Compound
The injection solution contains sodium heparin at a concentration of 5 thousand units/ml.
The auxiliary components of the drug include sodium chloride, benzyl alcohol, and water. 1 gram of gel contains 1 thousand units of sodium heparin , as well as auxiliary components: 96% ethanol, carbomer , dimethyl sulfoxide, propylene glycol, dietanolamine, methyl and propylparaben (additives E 218, E 216), lavender oil and purified water.
pharmachologic effect
Pharmacological group: anticoagulants .
Group of the drug Heparin, produced in the form of a gel: drugs for the treatment of cardiovascular diseases.
Group of the drug Heparin, produced in injection form: agents affecting blood and hematopoiesis.
Heparin sodium contained in the drug has an antithrombotic effect , slows down the aggregation and adhesion of leukocytes , platelets and erythrocytes ; reduces wall spasm and the degree of vascular permeability; helps improve collateral circulation.
Read also[edit | edit code]
- Treatment of thrombosis
- Hirudin
- Fibrinolytics
- Thrombosis
- Antiplatelet agents
- Plasma substitutes
- Hemostasis
- Drugs that affect blood clotting
- Hemostatics (coagulants, fibrinolysis inhibitors)
- Agents that reduce vascular permeability
- Anticoagulant blood system
- Direct anticoagulants
- Indirect anticoagulants
- Agents affecting fibrinolysis
- Agents affecting platelet aggregation
Pharmacodynamics and pharmacokinetics
What is Heparin?
Heparin (INN: Heparin) is an acidic mucopolysaccharide with Mr about 16 kDa. A direct anticoagulant that helps slow down the formation of fibrin .
The gross formula of heparin is C12H19NO20S3.
Pharmacodynamics
The mechanism of action of heparin is based primarily on its binding to AT III (its plasma cofactor). Being a physiological anticoagulant , it potentiates the ability of AT III to suppress activated coagulation factors (in particular, IXa, Xa, XIa, XIIa).
When used in high concentrations, heparin also inhibits thrombin activity .
Suppresses activated factor X, which is involved in the internal and external blood coagulation system.
The effect occurs when significantly lower doses of heparin are used than are required to inhibit the activity of coagulation factor II ( thrombin ), which promotes the formation of fibrin from the plasma protein fibrinogen .
This justifies the possibility of using small doses of heparin (subcutaneously) for prophylactic purposes, and large doses for treatment.
Heparin is not a fibrinolytic (i.e., it is capable of dissolving blood clots), but it can reduce the size of the blood clot and stop its expansion. Thus, the blood clot is partially dissolved under the action of fibrinolytic enzymes of natural origin.
Suppresses the activity of the enzyme hyaluronidase, helps reduce the activity of surfactant in the lungs.
Reduces the risk of developing MI, acute thrombosis of myocardial arteries and sudden death. In small doses it is effective for the prevention of VTE, in high doses it is effective against venous thrombosis and pulmonary embolism .
Deficiency of AT III at the site of thrombosis or plasma may reduce the antithrombotic effect of the drug
When applied externally, the product has a local antiexudative , antithrombotic and moderate anti-inflammatory effect .
Promotes the activation of fibrinolytic properties of blood, inhibits the activity of hyaluronidase, and blocks the formation of thrombin. Gradually released from the gel and passing through the skin, heparin helps reduce inflammation and has an antithrombotic effect .
At the same time, the patient’s microcirculation improves and tissue metabolism is activated and, as a result, the processes of resorption of blood clots and hematomas are accelerated, and tissue swelling is reduced.
Pharmacokinetics
When used externally, absorption is negligible.
After injection under the skin, TCmax is 4-5 hours. Up to 95% of the substance is in a state bound to plasma proteins, Vp - 0.06 l/kg (the substance does not leave the vascular bed due to strong binding to plasma proteins).
It does not penetrate the placental barrier or into breast milk.
Metabolized in the liver. The substance is characterized by rapid biological inactivation and short duration of action, which is explained by the participation of the antiheparin factor in its biotransformation and the binding of heparin to the macrophage system.
T1/2 - 30-60 minutes. Excreted by the kidneys. Up to 50% of the substance can be excreted unchanged only if high doses are used. It is not excreted by hemodialysis.
Publications in the media
Pharmgruppa is a direct-acting anticoagulant agent. Characteristic. Polysaccharide with mol. weighing about 16 thousand Da, obtained from the lungs of cattle or the mucous membrane of the small intestine of pigs.
Pharmaceutical action. Direct anticoagulant, belongs to the group of medium molecular heparins, slows down the formation of fibrin. The anticoagulant effect is detected in vitro and in vivo and occurs immediately after intravenous administration. The mechanism of action of heparin is based primarily on its binding to antithrombin III, an inhibitor of activated blood coagulation factors: thrombin, IXa, Xa, XIa, XIIa (the ability to inhibit thrombin and activated factor X is especially important). Increases renal blood flow; increases cerebral vascular resistance, reduces the activity of cerebral hyaluronidase, activates lipoprotein lipase and has a hypolipidemic effect. Reduces the activity of surfactant in the lungs, suppresses excessive synthesis of aldosterone in the adrenal cortex, binds adrenaline, modulates the ovarian response to hormonal stimuli, and increases the activity of parathyroid hormone. As a result of interaction with enzymes, it can increase the activity of brain tyrosine hydroxylase, pepsinogen, DNA polymerase and reduce the activity of myosin ATPase, pyruvate kinase, RNA polymerase, pepsin. In patients with coronary artery disease (in combination with ASA), it reduces the risk of acute coronary artery thrombosis, myocardial infarction and sudden death. Reduces the frequency of recurrent infarctions and mortality in patients who have had myocardial infarction. In high doses it is effective for pulmonary embolism and venous thrombosis, in small doses it is effective for the prevention of venous thromboembolism, incl. after surgical operations. With intravenous administration, blood coagulation slows down almost immediately, with intramuscular injection - after 15-30 minutes, with subcutaneous administration - after 20-60 minutes, after inhalation the maximum effect is within 24 hours; the duration of the anticoagulation effect is respectively 4-5, 6, 8 hours and 1-2 weeks, the therapeutic effect - prevention of thrombus formation - lasts much longer. Deficiency of antithrombin III in plasma or at the site of thrombosis may reduce the antithrombotic effect of heparin.
Pharmacokinetics. After subcutaneous administration, TCmax is 4-5 hours. Bonding with plasma proteins is up to 95%, the volume of distribution is very small - 0.06 l/kg (does not leave the vascular bed due to strong binding to plasma proteins). Does not penetrate the placenta or into breast milk. It is intensively captured by endothelial cells and cells of the mononuclear-macrophage system (RES cells), concentrated in the liver and spleen. When administered by inhalation, it is absorbed by alveolar macrophages, capillary endothelium, large blood and lymphatic vessels: these cells are the main site of heparin deposition, from which it is gradually released, maintaining the required concentration in the plasma. Metabolized in the liver with the participation of N-desulfamidase and platelet heparinase, which is involved in the metabolism of heparin at later stages. Participation in the metabolism of platelet factor IV (antiheparin factor), as well as the binding of heparin to the macrophage system explains the rapid biological inactivation and short duration of action. Desulfated molecules are converted into low molecular weight fragments by the action of kidney endoglycosidase. T1/2 - 1-6 hours (average - 1.5 hours); increases with obesity, liver and/or kidney failure; decreases with pulmonary embolism, infections, and malignant tumors. It is excreted by the kidneys, mainly in the form of inactive metabolites, and only with the administration of high doses is it possible to excrete (up to 50%) unchanged. Not excreted by hemodialysis.
