Posted by Andro-gynecology clinic at 2018-06-25. Posted on Women, Treatment Methods
The Androgynecological Clinic selects vaginal pessaries and rings for the treatment of prolapse of the uterus and vaginal walls, and urinary incontinence. The article will talk about the conservative treatment of pelvic organ prolapse and stress urinary incontinence, and specifically about the vaginal rings and pessaries of Dr. Arabin (Germany).
Back to contents
What are vaginal pessaries and rings
Vaginal pessaries are devices that are placed in the vagina and prevent prolapse of the uterus and vaginal walls. We wrote in detail about prolapse and prolapse of the vaginal walls and uterine prolapse here.
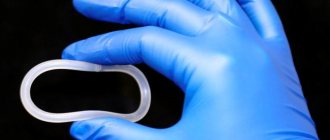
It should be understood that this method does not lead to a cure, it is a kind of “crutch” that helps a woman alleviate the symptoms of the disease and improve the quality of life. The method is simple, understandable and has been used successfully for a long time. Currently, thanks to modern technologies and hypoallergenic (inert) materials, various forms of pessaries have been created for different forms of pelvic organ prolapse (POP) in women (Figure 1). They are also successfully used for stress urinary incontinence (stress).
Figure 1. Various forms of vaginal pessaries
Back to contents
In what cases are pessaries used?
The need to wear vaginal pessaries and rings arises when the patient has complaints, usually with a moderate degree of pelvic organ prolapse. Most women with initial and moderate degrees of prolapse without complaints do not want to use pessaries, despite the fact that this method is a good prevention of disease progression. There are situations when surgical treatment is impossible for a number of reasons, or the woman herself does not want to undergo surgery. In such a situation, especially in the later stages of the disease, the only effective method of conservative treatment is vaginal pessaries.
Indications for wearing vaginal pessaries
- 2-4 degrees Rectocele (prolapse of the rectum);
- 2-4 degrees Cystocele (prolapse of the bladder);
- 2-4 degree of uterine prolapse;
- Stress incontinence;
- Contraindications to surgical treatment of pelvic organ prolapse and urinary incontinence;
- Woman's refusal to undergo surgery.
Back to contents
How pessaries are selected
Various degrees and combinations of forms of prolapse of the walls of the vagina and uterus, as well as the presence or absence of urinary incontinence, require the use of a certain form of this device. Only a specially trained doctor can choose the shape and size. In addition, this requires additional examination to identify contraindications.
Examination before using vaginal pessaries
- Ultrasound examination of the pelvic organs;
- Ultrasound of the bladder and residual urine;
- Flora smear;
- Smear for oncocytology;
- Uroflowmetry - for urinary incontinence;
- Gynecological examination.
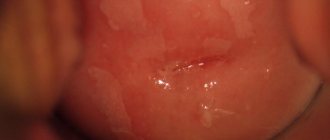
At the appointment, the doctor conducts a gynecological examination, determines the shape, degree of prolapse and the approximate size of the adaptation (size) ring, after which he installs it in the patient’s vagina (Fig. 2). Next, it is recommended for the patient with the adaptation ring installed for 15-20 minutes. walk around, climb the stairs, go to the toilet and return for a second examination. If the patient does not experience discomfort and the ring does not fall out of the vagina, this size of adaptation ring is considered suitable. Using a special table, the appropriate size of the pessary of the desired shape is selected, and an explanatory conversation is held about the rules of wearing and use.
Fig 2. Vaginal ring installed
A follow-up appointment is scheduled after 2-4 weeks. It is determined whether the patient uses the pessary correctly, the presence of complaints and the reaction of the vaginal mucosa to a foreign body.
Selection of vaginal pessaries
Back to contents
NuvaRing, 3 pcs., 15 mcg+120 mcg/24 h, vaginal rings
If any of the diseases, conditions or risk factors listed below are present, the benefits of using the drug NuvaRing® and the possible risks for each individual woman should be assessed before she starts using the drug NuvaRing®. In case of exacerbation of diseases, deterioration of the condition, or the occurrence of any of the conditions listed below for the first time, a woman should consult a doctor to decide on the possibility of further use of the drug NuvaRing®.
Circulatory disorders
The use of hormonal contraceptives may be associated with the development of venous thrombosis (deep vein thrombosis and pulmonary embolism) and arterial thrombosis, as well as associated complications, sometimes fatal.
