. However, it should be borne in mind that in this case there is a risk of obtaining false negative test results.
When performing a patch test, it should be remembered that the procedure itself may cause sensitization in the patient. Among the substances that have the ability to cause sensitization even at the first contact, it is worth noting plant resins, paraphenylenediamine, and methyl salicylate. Therefore, the application test must be justified. In addition, when conducting the test, it is necessary to exclude the possibility of nonspecific inflammation - primary irritation of the skin by the tested substances. To do this, the test materials, if they are not included in the standard test system, must be used in concentrations that do not cause irritation in the majority of healthy people (in the control group). The test should not be performed in cases of acute or extensive contact dermatitis, as increased skin reactivity may lead to a false positive result. In addition, testing with the causative allergen can cause a sharp exacerbation of the skin process. Therefore, before conducting the study, the patient must be instructed in detail, drawing his attention to the fact that if severe irritation occurs, he must remove the bandage with the allergen and contact the doctor.
When receiving a positive result from a skin patch test, it must be remembered that it only indicates sensitization to the test substance, but is not absolute proof that this particular allergen caused the dermatitis, because the possibility of long-term and polyvalent sensitization always remains. In other words, another antigen that you have not tested may also be the cause of your allergy. Therefore, when making a diagnosis, it is also necessary to take into account the history and physical examination.
Differential diagnosis
Allergic contact dermatitis must be differentiated from simple contact dermatitis, seborrheic and atopic dermatitis.
Simple contact dermatitis can develop due to damage to the epidermis by irritating chemicals (croton oil, kerosene, phenol, organic solvents, detergents, caustic soda, lime, acids, etc.) or physical impact (overheating, squeezing, compression). There is no primary sensitizing effect. Symptoms of inflammation occur immediately after exposure to the irritant, rather than 12 to 48 hours later, as with allergic contact dermatitis. The presence of papules in acute contact dermatitis indicates its allergic nature. Occupational simple contact dermatitis is similar in appearance to allergic dermatitis. The patch test allows you to differentiate these conditions.
The distinctive signs of seborrheic dermatitis include oily skin, as well as other signs of seborrhea and typical localization - the scalp and nasolabial folds. The affected areas are covered with greasy crusts and peel off profusely; Itching is usually not typical.
Atopic dermatitis usually begins in early childhood. The skin is dry. Itching is characteristic that appears before the rash, and not after it, as with allergic contact dermatitis. The flexor surfaces are most often symmetrically affected. The edges of the affected areas are indistinct; There is no consistent development of the elements of the rash: erythema => papule => vesicle.
In our practice, we encountered combined skin lesions when allergic contact dermatitis developed in response to ointments and other topical dosage forms for the treatment of dermatoses. Thus, in a 45-year-old woman suffering from microbial eczema, aggravated by the use of Zinerit (erythromycin, zinc acetate), we identified sensitization to erythromycin, an antibiotic from the macrolide group. 3 days after stopping this medication, the symptoms of exacerbation disappeared.
Three of the patients we examined, who received topical Celestoderm-B with garamycin for a long time, complained of the lack of therapeutic effect from the use of this medication. That is, despite the use of an anti-inflammatory drug, the itching and intensity of the rash not only did not decrease, but sometimes intensified some time after applying the medicine. During an allergological examination using the patch testing method, sensitization was established - a drug allergy to the antibiotic gentamicin (Garamycin), which is part of the drug. Replacing the drug with the topical glucocorticosteroid Elocom after a few days led to complete regression of dermatitis symptoms in all three patients.
When carrying out differential diagnosis, it is also necessary to remember about photocontact, phototoxic and true photoallergic dermatitis.
Photocontact dermatitis is caused by the interaction of a chemical and ultraviolet light in the skin. With it, rashes appear only on open, insolated areas of the body. The sensitizing agent is most often drugs (tetracyclines, sulfo compounds, griseofulfin, hormonal contraceptives) or locally applied resinous extracts. In phototoxic dermatitis, skin damage is caused by the action of substances (for example, hogweed juice) that acquire toxic local irritating properties under the influence of ultraviolet rays. In true photoallergic dermatitis, the sensitizing allergen undergoes chemical changes under the influence of ultraviolet rays. In the absence of insolation, it is harmless to the patient's body.
One of the rare variants of contact allergies is contact urticaria. Depending on the pathogenesis, allergic, non-immune and combined forms of this disease are distinguished. The non-immune form develops due to direct exposure of the skin or mucous membranes to an agent, most often nettle, leading to the release of mediators from mast cells. Allergic contact urticaria is caused by the production of specific IgE antibodies and, according to the mechanism of development, is classified as type 1 hypersensitivity. Most often it is caused by food products (fish, milk, peanuts, etc.), pet allergens (saliva, fur, epithelium) and penicillin antibiotics. Little is known about the combined form of contact urticaria, caused by the influence of both immune and nonspecific factors. It is believed that ammonium persulfate, an oxidizing substance found in hair bleach, often causes this type of reaction.