Indications. Treatment and prevention: deep vein thrombosis, pulmonary embolism (including in diseases of the peripheral veins), coronary artery thrombosis, thrombophlebitis, unstable angina, acute myocardial infarction, atrial fibrillation (including accompanied by embolization), DIC- syndrome, prevention and therapy of microthrombosis and microcirculation disorders, renal vein thrombosis, hemolyticouremic syndrome, mitral heart disease (prevention of thrombosis), bacterial endocarditis, glomerulonephritis, lupus nephritis. Prevention of blood clotting during operations using extracorporeal circulatory methods, during hemodialysis, hemosorption, peritoneal dialysis, cytapheresis, forced diuresis, when flushing venous catheters.
Contraindications. Hypersensitivity to heparin, diseases accompanied by increased bleeding (hemophilia, thrombocytopenia, vasculitis, etc.), bleeding, cerebral aneurysm, dissecting aortic aneurysm, hemorrhagic stroke, antiphospholipid syndrome, trauma (especially traumatic brain injury), uncontrolled arterial hypertension, erosive -ulcerative lesions of the gastrointestinal tract; cirrhosis of the liver, accompanied by varicose veins of the esophagus; menstrual period, threatened miscarriage, childbirth (including recent ones), recent surgical interventions on the eyes, brain, prostate gland, liver and biliary tract, condition after spinal puncture, pregnancy, lactation.
Carefully. Persons suffering from polyvalent allergies (including bronchial asthma), arterial hypertension, dental procedures, diabetes mellitus, endocarditis, pericarditis, ICH, active tuberculosis, radiation therapy, liver failure, chronic renal failure, old age (over 60 years, especially women ). Category of action on the fetus. C
Dosing. Heparin is prescribed as a continuous intravenous infusion or as regular intravenous injections, as well as subcutaneously (into the abdominal area). For prophylactic purposes - subcutaneously, 5 thousand IU/day, at intervals of 8-12 hours. The usual place for subcutaneous injections is the anterolateral abdominal wall (in exceptional cases, it is injected into the upper region of the shoulder or thigh), in this case, a thin needle is used, which should be inserted deeply, perpendicularly, into a fold of skin, held between the thumb and index finger until the solution is administered. The injection sites should be alternated each time (to avoid the formation of a hematoma). The first injection must be performed 1-2 hours before the start of surgery; in the postoperative period, administer for 7-10 days, and if necessary, for a longer period. The initial dose of heparin administered for therapeutic purposes is usually 5 thousand IU and is administered intravenously, after which treatment is continued using intravenous infusion. Maintenance doses are determined depending on the method of administration: - with continuous intravenous infusion, 1-2 thousand IU/hour (24-48 thousand IU/day) are prescribed, diluting heparin in a 0.9% NaCl solution; — for periodic intravenous injections, 5-10 thousand IU of heparin are prescribed every 4 hours. Doses of heparin for intravenous administration are selected so that the activated partial thromboplastin time (aPTT) is 1.5-2.5 times greater than the control. With subcutaneous administration of small doses (5 thousand IU 2-3 times a day) for the prevention of thrombus formation, regular monitoring of aPTT is not required, because it increases slightly. Continuous IV infusion is the most effective way to use heparin, better than regular (periodic) injections, because provides more stable hypocoagulation and is less likely to cause bleeding. When performing extracorporeal circulation, it is administered at a dose of 140-400 IU/kg or 1.5-2 thousand IU per 500 ml of blood. During hemodialysis, 10 thousand IU are first administered intravenously, then in the middle of the procedure another 30-50 thousand IU are administered. For older people, especially women, doses should be reduced. For children, the drug is administered intravenously: at the age of 1-3 months - 800 IU/kg/day, 4-12 months - 700 IU/kg/day, over 6 years - 500 IU/kg/day under APTT monitoring. Side effect. Allergic reactions: skin hyperemia, drug fever, urticaria, rhinitis, itching and feeling of heat in the soles, bronchospasm, collapse, anaphylactic shock. Dizziness, headaches, nausea, loss of appetite, vomiting, diarrhea. Thrombocytopenia (6% of patients), in rare cases fatal. Against the background of heparin-induced thrombocytopenia: skin necrosis, arterial thrombosis, accompanied by the development of gangrene, myocardial infarction, stroke. If severe thrombocytopenia develops (2 times the original number or below 100 thousand / μl), heparin administration is immediately stopped. With long-term use: osteoporosis, spontaneous bone fractures, soft tissue calcification, hypoaldosteronism, transient alopecia, increased activity of “liver” transaminases. Local reactions: irritation, pain, hyperemia, hematoma and ulceration at the injection site, bleeding. Bleeding: typical - from the gastrointestinal tract and urinary tract, at the site of drug administration, in areas exposed to pressure, from surgical wounds; hemorrhages in various organs (including adrenal glands, corpus luteum, retroperitoneal space).
Overdose. Symptoms: signs of bleeding.
Treatment: for minor bleeding caused by an overdose of heparin, it is enough to stop using it. In case of extensive bleeding, excess heparin is neutralized with protamine sulfate (1 mg of protamine sulfate per 100 IU of heparin). It must be borne in mind that heparin is rapidly eliminated, and if protamine sulfate is prescribed 30 minutes after the previous dose of heparin, only half the required dose should be administered; The maximum dose of protamine sulfate is 50 mg. Hemodialysis is ineffective.
Interaction. The effect of heparin is enhanced by some antibiotics (they reduce the formation of vitamin K by intestinal microflora), ASA, dipyridamole, NSAIDs and other drugs that reduce platelet aggregation (which remains the main mechanism of hemostasis in patients treated with heparin), indirect anticoagulants, drugs that block tubular secretion. Weakening - antihistamines, phenothiazines, cardiac glycosides, nicotinic acid, ethacrynic acid, tetracyclines, ergot alkaloids, nicotine, nitroglycerin (iv administration), thyroxine, ACTH, alkaline amino acids and polypeptides, protamine. Do not mix with other drugs in one syringe.
Special instructions. Heparin cannot be administered intramuscularly, because possible formation of hematomas at the injection site. The heparin solution may turn yellow, but this does not change its activity or tolerability. When prescribing heparin for therapeutic purposes, its dose is selected depending on the aPTT value. While using heparin, you should not administer other drugs intramuscularly or perform organ biopsies. To dilute heparin, only 0.9% NaCl solution is used. Although heparin does not pass into breast milk, its administration to nursing mothers in some cases caused the rapid (within 2-4 weeks) development of osteoporosis and spinal damage.
Indications for use
Indications for use of the gel
Heparin gel is used for the treatment and prevention of thrombophlebitis of the superficial veins , phlebitis (post-injection and post-infusion), lymphangitis , superficial periphlebitis, elephantiasis, localized infiltrates, bruises, swelling and injuries (including muscles, joints, tendons), superficial mastitis , subcutaneous hematomas .
Indications for use of the solution
Heparin injections are prescribed for thrombosis of deep veins , myocardial arteries , renal veins , pulmonary embolism, thrombophlebitis , atrial fibrillation (including if cardiac arrhythmia is accompanied by embolization), unstable angina , disseminated intravascular coagulation syndrome , acute myocardial infarction, mitral heart disease (prevention of blood clots ), bacterial endocarditis , hemolyticouremic syndrome , lupus nephritis , glomerulonephritis , for the prevention and treatment of microthrombosis and microcirculation disorders.
For preventive purposes, the drug is used during surgical interventions that use extracorporeal blood circulation methods, during cytapheresis, peritoneal dialysis, hemodialysis, forced diuresis, hemosorption, and when washing venous catheters.
When Heparin is administered intravenously, blood clotting slows down almost immediately, when administered into a muscle - after 15-30 minutes, when administered subcutaneously - after 20-60 minutes, when administered by inhalation, the effect is most pronounced after 24 hours.
