Author:
- Nikonov Mikhail Yurievich
5.00 (Votes: 1)
Many of us begin to think about the state of our health only when we hear an alarm bell from it, or even several. This also applies to the liver, the hottest organ of our body, which bears special responsibility for numerous and very important processes occurring in it.
For example, our liver courageously takes on the first “blow” of toxic substances, allergens and other substances that are unsafe for us (including metabolic products), practically transforming them into safer ones and ready for elimination from the body. It also comes with an excess of hormones, vitamins and other elements that are beneficial to us in normal doses.
On the other hand, the liver accumulates reserves of useful substances (for example, glycogen, vitamins and microelements) to regulate carbohydrate metabolism and a large amount of blood (in case of emergency compensation for blood loss). The liver also synthesizes hormones and enzymes, blood plasma proteins, cholesterol and lipids, bile (including the specific pigment bilirubin), without which our body simply could not exist.
During our lives, the liver copes with such a huge amount of work that if the load on it is too great, sooner or later it itself may need our help. Therefore, assessing the condition of our liver and nearby organs in time by undergoing a comprehensive ultrasound of the abdominal organs and kidneys with the adrenal glands means noticing alarming changes and starting the necessary treatment as early as possible!
What is jaundice
First of all, by jaundice we should not mean a specific disease (for example, hepatitis, as many people think), but a whole symptomatic complex that arises as a result of pathological processes in the liver and some organs. Essentially, jaundice is an excess amount of bilirubin in the body, which is externally manifested by the sclera, mucous membranes and skin becoming yellow.
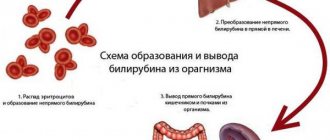
Normally, bilirubin is formed in the liver and spleen from hemoglobin as a result of the breakdown of red blood cells, after which it is converted by the liver into bile and excreted from the body. With jaundice, the normal process of conversion and excretion of bilirubin is disrupted, so it remains almost completely in the blood, slightly excreted through the kidneys and skin.
People with:
- neoplasms in the liver;
- congenital anomalies of the bile ducts;
- pathological processes in the liver and gall bladder;
- the presence of parasitic organisms;
- postoperative complications;
- post-reaction to certain medications.
Jaundice
Hepatitis
21733 November 26
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Jaundice: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
Jaundice is a condition in which the skin and mucous membranes turn various shades of yellow. Moreover, not in all cases this indicates pathological processes in the body.
Types of jaundice
There are false and true jaundice. False jaundice occurs when carotenes accumulate in the skin due to excessive consumption of carrots, beets, oranges, pumpkin, or when certain drugs are ingested (acriquine, picric acid, etc.).
True jaundice is a consequence of an increase in the concentration of total bilirubin in the blood plasma.
Jaundice discoloration of the skin and icterus (yellow pigmentation) of the sclera occur when the concentration of total bilirubin in the blood plasma is more than 35-45 µmol/l. The milk of nursing women, pleural and pericardial effusion, ascitic fluid, and semen may have a yellow tint.
The clinical picture and duration of true jaundice depend on the underlying disease, against the background of which an increase in blood bilirubin developed.
There are:
1. Hemolytic (prehepatic) jaundice:
- jaundice due to genetic diseases (hereditary microspherocytosis, hereditary stomacytosis, etc.);
- autoimmune (acquired) hemolytic anemia.
2. Parenchymal (hepatic) jaundice:
- caused by infectious diseases (viral hepatitis A, B, C, D, E; herpetic hepatitis, cytomegalovirus hepatitis, yellow fever, infectious mononucleosis, relapsing fever, intestinal yersiniosis, psittacosis, leptospirosis, salmonellosis, pseudotuberculosis, etc.);
- caused by non-infectious diseases (acute alcoholic hepatitis, drug-induced hepatitis, liver cirrhosis, poisoning with oxidizing agents based on nitric acid, hydrazine and its derivatives, chloroethane, ethylene glycol).
3. Constitutional jaundice
(Gilbert syndrome, Crigler–Najjar syndrome, Dabin–Johnson syndrome, Rotor syndrome).
4. Mechanical (subhepatic) jaundice
occur against the background of cholelithiasis, cholangitis, cicatricial strictures of the extrahepatic bile ducts, cancer of the head of the pancreas, major duodenal papilla, and gall bladder.
Hemolytic jaundice is characterized by moderate manifestations, lemon staining of the skin, sclera and mucous membranes, a slight enlargement of the liver and often a noticeably enlarged spleen. Anemia is observed.
In acute viral hepatitis, dull aching pain in the right hypochondrium and in the joints is disturbed, the temperature rises, appetite decreases, and the patient experiences weakness. Yellowness of the skin, dark urine and insufficiently colored feces appear. There may be bruises on the skin as a result of hemorrhages. Skin itching is not typical for acute viral hepatitis, since sufficient evacuation of bile through the bile ducts is ensured. When interviewing a patient, it is possible to identify a risk factor for developing the disease (contact with patients with hepatitis, recent surgical operations, blood transfusions, injections and manipulations associated with damage to the skin and mucous membranes).
With obstructive jaundice, the clinical picture may begin acutely or develop gradually.
With the acute onset of the disease (cholelithiasis), colicky pain suddenly appears in the right hypochondrium radiating to the right and to the back, chills, and fever. Then jaundice and skin itching occur. With the gradual development of the disease (cancer of the head of the pancreas), the patient may be bothered by moderate dull or pressing pain under the right costal arch, nausea, belching, and weight loss. Palpation of the abdomen reveals pain in the right hypochondrium. The yellowness of the skin gradually increases, the urine becomes dark in color, the feces become lighter, as less bilirubin is released into the intestines.
Constitutional jaundice is characterized by moderately severe intermittent (periodic) jaundice. Selective staining of the skin of the face, nasolabial triangle, palms, soles and axillary fossae is noted. Jaundice occurs or worsens after physical or mental stress, exacerbation of a concomitant disease, or alcohol intake. The liver and spleen do not increase in size.
