Under normal conditions, in a healthy person, the heart contracts rhythmically. The rhythm is provided by periodically occurring excitation processes in the heart muscle itself, causing contractions of the atria and ventricles in a certain sequence and making up the above-described heart cycle.
An abnormal heart rhythm is called arrhythmia. There are many types of arrhythmias. The frequency, sequence, or strength of contractions may change. Too rare heart contractions (less than 60 per minute) are called bradycardia, and frequent ones (more than 100 per minute) are called tachycardia.
Depending on the location of the source of excitation leading to arrhythmia, supraventricular (atrial) and ventricular arrhythmias are distinguished.
It is not always possible to accurately determine the cause of the disease, because there can be many such causes. Arrhythmia can develop after a myocardial infarction, when damage to the heart muscle makes it difficult to carry out normal impulses. More than 80% of patients with acute myocardial infarction experience arrhythmias. Arrhythmia can be caused by a violation of the metabolism of mineral substances - potassium, magnesium, calcium, sodium, which play an important role in the processes of occurrence and propagation of electrical impulses in the heart. Arrhythmia can also be caused by certain medications, such as cardiac glycosides. Disturbances in the nervous regulation of heart activity can contribute to the development of arrhythmia. If the arrhythmia threatens the health (and in some cases it can threaten the life) of the patient, medications are prescribed to help reduce its manifestations.
Most existing antiarrhythmic drugs can be divided into three main groups according to the predominant mechanism of action:
Rating of drugs for arrhythmia
When selecting appropriate medications, VyborExpert relied on the recommendations of leading cardiologists, after which effective and time-tested drugs were assessed for the following characteristics:
- Form of the disease;
- Presence of concomitant disorders;
- Patient's age;
- Composition of the drug;
- Mechanism of action;
- Presence of additional risk factors;
- Release form, ease of use;
- Contraindications, risks of side effects;
- Safety, bioavailability;
- Course duration, price.
The result of the comparative analysis was a list of drugs for arrhythmia consisting of 9 nominees. For convenience, they were divided into 5 groups according to the principle of action. These are both preventive and therapeutic agents. Thanks to customer reviews, it was possible to determine the strengths and weaknesses of each.
The best membrane stabilizing drugs
A set of therapeutic measures may include membrane-stabilizing medications, the principle of action of which is aimed at blocking the excitability of the heart muscle. Elimination of this cause is appropriate for all types of disease, except for the sinus type, since medications of this type do not affect the cells of the sinus node. 2 nominees received the best reviews, as well as approval from cardiologists.
Lidocaine
The rating opens with a well-known local anesthetic that has found application in the treatment of cardiac arrhythmia. Available in the form of ampoules with a liquid solution for injection, one package contains 10 pieces. It aims to block both open and inactivated sodium channels. At the same time, there is no effect on the internal conductivity of the heart, the time of contraction and widening of the ventricular QRS complex.
The drug is also valued for its selective effect on myocardial tissue and does not affect the tone of the autonomic nervous system or blood pressure. Most often, doctors prescribe Lidocaine for ventricular cardiac arrhythmias in order to restore the membrane after an impulse, including tachycardia and extrasystole. The tablet form is not used for home treatment.
Advantages:
- Stabilizing effect on the membrane;
- Acceleration of recovery after an impulse;
- Anesthetic effect;
- No effect on pressure;
- Minimal contraindications;
- Inexpensive.
Flaws:
- For internal administration only;
- Contraindications.
Hypotension, liver pathologies, and convulsive conditions are considered contraindications. For urgent help, 4 ml of a 2% solution injected into a vein will be sufficient. Subsequently, droppers of 1 ml of 4% are placed.
Propanorm
The sodium channel blocker Propanorm demonstrates good results in the complex treatment of this disease. Its action is aimed at preventing a wave of excitation in the myocardium, thereby normalizing the heart rhythm. The product is available in two forms - a solution for internal administration by injection, tablets for oral administration.
The active substance is propafenone hydrochloride, a local anesthetic. The effect occurs 1 hour after administration, lasting another 12 hours. Most often, doctors prescribe “Propanorm” for ventricular/supraventricular extrasystoles, for the purpose of prevention. The mandatory condition for the patient is the age of majority. Due to its arrhythmogenic effect, overdose is dangerous.
Advantages:
- Anesthetic effect;
- Sodium channel blockade;
- Different forms for administration;
- Performance;
- Prevention of attacks;
- Price.
Flaws:
- Admission restrictions;
- Risks of overdose.
You must take Propanorm as prescribed by your doctor. Much depends on age and weight, for example, if you are 70 kg, 150 mg of the active ingredient three times a day will be enough. Contraindications – severe heart failure, arterial hypotension, heart attack, bradycardia.