The use of any COC increases the risk of developing VTE compared to the risk of VTE in patients not using COCs. The greatest risk of developing VTE is observed in the 1st year of COC use. Data from a large prospective cohort study of the safety of various COCs suggest that the greatest increase in risk compared with the risk in women not using COCs is observed in the first 6 months after starting COC use or resuming their use after a break (4 weeks or more). In non-pregnant women not using oral contraceptives, the risk of developing VTE is 1 to 5 per 10,000 woman-years (WY). In women using oral contraceptives, the risk of developing VTE ranges from 3 to 9 cases per 10,000 women. However, the risk increases to a lesser extent than during pregnancy, when it is 5–20 cases per 10,000 YL (pregnancy data are based on the actual duration of pregnancy in studies; when converted to a pregnancy duration of 9 months, the risk ranges from 7 to 27 cases per 10,000 ZhL). In postpartum women, the risk of developing VTE ranges from 40 to 65 cases per 10,000 women. VTE is fatal in 1–2% of cases.
According to research results, the increased risk of developing VTE in women using NuvaRing® is similar to that in women using COCs (adjusted risk ratio, see Table 2 below). A large prospective observational study, TASC (Transatlantic Active Study of the Safety of the Drug NuvaRing® for Cardiovascular Stress), assessed the risk of developing VTE in women who started using the drug NuvaRing® or COCs, switched to NovaRing® or COCs from other contraceptives, or resumed using the drug NuvaRing® ® or COC, in a population of typical users. Women were followed up for 24–48 months. The results showed a similar level of risk of developing VTE in women using the drug NuvaRing® (8.3 cases per 10,000 YL) and women using COCs (9.2 cases per 10,000 YL). For women using COCs other than those containing desogestrel, gestodene and drospirenone, the incidence of VTE was 8.5 cases per 10,000 women.
A retrospective cohort study initiated by the FDA (US Food and Drug Administration) showed that the incidence of VTE in women who started using the drug NuvaRing® was 11.4 cases per 10,000 YL, while in women of those who started using COCs containing levonorgestrel, the incidence of VTE is 9.2 cases per 10,000 young people.
table 2
Assessment of the risk (risk ratio) of developing VTE in women using the drug NuvaRing®, compared with the risk of developing VTE in women using COCs
| Epidemiological study, population | Comparator(s) | Risk ratio (RR (95% CI) |
| TASC (Dinger, 2012). Women who started using the drug (including again, after a break) and switched from other means of contraception | All available COCs during the study1 | OR2: 0.8 (0.5–1.5) |
| Available COCs, except those containing desogestrel, gestodene, drospirenone | OR2: 0.9 (0.4–2) | |
| "FDA Initiated Study" (Sydney, 2011). Women who started using combined hormonal contraceptives (CHCs) for the first time during the study period | COCs available during the study period3 | OR4: 1.09 (0.55–2.16) |
| Levonorgestrel/0.03 mg ethinyl estradiol | RR4: 0.96 (0.47–1.95) |
1Incl. low-dose COCs containing the following progestins: chlormadinone acetate, cyproterone acetate, desogestrel, dienogest, drospirenone, ethynodiol diacetate, gestodene, levonorgestrel, norethindrone, norgestimate or norgestrel.
2Taking into account age, body mass index, duration of use, history of VTE.
3 Incl. low-dose COCs containing the following progestins: norgestimate, norethindrone or levonorgestrel.
4Taking into account age, place and year of inclusion in the study.
There are extremely rare cases of thrombosis of other blood vessels (for example, arteries and veins of the liver, mesenteric vessels, kidneys, brain and retina) when using COCs. It is unknown whether these cases are related to the use of COCs. Possible symptoms of venous or arterial thrombosis may be unilateral swelling and/or pain in the lower extremity, local increase in temperature in the lower extremity, hyperemia or discoloration of the skin on the lower extremity; sudden severe chest pain, possibly radiating to the left arm; attack of shortness of breath, cough; any unusual, severe, prolonged headaches; sudden partial or complete loss of vision; double vision; slurred speech or aphasia; dizziness; collapse, accompanied or not accompanied by a focal epileptic seizure; sudden weakness or severe numbness on one side of the body or any part of the body; movement disorders; acute stomach
Risk factors for the development of venous thrombosis and embolism:
- age;
- presence of diseases in the family history (venous thrombosis and embolism in brothers/sisters at any age or in parents at a young age). If a hereditary predisposition is suspected, before starting any hormonal contraceptives, the woman should be referred to a specialist for consultation;
- prolonged immobilization, major surgical interventions, any surgical interventions on the lower extremities or serious trauma. In such situations, it is recommended to stop using the drug (in the case of a planned operation, at least 4 weeks in advance) with subsequent resumption of use no earlier than 2 weeks after complete restoration of motor activity;
— obesity (body mass index more than 30 kg/m2);
- possibly thrombophlebitis of the superficial veins and varicose veins.