Buy Heparin injection solution 5000 IU/ml 5ml No. 5 in pharmacies
Heparin Buy Heparin in pharmacies DOSAGE FORMS solution for intravenous and subcutaneous administration 5000IU/ml injection solution 25000IU injection solution 5000IU/ml
MANUFACTURERS Slavyanskaya Pharmacy (Russia)
GROUP Direct acting anticoagulants
COMPOSITION The active substance is sodium heparin.
INTERNATIONAL NON-PROPENTED NAME Heparin sodium
SYNONYMS Heparin-Acrigel 1000, Heparin-sodium Brown, Heparin-Ferein, Heparin sodium salt, Lavenum, Lyoton 1000, Trombless, Thrombogel 1000
PHARMACOLOGICAL ACTION Anticoagulative, fibrinolytic, antiaggregatory. The complex with antithrombin III inhibits thrombus formation: it binds activated factor X and inhibits the conversion of prothrombin to thrombin. In large doses, it inactivates thrombin and reduces the conversion of fibrinogen to fibrin, preventing the activation of the fibrin-stabilizing factor. The highest bioavailability is observed with intravenous administration; with subcutaneous administration, bioavailability is low, maximum concentration is achieved after 2-4 hours; half-life is 1-2 hours; in plasma is mainly in a protein-bound state. In patients with coronary artery disease (in combination with aspirin), it reduces the risk of acute coronary artery thrombosis, myocardial infarction and sudden death. Reduces the frequency of recurrent infarctions and mortality in patients who have had myocardial infarction. In high doses it is effective for pulmonary embolism and venous thrombosis, in small doses it is effective for the prevention of venous thromboembolism, incl. after surgical operations; with intravenous administration, blood coagulation slows down almost immediately, with intramuscular injection - after 15-30 minutes, with subcutaneous administration - after 40-60 minutes, after inhalation the maximum effect is within a day; the duration of the anticoagulation effect is respectively 4-5 hours, 6 hours, 8 hours, 1-2 weeks, the therapeutic effect - prevention of thrombus formation - lasts much longer. Deficiency of antithrombin III in plasma or at the site of thrombosis may limit the antithrombotic effect of heparin.
INDICATIONS FOR USE Unstable angina, acute myocardial infarction; thromboembolic complications during myocardial infarction, operations on the heart and blood vessels, thromboembolism of pulmonary and cerebral vessels, thrombophlebitis; DIC syndrome, prevention of microthrombosis and microcirculation disorders; renal vein thrombosis; hemolytic-uremic syndrome; atrial fibrillation, mitral heart defects; bacterial endocarditis; glomerulonephritis; lupus nephritis; rheumatism; bronchial asthma; carrying out extracorporeal methods (extracorporeal circulation during cardiac surgery, hemosorption, hemodialysis, peritoneal dialysis, cytapheresis), forced diuresis; flushing venous catheters.
CONTRAINDICATIONS Hypersensitivity, hemorrhagic diathesis, leukemia, anemia, increased vascular permeability, polyps, malignant neoplasms and ulcerative lesions of the gastrointestinal tract, severe dysfunction of the liver and kidneys, surgery on the brain and spine.
SIDE EFFECTS Dizziness, headaches, nausea, anorexia, vomiting, diarrhea, alopecia; early (2-4 days of treatment) and late (autoimmune) thrombocytopenia; hemorrhagic complications - bleeding in the gastrointestinal tract or urinary tract, retroperitoneal hemorrhages in the ovaries, adrenal glands (with the development of acute adrenal insufficiency), osteoporosis, soft tissue calcification, inhibition of aldosterone synthesis, increased levels of transaminases in the blood, allergic reactions (fever, rashes, bronchial asthma, anaphylactoid reaction), local irritation, hematoma, pain upon injection.
INTERACTION The effectiveness is enhanced by acetylsalicylic acid, dextran, phenylbutazone, ibuprofen, indomethacin, warfarin, dicoumarin, and weakened by cardiac glycosides, tetracyclines, antihistamines, nicotinic acid, ethacrynic acid.
METHOD OF APPLICATION AND DOSAGE SC (deep into the subcutaneous fatty tissue, changing injection sites), IV (slow), IM, inhalation - 20-50 thousand units/day, depending on the indications; A loading dose of 5 thousand units is usually administered intravenously, and then 20-40 thousand units/day using an infusion pump (a constant or intermittent administration regimen is used - 5-10 thousand units every 4-6 hours). To prevent postoperative thrombosis, small doses are administered intravenously—17 thousand units/day for 3-5 days. To prevent thromboembolism subcutaneously - 5 thousand units 2-8 hours before surgery, then every 8 hours the same dose is administered for 7 days. To improve microcirculation, a subcutaneous injection is administered - an average of 2.5-5 thousand units 3-4 times a day for 5-7 days with a gradual dose reduction.
OVERDOSE Symptoms: bleeding of varying severity. Treatment: in case of minor bleeding, reduce the dose or stop using the drug; in case of severe bleeding, a 1% solution of protamine sulfate is slowly administered intravenously.
SPECIAL INSTRUCTIONS Use during pregnancy and breastfeeding is possible only under strict indications. Constant monitoring of blood clotting time is necessary; withdrawal should be carried out gradually.
STORAGE CONDITIONS List B, store in a cool place, protected from light.
Contraindications
Heparin containing ointments (Heparin, Heparin-Acrigel 1000, etc.) are contraindicated in cases of hypersensitivity to the components they contain, as well as in diseases accompanied by ulcerative-necrotic processes, and injuries that are accompanied by violations of the integrity of the skin.
Heparin gel (ointment) should be used with caution in case of thrombocytopenia and increased tendency to bleeding.
Contraindications to the use of the injection form of the drug:
- hypersensitivity;
- diseases accompanied by increased bleeding ( vasculitis, hemophilia , etc.);
- bleeding;
- aortic dissection , intracranial aneurysm;
- antiphospholipid syndrome;
- traumatic brain injury;
- hemorrhagic stroke;
- uncontrolled hypertension;
- liver cirrhosis , accompanied by pathological changes in the veins of the esophagus;
- threatened miscarriage;
- menstrual period;
- pregnancy;
- childbirth (including recent);
- lactation period;
- erosive and ulcerative lesions of the stomach and intestinal tract;
- recent surgical interventions on the prostate gland, brain, eyes, bile ducts and liver, as well as the condition after lumbar puncture .
Heparin injections should be prescribed with caution to patients with polyvalent allergies (including bronchial asthma ), diabetes mellitus , arterial hypertension , active tuberculosis , endo- and pericarditis , chronic renal failure, liver failure ; patients undergoing dental procedures or radiation therapy; persons over 60 years of age (especially women); women using an IUD.
Side effects
When used externally, Heparin sodium can cause skin hyperemia and hypersensitivity reactions.
When administering the solution, the following are possible:
- Hypersensitivity reactions ( drug fever , skin hyperemia, rhinitis , feeling of heat in the soles, urticaria , skin itching, collapse, bronchospasm , anaphylactic shock ).
- Headaches, dizziness, diarrhea, loss of appetite, nausea, vomiting;
- Thrombocytopenia (in approximately 6% of patients), sometimes (rarely) with death. Heparin-induced thrombocytopenia (HIT) is accompanied by: arterial thrombosis , skin necrosis and gangrene , stroke , myocardial infarction . In case of severe HIT (when the platelet is reduced to half the original number or below 100 thousand/μl), heparin should be stopped immediately.
- Local reactions ( hematoma , hyperemia , pain, ulceration, irritation at the injection site, bleeding).