Medicines that reduce the flow of sodium ions into heart cells.
As is known, the occurrence and propagation of an electrical impulse in cells in general and in heart cells in particular is associated with the activity of ion channels, among which a special role belongs to the sodium channel. Substances that block these channels stabilize cell membranes (they are also called membrane-stabilizing) and prevent the abnormal occurrence and propagation of electrical impulses. A malfunctioning cell becomes electrically “silent”, while the activity of normal cells does not change. However, with increasing doses, these substances suppress impulse conduction in normal tissues, provoking arrhythmia. Moreover, even a therapeutic concentration of the drug can become “arrhythmogenic” with rapid heartbeat, acidosis or hyperkalemia.
The ancestor of drugs in this group is quinidine, which is a derivative of quinine, an alkaloid from the bark of the cinchona tree. It also includes procainamide, disopyramide, lidocaine, mexiletine, moricizine, propafenone and others. They all have the same mechanism of action, similar to the action of local anesthetics that block sodium channels inside the cell.
The best beta blockers for arrhythmia
Thanks to such means, it is possible to reduce the need of the heart muscle for oxygen supply, as well as stop the functions of catecholamines. Cardiologists prescribe this group of medications to patients with sinus-type disease or caused by insufficient blood microcirculation. The list of beta blocker drugs for cardiac arrhythmia included 2 leaders according to reviews and assessments by cardiologists.
Metoprolol
The first in this category is a drug for normalizing cardiac activity. In terms of composition, it is a beta1-blocker with a wide spectrum of effects, but of a selective type. Another difference from analogues is the prolonged effect. The active substance is metoprolol succinate, which has antiarrhythmic, antihypertensive, and antianginal effects.
That is, proper use of tablets reduces blood pressure, prevents it from jumping, and prevents heart rhythm disturbances and angina attacks. The therapy also helps slow the pulse, muscle contractility, reduce the volume of ejected blood and myocardial excitability. The effect develops gradually, reaching a maximum after 2 weeks of the course.
Advantages:
- Large list of indications;
- Selective action;
- Possibility of use for prophylactic purposes;
- Bioavailability;
- Prolonged effect;
- Decreased heart rate and blood pressure.
Flaws:
- Withdrawal syndrome;
- Risks of side effects.
The standard treatment regimen is 100 mg in one or two doses per day, gradually increasing the dose to 200-400 mg. The product is not recommended for low blood pressure, heart failure, impaired peripheral blood supply, or lactation.
Anaprilin
Tablets for arrhythmia of non-selective action, designed to normalize heart rhythm by influencing blood pressure, the sympathetic nervous system, and pulse. The active substance is propranolol hydrochloride, which reduces the frequency of muscle contractions and blood pressure. The list of indications also includes tachycardia, angina pectoris, extrasystole, and hypertension.
The tablet form can be of 3 types depending on the concentration of the active substance - 10, 50, 100 mg. Medical practice shows that the correct use of Anaprilin has a beneficial effect on the myocardium, eliminates dizziness, shortness of breath, and discomfort in the chest area. Improvement occurs within 30 minutes, even faster if administered by injection.
Advantages:
- Calm, lower blood pressure;
- Quick relief;
- Help with VSD, panic attacks;
- “First aid” for rhythm disturbances;
- Availability;
- Inexpensive.
Flaws:
- Lots of side effects;
- Specific taste.
Treatment in this way is unacceptable for acidosis, acute infarction, peripheral circulatory disorders, bronchospasms, and sinus bradycardia. Otherwise, start with 20 mg three times a day with a gradual increase in dose. For better digestibility, this should be done half an hour before meals.
The best calcium and potassium channel blockers for arrhythmia
When potassium and sodium leave the myocardial cells, they become excited. Therefore, doctors can prescribe special medications to prevent this. Calcium channel blockers will also help, as they slow down the formation of signals in the sinus node, the speed of their movement through the myocardium, and also contribute to partial inhibition of atrioventricular conduction.
Amiodarone
List of modern iodine-based anti-arid drugs for widespread use in hospital settings. The drug promotes vasodilation, which has a beneficial effect on heart rate. It also prevents the excretion of intracellular potassium, thereby slowing down repolarization. The tablet form assumes a dosage of 200 mg of the active ingredient, 30 or 60 pieces per package.
Indications for use: ventricular flutter, tachycardia. Unlike many analogues, this remedy is highly effective for supraventricular and ventricular cardiac arrhythmias. A long elimination period ensures that tablets are taken infrequently. In addition, Amiodarone is approved for people with heart failure, since it does not affect ventricular function.
Advantages:
- High arrhythmolytic efficiency;
- Elimination of ventricular fibrillation;
- Moderate a-blocking, antioxidant;
- Long removal process;
- Children allowed;
- No effect on ventricular function.