Treatment
The treatment of allergic contact dermatitis is based on eliminating contact of the body with the allergen that caused the disease. In the acute stage, with swelling and oozing, wet-dry dressings are indicated, followed by topical application of glucocorticoids. If the rashes are represented by large blisters, then they are punctured, allowing the liquid to drain; the bladder cover is not removed; every 2–3 hours, change bandages moistened with Burov's liquid. In severe cases, systemic corticosteroids are prescribed.
Prevention and treatment of staphylococcal and streptococcal skin infections play an important role.
Allergic contact dermatitis generally has a favorable prognosis. With timely identification of the causative allergen and elimination of contact with it, the symptoms of the disease completely regress within 1–3 weeks, and sufficient patient awareness of the nature and causative factors of the disease significantly reduces the possibility of chronicity and recurrence of dermatitis.
Prevention
To prevent the formation of allergic contact dermatitis, the local use of medications with a high sensitizing ability, primarily beta-lactam antibiotics, furatsilin, antihistamines, sulfonamides and local anesthetics, should be avoided.
In case of frequent and professional contact with low-molecular compounds, it is necessary to use personal protective equipment for the skin, mucous membranes and respiratory tract - special protective clothing, gloves, and protective creams.
Once the cause of allergic contact dermatitis has been identified, the patient must be carefully instructed and all possible sources of the allergen discussed with him, drawing his attention to the need to stop contact with this reagent and cross-reacting substances (the most common allergens, their sources and cross-reactive substances are listed in
). For example, patients with nickel allergies are not recommended to wear stainless steel jewelry or use nickel-plated cookware. For such patients, implants containing nickel are contraindicated, including dental crowns and white metal braces, and steel structures for osteosynthesis. It is also recommended that steel rivets and fasteners on jeans or other underwear be sealed on the inside with adhesive tape or cloth to prevent their contact with the skin.
If dermatitis is caused by rubber gloves, they can be replaced with vinyl ones. It is also necessary to remember that rubber drains and other medical supplies should not be used in such patients. The use of latex condoms is contraindicated for them.
If you are allergic to formaldehyde, the patient should not use certain medications and cosmetics containing this preservative. The patient should be explained that before using medications and cosmetics, it is necessary to familiarize themselves with their composition indicated on the packaging.
In the case of occupational dermatitis, it is necessary to recommend acceptable types of work to the person.
Literature
- Harrison T.R. Internal diseases. Ed. E. Fauci, J. Braunwald and others. In two volumes. Per. from English M., Practice - McGraw-Hill (joint ed.), 2002.
- Patterson R., Grammer L.K., Greenberger P.A. Allergic diseases: diagnosis and treatment. Per. from English edited by A. G. Chuchalina. M., GEOTAR MEDICINE, 2000.
- Popov N. N., Lavrov V. F., Soloshenko E. N. Clinical immunology and allergology. M., REINFOR, 2004.
- Luss L.V., Erokhina S.M., Uspenskaya K.S. New possibilities for diagnosing allergic contact dermatitis // Russian Journal of Allergology. 2008. No. 2.
- Fitzpatrick T., Johnson R., Wolfe K. et al. Dermatology. Atlas-directory. Per. from English edited by E. R. Timofeeva. M., Praktika, 1999.
E. V. Stepanova , Candidate of Medical Sciences, Research Institute of Vaccines and Serums named after. I. I. Mechnikova RAMS, Moscow
Key words: allergic contact dermatitis, patch skin tests, preventive dermatitis, allergic dermatitis, drug allergens, occupational allergens, contact allergens, metal allergy, contact dermatitis, metal dermatitis, contact urticaria.
How is the diagnosis made?
To rule out or confirm allergic contact dermatitis, your doctor will perform a skin test. It consists of applying samples of common common allergens and those found in your workplace to the skin. If redness and inflammation occur, then there is an allergy to the applied substance.
In rare cases, a biopsy (analysis of a tissue sample) of the skin is required to rule out other diseases (psoriasis or other inflammatory dermatoses).
If the diagnosis of irritant contact dermatitis is confirmed, then treatment will have three directions:
- Avoid exposure to irritant.
- Restore damaged skin.
- Relieve inflammation.
If contact with an irritating substance cannot be excluded, then you can wear a respirator, goggles, overalls or, for example, latex gloves with an inner cotton layer. This is necessary so that sweat is absorbed by the fabric and does not harm the skin.