As a result of long-term toxic effects of high concentrations of bilirubin on the body, damage to the central nervous system develops, foci of necrosis form in parenchymal organs, the cellular immune response is suppressed, and anemia occurs. Children may experience serious complications: kernicterus, mental retardation, cerebral palsy.
Possible causes of jaundice
True jaundice is the result of an imbalance between the formation and excretion of bilirubin. The cause of this disorder may be increased formation of bilirubin (hemolytic jaundice), a failure in its transportation to liver cells and excretion by these cells, as well as deterioration in the binding processes of free bilirubin (parenchymal jaundice). Obstructive jaundice occurs as a result of deterioration in the secretion of bilirubin through the extrahepatic ducts.
The basis of the mechanism of development of hemolytic jaundice
lies hemolysis (increased destruction of red blood cells), when the life span of red blood cells is significantly shortened, sometimes to several hours. Hemolysis can be intravascular and extravascular. Intravascular hemolysis occurs as a result of mechanical destruction of red blood cells in small blood vessels (marching hemoglobinuria), turbulent blood flow due to dysfunction of prosthetic heart valves, as a result of incompatibility of red blood cells in the AB(0), Rhesus or any other system, due to direct toxic effects ( snake venom), etc.
Extravascular hemolysis occurs in the spleen and liver as a result of the capture and destruction of altered red blood cells. The spleen is capable of capturing and destroying slightly altered red blood cells, the liver – red blood cells with major disturbances.
Hepatic (parenchymal) jaundice
are caused mainly by damage to hepatocytes (liver cells). In some cases, this syndrome is associated with damage to liver cells and stagnation of bile, for example, in acute and chronic viral hepatitis. In others, the release of bilirubin is impaired (with cholestatic jaundice, cholestatic hepatitis, primary biliary cirrhosis).
Obstructive (mechanical) jaundice occurs when there is a disturbance in the outflow of bile through the extrahepatic bile ducts.
.
, enzymopathic or constitutional jaundice occurs
. The most common is Gilbert's syndrome, which develops against the background of impaired uptake of free bilirubin and its binding to glucuronic acid due to deficiency of the enzyme glucuronyltransferase.
In 60-80% of newborns, yellowness of the skin is observed, which appears on the 2-3rd day of life.
Jaundice in newborns can be caused by a high release of red blood cells during childbirth, a high content of fetal hemoglobin, rapid destruction of bilirubin after birth, and a deficiency of conjugating enzymes in the liver. In this case, the rise in bilirubin levels does not reach critical values, and the child’s condition remains satisfactory.
Breast milk jaundice (jaundice from mother's milk) is not considered a pathology and is associated with the baby's body's reaction to the fats contained in breast milk. This condition develops on the 3rd-7th day after birth, when the baby already receives a sufficient amount of mother’s milk. Stopping breastfeeding for 24-48 hours leads to a sharp decrease in bilirubin and a decrease in the severity of jaundice. If the baby continues to receive breast milk, jaundice persists for 4-6 weeks, then gradually decreases - the condition of the skin and mucous membranes returns to normal by the 12-16th week of life.
Hemolytic disease of newborns is caused by incompatibility of the blood of mother and fetus for various antigens, when the body of a pregnant woman produces antibodies that penetrate the placental barrier into the blood of the fetus and cause destruction (hemolysis) of its red blood cells. The intensity of jaundice depends on the level of bilirubin - when critical numbers are reached, this enzyme can affect neurons in the brain, resulting in the development of bilirubin encephalopathy (kernicterus).
Which doctors should I contact?
If jaundice appears, to clarify the diagnosis and determine further treatment tactics, the patient should consult a general practitioner, or if the patient is a child. In the future, a consultation with a hematologist, an infectious disease specialist, may be indicated.
Diagnosis of jaundice
To determine the cause of jaundice, a set of laboratory and instrumental examination methods is performed (according to indications):
- clinical blood test with determination of hemoglobin concentration, number of erythrocytes, leukocytes and platelets, hematocrit and erythrocyte indices (MCV, RDW, MCH, MCHC), leukoformula and ESR (with microscopy of a blood smear in the presence of pathological changes);
Types of jaundice
Depending on the reasons that caused jaundice, it is divided into forms:
- physiological (neonatal) - usually occurring in newborns (more often in weakened or premature infants) due to the adaptation of an immature enzyme system to new environmental conditions;
- parenchymal (liver) - usually occurring when the structure and function of liver cells (hepatocytes) are disrupted due to neoplasms and drug effects on the liver, or hepatitis or cirrhosis;
- hemolytic (suprahepatic) - usually occurring when red blood cells are destroyed and indirect bilirubin increases in anemia, lymphocytic leukemia, lymphosarcoma or tropical malaria;
- conjugation – usually occurring when the liver is exposed to provoking factors and congenital pathologies;
- mechanical (subhepatic) - usually occurring when direct bilirubin increases due to the inability to remove it through bile ducts blocked (by stones, tumors or helminths).
According to the duration of its course, jaundice is divided into:
- spicy;
- protracted;
- chronic.
Publications in the media
Jaundice is a symptom of various diseases: yellow discoloration of the mucous membranes, sclera and skin, due to the deposition of bile pigments in them.
Classification • Suprahepatic • Hepatic (hepatocellular) • Subhepatic (cholestatic).