- Bleeding. Typical ones are considered to be from the urinary tract and gastrointestinal tract, in areas that are subject to pressure, at the site of drug administration, from surgical wounds. Hemorrhages are also possible in various internal organs: in the retroperitoneal space, corpus luteum, adrenal glands, etc.
With long-term use of Heparin, intermittent alopecia , osteoporosis , hypoaldosteronism , soft tissues become calcified, spontaneous bone fractures occur, and the activity of liver transaminases increases.
Instructions for use of Heparin (Method and dosage)
Heparin injections, instructions for use, administration features
Heparin in ampoules is prescribed in the form of:
- regular injections into a vein;
- continuous infusion;
- subcutaneously (injections in the stomach).
For preventive purposes, sodium heparin is administered subcutaneously at a dose of 5 thousand IU/day, leaving 8-12 hours between injections (to prevent thrombosis, the patient is injected with 1 ml of solution under the skin of the abdomen 2 times/day).
For medicinal purposes, the solution is infused intravenously (the method of administration is drip infusion). Dose - 15 IU/kg/h (that is, an adult with average body weight is prescribed 1 thousand IU/h).
To achieve a rapid anticoagulant effect, 1 ml of solution is injected intravenously into the patient immediately before infusion. If administration into a vein is impossible for some reason, then the medicine is injected under the skin 4 times a day. 2 ml.
The highest daily dose is 60-80 thousand IU. The use of Heparin at the indicated dose for more than 10 days is permitted only in exceptional cases.
For children, the solution is injected into a vein by drip. The dose is selected depending on age: at the age of 1 to 3 months the daily dose is 800 IU/kg, from 4 months to a year - 700 IU/kg, children over 6 years of age are prescribed (under APTT monitoring) 500 IU/kg/ days
Technique for administering Heparin, preparation for manipulation and administration of solution
Subcutaneous injections are usually given into the anterolateral wall of the abdomen (if this is not possible, the medicine can be injected into the upper thigh/shoulder area).
A thin needle is used for injection.
The first injection is given 1-2 hours before the start of the operation; in the postoperative period, the drug continues to be administered for 7-10 days (if necessary, longer).
Treatment begins with a jet injection of 5 thousand IU of heparin into a vein, after which the solution is continued to be administered using an intravenous infusion (a 0.9% NaCl solution is used to dilute the drug).
Maintenance doses are calculated depending on the route of administration.
The algorithm for administering Heparin is as follows:
- 15-20 minutes before administering the drug, apply cold to the injection site in the abdominal area (this will reduce the likelihood of bruising).
- The procedure is performed in compliance with the rules of asepsis.
- The needle is inserted into the base of the fold (the fold is held between the thumb and forefinger until the end of drug administration) at an angle of 90°.
- Do not move the tip of the needle after insertion or retract the piston. Otherwise, tissue damage and hematoma formation may occur.
- The solution should be injected slowly (to reduce pain and avoid tissue damage).
- The needle is removed easily, at the same angle at which it was inserted.
- There is no need to wipe the skin; the injection site is lightly pressed with a sterile dry swab (the swab is held for 30-60 seconds).
- It is recommended to alternate anatomical sites for injection. The areas in which injections are given during the week should be 2.5 cm apart from each other.
Heparin ointment, instructions for use
The gel is used as an external agent. It should be applied to the affected area from 1 to 3 times a day. A single dose is a column 3 to 10 cm long.
For thrombosis of hemorrhoidal veins, the drug is used rectally.
Gel-impregnated cotton pads are applied to the inflamed nodes and secured with a bandage. Gel-soaked tampons are inserted into the anus. Treatment usually lasts 3-4 days.
For leg ulcers, the ointment is carefully applied to the inflamed skin around the ulcer.
Frequency of applications - 2-3 rubles/day. Treatment is continued until the inflammation disappears. Usually the course lasts from 3 to 7 days. The doctor decides whether a longer course is necessary.
Other heparin-containing ointments are used in a similar way (for example, the instructions for Heparin-Acrigel 1000 are practically no different from the instructions for Heparin gel or Lyoton 1000 ).
For the treatment of hemorrhoids (external and internal), anal fissures , thrombophlebitis of the anal veins , as well as to relieve itching and eliminate eczema suppositories for hemorrhoids (for example, Hepatrombin G can be used as an alternative to Heparin ointment .
Additional Information
Heparin is available only in the form of a solution, ointment or gel (gel, unlike ointment, contains a larger amount of the active substance and is better absorbed into the skin).
Heparin tablets are not available because heparin is practically not absorbed from the digestive tract.
Heparin therapy in the acute period of myocardial infarction
A.N.YAKOVLEV , Doctor of Medical Sciences, Professor, Federal State Institution “Federal Center of Heart, Blood and Endocrinology named after V.A. Almazov Rosmedtekhnologii”, St. Petersburg
The development of acute thrombosis of the coronary artery is the leading pathogenetic mechanism of destabilization of the course of coronary heart disease. Drug interventions related to the effect on the blood coagulation system play a key role in the treatment of patients in the acute period of myocardial infarction after reperfusion therapy (thrombolysis or primary coronary angioplasty), if the latter can be performed taking into account the timing of the disease and possible contraindications. The maximum therapeutic effect can be achieved by simultaneous administration of drugs that act on different parts of hemostasis. Correct prescription of anticoagulants and antiplatelet agents can reduce the risk associated with both the threat of relapse of the disease with expansion of the area of myocardial damage, and the risk of bleeding.
In practical medicine, a rather narrow range of drugs is used, the effectiveness of which has been proven in large multicenter randomized clinical trials. Thus, unfractionated heparin, low molecular weight heparins, fondaparinux are used as anticoagulants, and acetylsalicylic acid and clopidogrel are used as antiplatelet drugs. Unfractionated heparin
The official heparin solution contains a mixture of sulfated polysaccharides with a molecular weight of 2000 to 30,000 Da. About a third of the drug molecules consist of 18 or more polysaccharide residues and, in combination with antithrombin III, can significantly reduce the activity of thrombin (factor IIa), as well as Xa, IXa and other coagulation factors. Inhibition of thrombin is accompanied by a decrease in coagulation, which can be assessed by determining the activated partial thromboplastin time (aPTT). The antithrombotic effect is mainly due to inhibition of prothrombinase (factor Xa). Short chain heparin has a low molecular weight and primarily affects factor Xa. The bioavailability of heparin is low and is influenced by many factors - interaction with plasma proteins, uptake by endothelial cells and macrophages, platelet activity. Also important is the plasma level of antithrombin III, with which heparin forms an active complex.
In Russia, unfractionated heparin is used in the form of a sodium salt solution (Heparin Sodium) containing 5000 IU of heparin per 1 ml. With a single intravenous administration, the effect of the drug occurs immediately and lasts up to 3 hours; The half-life from plasma is 30-60 minutes. The most stable and controlled hypocoagulation effect is observed with prolonged intravenous infusion using a syringe or pump dispenser, therefore this method of administration is standard when treating with unfractionated heparin.
In myocardial infarction, anticoagulant therapy with heparin should be started as soon as possible after the onset of symptoms.
The relationship between the dose of heparin and its anticoagulation effect is nonlinear. The severity and duration of the effect increases disproportionately with increasing dose. Thus, with an intravenous bolus of 25 IU/kg, the half-life of heparin is 30 minutes, with a bolus of 100 IU/kg - 60 minutes, with 400 IU/kg - 150 minutes. To objectively assess the anticoagulant effect of heparin and get an idea of the state of the internal pathway of plasma hemostasis, it is possible to determine the activated partial thromboplastin time (aPTT), which reflects the initial stage of coagulation - the formation of thromboplastin. When treating with heparin, it is necessary to determine the aPTT, since it is this indicator that allows you to individually select the dosage regimen and monitor the effectiveness of therapy.