Flaws:
- Risks of arrhythmogenic effect;
- Possibility of extracardiac side effects.
A common prescription regimen is 600 mg per day for a week, usually divided into 3 doses. After this, the dosage is gradually reduced until normal health is restored. For children, 200 mg per day is sufficient. Tablets are prohibited for pathologies of the thyroid gland, respiratory system, pregnancy, and lactation.
Cordaron
The leader among drugs for atrial fibrillation, which has a positive effect on energy metabolism in the myocardium. It is based on the substance amiodarone hydrochloride, which blocks the electrical signals that cause irregular heartbeats. In addition, the composition will partially block potassium, calcium, and sodium channels. The product is presented in tablet form, as well as liquid for injection.
Uniqueness - a combination of calcium/sodium/potassium blocker properties with a beta-adrenergic blocking effect. Regular use reduces the sensitivity of the heart to stress hormones and the effect of thyroid hormones on the myocardium. Cordarone is highly valued because it is approved for chronic heart failure. The therapeutic properties develop gradually and last up to 3-6 months.
Advantages:
- Prevention of angina attacks;
- Pulse equalization;
- Multifunctionality;
- Protection from the negative effects of hormones;
- Allowed for heart failure;
- Long-lasting cumulative effect.
Flaws:
- List of contraindications, risks;
- Price.
The initial dose is 800 mg, divided into several doses. Then, as they feel better, they are reduced to 400 mg by the second week. And after that, to maintain the results obtained, 200 mg will be enough. Cordarone is definitely not allowed for people under 18 years of age or for pregnant or breastfeeding women.
Antiarrhythmic drugs
The main method of treating arrhythmias is the use of antiarrhythmic drugs (AAP). Although they do not “cure” arrhythmias, they can reduce or suppress arrhythmic activity and prevent recurrence of arrhythmias.
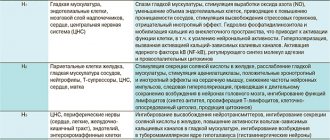
AAP classification. The most widely known classification of AAP, proposed by EM Vaughan Williams (1969; 1984) and supplemented by D. Harrison (1979):
Class I - sodium channel blockers;
Class II - β-adrenergic receptor blockers;
Class III - drugs that increase the duration of the action potential and myocardial refractoriness (potassium channel blockers);
Class IV - calcium channel blockers.
The vast majority of AAPs belong to class I. According to the proposal of D. Harrison (1979), class I drugs were further divided into three subclasses: IA, IB and IC (Table 1).
All class I drugs slow down the rate of depolarization and conduction velocity in the myocardium of the atria and ventricles. This effect is most clearly expressed in class IC AAP. Class IB drugs have a minimal effect on the rate of depolarization, and class IA AAPs occupy an intermediate position. At the same time, class IA AAPs slow down repolarization - they increase the duration of the action potential and the effective refractory period, class IB drugs can slightly accelerate repolarization, and class IC AAPs have almost no effect on the process of myocardial repolarization (although they lengthen the effective refractory period of the atria at a high frequency of atrial contractions, for example, with atrial fibrillation). Thus, the action of class I drugs is distinguished by speed:
IA - moderate slowing of the rate of depolarization and repolarization;
IB - minimal deceleration of depolarization rate and acceleration of repolarization;
IC—maximum deceleration of depolarization rate and minimal effect on repolarization.
On the electrocardiogram (ECG), a slowing of the rate of depolarization is manifested as widening of the P wave and the QRS complex. Slowing of ventricular repolarization on the ECG manifests itself as a prolongation of the QT interval.
The classification of AARP by EM Vaughan Williams, even in its modern modification, has significant drawbacks. The effect of AAP in the whole organism is often noticeably different from the effect on myocardial cells identified experimentally: various pathological conditions significantly change the electrophysiological properties of the myocardium and the nature of the effect of AAP; many drugs exhibit the properties of several or even all classes at the same time. Therefore, repeated attempts have been made to supplement and revise the classification of AAP, to create new classifications based on theoretical developments, data from experimental and clinical studies, and practical experience in the treatment of arrhythmias.
One of the attempts to create a more advanced AAP classification is the so-called “Sicilian Gambit”. Leading experts on arrhythmias gathered in Sicily and made an attempt to bring together data from theoretical, experimental and clinical studies, the entire range of knowledge about the mechanisms of arrhythmias and the action of AAP. They called their report “The Sicilian Gambit” (Sicily, 1990), by analogy with the “Queen's Gambit” in chess, the use of which provides the chess player with “a wide choice of aggressive actions.” It was truly a brainstorming session on the problem of treating arrhythmias. This report is an excellent systematic review of modern ideas about the electrophysiology of the heart, the mechanisms of arrhythmias and the action of AAP.