Bilirubin metabolism • Indirect bilirubin (unbound, unconjugated) is formed during the breakdown of Hb in the cells of the reticuloendothelial system (80%) and other heme-containing proteins (myoglobin, cytochromes, etc.) in the liver (20%) •• Indirect bilirubin is insoluble in water, lipotropic, not excreted by the kidneys, toxic, bound to albumin in the blood •• Liver cells absorb indirect bilirubin from the blood and conjugate it with glucuronic acids (using the enzyme uridine diphosphate glucuronyltransferase [UDPGT]) to form direct (bound, conjugated) bilirubin •• Direct bilirubin water-soluble, insoluble in fat, non-toxic, can be excreted by the kidneys (when circulating in the blood in high concentrations) •• Direct bilirubin is excreted in bile •• In the intestine, under the influence of bacterial enzymes, direct bilirubin is converted into urobilinogens, which give the characteristic color to stool. Urobilinogens are partially absorbed and enter the liver through the portal vein, where they are destroyed by hepatocytes to di- and tripyrroles. Through the middle and lower rectal veins, anastomosing with the inferior vena cava system, urobilinogens enter the systemic circulation and are then excreted by the kidneys •• In healthy individuals, total serum bilirubin is mainly represented by indirect bilirubin (no more than 20 µmol/l), direct bilirubin is not more than 25% of the total, the feces are colored, traces of urobilin are present in the urine.
ETIOLOGY
• Suprahepatic jaundice is caused by increased hemolysis of red blood cells •• Poisoning with substances that cause hemolysis (for example, snake venom, sulfonamides, arsenic hydrogen) •• Transfusion of incompatible blood •• Large hematomas •• Hemolytic disease of the newborn •• Autoimmune hemolytic anemia •• Hereditary hemolytic anemia ( microspherocytic anemia of Minkowski–Choffard, sickle cell anemia, thalassemia, etc.).
• Hepatic jaundice •• Damage to hepatocytes: infectious, toxic (drugs, alcohol) hepatitis, liver cirrhosis •• Low activity of UDPHT in newborns (transient jaundice of newborns) •• Hepatic jaundice can be hereditary ••• Impaired transport of bilirubin from hepatocytes to bile ( Dubin-Johnson syndrome) ••• Absence of UDFGT - Crigler-Nayar syndrome type I ••• Significant deficiency (less than 10% of the norm) UDFGT - Crigler-Nayar syndrome type II ••• Insufficient activity of UDFGT (Gilbert-Meulengracht syndrome).
• Subhepatic jaundice develops when there is an obstruction to the outflow of bile into the duodenum •• Stones in the bile ducts •• Cancer of the biliary tract and cancer of the head of the pancreas •• Parasitic lesions of the liver •• Atresia of the biliary tract.
PATHOGENESIS • All types of jaundice are united by one symptom - hyperbilirubinemia, on which the brightness of the skin color depends: from a light lemon tint to orange-yellow and green or olive-yellow •• Yellowing of the skin and sclera begins when the bilirubin concentration is more than 26 mmol/l • • Impregnation of the skin with pigment takes time: during experimental ligation of the common bile duct, hyperbilirubinemia increases after 24 hours, but the skin becomes colored only 5–8 days later • There are 4 main mechanisms for the development of jaundice •• Increased formation of indirect bilirubin (hemolysis) •• Impaired uptake of indirect bilirubin hepatocytes and its transport inside the hepatocyte •• Impaired conjugation of indirect bilirubin in hepatocytes •• Impaired excretion of direct bilirubin from the hepatocyte into the bile capillary or obstruction at the level of larger biliary tracts.
• Hemolysis •• The concentration of indirect bilirubin in the blood serum is moderately increased (usually 2-3 times), because. liver functions are not impaired •• The stool is very intensely colored (a lot of direct bilirubin is formed and it is excreted into the bile) •• The concentration of urobilin is increased in the urine (because urobilinogen is absorbed in large quantities through the rectal veins and filtered into the urine).
• Hepatitis •• In the blood serum, the concentration of indirect (impaired uptake, transport and conjugation) and direct (impaired excretion, destruction of hepatocytes, impaired outflow due to compression of the bile ducts in the portal tracts by inflammatory infiltrates) bilirubin is increased •• In most cases, the concentration is increased to a greater extent direct bilirubin (intrahepatic cholestasis); an increase in the concentration of indirect bilirubin indicates the predominance of necrosis of hepatocytes •• Feces are usually discolored, but may not be changed •• Urine is dark due to direct bilirubin (filtered into urine) and urobilinogen (not destroyed in the liver, enters the systemic circulation and is filtered into urine ).
• Cholestasis •• The concentration of direct bilirubin is increased in the blood serum •• The feces are discolored •• The urine is dark (due to the filtration of direct bilirubin into the urine), there is no urobilin in the urine (since direct bilirubin does not enter the intestine).
• Isolated disorders of conjugation or excretion of bilirubin are characteristic of hereditary syndromes. Pathomorphology in cholestasis • Bile pigment in hepatocytes • “Bile lakes” • Dilation of bile canaliculi • Signs of damage to the bile ducts • Formation of new bile ducts.
History • Compounded family history of anemia, any manifestations of liver and biliary tract diseases • Contact with patients with infectious hepatitis, stay in hepatitis endemic regions during the last 2 months, parenteral interventions, drug administration, casual sexual intercourse during the last 6 months • Working with hepatotoxic substances • Alcohol abuse • Treatment with hepatotoxic drugs • Biliary colic, cholelithiasis • Deterioration of general condition, weight loss.
CLINICAL MANIFESTATIONS
• Onset of the disease: from the prodromal period (intoxication syndrome, nausea, vomiting, dyspepsia - with infectious hepatitis), after biliary colic (with cholelithiasis), gradual (with tumors), after infection or hypothermia (with hemolytic anemia) • Jaundice with hemolysis dim, the patient is more pale than jaundiced, with obstruction the jaundice has a green tint, with hepatitis - with an orange tint (with cholestatic forms - with a green tint).
• Suprahepatic jaundice •• Splenomegaly predominates over liver enlargement •• Intense coloring of stool •• Manifestations of anemia.