The development of bleeding is the most likely and dangerous complication of heparin therapy. Most often, the source of blood loss is erosion and ulcerative defects localized in the upper parts of the gastrointestinal tract. It should be noted that the development of posthemorrhagic anemia in patients with myocardial infarction is an independent unfavorable prognostic factor. A detailed history collection, including information on previous anticoagulant therapy, identification of symptoms of hemorrhagic diathesis, determination of the platelet count and initial aPTT allows assessing the risk of developing hemorrhagic complications.
When treating with heparin, it is necessary to determine the aPTT, since it is this indicator that allows you to individually select a dosage regimen and monitor the effectiveness of therapy
Serious complications are also the development of thrombocytopenia followed by heparin-induced thrombosis, osteoporosis, and antithrombin III deficiency.
A number of multicenter studies (ATACS, RISC, SESAIR and others) have confirmed the effectiveness of heparin and combination therapy with heparin and aspirin in acute myocardial infarction (AMI). In the prethrombolytic era, heparin administration led to a reduction in deaths (by 17%), recurrent infarctions (by 22%), as well as a decrease in the incidence of strokes and episodes of pulmonary embolism. At the same time, the number of non-cerebral bleedings increased.
The effectiveness of heparin in AMI in combination with thrombolytic therapy was assessed in the GUSTO study. In the group of patients receiving continuous intravenous infusion of heparin, the patency of the coronary artery supplying the infarction area was significantly higher (84 vs. 71%, p<0.05), and the 5-year survival rate was 1% higher compared to the group of patients receiving heparin by subcutaneous injection. In accordance with current recommendations for the treatment of AMI, unfractionated heparin can only be prescribed as a continuous intravenous infusion.
In myocardial infarction (MI), anticoagulant therapy with heparin should be started as soon as possible after the onset of symptoms. For non-ST segment elevation MI, treatment with unfractionated heparin should be continued for at least 48 hours. For ST-segment elevation MI, heparin treatment is considered as part of a reperfusion strategy. In the case of thrombolytic therapy, the administration of heparin should begin simultaneously with it and continue for at least 24-48 hours. When performing primary coronary angioplasty, heparin is administered before and during the procedure. If the intervention is successful, heparin therapy can be discontinued.
For ST-elevation MI without reperfusion therapy, treatment tactics with unfractionated heparin are similar to those for thrombolytic therapy. Thrombolytic therapy with streptokinase is the only clinical situation in which current recommendations allow the use of fixed doses and subcutaneous administration of unfractionated heparin. In this case, it is possible to administer a bolus of 5000 IU of heparin followed by an infusion of 1000 IU/hour in patients weighing over 80 kg and 800 IU/hour in patients weighing less than 80 kg. Only in this situation, instead of infusion, subcutaneous administration of heparin at a dose of 12,500 IU twice a day is permissible.
The current standard for prescribing therapy with unfractionated heparin is to individually calculate the dose depending on body weight, taking into account the clinical situation and concomitant therapy. Rules for calculating the dose of heparin are presented in Table 1.
Therapy is monitored by re-evaluating the APTT. Target APTT values are considered to be within 50–75 seconds or 1.5–2.5 times higher than the upper limit of normal established for a given laboratory. During the first day after the start of heparin therapy, it is advisable to determine the aPTT at 3, 6, 12 hours from the start of the infusion and then depending on its values (Table 2). After changing the infusion rate, the APTT is re-monitored after 6 hours. If APTT values exceed 130 seconds, it is recommended to take a break in the infusion for 90 minutes and conduct additional monitoring of the APTT at the end of the infusion break. If the aPTT is within the target range for two consecutive measurements with an interval of at least 6 hours against the background of a constant rate of heparin infusion, in the future it is permissible to monitor the aPTT once a day if the rate of heparin administration remains the same. In case of hemorrhagic complications, APTT must be determined immediately.
In some cases, in particular with a deficiency of coagulation factors, antiphospholipid syndrome, against the background of thrombolytic therapy, when taking indirect anticoagulants, the specificity of the APTT test can be significantly reduced.
In rare cases, high doses of heparin (more than 35,000 IU per day) are required to achieve target aPTT values, indicating heparin resistance. To confirm the phenomenon, it is recommended to determine the activity of the factor Xa inhibitor. Low molecular weight heparins
Low molecular weight heparins are preparations of mucopolysaccharides with a molecular weight of 4000–7000 Da. Low molecular weight heparins, unlike unfractionated heparins, have an antithrombotic effect by inhibiting factor Xa and without having a significant effect on thrombin activity. Heparins, which have very short polysaccharide chains and a very low molecular weight, do not have an aptithrombotic effect. With chain lengths ranging from 8 to 18 polysaccharide units, the drugs primarily inhibit factor Xa and exhibit antithrombotic activity with a minimal risk of bleeding. The bioavailability of low molecular weight heparins reaches almost 100%, while the half-life is 2-4 times higher than that of unfractionated heparin. In general, low-molecular-weight heparins have a more predictable, long-lasting, and selective effect and can be administered by subcutaneous injection once or twice daily. Therapy with low molecular weight heparins does not require monitoring of laboratory parameters of blood coagulation.
The main pharmacological characteristics of low molecular weight heparins are presented in Table 3.
Adverse effects when treated with low molecular weight heparins are similar to those when using unfractionated heparin. Moreover, according to a meta-analysis that combined data on 4669 patients, in the group of patients receiving low molecular weight heparins, the risk of major bleeding was 52% lower. The metabolism of low molecular weight heparins is carried out with the participation of the kidneys, therefore the use of drugs of this group in patients with a decrease in creatinine clearance of less than 30 ml/hour is contraindicated.
Therapy with low molecular weight heparins does not require monitoring of laboratory parameters of blood clotting
The most studied drug from the group of low molecular weight heparins for use in patients with AMI is enoxaparin, registered for use both in acute coronary syndrome without ST-segment elevation and in AMI with ST elevation. According to the results of a meta-analysis of 6 large multicenter studies, including a total of about 22,000 patients with acute coronary syndrome, the advantages of enoxaparin therapy compared with unfractionated heparin were convincingly demonstrated, consisting in a significant reduction in the risk of death and non-fatal myocardial infarction.
In combination with thrombolytic therapy, the use of enoxaparin is preferable to unfractionated heparin. For patients under 75 years of age without renal impairment, bolus intravenous administration of enoxaparin at a dose of 30 mg is indicated, followed (after 15 minutes) by subcutaneous administration at a rate of 1 mg/kg every 12 hours. For patients over 75 years of age, bolus administration is not required. The duration of enoxaparin therapy should not exceed 8 days.
When performing primary endovascular intervention, an infusion of unfractionated heparin should be prescribed. In patients who have not received reperfusion therapy, enoxaparin can be used in accordance with the above regimen for patients who have received thrombolytic therapy.
Conclusion
Heparin therapy is an integral component in the treatment of patients with myocardial infarction. To achieve maximum effect, it is necessary to adequately select the drug, taking into account contraindications, assessing possible risks, carefully following dosing recommendations and conducting adequate laboratory monitoring.