Three reasons to treat contact dermatitis at El.En.
Rapid improvement.
If you follow medical recommendations, improvement occurs in a matter of days. The doctor tries to choose a treatment tactic that will give the fastest maximum effect.
Individual approach.
All symptoms and complaints of the patient must be taken into account - sometimes the causes of diseases are found where no one had thought to look for them before...
Stable result.
All our patients note long remissions and rare deterioration (in case of accidental contact with an irritant). Of course, you will have to strictly follow the proposed rules and change your habits a little.
What can you do yourself?
To restore damaged hand skin, you need to follow a number of simple rules:
- wear gloves in cold weather;
- Use warm water and a little mild detergent to wash your hands;
- rinse off the soap well and dry your hands;
- often (at least every time after washing your hands) use moisturizing and skin softening products, as well as those that prevent skin dehydration. These are usually creams with petroleum jelly, lanolin, glycerin, ceramides, dimethicone, propylene glycol, urea, etc.
It is recommended to relieve inflammation with the help of corticosteroids (in the form of cream, lotion, foam or, better yet, ointment). If the dermatitis is severe or chronic, with noticeable thickening of the skin and is not on the face or in the area of skin folds, then clobetasol, diflucortolone, etc. are used for 2-4 weeks. In less severe cases, betamethasone, diflucortolone, mometasone, triamcinolone, etc. are used (also for 2–4 weeks). When dermatitis is on the face or in the area of skin folds, weaker corticosteroids or corticosteroids in lower dosages are used: triamcinolone, betamethasone, hydrocortisone, etc. for 1–2 weeks.
It is highly advisable not to scratch the sore spot, otherwise additional damage to the skin may create a suitable environment for bacterial infection.
After a case of acute dermatitis, recovery takes about a month if there is no further exposure to the irritating agent. With chronic contact dermatitis, symptoms may not go away for months or years.
For allergic contact dermatitis, the most important thing is to avoid the substance that caused the disease and relieve inflammation. The methods are approximately the same: wear gloves, overalls, a mask and goggles, use corticosteroids for 1-2 weeks (in severe cases it is better to take systemic drugs, that is, in tablets) or calcineurin inhibitors (for example, pimecrolimus cream).
Treatment of dermatitis
Treatment tactics for dermatitis depend on the cause and form of the disease. General recommendations for the patient include:
- establishing a work and rest schedule, sleeping at least 8 hours a day;
- a diet based on limiting fried, spicy and canned foods, possible food allergens;
- carrying out hygiene procedures in warm water (not higher than 34°C);
- eliminating stress and nervous overload.
In case of severe itching, accompanied by sleep disturbances and neurological disorders, the prescription of sedatives, mainly of herbal origin, is indicated.
It is important to stop contact of irritants with the skin or internal environment of the body as soon as possible. To achieve this, cleansing and general detoxification measures are carried out:
- in case of chemical exposure to the skin, it is thoroughly washed and a bandage is applied with a neutralizing substance - alkali for an acid burn or an acid for an alkali burn;
- for perioral, drug-induced and allergic dermatitis, after washing the skin, enterosorbents, a hypoallergenic diet, and in severe cases, intravenous infusions of special solutions are prescribed;
- Treatment of parasitic infestation is carried out using anthelmintic drugs.
Also in the treatment of dermatitis, antihistamines, antibiotics and antifungals are used both locally, on the skin, and systemically.
Wet areas of the skin can be treated with antiseptic solutions and herbal infusions that have a drying effect. Hormonal ointments for dermatitis have an anti-inflammatory effect. Severe itching and pain, as well as a large area of damage and the appearance of areas of tissue necrosis, are indications for urgent hospitalization of the patient. In case of severe disease with damage to more than 20% of the skin, a course of prednisolone tablets is recommended. In such situations, treatment may be supplemented with immunosuppressive drugs.
Author:
Pugonina Tatyana Alekseevna, Therapist
Dangerous symptoms of dermatitis
If you have signs of contact dermatitis, consult your doctor. The doctor will make a diagnosis and prescribe treatment that will alleviate your condition. You should not hesitate if, along with redness on the skin, signs of infection appear (pus, fever), or if you feel that the mucous membranes of the respiratory tract (it hurts to breathe) or the gastrointestinal tract (it hurts to chew and swallow) are damaged.
To diagnose and treat contact dermatitis, make an appointment with a dermatologist - call +7 (495) 120-08-07.
Diagnostics
To establish a diagnosis, special application tests (patch tests) are used, which involve applying the allergen to a particular area of the skin. At the same time, during the diagnostic examination, a clinical and biochemical analysis of blood and urine is prescribed. If there are indications, a blood test is performed for hormones, a coprogram, tests for dysbacteriosis are taken, and an ultrasound examination of the abdominal organs is performed (in order not to miss concomitant pathologies).