• Hepatic jaundice •• Enlargement and hardening of the liver from the onset of the disease •• Skin itching is possible •• The spleen is sometimes enlarged •• In severe forms there may be manifestations of hemorrhagic syndrome, hepatic encephalopathy •• Feces are discolored at the height of the disease, urine is dark •• With chronic hepatitis and liver cirrhosis - extrahepatic signs (telangiectasia, hepatic palms), signs of portal hypertension, ascites.
• Subhepatic jaundice •• Skin itching, as a rule, is pronounced •• The gallbladder is enlarged and painless with tumors; in case of cholelithiasis, it may not be palpable, but a pain point is found in its projection •• The liver is enlarged •• Feces are discolored, urine is dark • • Signs of the underlying disease.
LABORATORY RESEARCH
• CBC • Liver function tests • Determination of direct bilirubin and urobilin in urine • Proteinogram • Reticulocyte count, determination of osmotic resistance of erythrocytes, blood smear examination, Coombs test, bone marrow puncture are indicated for suspected hemolytic anemia • Markers of viral hepatitis in hepatic jaundice.
• Suprahepatic jaundice •• The concentration of bilirubin in the blood serum is increased mainly due to indirect bilirubin •• Other indicators of liver function tests are not changed •• Reticulocytosis •• Osmotic resistance of erythrocytes may be reduced •• Possible changes in the shape and size of erythrocytes •• Signs of bone marrow irritation .
• Hepatic jaundice •• The concentration of bilirubin in the blood serum is increased mainly due to direct bilirubin •• The activity of ALT in the blood serum is significantly increased in acute hepatitis, slightly or moderately in chronic hepatitis •• In cholestatic forms of acute hepatitis, the concentrations of cholesterol, -glutamyl transpeptidase are increased , alkaline phosphatase •• In severe forms of acute hepatitis, liver cirrhosis, the albumin content, prothrombin index, and the results of the sublimate test are reduced •• The concentration of immunoglobulins and the results of the thymol test may be increased.
• Subhepatic jaundice •• The concentration of bilirubin in the serum is increased mainly due to the direct fraction •• The concentrations of cholesterol, alkaline phosphatase, g-glutamyl transpeptidase in the blood serum are significantly increased •• The activity of ALT in the blood serum is not changed, with prolonged cholestasis it is moderately increased •• PTI may be reduced, after the introduction of menadione sodium bisulfite it increases •• The concentration of a2- and b-globulins is increased.
INSTRUMENTAL STUDIES • Ultrasound, CT of the liver, biliary tract, pancreas allows you to diagnose obstructive jaundice, as well as identify an empty gallbladder (no mechanical obstructions) in the cholestatic form of acute viral hepatitis • Plain radiography of the chest allows you to identify tumors and their metastases • With FEGDS you can assess the condition of the major duodenal papilla and the possibility of bile outflow through it • Endoscopic retrograde cholangiopancreatography or percutaneous transhepatic cholangiography is indicated for questionable ultrasound results in cases where blockage of the extrahepatic bile ducts is suspected.
TREATMENT is determined by the etiology of the disease that caused jaundice - see Hemolytic anemia, Autoimmune hemolytic anemia, Sickle cell anemia, Acute viral hepatitis, Chronic viral hepatitis, Liver cirrhosis, Gallstone disease.
ICD-10 • P58 Neonatal jaundice due to excessive hemolysis • P59 Neonatal jaundice due to other and unspecified causes • D58 Other hereditary hemolytic anemias • D59 Acquired hemolytic anemia • A27.0 Leptospirosis icteric-hemorrhagic •• E80 Disorders of porphyrin and bilirubin metabolism • P55 Hemolytic disease of the fetus and newborn • B15 Acute hepatitis A • B16 Acute hepatitis B • B17 Other acute viral hepatitis • B18 Chronic viral hepatitis • B19 Viral hepatitis, unspecified
APPLICATIONS
Familial jaundice of newborns is a transient hereditary (r) form of hyperbilirubinemia, starting with jaundice 4 days after birth and developing due to a transient defect of glucuronyl transferase associated with the presence of inhibitors of its activity in the mother’s blood; may lead to bilirubin encephalopathy and cerebral palsy. Treatment: timely replacement blood transfusions and phototherapy. Synonyms: non-hemolytic transient jaundice of newborns, Lucea-Driscoll syndrome, Lucea non-hemolytic jaundice. ICD-10. P59 Neonatal jaundice due to other and unspecified causes.
Jaundice during breastfeeding (jaundice from mother's milk) is a spontaneously transient hyperbilirubinemia of unknown etiology in healthy children in the neonatal period. It can be early (appears within 3–4 days after birth) or late (within 4–5 days after birth) with maximum manifestations at 10–15 days. The maximum concentration of bilirubin can reach 20–30 mg% (340–510 µmol/l). No cases of bilirubin encephalopathy have been described. Diagnostic test: temporary cessation of breastfeeding for 24–48 hours. Treatment: phototherapy, phenobarbital, bilirubin adsorbents. ICD-10. P59 Neonatal jaundice due to other and unspecified causes.
Nuclear jaundice is a severe form of jaundice in newborns with a high concentration of unconjugated bilirubin in the blood, deposition of bilirubin in the basal ganglia and nuclei of the brain stem, occurring with severe impairment of brain functions. Etiology: excessive levels of indirect bilirubin in the blood (over 320 µmol/l in full-term infants and 150–250 µmol/l in premature infants). Causes of hyperbilirubinemia: incompatibility of mother and fetus by blood groups; hereditary spherocytosis, non-spherocytic hemolytic anemia, hemolysis caused by a lack of vitamin K3, taking nitrofurantoin, sulfonamide drugs, etc., hemorrhages, pyloric stenosis, Hirschsprung's disease; metabolic and endocrine disorders, obstructive disorders (Dabin-Johnson-Rotor syndrome, cystic fibrosis, tumors), sepsis, intrauterine infections, neonatal respiratory distress syndrome, severe fetal erythroblastosis. Clinical picture • Yellow-colored amniotic fluid • From birth, moderate jaundice, progressing hourly • Arterial hypotension • Motor restlessness, convulsions • Enlargement of parenchymal organs • Opisthotonus, drowsiness, poor sucking, distorted or absent Moro reflex; late manifestations (after 6 months of life): deafness, paralysis, mental retardation. Diagnosis, treatment, prevention, prognosis - see Erythroblastosis fetalis; additionally treat the underlying disease. Synonym: bilirubin encephalopathy. ICD-10. P57 Kernicterus.