Literature
1. Panchenko E.G., Dobrovolsky A.B. Possibilities for diagnosing hemostasis disorders and promising directions of antithrombotic therapy for coronary heart disease. // Cardiology. – 1996. – No. 5. – P. 4-9. 2. Cairns JA, Throux P, Lewis HD, Ezekowitz M, Meade TW Antithrombotic Agents in Coronary Artery Disease. In: Sixth ACCP Consensus Conference on Antithrombotic Therapy. Chest 2001; 119:228S—252S. 3. Dinwoodey DL, Ansell JE Heparins, Low-Molecular-Weight Heparins, and Pentasaccharides: Use in the Older Patient. // Cardiol. Clin. – 2008/ – V. 26. P. 145–155. 4. Hirsh J., Bauer KA, Donati MB Parenteral Anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133; 141S—159S. 5. Kitchen S. Problems in laboratory monitoring of heparin dosage. // Br. J. Haematol. 2000. – V. 111. – P. 397–406. 6. MacMahon S., Collins R., Knight C. Reduction in major morbidity and mortality by heparin in acute myocardial infarction. // Circulation. – 1998. – V. 78(suppl II). –P. 98.-104. 7. Peterson JL, Mahaey KW, Hasselblad M. Ef?cacy and bleeding complications among patients randomized to enoxaparin or unfractionated heparin for antithrombin therapy in non-ST-segment elevation acute coronary syndrome. // JAMA. – 2004. – V. 292. P. 89–96. 8. The Global Utilization of Streptokinase, and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO) Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. // N. Engl. J. Med. – 1993. V. 329 (10). – P. 673-82.
Tables and figures are in the attached file
Overdose
Symptoms of overdose with parenteral use are bleeding of varying severity.
Treatment: for minor bleeding caused by an overdose of the drug, it is enough to stop using it. If bleeding is extensive, protamine sulfate (1 mg per 100 IU of heparin) is used to neutralize excess heparin.
Please note that heparin is eliminated quickly. Thus, if protamine sulfate is administered 30 minutes after the previous dose of heparin, it should be administered at half the dose; The highest dose of protamine sulfate is 50 mg.
It is not excreted by hemodialysis.
Cases of overdose with external use of the drug have not been described. Due to the low systemic absorption of the drug, an overdose is considered unlikely. With prolonged use on large surfaces, hemorrhagic complications .
Treatment: discontinuation of the drug, if necessary, use of a one percent solution of protamine sulfate (heparin antagonist).
Heparin gel I 1000IU/g 30g No. 1
Name
Heparin gel 1000IU/1g 30g
Description
The gel is colorless to light yellow with a specific odor.
Main active ingredient
Heparin sodium
Release form
Gel
Dosage
1000IU/1g
pharmachologic effect
Pharmacological studies show that when applied externally, Heparin gel has a pronounced antiexudative, antiedematous, antigranulomatous, anti-inflammatory and anticoagulant effect.
Indications for use
- symptomatic treatment and reduction of swelling and bruising after blunt trauma (for example, after a bruise); — symptomatic treatment of diseases of the superficial veins (varicose veins, phlebitis, periphlebitis, thrombophlebitis), varicose ulcers, varicophlebitis, conditions after removal of the great saphenous vein of the thigh as part of complex therapy.
Directions for use and doses
1-3 times a day, apply 3-10 cm of gel to the affected area of the skin and rub in gently. Due to limited experience with the drug in children and because there is insufficient research data, this drug should not be used in the treatment of children.
Use during pregnancy and lactation
Use during pregnancy is possible only if indicated under medical supervision. Can be used during lactation according to indications.
Impact on the ability to drive vehicles and other potentially dangerous mechanisms
The drug does not affect the ability to drive vehicles and potentially dangerous machinery.
Precautionary measures
If there are signs of bleeding, the possibility of using Heparin gel should be carefully considered. Heparin gel should not be used for bleeding, applied to open wound surfaces, weeping eczema or mucous membranes, as well as to infected areas in the presence of purulent processes. The penetration of heparin into healthy skin has been described in the case of topical application; Therefore, if thromboembolic complications are suspected, a platelet count should be checked to differentiate heparin-induced thrombocytopenia type II. Therefore, regular platelet count checks in patients with a history of thromboembolic complications are necessary whenever heparin is used (before starting heparin, on the first day after starting use, and then regularly every 3-4 days during treatment until the end of treatment). Heparin gel contains methyl parahydroxybenzoate and propyl parahydroxybenzoate as excipients, so it cannot be used in patients with allergies to parabens.
Use in pediatrics
Due to limited experience with the drug in children and because there is insufficient research data, the gel should not be used in the treatment of children.
Interaction with other drugs
The anticoagulant effect of heparin is enhanced by the simultaneous use of anticoagulants, antiplatelet agents and non-steroidal anti-inflammatory drugs. Ergot alkaloids, thyroxine, tetracycline, antihistamines and nicotine reduce the effect of heparin.
Contraindications
- known hypersensitivity to heparin or any component of the drug; - history of heparin-induced thrombocytopenia type II (immune-mediated HIT type II).
Compound
per tube: active substance - heparin (in the form of sodium heparin) - 1000 IU/g; excipients - carbopol 980 NF, levomenthol, methyl parahydroxybenzoate (E-218), propyl parahydroxybenzoate (E-216), rectified ethyl alcohol from food raw materials, triethanolamine, purified water.
Overdose
Due to low systemic absorption, overdose is unlikely. To date, the phenomena of overdose when using Heparin gel have not been described. With prolonged use on large surfaces, hemorrhagic complications are possible. Treatment: drug withdrawal. If necessary, use a heparin antagonist - protamine sulfate (1% solution).
Side effect
Allergic reactions to heparin after applying the drug to the skin are very rare. However, in some cases, hypersensitivity reactions may occur, such as skin redness and itching, which quickly disappear after stopping use of the drug. Incidence of heparin-induced antibody-mediated thrombocytopenia type II (platelet count
Storage conditions
Store at a temperature not exceeding 25°C. Keep out of the reach of children.
Buy Heparin gel d/nar.approx. 1000IU/g in tubes 30g in pack No. 1 in the pharmacy
Price for Heparin gel d/nar.approx. 1000IU/g in tubes 30g in pack No. 1
Instructions for use for Heparin gel d/nar. approx. 1000 IU/g in tubes 30 g in pack No. 1
Interaction
Drugs that block tubular secretion, indirect anticoagulants that reduce the formation of vitamin K by intestinal microflora, antibiotics, NSAIDs, dipyridamole , ASA and other drugs that reduce platelet aggregation enhance the effect of heparin.
The weakening of the effect is facilitated by: cardiac glycosides , ergot alkaloids , phenothiazines , antihistamines, nicotine , ethacrynic and nicotinic acids , nitroglycerin (iv administration), ACTH, tetracyclines , alkaline amino acids and polypeptides, thyroxine , protamine .
Do not mix the solution in the same syringe with other medications.
When applied topically, the anticoagulant effect of the drug is enhanced when the gel is used in combination with antiplatelet agents, NSAIDs, and anticoagulants. Tetracycline , thyroxines , nicotine and antihistamines reduce the effect of heparin.
special instructions
Due to the risk of hematoma formation at the injection site, the solution should not be injected into the muscle.
The solution may acquire a yellowish tint, which does not affect its activity or tolerability.
When prescribing the drug for therapeutic purposes, the dosage should be selected taking into account the aPTT value.
During treatment with the drug, organ biopsies and other medications should not be administered intramuscularly.
To dilute the solution, only 0.9% NaCl solution can be used.
The gel should not be applied to mucous membranes or open wounds. In addition, it is not used in the presence of purulent processes. The use of ointment is not recommended for DVT.
Unfractionated Heparin
Heparin with an average molecular weight of 12-16 thousand daltons, which is isolated from bovine lung or the mucous membrane of the intestinal tract of pigs, is called unfractionated. It is used in the production of drugs that have local and systemic effects (heparin containing ointments and solutions for parenteral administration).
The drug, through interaction with AT III (indirectly), inhibits the main enzyme of the blood coagulation system, as well as other coagulation factors, and this in turn leads to antithrombotic and anticoagulation effects.
