Vaginal discharge may be normal or indicate an intimate infection.
In a healthy woman, mucus helps moisturize the vagina, it is thick and milky white or transparent and stretchy - it all depends on the phase of the menstrual cycle. All other types of discharge, except menstrual discharge, indicate problems in the intimate area.
Normal vaginal discharge contains 99% lactobacilli, which have a beneficial effect on the bacterial flora of the vagina, and 1% are pathogenic microorganisms such as intestinal bacteria or Staphylococcus aureus. When the balance of the bacterial flora is disturbed and the level of pathogenic microorganisms increases, we can talk about the occurrence of an intimate infection, the most common symptom of which is discharge with an abnormal color and an unpleasant odor.
White vaginal discharge - what does this mean?
White vaginal discharge is completely normal. The problem arises when they acquire a dense consistency that begins to resemble cottage cheese, and numerous lumps appear in them. Such symptoms may indicate an infection of the yeast (fungus) Candida albicans, which colonizes the vagina, perineal area, labia and anus, also causing additional problems.
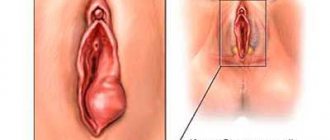
The most common symptoms of thrush include persistent itching and burning in the intimate area and vagina, redness and swelling of the labia, and a feeling of dryness in the vagina. Usually the white discharge from a yeast infection does not have a bad odor, but sometimes you may notice a yeast-like odor.
White vaginal discharge
How to treat white vaginal discharge? First of all, it is recommended to consult a gynecologist who will prescribe suppositories or ointments with antifungal substances. Most often, the use of both forms of medication is required - suppositories heal the infection in the vagina and restore normal microflora of the genital tract, while ointments applied to the labia and anal area minimize unpleasant symptoms - itching and burning.
Normal or pathological?
Any gynecologist will be able to confirm that women have different discharges that are normal.
As a rule, the discharge does not cause problems or discomfort, and is colorless in color, sometimes with a tint of white. On underwear, such discharge is noticeable in yellow shades.
Moreover, it should be clarified that the discharge does not cause the patient an unpleasant sensation as such, and also does not provoke itching and a burning sensation in the vagina, as well as a sharp and characteristic odor.
The volume of discharge begins to increase when the woman is aroused.
This can also occur after completion of sexual intercourse. Discharge is noticed during ovulation, the middle of the cycle. This is explained, first of all, by such a process as ovulation, which is inevitable for any woman.
Most women often mention to doctors about the increased volume of discharge during early pregnancy. This cannot be a reason for concern and does not at all mean that the embryo is in danger. Usually, over time, the discharge will normalize and the volume will decrease. This is explained, first of all, by the fact that a woman’s hormonal background changes.
Pathology
There are cases when discharge can serve as a cause for concern and an indicator that one of the pathologies is occurring.
The first factor causing concern is a change in the microflora of the vagina itself. It is in this place that a large volume of microorganisms, which form the basis of the microflora, is concentrated.
Among the microorganisms there are those that are classified as opportunistic microorganisms, as well as those that begin their development under specific conditions, as a result of which various kinds of diseases arise.
In this case, we mean two main diseases that are common and not sexually transmitted, and also are not considered sexually transmitted diseases:
- candidiasis;
- gardnerellosis.
Candidiasis
Often, women notice white discharge, produced in large volumes, and somewhat similar to curdled flakes.
Such discharge causes severe itching and a burning sensation. In such situations, most often all symptoms are caused by a fungal pathogen of the candida species . Women experience swelling of the vulva and labia during this period.
The treatment process should be started only when there is enough evidence to believe that the symptoms correspond to the disease and the result of the smear taken for diagnosis is really not the best.
There are a number of medicines that promote the recovery of women and can fight thrush.
Gardnerellosis
There are also other symptoms that appear in the form of grayish discharge with a rotten odor, reminiscent of rotten fish. This infection is called gardnerellosis.
The causative agent of this disease is gardnerella. Diagnosis of this disease also occurs by taking a smear to check the condition of the flora. In exceptional cases, green discharge is possible, scaring and misleading women.
Treatment
When diagnosing these two diseases, it is necessary to undergo a full course of examination and diagnosis.
It is because of diseases such as thrush and gardnerella that the microflora of the vaginal environment is disrupted and subject to change. When treating gardnerella disease, it is necessary at the first stage to eliminate the pathogenic flora, and then restore the normal microflora that a healthy woman should have.