Gilbert's syndrome (#143500, defects of the UGT1A1 UGT1A1 gene, 1q21 q23, B) is a benign unconjugated hyperbilirubinemia of moderate severity. Prevalence is 5–7%, the syndrome more often develops in males in adolescence • In the blood serum, the concentration of indirect bilirubin periodically increases to 17–85 µmol/l. Jaundice is not constant, it can appear or intensify after infections, fasting and decrease after taking phenobarbital (tests with phenobarbital and fasting are used in diagnosis). Liver function is not impaired, the histological picture is not changed. The prognosis is favorable, no treatment is required. Synonyms: Gilbert–Meulengracht syndrome, Meulengracht jaundice, congenital hyperbilirubinemia, constitutional hyperbilirubinemia, Gilbert–Lerbouyer syndrome. ICD-10. E80.4 Gilbert's syndrome
Crigler–Nayjar syndrome (type I, 218800, r; type II, 143500, Â) is a rare hereditary disorder associated with UDPG deficiency and manifested by unconjugated hyperbilirubinemia.
• Type I •• UDFGT activity is completely absent in the liver •• Very high concentration of indirect bilirubin in the blood serum, kernicterus develops •• Patients usually die in the 1st year of life •• Phenobarbital is ineffective, plasmapheresis has a temporary effect •• Phototherapy can reduce the concentration of indirect bilirubin is 2 times •• Encephalopathy (kernicterus) can develop at any time during the first 10–20 years of life •• Liver transplantation leads to normalization of bilirubin metabolism, the prognosis improves • Transplantation should be performed at a young age, before the development of kernicterus . • Type II •• UDFGT activity is reduced to 10% or lower compared to normal •• The concentration of indirect bilirubin is high, but usually lower than in Crigler-Nayjar syndrome type I •• Phenobarbital is effective •• Sometimes the combined use of phenobarbital and phototherapy is necessary • • Patients survive to adulthood.
Abbreviations: UDPGT—uridine diphosphate glucuronyl transferase. Synonyms: congenital non-hemolytic jaundice type I, non-hemolytic hyperbilirubinemia with kernicterus. ICD-10. E80.5 Crigler–Najar syndrome.
Dubin-Johnson syndrome (*237500, defect in the gene for the tubular transporter of organic anions CMOAT, 10q24 [*601107], r) is a hereditary pigmentary hepatosis caused by impaired transport of bilirubin from hepatocytes to bile due to a mutation in the protein gene responsible for the hepatobiliary transport of various organic anions; clinically manifested by jaundice with a moderate increase in the content of direct bilirubin in the blood and its appearance in the urine; During a liver biopsy, a dark, brown-orange pigment (lipochrome) is found in hepatocytes. Treatment: reduction of bilirubinemia with phenobarbital. Synonyms: Dubin-Johnson jaundice, non-hemolytic constitutional jaundice with lipochromic hepatosis, conjugative hyperbilirubinemia type II. ICD-10. E80.6 Other disorders of bilirubin metabolism.
Rotor syndrome (*237450, conjugated hyperbilirubinemia type I, r) is clinically similar to Dubin-Johnson syndrome; Unlike the latter, with Rotor syndrome there is no accumulation of pathological pigment in liver cells, oral cholecystography is often normal, and an increase in urinary excretion of coproporphyrin is noted. ICD-10. E80.6 Other disorders of bilirubin metabolism.
Cholestasis rare • Cholestasis with gallstones, ataxia and visual impairment (214980, r). Clinically: congenital cholestasis, gallstones, cerebellar ataxia, bilateral ptosis, retinal damage, optic nerve atrophy, camptodactyly, jaundice, prurigo. Laboratory: giant cell hepatitis according to the results of liver biopsy • Intrahepatic cholestasis with impaired metabolism of trihydroxycoprostanoic acid (*214950, r). Clinically: congenital jaundice, intrahepatic cholestasis, bile duct insufficiency. Laboratory examination: absence of bile acids in bile, detection of trihydroxyprostanoic acid in bile. Synonym: alligator defect. Note. Typically, bile acids are synthesized in the liver by hydrogenation and hydroxylation of the steroid core of cholesterol with oxidation of the side chains. In some lower vertebrates, side chains are oxidized without hydroxylation (in alligators, trihydroxycoprostanic acid is the main component of bile) • Progressive intrahepatic cholestasis type 2 (*601847, 2q24, defect in the PFIC2, r gene) is a form of severe cholestatic liver disease; manifests in infancy with intermittent jaundice and cholestasis and rapidly progresses to end-stage liver failure and death in childhood. Clinically: progressive familial intrahepatic cholestasis, intermittent jaundice.
Diagnosis of jaundice
Typically, the danger is not caused by jaundice itself, but by the pathologies that caused it. As a result of intoxication of the body with bilirubin, a serious failure of its various systems can occur, and in young children - mental retardation. Therefore, accurate diagnosis of this condition is so important, for which they carry out:
- comprehensive ultrasound of the abdominal cavity and retroperitoneal space;
- laboratory blood tests (general and biochemical blood tests);
- liver functional studies;
- liver biopsy.
What is hepatitis
Hepatitis is an inflammatory process in the liver under the influence of a provoking (in most cases viral) agent, causing damage to its tissues.
Today, hepatitis is considered one of the most common infectious diseases after ARVI, influenza and chickenpox. Most often, the disease is diagnosed in young people aged 15-30 years (especially those prone to unprotected sex and drug use), another “risk group” is usually represented by medical specialists who have direct contact with blood (including infected people).