Endogenous heparin in the human body can be found in muscles, intestinal mucosa, and lungs. In structure, it is a mixture of glycosaminoglycan fractions, which consist of sulfatide residues of D-glucosamine and D-glucuronic acid with a molecular weight of 2 to 50 thousand daltons.
Fractionated Heparin
Fractionated (low molecular weight) heparins are obtained by enzymatic or chemical depolymerization of unfractionated heparins. This Heparin consists of polysaccharides with an average molecular weight of 4-7 thousand daltons.
LMWHs are characterized as weak anticoagulants and highly effective direct-acting antithrombotics. The action of such drugs is aimed at compensating hypercoagulation processes.
LMWH begins to act immediately after administration, while its antithrombotic effect is pronounced and prolonged (the drug is administered only 1 time per day).
Classification of low molecular weight Heparins:
- drugs used to prevent thrombosis/thromboembolism ( Klivarin , Troparin , etc.);
- drugs used to treat unstable angina and MI without a pathological Q wave, thrombosis and thromboembolism , acute DVT, PE ( Fragmin , Clexane , Fraxiparine );
- drugs used to treat severe vein thrombosis ( Fraxiparine Forte );
- drugs used to prevent thrombus formation and coagulation during hemofiltration and hemodialysis ( Fraxiparine , Fragmin , Clexane ).
Heparin[edit | edit code]
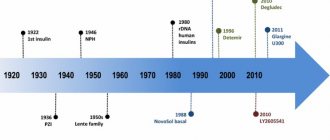
Historical reference
. In 1916, medical student McLane, who was studying the nature of ether-soluble procoagulants, was lucky enough to discover a phospholipid anticoagulant. Shortly thereafter, Govell, in whose laboratory McClain worked, discovered a water-soluble glycosaminoglycan, named heparin because of its high content in the liver (Jaques, 1978). Heparin's success in preventing coagulation in vitro led to its later use in the treatment of venous thrombosis.
Chemical properties and mechanism of action[edit | edit code]
Heparin
- glycosaminoglycan found in mast cell granules. During its synthesis, a polymer consisting of alternating D-glucuronic acid and N-acetyl-glucosamine residues is formed from various UDP sugars (Bourin and Lindahl, 1993). Approximately 10-15 such glycosaminoglycan chains (200-300 monosaccharides each) are attached to the protein part of the molecule, forming a proteoglycan with a molecular weight of 750,000-1,000,000. Then modification of the glycosaminoglycan chains occurs: N-deacetylation and N-sulfation of glucosamine residues, epimerization D-glucuronic acid into L-iduronic acid, O-sulfation of residues of these acids in position 2, O-sulfation of glucosamine residues in positions 3 and 6 (Fig. 55.2). Since these reactions do not affect all monosaccharides, the structure of the resulting molecules is quite diverse. The glycosaminoglycan chains of heparin transferred to mast cell granules are cleaved by p-glucuronidase into fragments with a molecular weight of 5000-30,000 (on average about 12,000, that is, 40 monosaccharides) within a few hours.
Related glycosaminoglycans[edit | edit code]
Heparan sulfate is present on the cell membrane of most eukaryotic cells and in the extracellular matrix. It is synthesized from the same repeating disaccharide sequences as heparin (D-glucuronic acid and N-acetylglucosamine), but undergoes less modification and therefore contains more D-glucuronic acid and N-acetylglucosamine and fewer sulfate groups. Heparan sulfate also has anticoagulant properties in vitro, but at much higher concentrations.
Dermatan sulfate is a polymer of L-iduronic acid and N-acetylgalactosamine with varying degrees of O-sulfation of L-iduronic acid at position 2 and galactosamine at positions 4 and 6. Like heparan sulfate, dermatan sulfate is present on the cell membrane and in the extracellular matrix and has anticoagulant properties in vitro.
Sources[edit | edit code]
Heparin is usually obtained from bovine lung or porcine intestinal lining. Such drugs may contain a small admixture of other glycosaminoglycans. Although the composition of heparins from different manufacturers is somewhat different, their biological activity is approximately the same (about 150 units/mg). 1 unit is taken to be the amount of heparin that prevents the clotting of 1 ml of citrated sheep plasma within an hour after adding 0.2 ml of 1% CaCl2.
Low molecular weight heparins with a molecular weight of 1000–10,000 (average 4500, i.e. 15 monosaccharides) are obtained from a conventional preparation by gel filtration, ethanol precipitation or partial depolymerization using nitrous acid and other reagents. Low molecular weight heparins differ from regular heparins and from each other in pharmacokinetic properties and mechanism of action (see below). Their activity is usually determined by inhibition of factor Xa.
Physiological role[edit | edit code]
Heparin is found in tissues inside mast cells. It appears to be required for the storage of histamine and some proteases within the granules of these cells (Humphries et al., 1999; Forsberg et al., 1999). Once released from mast cells, heparin is quickly taken up and destroyed by macrophages. It cannot be detected in the plasma of healthy people. However, in patients with systemic mastocytosis with massive degranulation of mast cells, a slight prolongation of the aPTT is sometimes observed, presumably associated with the release of heparin into the bloodstream.
Heparan sulfate molecules on the surface of endothelial cells and in the extracellular matrix of the subendothelial layer interact with antithrombin III, preventing thrombus formation. With malignant neoplasms, bleeding is sometimes observed, caused by heparan sulfate or dermatan sulfate entering the bloodstream (probably due to tumor disintegration).
Mechanism of action[edit | edit code]
In 1939, Brinkhaus et al. discovered that the anticoagulant effect of heparin is mediated by one of the plasma components and called it the heparin cofactor. Thirty years later, it was discovered to be antithrombin III, a plasma protein that rapidly inactivates thrombin in the presence of heparin (Olson and Bjork, 1992). Antithrombin III is a glycosylated single-chain polypeptide with a molecular weight of approximately 58,000, homologous to the serpin family (spin yrothease inhibitors), in particular agantitrypsin. Antithrombin III is synthesized in the liver, its serum concentration is 2.6 µmol/l. It is active against factors of the intrinsic and general coagulation mechanisms (in particular, 1Xa, Xa and thrombin), but has little effect on factor Vila. The mechanism of the inhibitory effect of antithrombin III is as follows. The listed coagulation factors, as already mentioned, are proteases. Antithrombin III acts as their substrate: active coagulation factors attack a specific peptide bond between arginine and serine in the reactive center of its molecule. However, cleavage of this bond does not occur, and a stable complex is formed from the coagulation factor and antithrombin III in an equimolar ratio. As a result, the coagulation factor loses its proteolytic activity.
Heparin accelerates the interaction of antithrombin III with thrombin by more than 1000 times due to the fact that it serves as a matrix linking both proteins. Binding to heparin also changes the conformation of antithrombin III, making its reactive site more accessible to thrombin (Jin et al., 1997). After the formation of the thrombin-antithrombin III complex, the heparin molecule is released. The region of the heparin molecule responsible for binding to antithrombin III is a pentasaccharide sequence containing a glucosamine residue O-sulfated at position 3 (Fig. 55.2). This structure is found in approximately 30% of heparin molecules and, less commonly, in heparan sulfate. Other glycosaminoglycans (dermatan sulfate, chondroitin sulfates) lack this structure and are not able to activate antithrombin III. Heparins with a molecular weight of less than 5400 (containing less than 18 monosaccharides) cannot bind both antithrombin III and thrombin and therefore do not accelerate the inactivation of the latter. At the same time, shown in Fig. 55.2 pentasaccharide catalyzes the inhibition of factor Xa by antithrombin III (apparently, only conformational changes in antithrombin III are sufficient for this). This explains the anticoagulant effect of low molecular weight heparins, most of whose molecules are too short to bind thrombin.