These two types of diseases usually develop under the following conditions:
- excessive intake of drugs related to antibiotics;
- frequent change of sexual partners;
- use of hormonal contraception;
- complete absence of barrier contraception;
- douching with chlorine;
- use of spermicides and lubricants.
It is worth saying that these two diseases are common not only for women, but also for men. Doctors insist on treating both partners, regardless of whether the man exhibits symptoms or not. This is necessary to eliminate infection after therapy.
Is yellow vaginal discharge a cause for concern?
Not every yellow-colored vaginal mucus indicates an intimate infection. Yellowish discharge - cervical mucus - also appears outside the ovulation period. If yellow discharge is not accompanied by any additional symptoms, this is a sign that the bacterial flora of the vagina is in good condition.
Yellow vaginal discharge
In the case of discharge, the occurrence of which is associated with itching, burning in the intimate area, as well as an unpleasant odor, this may indicate the occurrence of cervical erosion.
Yellow and greenish discharge also occurs with trichomoniasis. Other signs of trichomoniasis:
- pain in the lower abdomen;
- itching and redness around the vagina and labia;
- frequent urination;
- pain during intercourse;
- Possible menstrual irregularities.
Treatment of this intimate infection requires the use of an antibiotic.
Is this normal?
Dark brown discharge is mainly caused by normal processes in the female body and means that the fetal egg has been attached. This phenomenon is called implantation bleeding. But if conception has occurred, then the daub may well indicate that violations have occurred. If you know for sure that you are pregnant and encounter spotting during the period when you usually had your period, this may mean:
- risk of miscarriage;
- ectopic pregnancy;
- fetal freezing;
- hormone failure;
- infections and inflammations;
- diseases of the cervix.
As a conclusion, if you have brown discharge, you need to consult a doctor in a timely manner and, of course, do a test. If the result is positive, you will know that conception has taken place, then you will need to do an ultrasound.
Green vaginal discharge is a bacterial infection
Vaginal discharge with a characteristic greenish color often indicates a bacterial infection (vaginosis), which can be caused, for example, by pathogenic microorganisms of the species Gardnerella vaginalis.
Gardnerellosis is most often accompanied by burning and itching of the perineum, swelling of the labia, pain when urinating, as well as a characteristic fishy odor from the vagina. If these symptoms appear, consult a gynecologist, as ignoring them can lead to serious health problems - bacteria can enter the cervical canal.
Burning and itching of the perineum
Green vaginal discharge may also indicate atrophic vaginosis, which affects women during menopause and when estrogen levels in the blood are low.
Recommendations from gynecologists
- A common cause of brown discharge without pain and odor in the middle of the menstrual cycle is a violation of personal hygiene standards. Perform water procedures 1-2 times a day. You shower too rarely or, conversely, wash yourself 10 times a day.
- Do not overuse panty liners. They promote the growth of bacteria. Wear them only immediately after your period and before your period.
- Don't use someone else's towel. You can easily get an infection in your vagina. There should be a separate towel for the genitals.
- Wear underwear made of cotton fabric. Synthetics do not allow the skin to breathe.
- Visit your gynecologist regularly.
If you notice brown secretion, do not worry, provided that it is not abundant and without clots. When thick brown mucous vaginal discharge appears in the middle of the cycle, a pathological process should be suspected.
During pregnancy, monitor your condition especially closely. Do not self-medicate or take popular medications without prescription. Use the article material for reference purposes only. The Internet will not help you accurately determine the reason for the secret being released. If you feel unwell, be sure to seek qualified help from medical institutions.
Brown vaginal discharge - what to be afraid of?
Not all brown vaginal discharge is cause for concern. Very often, this type of spot appears just before the start of menstruation. Vaginal discharge can also occur during ovulation or during the first stage of pregnancy when the embryo implants into the uterine lining.
However, sometimes brown vaginal discharge can be a sign of health problems if it is a symptom of bacterial vaginosis or pelvic inflammatory disease.
Brown spots may appear after taking birth control pills. In general, this is not a cause for concern - the body reacts to hormones in this way. However, if the problem persists for more than 2-3 days, you should seek help from a doctor, who will determine whether the vaginal discharge is a symptom of a more serious condition.
Self-medication for any type of discharge is prohibited, as you can do more harm to the body than good.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Spotting for threatened miscarriage
With an incomplete miscarriage, brown discharge also occurs, but in this case it becomes bloody and includes clots. You will also feel cramps in the lower abdomen and pain.