What are the symptoms of hepatitis
It must be remembered that the symptoms of hepatitis can be vivid, but sometimes they can be almost completely absent (giving time for the undetected disease to become chronic). However, quite often all types of hepatitis are characterized by common symptoms of any intensity:
- jaundice;
- change in urine color (darkening to brown)
- pain (often pressing) in the liver area;
- indigestion (nausea, vomiting with a bitter taste, diarrhea or constipation);
- weakness and increased fatigue;
- increased body temperature and headache;
- skin itching;
- increased liver size.
Hepatitis classification
In its form, hepatitis can be acute or chronic.
Depending on the provoking factor, hepatitis is divided into:
- infectious (caused by viruses or bacteria);
- toxic (when the body is poisoned with alcohol, chemicals or drugs);
- autoimmune (caused by autoimmune pathologies);
- radiation (for example, as a consequence of radiation therapy).
Viral hepatitis, in turn, is divided into types (depending on the virus that provokes the disease):
- hepatitis A (Botkin's disease) - transmitted through contaminated food and water, with an incubation period of 2-6 weeks, after the disease giving lifelong immunity to this type;
- hepatitis B - transmitted through unprotected sexual contact and through open access to blood (at home, dentistry, cosmetology, etc.) using unsterilized instruments, with an incubation period of 1.5-6 months, the duration of the acute disease is from 6 to 8 weeks (with recovery in 90% of cases) and rare transition to chronic;
- hepatitis C is the most dangerous type, transmitted in the same way as hepatitis B, but with almost unnoticeable symptoms, which is why the disease can proceed unnoticed by the patient for years in a chronic form, leading to cirrhosis and liver cancer;
- hepatitis D – transmitted in the same way as hepatitis B and C, but developing only after infection with the hepatitis B virus, easily becoming chronic and ending in cirrhosis of the liver;
- hepatitis E is transmitted in the same way as hepatitis A, with similar symptoms, usually common in African and Asian countries.
Why do people turn yellow?
Many people commonly associate the term “jaundice” with hepatitis. But is this always the case? Let's figure it out.
What's normal?
The prerequisites for the development of jaundice are disturbances in metabolism, excretion and, as a consequence, excessive accumulation of bilirubin in the tissues. It is formed as a result of the breakdown of expired red blood cells, cytochromes, and myoglobin.
There are two forms of bilirubin: unbound (or, otherwise, indirect) and bound (direct). Unbound bilirubin is toxic; normally it combines with the protein albumin and enters the liver through the bloodstream. Liver cells bind bilirubin with glucuronic acid and convert it into conjugated bilirubin. As part of the bile produced by the liver, bilirubin enters the intestines and is excreted in the feces.
There are two forms of bilirubin:
unrelated (or otherwise indirect)
and connected (direct)
Why does jaundice occur?
If changes occur at any stage of bilirubin metabolism, jaundice may develop. In this regard, the following types are distinguished:
Physiological jaundice.
It happens in children due to immaturity of the liver tissue. It appears in 60-70% of newborns on the 3rd-4th day of birth. It is more often registered in children born prematurely and is associated with the body’s adaptation to a new environment. In this case, jaundice disappears after 1-2 weeks (in premature babies - after 3-4 weeks) and does not harm the baby.
Hemolytic jaundice.
It develops as a result of the active destruction of red blood cells and the conversion of released hemoglobin into bilirubin. This type of jaundice may be a consequence of certain types of anemia, a violation of the structure of the hemoglobin protein. Red blood cells can also be destroyed by a number of medications and poisons. The cause of this type of jaundice is the Rh conflict between the woman and the fetus.
Parenchymal (liver) jaundice.
Caused by inflammation of the liver tissue caused by hepatitis viruses, toxins, hypoxia (lack of oxygen in the blood) or an autoimmune process in which liver cells are destroyed by the body's own immune system.
“The best known are hepatitis viruses A, B, C, D, E, F, G.” Quote from the material “Shield and sword against hepatitis C. How to protect yourself and your loved ones?”
Mechanical jaundice.
They talk about it when there is a violation of the outflow of bile from the liver into the duodenum. Some of the reasons contributing to the development of obstructive jaundice:
- stones and neoplasms in the bile ducts, narrowing and inflammation of the ducts;
Gallstone disease is dangerous due to its complications. Among them are cholecystitis; blockage of the gallbladder duct; obstructive jaundice; formation of fistulas (including between the gallbladder and intestine)…
You can read more about gallstone disease in our article
- tumors of the liver and pancreas;
- helminths - roundworms, in the intestinal phase of existence. They are capable of spiral movements forward, and, trying to penetrate narrow openings, can lead to serious complications: blockage of the bile ducts and their inflammation, which is manifested by obstructive jaundice and pancreatitis.
“The consequences of acute pancreatitis can be, in particular, the formation of cysts, necrosis of gland tissue, and the formation of ulcers in it.” Quote from the material “Acute pancreatitis: prevent and neutralize”
In addition, helminthiasis also contributes to the development of anemia. The red blood cells formed in this case have a shorter lifespan than normal, and therefore their breakdown (hemolysis) increases. This can also cause the appearance of jaundice.
Among other things, jaundice can be acute or chronic. If in an acute course all symptoms appear simultaneously and rapidly increase, then the chronic process is characterized by the gradual manifestation of symptoms, the change in intensity of which is associated with the course of the primary disease.
Among the serious causes of yellow skin, in addition to a number of pathologies of the digestive and blood organs, there may be disturbances in the functioning of the cardiovascular, endocrine system and lipid metabolism.
Important to remember:
A person can also “turn yellow” if the body is oversaturated with carotene. This effect is observed with excessive consumption of beets, pumpkin, carrots, citrus fruits, and persimmons. It is not difficult to distinguish false jaundice from true jaundice in this case - carotene stains only the skin, and the mucous membranes have their usual color. A similar coloration can also occur as a response to excessive intake of picric acid or medications containing acryquine.