There is no consensus on the possible role of these conditions in the etiology of venous thrombosis.
Risk factors for the development of complications of arterial thromboembolism:
- age;
- smoking (with heavy smoking and with age, the risk increases even more significantly, especially in women over 35 years of age);
- dislipoproteinemia;
— obesity (body mass index more than 30 kg/m2);
- increased blood pressure;
- migraine;
- heart valve disease;
- atrial fibrillation;
- presence of diseases in the family history (arterial thrombosis in brothers/sisters at any age or parents at a relatively early age).
If a hereditary predisposition is suspected, the woman should be referred to a specialist for consultation before starting any hormonal contraceptives. Biochemical factors that may indicate hereditary or acquired predisposition to venous or arterial thrombosis include activated protein C resistance, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant).
Other conditions that can lead to unwanted circulatory problems include diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome and chronic inflammatory bowel disease (such as Crohn's disease or ulcerative colitis), as well as sickle cell anemia. It is necessary to take into account the increased risk of thromboembolism in the postpartum period.
An increase in the frequency or severity of migraine (which may be a prodromal symptom of cerebrovascular accidents) while using hormonal contraceptives may be a reason to immediately discontinue use of hormonal contraceptives.
Women using CHCs should be advised to consult a doctor if possible symptoms of thrombosis occur. If thrombosis is suspected or confirmed, CHC use should be discontinued. In this case, it is necessary to use effective contraception, since anticoagulants (coumarins) have a teratogenic effect.
Risk of developing tumors
The most important risk factor for developing cervical cancer is infection with the human papillomavirus. Epidemiological studies have shown that long-term use of COCs leads to an additional increase in this risk, but it remains unclear to what extent this is due to other factors, such as more frequent cervical smears and differences in sexual behavior, including. use of barrier contraceptives. It remains unclear how this effect is related to the use of the drug NuvaRing®.
A meta-analysis of 54 epidemiological studies found a small increase (1.24) in the relative risk of breast cancer in women taking COCs. The risk gradually decreases over 10 years after stopping the drugs. Breast cancer rarely develops in women under 40 years of age, so the additional incidence of breast cancer in women who take or have taken COCs is small compared to the overall risk of developing breast cancer. Breast cancer diagnosed in women who use COCs is clinically less severe than cancer diagnosed in women who have never used COCs. The increased risk of breast cancer may be due to both earlier detection of breast cancer in women taking COCs, the biological effects of COCs, or a combination of both.
In rare cases, women taking COCs have developed benign, and even more rarely, malignant liver tumors. In some cases, these tumors led to the development of life-threatening bleeding into the abdominal cavity. The doctor should consider the possibility of a liver tumor in the differential diagnosis of diseases in a woman taking NuvaRing® if symptoms include acute pain in the upper abdomen, liver enlargement, or signs of intra-abdominal bleeding.
Other states
Women with hypertriglyceridemia or a corresponding family history have an increased risk of developing pancreatitis when taking hormonal contraceptives.
Many women taking hormonal contraceptives experience a slight increase in blood pressure, but clinically significant increases in blood pressure are rare. A direct connection between the use of hormonal contraceptives and the development of arterial hypertension has not been established.
If a constant increase in blood pressure is observed when using the drug NuvaRing®, you should contact your doctor to decide whether it is necessary to remove the vaginal ring and prescribe antihypertensive therapy. With adequate blood pressure control using antihypertensive drugs, it is possible to resume use of the drug NuvaRing®.
During pregnancy and during the use of COCs, the development or worsening of the following conditions was noted (although their relationship with the use of contraceptives has not been definitively established): jaundice and/or itching caused by cholestasis, formation of gallstones, porphyria, systemic lupus erythematosus, hemolytic uremic syndrome, Sydenham's chorea (minor chorea), herpes of pregnancy, hearing loss due to otosclerosis, (hereditary) angioedema.
Acute or chronic liver dysfunction may serve as a basis for discontinuation of the drug NuvaRing® until normalization of liver function indicators. Recurrence of cholestatic jaundice, previously observed during pregnancy or during the use of sex hormones, requires discontinuation of the drug NuvaRing®.
Although estrogens and progestogens may influence peripheral insulin resistance and tissue glucose tolerance, there is no evidence to support the need to change hypoglycemic therapy during the use of hormonal contraceptives. However, women with diabetes should be under constant medical supervision when using NuvaRing®, especially in the first months of contraception.