In the case of a frozen pregnancy, menstruation is delayed and bleeding occurs, accompanied by abdominal pain. It is enough to donate blood for hCG and do an ultrasound to confirm or refute the death of the fetus in the womb. Here are the reasons why threats of miscarriage may arise:
- there is not enough progesterone in the body;
- there are diseases of the endocrine system;
- there are problems with the pituitary gland;
- the body is exposed to stress;
- excess physical activity;
- bad habits (smoking, alcohol and drugs).
If you do not consult a doctor in time if there is a threat of miscarriage, you will lose your baby and also risk having to have a curettage.
Is dark discharge dangerous during pregnancy?
Of course, not all discharge can pose a danger to a woman’s health. It is worth noting that brown discharge during pregnancy can be either normal or indicate the presence of one or another pathology.
With pathology, brown discharge can occur when pregnancy develops outside the uterus or an unauthorized abortion occurs, that is, a miscarriage.
Also, brown discharge may indicate that a disease such as uterine fibroids has begun to manifest itself.
If during the first two to twelve days brown discharge continues to be produced by the body in small quantities, then there is no cause for concern, but the doctor must be warned about this.
Causes of brown transudate
Dark discharge can appear due to normal physiological processes and various pathological conditions. For this reason, doctors divide the factors influencing the appearance of brown transudate into 2 groups: normal and pathological.
Normal Factors
Brown discharge often appears the day before menstruation begins. They always indicate that the rejection of endometrial cells has begun in the uterus. This is the norm, but only if the spotting leucorrhoea goes away within 2 days. If this does not happen, then you should consult a gynecologist.
Discharge as a sign of a disturbance in the functioning of the body
As mentioned earlier, discharge in a woman can be a sign of disruption in the work and functioning of the entire body. Undoubtedly, this is directly related to a weakened immune system, as well as diseases such as candidiasis and gardnerella.
Initially, any woman feels discomfort, which is usually accompanied by itching or a burning sensation. Diseases such as candidiasis or gardnerella are among the diseases that occur due to a weakened immune system.
It is worth understanding that immunity is far from the last place in human health. Discharge is considered a sign of disturbances in the functioning of the body when it is released in large volumes and has a characteristic color.
Most often, in terms of color, the discharge is grayish and greenish. In addition, a characteristic feature is the presence of a sharp, characteristic and unpleasant odor. To determine the disease that has begun to develop in the body, you will need to undergo a comprehensive analysis.
Treatment methods
The treatment regimen depends on the cause of the brown secretion and accompanying symptoms. Treatment is prescribed by a specialist after receiving diagnostic results.
Treatment methods depending on the pathological process:
- in case of bacterial infection and inflammation arising from it, antibacterial drugs are prescribed orally and locally in the form of ointments, creams, suppositories;
- Fungal infections are treated with antifungal drugs. It is worth noting that thrush is a local symptom of extensive damage to the body by a fungus. Her therapy is not limited to the use of creams and suppositories. The main amount of fungus is in the intestines, so treatment includes taking antifungal drugs orally;
- therapy for viral infections includes the use of antiviral drugs, as well as immunostimulants, since increasing immunity is of great importance in the fight against viruses;
- When diagnosing neoplasms, conservative therapy or surgery is used. The choice of method depends on whether the tumor is benign or malignant, as well as its size;
- If there is a threat of miscarriage during pregnancy, treatment is carried out in a hospital setting. During the examination, the condition of the placenta, reproductive organ, and fetus is assessed;
- ectopic pregnancy requires immediate surgery to remove the fertilized egg from the fallopian tube;
- in case of hormonal imbalance during menopause, hormonal drugs are prescribed;
- endometriosis, erosion, polyps and neoplasms are eliminated using surgical treatment or laparoscopy;
- during the rehabilitation period after surgery, she carries out drug therapy in order to restore the functioning of the woman’s reproductive system.
When unhealthy discharge appears, you need to be especially careful about hygiene, as it irritates the skin of the genitals, causing itching. Under no circumstances should you self-medicate. This can lead to infertility and the development of complications that will require serious, long-term therapy. Only after receiving the diagnostic results, the doctor will determine treatment tactics, taking into account the diagnosis.
Establishing diagnosis
External signs and history are not enough to make an accurate diagnosis. Before deciding on treatment, the doctor prescribes the following types of research to the patient:
Blood and urine analysis for general indicators.- Biochemistry of blood.
- Smears from the vagina and cervical canal. They are necessary for cytological examination.
- Ultrasound of the female reproductive system.
- Studying blood for hormone content and their ratio.
- HCG analysis.
- Colposcopy.
- Hysteroscopy.
- Tests to detect sexually transmitted diseases.
If necessary, doctors of other specialties may be involved in the examination. In the future, they take part in drawing up treatment tactics.