“The Sicilian Gambit” summarizes and systematizes all the information collected to date on the action of AAP (including at the cellular and subcellular levels). Each AAP has its own place - taking into account all the features of its action.
However, the “Sicilian Gambit” has no practical significance, since the authors of the “Sicilian Gambit” only systematized the terms and definitions in already known treatment schemes. When attempting to use the provisions of the “Sicilian Gambit” in practical work, an illusion of certainty is created where there is none. The new approach is aimed at increasing the effectiveness of further scientific research on the problem of cardiac arrhythmias and may contribute to the understanding of various aspects of the problem of drug treatment of arrhythmias, as well as facilitate the teaching of materials on arrhythmias to students or doctors who want to become arrhythmologists. The famous arrhythmologist RN Fogoros (1997) defined the role of the Sicilian Gambit as follows: “It cannot be said that the Sicilian Gambit is unsuitable for practice. Once the mechanisms of arrhythmias are more clearly defined, knowledge of the specific properties of certain drugs can help predict the effectiveness of pharmacological therapy (which is the goal of the authors of the Sicilian Gambit). Moreover, such a tabular system is certainly useful for research... The Vaughan Williams system (with all its limitations) is still the most useful means of classifying antiarrhythmic drugs."
Undesirable effects of AAP. Any action of AAP can cause both antiarrhythmic and arrhythmogenic effects. The probability of an antiarrhythmic effect for most drugs averages 40–60%. The exception is amiodarone, whose effectiveness reaches 70–80%, even in the absence of effect from other AAPs. The probability of an arrhythmogenic effect is on average about 10%, and for class IC drugs it reaches 20% or more. In this case, the arrhythmogenic effect can manifest itself in the form of life-threatening arrhythmias. In severe ventricular arrhythmias in patients with severe organic heart disease, the likelihood of an arrhythmogenic effect may exceed the likelihood of an antiarrhythmic effect.
Several large clinical studies have revealed a significant increase in overall mortality and the incidence of sudden death (2-3 times or more) in patients with organic heart disease (post-infarction cardiosclerosis, cardiac hypertrophy or dilatation) while taking class I AAP, despite effective elimination arrhythmias. The most famous work, which for the first time revealed a complete discrepancy between the clinical effectiveness of drugs and their effect on prognosis, is the Cardiac Arrhythmia Suppression Trial (CAST). The effect of three AAPs was studied: flecainide, encainide and moricizine (ethmosine). At the interim analysis, a sharp increase in overall mortality and the incidence of sudden death (2.5 and 3.6 times, respectively) was found among patients taking flecainide and encainide, despite the effective elimination of ventricular premature beats. Subsequently, an increase in mortality was also detected when taking moricizine (CAST-II). The results of the CAST study forced us to reconsider treatment tactics not only for patients with cardiac arrhythmias, but also for cardiac patients in general. The CAST study played perhaps the main role in the development of evidence-based medicine.
The only AAPs associated with a reduction in mortality are β-blockers and amiodarone. Therefore, beta-blockers and amiodarone are currently the drugs of choice for the treatment of arrhythmias in patients with organic heart disease.
All AAPs have unwanted side effects. As a rule, their frequency and severity depend on the dose of the drug. A detailed list of side effects of AAP takes up several dozen pages. A list of side effects of each AAP is given in the annotations for the drugs.
The high frequency of arrhythmogenic effects and side effects of AAP allows us to propose the following as one of the basic principles for the treatment of arrhythmias: “Avoid the use of antiarrhythmic drugs whenever possible” (RF Fogoros, 1997).
AAPs used for intravenous administration and recommended daily doses are shown in Table 2, for oral administration - in Table 3.
Brief characteristics of the AAP. Of the class I AAPs, four drugs are mainly used in Russia: quinidine (kinidin durules), allapinin, etatsizin and propafenone (ritmonorm, propanorm). These drugs have approximately the same effectiveness and tolerability. In addition to these class I drugs, intravenous administration of novocainamide and lidocaine is used in emergency situations.
After the CAST study and the publication of the results of a meta-analysis of studies on the use of class I AAPs, which showed that almost all class I AAPs are able to increase mortality in patients with organic heart disease, β-blockers have become the most popular AAPs.
The antiarrhythmic effect of beta-blockers is due precisely to the blockade of beta-adrenergic receptors, i.e., a decrease in sympathetic-adrenal effects on the heart. Therefore, β-blockers are most effective for arrhythmias associated with sympathetic-adrenal influences - the so-called catecholamine-dependent, or adrenergic, arrhythmias. Their occurrence is usually associated with physical activity or psycho-emotional stress.
β-blockers are the drugs of choice for the treatment of arrhythmias in congenital long QT syndromes.