There is evidence of a worsening of Crohn's disease and ulcerative colitis with the use of hormonal contraceptives.
In rare cases, pigmentation of the facial skin (chloasma) may occur, especially if it occurred earlier during pregnancy. Women predisposed to the development of chloasma should avoid exposure to sunlight and UV radiation while using NovaRing®.
The following conditions may prevent the ring from being inserted correctly or may cause it to fall out: cervical prolapse, bladder and/or rectal hernia, severe chronic constipation.
In very rare cases, women have unintentionally inserted the NuvaRing® vaginal ring into the urethra and possibly into the bladder. When symptoms of cystitis appear, it is necessary to consider the possibility of incorrect insertion of the ring.
Cases of vaginitis have been described during use of the drug NuvaRing®. There is no evidence that treatment of vaginitis affects the effectiveness of the use of the drug NuvaRing®, as well as evidence of the effect of the use of the drug NovaRing® on the effectiveness of treatment of vaginitis.
Very rare cases of difficult ring removal have been described that required removal by a medical professional.
Medical examination/consultation
Before prescribing the drug NuvaRing® or resuming its use, you should carefully review the woman’s medical history (including family history) and conduct a gynecological examination to exclude pregnancy. It is necessary to measure blood pressure, conduct an examination of the mammary glands, pelvic organs, including a cytological examination of cervical smears and some laboratory tests, to exclude contraindications and reduce the risk of possible side effects of the drug. The frequency and nature of medical examinations depend on the individual characteristics of each patient, but medical examinations are carried out at least once every 6 months. A woman should read the instructions and follow all recommendations. The woman should be informed that NuvaRing® does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Reduced efficiency
The effectiveness of NovaRing® may decrease if the regimen is not followed or if concomitant therapy is carried out.
Changes in the nature of menstruation
During use of the drug NovaRing®, acyclic bleeding (spotting or sudden bleeding) may occur. If such bleeding is observed after regular cycles with the correct use of the drug NuvaRing®, you should contact your gynecologist to conduct the necessary diagnostic studies, incl. to exclude organic pathology or pregnancy. A diagnostic curettage may be required. Some women do not bleed after the ring is removed. If the drug NuvaRing® was used according to the instructions, it is unlikely that the woman is pregnant. If the recommendations of the instructions are not followed and there is no bleeding after removing the ring, as well as if there is no bleeding for two cycles in a row, pregnancy must be excluded.
Effects of ethinyl estradiol and etonogestrel on a sexual partner
The possible pharmacological effects and extent of exposure of ethinyl estradiol and etonogestrel to male sexual partners (due to absorption through penile tissue) have not been studied.
Ring damage
In rare cases, when using the drug NuvaRing®, ring rupture was observed.
The core of the drug NuvaRing® is solid, so its contents remain intact, and the release of hormones does not change significantly. If the ring ruptures, it usually falls out of the vagina (see the recommendations in the subsection What to do if the ring has been temporarily removed from the vagina
in the section “Method of administration and dosage”). If the ring ruptures, a new ring must be inserted.
Ring falling out
Sometimes the NuvaRing® vaginal ring may fall out of the vagina, for example, if it is inserted incorrectly, a tampon is removed, during sexual intercourse, or due to severe or chronic constipation. In this regard, it is advisable for a woman to regularly check the presence of the NuvaRing® vaginal ring in the vagina. If the NuvaRing® vaginal ring falls out of the vagina, you must follow the recommendations of the subsection What to do if the ring has been temporarily removed from the vagina
in the section "Method of administration and dosage".
Impact on the ability to drive vehicles and operate machinery.
Based on information about the pharmacodynamic properties of the drug NovaRing®, it can be expected that it does not affect the ability to drive vehicles and operate machinery.
Rules for using vaginal pessaries
Vaginal rings can be left in the vagina for up to 5-6 days; cubic and mushroom-shaped pessaries cannot be worn for more than 24 hours; they are removed daily before bed! If a woman does not need the ring while sleeping, it is also removed. After removal, the pessary should be washed under warm running water and soap and dried. It should be stored in a plastic container or bag.
The pessary is inserted in the morning in a standing position with a raised leg or squatting, this is described in detail in the video above. To facilitate insertion, you can use a hygienic gel.
Back to contents
Indications for use
Answering the question why a uterine ring is needed, doctors recommend using it in the following cases:
- with prolapse/loss of the genitals;
- for the treatment of urinary incontinence syndrome;
- to support the pelvic organs before surgical treatment;
- during the rehabilitation period after genital surgery to reduce the load on the muscles.