During the study, it is mandatory to carry out a differential diagnosis of contact dermatitis with various forms of eczema and atopic dermatitis.
Sign up for a study at the NEARMEDIC clinic
NEARMEDIC became the first private clinic in the capital to receive the Quality Mark and the Moscow Quality award. In the NEARMEDIC network of clinics, treatment is carried out by experienced immunologists-allergists and dermatologists with specialized qualifications and many years of practice. In clinics you can undergo laboratory diagnostics.
Specialists will conduct a full examination of children and adults, including not only skin tests, but also taking an anamnesis and a full comprehensive examination of the body. This makes it possible to exclude the total effect of different substances or the absence of an allergen in standard test systems. The allergist will select desensitizing therapy and develop a plan of preventive measures. Within 1-3 weeks, the unpleasant symptoms will subside and the treatment will be completed.
To make an appointment yourself or to register your children for an appointment, use the form on the website or call us. We will help you choose a convenient time and answer all your questions.
Treatment of simple contact and allergic dermatitis
Treatment can only be prescribed by a specialist dermatologist after a preliminary consultation and examination of the patient. Depending on the type of skin pathology, the patient may be referred to an allergist, who will study the medical history and assess the nature and extent of the lesion. This is necessary in order to determine the allergen that provoked the disease, since treatment is primarily aimed at partial or even complete elimination of the provoking substance.
Therapy used for dermatoses is divided into supportive and medicinal. The first includes cold compresses, bandages, and antihistamines. Drug treatment is carried out mainly with external topical glucocorticosteroids in the form of ointments and creams.[4] Such drugs have a versatile effect on the source of inflammation, therefore they are the most popular drugs with wide application possibilities.[5] Akriderm preparations are also local glucocorticosteroids.
Prevention
To prevent contact dermatitis, you need to pay attention to medications that are highly allergenic, including furatsilin, antihistamines, and topical anesthetics. Persons frequently in contact with low molecular weight substances are advised to use gloves, protective clothing and moisturizers.
After identifying the allergen, it is necessary to prepare a comprehensive list of drugs, objects, and substances that should not come into contact. If you are allergic to fasteners and rivets of clothing, it is recommended to seal them on the reverse side with a plaster or cover them with fabric. If you are allergic to latex, you should avoid wearing gloves and latex condoms. If you are allergic to formaldehyde or other components of cosmetics, you must carefully study the packaging of purchased cosmetics.
How does the reaction occur?
How quickly an allergen can trigger an immune response depends on its ability to bind to the protein compounds contained in the skin.
For example, dinitrochlorobenzene (a very strong allergen) binds to proteins containing the amino acids lysine and cysteine and forms an antigen. Macrophages (Langerhans cells), which respond to the penetration of foreign components into the body, begin to form an immune response, which leads to an inflammatory reaction. Some T-lymphocytes turn into memory cells during their work, which is why upon subsequent contact with the allergen, the reaction occurs again. Among medical drugs and products, allergic manifestations are most often caused by antiseptics, local anesthetics, and latex products.
Symptoms
Allergic dermatitis most often occurs in older children and middle-aged adults. All appearances are divided into two groups of three subgroups:
- acute, subacute and chronic;
- mild, moderate and severe.
The primary reaction can appear 10-14 days, and sometimes several years after regular exposure to the allergen, if it is weak. A repeated reaction may occur within 12-72 hours.
Main symptoms:
- itchy sensations;
- swelling and redness at the site of contact;
- the appearance of vesicles and bubbles against the background of hyperemia;
- vesicle formation;
- in place of the opened bubbles, weeping erosions appear;
- erosions heal, crusts and scales appear.
The step-by-step process described above is characteristic of the acute form of the disease; in the chronic form, the process proceeds a little differently - it begins with papules, then peeling appears, and lastly excoriation (scratching). If the substance stimulating the reaction was a very serious allergen (for example, poison), general symptoms of intoxication may appear: headache, fever and weakness.
Symptoms appear in the place where there was contact with the allergen. For this reason, this dermatitis does not show symmetrical manifestations on the arms and legs, and its causative agent is easy to identify. Occupational allergies manifest themselves on the hands - palms, sides of the hands, skin between the fingers, forearms. If the problem is caused by jewelry or fasteners, then the manifestation will be noticed at the point of contact with them.
Contact dermatitis, when it first appears, is clearly visible at the site of contact with the skin, so its cause is easy to determine. With subsequent exacerbations, redness with papules may appear in any other place on the body, which causes much more inconvenience to patients. If with a single contact the disease can be eliminated after 1-3 weeks, it may take months to enter the chronic stage.