Another reason for yellowing of the skin can be excessive consumption of various spices, fatty and spicy foods, prolonged fasting, alcohol abuse and drug use, etc.
How does jaundice manifest?
The symptoms accompanying jaundice syndrome depend on its type.
For example, jaundice due to viral hepatitis is characterized by the coloring of the skin and mucous membranes in a bright yellow-orange color against the background of loss of appetite, nausea, and vomiting. Patients' urine darkens and their stool becomes discolored.
The skin, sclera, and mucous membranes with jaundice that develops against the background of a pancreatic tumor become yellow in color with a greenish or gray tint. The patient quickly loses weight and complains of unbearable itching of the skin. In this case, feces become white, and urine the color of dark beer.
“The so-called acholic stool (light-colored) is characteristic of patients with diseases of the hepatobiliary system.” Quote from the material “Not only a colonoscopy: what will a stool test tell you?”
How to diagnose jaundice
To identify jaundice syndrome and the diseases in which it is observed, laboratory diagnostics and some other research methods are necessary. The following methods are considered informative in this case:
- general blood analysis. Thanks to it, you can, in particular, find out the level of hemoglobin and suspect the presence of an inflammatory process in the body;
- blood chemistry. Makes it possible to evaluate the content of total bilirubin and its fractions, liver enzymes, etc.;
— study of thyroid hormones, lipid profile;
— test for roundworms;
— analysis for tumor markers – CA19-9, C242, CEA;
- General urine test for jaundice. Necessary for determining the level of bilirubin and its derivatives;
— immunological analysis to detect antibodies to hepatitis viruses;
— PCR (polymerase chain reaction) to detect hepatitis viruses;
- antiglobulin test, which determines the likelihood of the risk of developing hemolytic jaundice in newborns;
—
fibrogastroduodenoscopy, ultrasound, CT and MRI of the abdominal organs will reveal inflammatory, tumor changes, and stones in the bile ducts.
The selection of the necessary diagnostic methods for a particular patient is made by the doctor who initially assessed the complaints, symptoms and suggested a possible cause for the development of the syndrome.
Treatment of jaundice
It directly depends on the underlying pathological process, the manifestation of which is jaundice, and is carried out by specialists of the relevant profile (gastroenterologist, infectious disease specialist, hematologist, surgeon, oncologist, endocrinologist, cardiologist).
Prevention of diseases accompanied by jaundice syndrome
You can prevent the development of jaundice by following simple recommendations:
— observe the rules of personal hygiene;
- monitor your diet;
- do not eat food in unsanitary conditions;
— avoid contact with virus carriers;
— observe occupational and rest hygiene;
— undergo a scheduled medical examination;
- promptly seek help from a medical facility if any symptoms occur.
Sevil Ibraimov
The article was prepared with the advisory support of specialists from Clinic Expert Smolensk
The editors recommend:
How to prepare for an abdominal ultrasound?
Where can I find the courage to make up my mind? Gastroscopy – without fear!
Acute pancreatitis: prevent and neutralize
Is it possible to cleanse the liver?
What is liver cirrhosis
Liver cirrhosis is a pathological and chronic process in the liver, as a result of which its parenchymal tissue is replaced by fibrous connective tissue (stroma). There is also a structural restructuring of the vascular bed and a decrease in the number of normally functioning hepatocytes (liver cells).
According to statistics, the global annual mortality rate from cirrhosis is about 300 thousand people, with a progressive upward trend. The disease most often affects men over 40 years of age, those prone to alcoholism, as well as patients with:
- chronic hepatitis B, C and D;
- pathologies complicated by fatty hepatosis;
- some hereditary diseases (for example, hemochromatosis);
- some autoimmune diseases;
- toxic liver damage from chemicals.
Consequences and prognosis for obstructive jaundice
The prognosis will be favorable in cases where the treatment of jaundice was timely and correct. The behavior of the patient himself is also of great importance. If you adhere to the principles of proper nutrition and strictly follow all the doctor’s instructions, the risk of relapse or complications will be minimal. Otherwise, the likelihood of recurrent obstructive jaundice will be very high. In addition, the risk of developing concomitant diseases, for example, liver failure, liver cirrhosis, encephalopathy, sepsis, etc., will increase.
What are the symptoms of cirrhosis
Symptoms of cirrhosis may be completely absent for quite a long time, or appear slightly. Most often, the disease can begin to manifest itself:
- increased fatigue and decreased mental activity, weakness and irritability;
- indigestion (a feeling of bitterness in the mouth, nausea and vomiting, flatulence and upset stool), especially in the morning;
- pain in the right hypochondrium (increased after drinking alcohol or fatty foods, as well as during physical activity);
- increased bleeding in the mucous membranes and subcutaneous hemorrhages (with characteristic spider veins at the top of the body and redness of the palms);
- itchy skin and aching joints.
A long-term progressive disease is also characterized by:
- decrease in body weight and muscle volume;
- “protrusion” of the abdomen (against the background of thinning limbs with thickening fingertips) with an enlarged liver and spleen, ascites;
- painful swelling of the joints;
- jaundice;
- decreased sexual function and secondary sexual characteristics.
Diagnosis of cirrhosis
Diagnosis of the disease is based on the results of a comprehensive examination of the condition of the liver and organic systems most closely related to its work, as well as establishing the causes of cirrhosis. To do this:
- comprehensive ultrasound of the abdominal organs and retroperitoneal space (kidneys and adrenal glands), as well as portal vessels;
- laboratory blood test (including biochemical, for the presence of hepatitis viruses, as well as a coagulogram);
- esophagogastroduadenoscopy to identify dilated veins of the esophagus;
- liver biopsy and scintigraphy.