Antithrombin III quickly (T1/2 <0.1 s) inhibits factors 1Xa, Xa and thrombin at plasma heparin concentrations of 0.1 - 10 units/ml. At the same time, the aPTT and thrombin time (plasma clotting time when thrombin is added) are prolonged; PV changes less. Factor Xa on the surface of platelets (as part of the prothrombinase complex) and thrombin bound to fibrin are not inhibited by heparin and antithrombin III.
Figure 55.2. Antithrombin-binding region of the heparin molecule.
Thus, heparin accelerates the inactivation of factor Xa and jumbin only after they are released from their binding sites. Platelet factor 4, released from α granules during platelet aggregation, interferes with the binding of antithrombin III to heparin and heparan sulfate, promoting thrombus formation at the site of clotting.
When the concentration of heparin or dermatan sulfate is above 5 units/ml, their inhibitory effect on thrombin is mediated primarily by the heparin cofactor P. Heparin also stimulates the suppression of thrombin activity by plasminogen antiactivator 1, protein C inhibitor and nexin-1 protease and factor Xa activity by an inhibitor of the extrinsic coagulation mechanism. The concentrations of the last four inhibitors in plasma are more than 100 times less than the concentration of antithrombin III. IV administration of heparin increases the concentration of the inhibitor of the extrinsic coagulation mechanism several times (possibly causing its release from binding sites on the endothelium).
Other properties of heparin[edit | edit code]
High doses of heparin may prolong bleeding time by interfering with platelet aggregation. It is not clear whether the antiplatelet effect of heparin contributes significantly to the bleeding it causes. Heparin clarifies chylous plasma, causing the release of lipoprotein lipase into the bloodstream, which breaks down triglycerides into fatty acids and glycerol. This phenomenon is observed even at low concentrations of heparin, insufficient to exhibit an anticoagulant effect. After discontinuation of the drug, rebound hyperlipoproteinemia is possible.
Heparin inhibits the growth of many cells in culture, including endothelial and vascular smooth muscle cells, as well as renal mesangial cells. In animal experiments, it prevented the proliferation of vascular smooth muscle cells after damage to the endothelium of the carotid arteries. This effect of heparin is in no way related to its anticoagulant activity (Wright et al., 1989).
Acid and basic fibroblast growth factors have a high affinity for heparin. These factors stimulate the growth of smooth muscle, endothelial and other mesenchymal cells, as well as angiogenesis. Heparin itself suppresses the growth of capillary endothelial cells, but at the same time potentiates the effect of acidic fibroblast growth factor on these cells (Sudhal-tere et al., 1989). This effect does not depend on its anticoagulant activity, but on the size and degree of sulfation of heparin molecules. Heparan sulfate on the surface of mesenchymal cells serves as a low-affinity binding site for basic fibroblast growth factor, and in the extracellular matrix it stabilizes this factor and acts as a depot from which basic fibroblast growth factor is released under the action of heparin sulfate lyase or excess heparin. In addition, like heparin, it is necessary for the biological activity of basic fibroblast growth factor, facilitating its binding to a high-affinity receptor with its own tyrosine kinase activity (Yayon et al., 1991).
Analogs
Level 4 ATC code matches:
Girudoproct
Heparoid Zentiva
Heparin ointment
Gepatrombin G
Lyoton
Trombless
Venolife
Hepatrombin
Gel analogues: Heparin-Acrigel 1000 , Lyoton 1000 , Lavenum , Trombless .
Generic injection forms: Heparin J , Heparin-Ferein , Heparin-Sandoz .
Drugs with a similar mechanism of action: tablets - Piyavit , Angioflux , Wessel Due F ; solution - Angioflux , Hemapaxan , Antithrombin III human , Wessel Due F , Fluxum , Anfibra , Fraxiparine , Enixum .
Use during pregnancy and lactation
Heparin solution is not contraindicated for pregnant women. However, despite the fact that the active substance of the drug does not penetrate into milk, its use in nursing mothers in some cases led to the rapid (within 2-4 weeks) development of osteoporosis and spinal damage.
The feasibility of use should be decided individually, taking into account the risk to the fetus/benefit to the mother ratio.
There are no data on the use of the gel during pregnancy and lactation.
Reviews
Heparin is an effective and well-studied antithrombotic agent , the mechanism of action of which is to suppress the activity of thrombin , which catalyzes the biotransformation of fibrinogen into fibrin and a number of other reactions in the hemostatic system.
Most often, the external use of gel and ointment forms of the drug is discussed on the Internet. Reviews of heparin-containing ointments and gels (in particular, reviews of Heparin Acrigel 1000 ) are overwhelmingly positive: such drugs really help with bruises, thrombophlebitis and hemorrhoids , and also remove localized infiltrates well.
Content
- 1 Heparin 1.1 Chemical properties and mechanism of action 1.1.1 Related glycosaminoglycans
- 1.1.2 Sources
- 1.3.1 Other properties of heparin
- 2.1 Pharmacokinetics
- 2.3.1 Bleeding
Heparin price
The average price of Heparin injections in Ukrainian pharmacies is from 180 to 226 UAH (5 ml ampoules, No. 5). You can buy Heparin ointment for an average of 35 UAH. The price of Heparin Acrigel 1000 in Ukraine is about 250 UAH.
In Russian pharmacies, sodium heparin in ampoules can be purchased for 360-550 rubles. The price of Heparin gel is 260-300 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Heparin-Akrikhin 1000 gel 1 thousand.
IU/1g 30gAO Akrikhin 362 rub.order - Heparin-Akrikhin 1000 gel for external use. approx. 1000 IU/g tube 50g JSC AKRIKHIN
RUR 437 order
- Heparin ointment 25g Belmedpreparaty RUP Belmedpreparaty
73 rub. order
- Heparin ointment 25g NizhpharmAO "Nizhpharm"
82 RUR order
- Heparin ointment 25g n1Altaivitaminy JSC
63 RUR order
Pharmacy Dialogue
- Heparin ointment (tube 25g) Nizhpharm JSC
72 RUR order
- Heparin-Akrikhin gel 1000IU/g 30gAkrikhin OJSC
RUB 355 order
- Heparin-Akrikhin gel (gel 1000EM/g 50g) Akrikhin JSC
RUR 459 order
- Heparin-Akrikhin gel (gel 1000EM/g 30g) Akrikhin JSC
RUB 367 order
- Heparin (vial IV and SC injection 5tIU/ml 5ml No. 5) Moscow Endocrine Plant
RUB 1,595 order
show more
Pharmacy24
- Heparin-Darnitsa 600 units 30 g gel PrAT" Pharmaceutical company "Darnitsa", Ukraine
62 UAH. order - Heparin ointment 25 g TOV DKP Pharm.Fabrika, Ukraine
46 UAH order
- Heparin-Indar 5000 MO/ml 5 ml (25000 MO) No. 1 solution PrAT “On the production of insulin” Indar”, m. Kiev, Ukraine
34 UAH order
- Heparin-Novopharm 5000 MO/ml 5 ml No. 5 solution Novofarm-Biosintez TOV, Novograd-Volinsky, Ukraine
256 UAH order
PaniPharmacy
- Heparin ointment Heparin ointment 25g tube Ukraine, Zhytomyr FF LLC
60 UAH.order
- Heparin gel Heparin gel 30g Ukraine, Darnitsa ChAO
68 UAH order
- Heparin bottle Heparin solution d/in. 5000U/ml 5ml vial. №5 Ukraine, Pharmstandard-Biolek
166 UAH order
- Heparin solution d/in. 25000U/ml 5ml No.1 Ukraine, INDAR
39 UAH order
- Heparin bottle Heparin-Novopharm solution d/in 5000 MO bottle. 5ml. No.5 Ukraine, Novofarm-Biosintez LLC
268 UAH order
show more