For arrhythmias not associated with activation of the sympathetic nervous system, β-blockers are much less effective, but their addition to the treatment regimen often significantly increases the effectiveness of other AAPs and reduces the risk of the arrhythmogenic effect of class I AAPs. Class I drugs in combination with β-blockers do not increase mortality in patients with organic heart disease (CAST study).
Doses of β-blockers are adjusted according to their antiarrhythmic effect. An additional criterion for sufficient β-blockade is a decrease in heart rate (HR) to 50/min.
The original drug is amiodarone. It has the properties of all four classes of AAP and, in addition, has a moderate α-blocking and antioxidant effect. Amiodarone is undoubtedly the most effective AAP available. It is even called an “arrhythmolytic drug.” However, the attitude of cardiologists towards amiodarone from the very beginning of its use for the treatment of arrhythmias caused the greatest disagreement. Due to the high incidence of extracardiac side effects, amiodarone was considered a reserve drug for quite a long time: it was recommended to use it only for life-threatening arrhythmias and only in the absence of effect from all other AAPs (LN Horowitz, J. Morganroth, 1978; JW Mason, 1987; JC Somberg , 1987).
However, after conducting CAST and other studies, it became clear that amiodarone is not only the most effective, but also the safest (after β-blockers) AAP. Numerous large controlled studies of the effectiveness and safety of amiodarone not only did not reveal an increase in mortality, but, on the contrary, a decrease in overall mortality and the incidence of arrhythmic and sudden death was observed. The incidence of torsade de pointes (TdP) while taking amiodarone is much lower than with other AAPs that prolong the QT interval and is less than 1%. As a result, amiodarone moved from reserve drugs to first-choice drugs for the treatment of arrhythmias.
The main disadvantage of the drug is the high incidence of extracardiac side effects with long-term use (JA Johus et al., 1984; JF Best et al., 1986; WM Smith et al., 1986). The main side effects of amiodarone include: photosensitivity, skin discoloration, thyroid dysfunction (both hypothyroidism and hyperthyroidism), increased transaminase activity, peripheral neuropathies, muscle weakness, tremor, ataxia, visual impairment. Most of these side effects are reversible and disappear after discontinuation or reduction of the dose of amiodarone. Hypothyroidism can be controlled by taking levothyroxine. The most dangerous side effect of amiodarone is damage to the lungs (“amiodarone lung disease”). According to various authors, its frequency ranges from 1 to 17%, and mortality in the case of pulmonary fibrosis develops from 10 to 20% (JJ Heger et al., 1981; B. Clarke et al., 1985, 1986). However, in most cases, lung damage develops only with long-term use of relatively large maintenance doses of amiodarone - more than 400 mg/day (up to 600 or even 1200 mg/day). Such doses are practically not used at present. The maintenance dose of the drug in Russia is usually 200 mg/day or even less (200 mg 5 days a week). Currently, the incidence of “amiodarone-induced lung injury” is no more than 1% per year (SJ Connolly, 1999; MD Siddoway, 2003).
Amiodarone has unique pharmacokinetic properties. For the antiarrhythmic effect to occur from taking the drug, a period of “saturation”—“cordaronization”—is required.
In Russia, the most common dosage regimen for amiodarone is 600 mg/day (3 tablets per day) for 1 week, then 400 mg/day (2 tablets per day) for another 1 week, a maintenance dose of 200 for a long time. mg per day (1 tablet per day) or less. The antiarrhythmic effect occurs more quickly when high loading doses of amiodarone are prescribed during “saturation”, for example, 1200 mg/day or more for 1 week, then a gradual dose reduction to 200 mg per day (titration according to the effect to the minimum effective doses). There are reports of the effective use of very high doses of amiodarone - 800-2000 mg 3 times a day (i.e. up to 6000 mg / day - up to 30 tablets per day!) in patients with severe life-threatening diseases refractory to other treatment methods ventricular arrhythmias with repeated episodes of ventricular fibrillation (ND Mostow et al., 1984; SJL Evans et al., 1992). A single dose of amiodarone at a dose of 30 mg/kg body weight is officially recommended as one of the ways to restore sinus rhythm in atrial fibrillation.
After achieving the antiarrhythmic effect, the dose is gradually reduced to the minimum effective. Effective maintenance doses of amiodarone can be 100 mg/day and even 50 mg/day (M. Dayer, S. Hardman, 2002).
The effect and effectiveness of intravenous amiodarone has been less studied compared to oral administration. When administered intravenously as a bolus, the drug is usually administered at a dose of 5 mg/kg body weight over 5 minutes. One of the most popular intravenous amiodarone regimens is a bolus of 150 mg over 10 minutes, then an infusion at a rate of 1 mg/min for 6 hours (360 mg over 6 hours), then an infusion at a rate of 0.5 mg/min.