The length of time it remains in the vagina ranges from several days to three weeks and depends on why the doctor prescribed wearing a pessary. Treatment can be combined with other conservative methods (wumbuilding, physical therapy, exercise equipment to strengthen the muscles of the pelvic organs).
Other conservative treatments for pelvic organ prolapse
When a diagnosis of pelvic organ prolapse is made, it is recommended to carry out protective measures aimed at reducing increased intra-abdominal pressure.
Preventive actions
- Lifestyle changes and weight loss;
- Reducing the intensity of physical activity (limiting heavy lifting);
- Change of occupation - transfer to light work;
- Prevention of constipation and respiratory diseases accompanied by a chronic increase in abdominal pressure.
Exercises to strengthen the pelvic floor muscles
In the initial stages of prolapse of the vaginal walls, it is possible to perform exercises to strengthen the pelvic floor muscles (Kegel exercises). These exercises are effective only in the early stages of the disease when the muscles of the pelvic floor and the tendon center of the perineum are preserved. If the pelvic floor muscles are incompetent, these exercises will only do harm - they will lead to the progression of pelvic organ prolapse.
Physiotherapy
There are various methods of influencing physical factors (laser, magnetic field) on the vaginal walls and underlying tissues. This method can lead to a reduction in the degree of prolapse by improving tissue nutrition - increasing the tone of the pelvic floor. The use of physical factors is effective in the early stages of the disease, when there are still no complaints and the diagnosis is made only upon examination in a chair.
Physiotherapy is widely used as a recovery stage after surgical treatment and in the prevention of the development of prolapse in the postpartum period.
Volume-forming methods based on hyaluronic acid
The method is used to treat urinary incontinence in the early stages of the disease. It consists of creating additional support for the urethra during stress urinary incontinence through tissue tension by creating additional volume. The effect is temporary, from 6 to 8 months. for hyaluronic acid fillers, up to a year or more for lipofilling.
Injections and fillers of hyaluronic acid are used to treat degenerative processes in the tissues of the perineum and pelvic floor; the effect is very pronounced but also temporary.
All of these methods are prescribed when a diagnosis has been established, after a preliminary examination, because they have contraindications. The most pronounced effect can be achieved by combining these techniques, taking into account contraindications to each of them. It is not possible to do this on your own! We recommend that all women at risk undergo a specialized consultation with a gynecologist at the Androgynecological Clinic to identify pelvic organ prolapse
Back to contents
Risk group for the development of uterine and vaginal prolapse
Women who have aggravating factors that contribute to the development of POP are at risk.
Risk factors
- Childbirth with a large fetus, traumatic birth, rapid labor, multiple pregnancies, multiparous women;
- Hard physical work, sports;
- Sedentary lifestyle and work (doctors, teachers, office workers, etc.);
- Connective tissue dysplasia;
- Obesity;
- Chronic constipation and cough (chronic bronchitis, smoking);
- Age over 45 years - hypoestrogenism and associated dystrophic changes in the tissues of the pelvic floor and lower parts of the genitourinary system.
READ SUMMARY
Consultation and treatment of women with pelvic organ prolapse in our clinic is carried out by a regional representative of the Pelvioperinatology Center (St. Petersburg):
Types and sizes of uterine rings
The devices are produced in a wide range of sizes from medical plastic or silicone. Taking into account why and for what purpose the uterine ring is needed, it may have a special spring in its design that maintains the shape of the product and evenly distributes pressure along the entire vaginal wall.
All uterine rings can be divided into two types, based on why they are used:
- Supportive – thick and thin uterine rings, cup, urethral and combined models. The required product is prescribed by the gynecologist based on why the pessary is needed. After installation, it supports the pelvic organs in an anatomically correct position, preventing the development of genital prolapse.
- Fillers – mushroom/cuboid models. Why are such pessaries needed? After insertion, they fill the volume of the vagina, preventing prolapse of the genitals. They are prescribed when prolapse progresses, when standard uterine rings are not effective enough.
The correct size of the product plays an important role in treatment. The manufacturer indicates this parameter on the packaging. It corresponds to the diameter of the pessary and can range from 55 to 95 mm.
(see video after article)
The size, as well as the desired shape of the uterine ring, can only be determined by a specialist. For treatment to be effective, you need to undergo a gynecological examination, after which the gynecologist will prescribe a suitable model, taking into account why the patient needs it. The first installation/removal should also be entrusted to a doctor.