Treatment of cirrhosis
Typically, treatment of liver cirrhosis is aimed at stopping (in the initial stages of the disease) or slowing down progressive pathological processes. Conservative therapy is strictly individual and often consists of:
- taking medications (hepatoprotectors);
- following a diet (with the obligatory exclusion of alcohol, fatty and canned foods);
- excluding physical and emotional overload.
Treatment of end-stage cirrhosis can only be associated with liver transplantation.
It must be remembered that only a preventive comprehensive ultrasound of the abdominal organs in most cases can help to recognize pathological changes in the liver in time, even before the first symptoms appear! Save your health!
Principles of treatment of obstructive jaundice
The main objectives when drawing up a treatment plan are the elimination of cholestasis (stagnation of bile) and the prevention of liver failure. To do this, the doctor draws up a comprehensive program, which can include both conservative and surgical methods.
Diet for obstructive jaundice
It is necessary to follow certain nutritional rules both before the main treatment and after its completion. Patients with obstructive jaundice are advised to maintain a drinking regime, as water accelerates the excretion of bilirubin, thereby reducing its negative effect on the body. It is also very important to completely avoid alcohol, very fatty and fried foods, mayonnaise, sauces, and hot seasonings. Food should be consumed in small portions 5-6 times a day. In this case, it is necessary to monitor the temperature of the dish. It shouldn't be too hot or cold. The best option is warm food, as it helps regulate the secretion of bile, which is especially important for obstructive jaundice.
Other general recommendations regarding diet include limiting the amount of salt in the diet. It is known that excess salt contributes to fluid retention in the body, causes swelling and makes it difficult to remove harmful substances from the body. Patients with obstructive jaundice are recommended to consume no more than 4 grams of salt per day. In general, the exact nutrition plan, calorie content and composition of dishes are selected individually for each patient, taking into account his preferences. There are lists of permitted and prohibited foods, as well as those foods that should be limited. It is these lists that the doctor is guided by when drawing up a nutrition program. For example, permitted products include:
- Vegetables (carrots, cucumbers, cabbage, tomatoes, broccoli).
- Bananas and apples.
- Dried fruits.
- Various porridges (buckwheat, oatmeal, pearl barley).
- Bran bread, pasta, crispbread.
- Jam, honey, marmalade.
- Lean meat (rabbit, beef), poultry (chicken breasts, turkey fillet) and fish (pollock, hake).
- Fruit juices and tea.
A diet for obstructive jaundice involves the complete exclusion of canned vegetables, legumes, grapes, baked goods, white bread, full-fat milk, cream, fatty meats and fish, smoked meats, carbonated drinks, coffee, and animal fats.
Drug treatment
Drug therapy for obstructive jaundice is prescribed to reduce the severity of symptoms, prepare the patient for surgery and reduce the risk of complications. The extent of medical care largely depends on the degree of jaundice. For example, in severe cases, drug treatment is carried out in an intensive care unit and includes:
- Massive infusion therapy.
- Forced diuresis.
- Vitamin therapy.
- Hepatoprotectors.
- Amino acids.
- Metabolism stimulants.
- Hormonal drugs.
To relieve symptoms, in mild forms of obstructive jaundice, antispasmodics, enveloping drugs, antacids and other medications can be prescribed.
Surgery
Surgical treatment is the only effective method that allows you to restore the patency of the bile ducts and thereby eliminate the cause of obstructive jaundice. All known types of operations can be divided into two groups: minimally invasive techniques and direct operations.
Minimally invasive methods of surgical treatment
This group of methods is highly effective and low-traumatic, but it is impossible to apply them to all patients in a row due to certain limitations. Minimally invasive treatment of obstructive jaundice is carried out using endoscopic techniques and percutaneous transhepatic cholangiostomy. Endoscopic operations can be of the following types:
- Endoscopic papillosphincterotomy and lithoextraction.
- Local lithotripsy and lithoextraction.
- Bougienage and stenting of the bile ducts.
In these cases, to treat obstructive jaundice, a gastroduodenoscope with special instruments is used that allow crushing and removing stones, installing stents, and removing tissue. Endoscopic operations in most cases are performed without general anesthesia and do not require long recovery time.
Percutaneous transhepatic cholangiostomy is used in cases where it is impossible to perform decompression of the biliary tract using a gastroduodenoscope. The essence of the operation is to install a drainage tube under ultrasound or x-ray control. In this case, the skin, muscles of the anterior abdominal wall and liver tissue are pierced with a special puncture needle. In the future, the drainage tube can be used not only to drain bile, but also to introduce antibacterial or other drugs directly into the bile ducts.
Direct surgical interventions allow you to create full access to the gallbladder and eliminate obstructive jaundice of any complexity. The surgeon can perform anastomoses, install stents, and perform reconstructive operations. The intervention can be performed using laparoscopic instruments or the classic open cavity method. The latter option is the most traumatic, requires long-term rehabilitation and is accompanied by an increased risk of complications, so it is used only in the treatment of complex cases of obstructive jaundice.
General principles of treatment of obstructive jaundice
Generally speaking, the treatment tactics for obstructive jaundice include two stages. At the first stage, conservative therapy and minimally invasive methods of surgical treatment are prescribed. It is recommended to carry out such treatment in the first 2-3 days from the moment the patient is admitted to the hospital. If these methods are ineffective, then move on to the second stage of treatment of obstructive jaundice, which involves more radical methods. Treatment at the peak of jaundice is associated with a high risk of developing postoperative complications, so it is carried out only if there are vital indications.
Other treatments
Effective treatment of jaundice involves eliminating the underlying disease that led to the development of this symptom. To do this, it is necessary to use either conservative or surgical methods. Other treatment options for obstructive jaundice, in particular traditional medicine, home treatment and self-medication will not help achieve the desired result. For a certain period of time, they will help hide the symptoms and alleviate the patient’s condition, but the main process will continue to progress and lead to the development of complications. Therefore, when the first signs of obstructive jaundice appear, it is necessary to seek qualified medical help, which will help radically solve the problem.