Published data suggest that intravenous amiodarone is more effective for ventricular tachyarrhythmias than lidocaine, bretylium tosylate, and procainamide. The use of amiodarone is effective for all types of supraventricular and ventricular arrhythmias. Even with arrhythmias refractory to all other AAPs, the effectiveness of the drug reaches 60–80%, both when administered intravenously and when taken orally.
When using sotalol (Sotalex), the average daily dose is 240–320 mg. Start with 80 mg 2 times a day. While taking sotalol, there is an increased risk of developing ventricular tachycardia of the “pirouette” type. Therefore, it is advisable to start taking this drug in a hospital. When prescribing it, it is necessary to carefully monitor the QT interval, especially in the first 3 days. The corrected QT interval should not exceed 0.5 s.
The new class III AAPs include the so-called “pure” class III AAPs - dofetilide, ibutilide and the domestic drug nibentan. These drugs are used primarily to treat atrial fibrillation. They prolong the QT interval and their use is accompanied by an increased risk of torsade de pointes (TdP).
Dofetilide is prescribed orally 0.5 g 2 times a day. The incidence of tachycardia of the “pirouette” type is about 3%, mainly in the first 3 days of taking the drug. Dofetilide is discontinued if the corrected QT interval prolongs by more than 0.5 seconds. Ibutilide is prescribed intravenously to restore sinus rhythm in atrial fibrillation. Ibutilide is administered intravenously as a bolus of 1 mg over 10 minutes. If there is no effect, the drug is re-administered. The effectiveness of ibutilide in stopping atrial fibrillation and flutter is about 45%. The incidence of tachycardia of the “pirouette” type reaches 8.3%.
Nibentan, ampoules of 20 mg (2 ml of 1% solution), a domestic drug, most effective for atrial fibrillation. According to published data, nibentan is far superior to all available foreign analogues. Its effectiveness in restoring sinus rhythm even with a permanent form of atrial fibrillation reaches 100%. The drug is administered intravenously at a dose of 0.125 mg/kg (i.e., approximately 1 ml - 10 mg) over 3 minutes (in 20 ml of isotonic sodium chloride solution). In recent years, data have been obtained that administration of a 2 times smaller dose (0.0625 mg/kg - approximately 0.5 ml - 5 mg), as a rule, is no less effective. If there is no effect, nibentan is reintroduced after 15 minutes at the same dose. Side effects (the appearance of a sour or “metallic” taste in the mouth, a feeling of “hot” or “cold”, double vision, slight dizziness, sore throat) and the arrhythmogenic effect of nibentan (ventricular extrasystoles and ventricular tachycardia of the “pirouette” type) are observed relatively rarely - in about 1% of cases.
The main indication for the use of verapamil and diltiazem is the relief of paroxysmal reciprocal atrioventricular nodal tachycardias. The effectiveness of verapamil and diltiazem in stopping paroxysmal supraventricular tachycardia is 80–100%. The second indication for the use of verapamil and diltiazem is a decrease in heart rate in the tachysystolic form of atrial fibrillation. It should be noted that intravenous administration of verapamil is contraindicated for atrial fibrillation in patients with Wolff–Parkinson–White syndrome, since in some patients after the administration of verapamil there is a sharp increase in the frequency of ventricular contractions up to 300 per minute or more. There is a variant of ventricular tachycardia in which verapamil acts as the drug of choice and often the only effective drug. This is the so-called verapamil-sensitive ventricular tachycardia - idiopathic ventricular tachycardia, in which the QRS complexes have the form of right bundle branch block with deviation of the electrical axis to the left.
Principles for choosing AARP. As in the treatment of other diseases, the choice of AAP is made primarily on the basis of data on effectiveness, safety, side effects and contraindications to its use. If there are indications for the treatment of one or another type of rhythm disturbance, choose the drug that is most appropriate for the patient. In the future, if necessary, all available AAPs are sequentially evaluated until the first effective drug is discovered, or the most suitable drug is selected from several effective ones. If there is no effect from monotherapy, a combination of AAPs is selected or non-drug methods of treating arrhythmias are used.
In patients with arrhythmias, but without signs of organic heart disease, the prescription of any AAP is considered acceptable.
In patients with organic heart disease (post-infarction cardiosclerosis, ventricular hypertrophy and/or cardiac dilation), β-blockers and amiodarone are the first choice drugs. Taking into account the safety of AAP, it is advisable to begin assessing the effectiveness with β-blockers or amiodarone. If monotherapy is ineffective, the effect of a combination of amiodarone and β-blockers is assessed. If there is no bradycardia or prolongation of the PR interval, any β-blocker can be combined with amiodarone. In patients with bradycardia, pindolol (Wisken) is added to amiodarone. Coadministration of amiodarone and β-blockers has been shown to significantly reduce mortality among patients with cardiovascular disease than either drug alone. Only if there is no effect from β-blockers and/or amiodarone, class I AAPs are used. In this case, class I drugs are usually prescribed against the background of therapy with a beta-blocker or amiodarone.
An approximate sequence for selecting effective drug therapy in patients with recurrent arrhythmias:
- β-blocker or amiodarone.
- β-blocker + amiodarone.
- Sotalol.
- AAP class I.
- Amiodarone + class IC AAP.
- β-blocker + any class I drug.
- Amiodarone + β-blocker + Class IC AAP.
- Sotalol + AAP IC class.
P. Kh. Dzhanashiya , Doctor of Medical Sciences, Professor N. M. Shevchenko , Doctor of Medical Sciences, Professor S. V. Shlyk , Doctor of Medical Sciences, Professor E. O. Khamitsaeva, Candidate of Medical Sciences Russian State Medical University, Moscow
The best anticoagulant for arrhythmia
To facilitate blood circulation through the vessels and through the heart, anticoagulants are used. They thin the blood and prevent the formation of blood clots. It is especially important to take such drugs for atrial fibrillation. In this case, tablet forms are used to complete the course. One nominee, approved by leading cardiologists, is recognized as the leader of this category.
Aspirin
An antiplatelet drug with clinically proven efficacy and safety. The mechanism of action is inhibition of platelet cyclooxygenase-1, due to which platelets are released and the blood thins. Patients with arrhythmia are prescribed this drug for the purpose of primary prevention of stroke; these are persons no older than 65 years. The antiplatelet effect also prevents heart attack.
Acetylsalicylic acid is well absorbed from the gastrointestinal tract, making it active within 1-2 hours and throughout the day. The tablet form is available in different dosages - 50-150 mg. Despite the safety of the composition, it is important to consult a doctor due to its ulcerogenic effect, which can cause ulcers, bleeding, and erosion of the gastric mucosa. Aspirin is allowed from 15 years of age.
Advantages:
- Blood thinning;
- Antipyretic, analgesic effect;
- Prevention of blood clots, heart attack, stroke;
- Anti-inflammatory effect;
- No negative effect on blood pressure;
- Inexpensive.
Flaws:
- Risks of bleeding, ulcers, erosions;
- Contraindications.
The daily dose recommended by doctors is from 40 to 1000 mg, divided into several doses (from 2 to 6 times). If the patient has diabetes mellitus, thyrotoxicosis, ischemia, as well as over the age of 65-75 years, Aspirin is contraindicated.
Other antiarrhythmic drugs for arrhythmia
Cardiovascular pathologies are one of the most common problems of humanity, so pharmaceutical companies and medical specialists are constantly creating new drugs. We conducted a study of new products presented by pharmacy chains. The review included the 2 best drugs for cardiac arrhythmia of the latest generation.
Coraxan
Antianginal, anti-ischemic drug in tablet form for oral administration, which is based on the new agent ivabradine. It effectively prevents increased heart rate. At the same time, there is no negative effect on contractility, intracardiac conduction, or ventricular repolarization processes, which reduces the likelihood of side effects.
The uniqueness of this substance lies in the dose-dependence of the reduction in heart rate. The plateau effect (no increase in therapeutic effect) prevents the risk of developing bradycardia. Coraxan is approved even for people with diabetes, since the active ingredient, which relieves anxiety symptoms, does not affect the metabolism of lipids and glucose.
Advantages:
- Fast safe absorption;
- Normalization of pulse;
- Lack of influence on other processes of the heart and blood vessels;
- Elimination of symptoms of angina pectoris, tachycardia;
- No withdrawal syndrome;
- Allowed for diabetics.
Flaws:
- Contraindications based on age, health status;
- Price.
The daily dosage is selected by the doctor individually for each patient; it is divided into 2 doses. Usually start with 5 mg, gradually increasing after 3-4 weeks. Contraindications – pregnancy, age under 18 years, bradycardia, acute heart attack, unstable angina, etc.
Panangin
This nominee belongs to the group of electrolytes that replenish the lack of important microelements for the full functioning of the cardiovascular system. The vitamin composition includes 2 components - magnesium and potassium salts. In this regard, “Panangin” acts as an auxiliary means of complex treatment. By improving metabolic processes, it provides an antiarrhythmic effect.
The nominee is especially useful for rhythm disturbances associated with electrolyte imbalance. Despite the safety of the components, irrational use can cause problems with the respiratory system. Parallel use with other medications against such pathologies enhances their effectiveness and improves nervous regulation.
Advantages:
- Vitamin composition;
- Safety;
- Increasing the effectiveness of antiarrhythmics;
- Beneficial effect on nervous regulation;
- Ease of use;
- Price.
Flaws:
- Risks of respiratory depression;
- Only an aid.
For better absorption, the tablets should be taken with meals, the optimal regimen is 2 tablets per day for a month. After this, be sure to take a break so as not to provoke an overdose. "Panangin" is prohibited in case of acid metabolism disorders, kidney or liver failure.
Classification of drugs
There are several classifications of antiarrhythmic drugs. The most famous is the Vaughan-Williams classification (1971), according to which there are 4 classes of antiarrhythmics.
I class.
Substances that block fast sodium channels. Drugs in this group help reduce the rate of depolarization and slow down conduction along Purkinje fibers and the His bundle. Among the many modern antiarrhythmic drugs in this group, propafenone deserves special attention. Propafenone causes a dose-dependent decrease in the rate of depolarization, inhibits phase 0 of the action potential and its amplitude in Purkinje fibers, which leads to an extension of the effective refractory period in the atria, atrioventricular node, accessory bundles, and, to a lesser extent, in the ventricles
II class.
Beta-blockers - reduce the impact of sympathetic (adrenergic) impulses on the heart muscle, which can play a role in the development of arrhythmia. Most of the drugs in this group help to slow the heart rate and reduce sinoatrial and atrioventricular conduction.
III class.
Drugs that slow down repolarization. These include sotalol and amiodarone. Antiarrhythmics of this group help to increase the duration of the action potential (AP) of cardiomyocytes and slow down the conduction of impulses in all areas of the conduction system of the heart.
IV class.
Group IV includes calcium ion antagonists, which block “slow” calcium channels. They help inhibit the slow flow of calcium ions into myocardial cells, which reduces the automaticity of ectopic foci of excitation in the heart.
How to choose a drug for arrhythmia
It is impossible to choose medications for the treatment of abnormal heart rhythms on your own. To avoid harm to your health, consult your doctor. What to buy at the pharmacy largely depends on the form of arrhythmia determined by the cardiologist and concomitant pathologies. There are also a number of other factors in individual development of a treatment regimen.
The doctor's consultation
The list of medications and the regimen for taking them is prescribed only by a specialist, a cardiologist. We are talking about a whole group of antiarrhythmic drugs, which are selected only after diagnosis. If you do not solve the problem comprehensively, there is a high probability of relapses and complications. Self-medication, incorrect choice of dosages, all this threatens with serious side effects.
Form of arrhythmia
The choice of medications depends on what form of heart rhythm disturbance the doctor has diagnosed. The generally accepted classification considers nootropic, heterotropic form, atrioventricular block, changes/disturbances in excitability, conductivity or excitatory function. The type of pathology depends on the reasons that provoke it. Each case is individual, as is the treatment plan.
Presence of other diseases
Since we are talking about a disease of the cardiovascular system, there is a high probability of developing associated disorders. Medical practice considers sinus bradycardia or tachycardia, atrial fibrillation or flutter, reciprocal AV nodal or ventricular tachycardia, atrial/ventricular extrasystole. Depending on this, auxiliary means are selected.
Other selection factors
There are a number of minor factors that determine which agents are appropriate in treatment. The first is the severity of the pathology. The specialist also takes into account the patient’s age, for example, drugs for arrhythmia for older people should not affect blood pressure. Take into account the contraindications in the instructions so as not to encounter side effects.
Which drug for arrhythmia is better?
As part of drug therapy, the doctor selects primary and auxiliary drugs. The most popular groups are considered in our rating. The assessment criteria and recommendations of Vyborexperta.ru will simplify the choice of how to treat such a pathology:
- Propanorm is a sodium channel blocker with local anesthetic action for the prevention of attacks;
- Metoprolol is a selective beta1-blocker with good bioavailability and prolonged effect;
- Cordarone – 2 in 1 remedy against atrial fibrillation, calcium/sodium/potassium blocker + beta-adrenergic blocking agent;
- Aspirin is the best prevention of blood clots, stroke, heart attack, anti-inflammatory, antipyretic properties;
- Panangin is an electrolyte with an antiarrhythmic effect, a source of magnesium and potassium, prevention for the elderly.
Two patients with a similar clinical picture may benefit from different treatment regimens. Therefore, self-medication, which increases the risk of worsening the situation to a critical condition, is strictly prohibited. Our rating is designed to help narrow your search for reliable, proven drug names.
Mechanism of action
The mechanisms of action of antiarrhythmic drugs have not yet been clarified. However, many drugs have similar effects. Antiarrhythmic drugs change the flow of sodium, potassium and calcium ions across the cardiomyocyte membrane, resulting in a change in its electrical potential. The main electrophysiological effect is a change in the speed and duration of AP phases, the speed of electrical impulse conduction, refractoriness and automaticity of the heart muscle.