- How does ascites manifest?
- What causes fluid to accumulate?
- Risk factors for ascites
- Classification and types of ascites
- How to treat ascites?
- Clinical case
- What causes ascites to develop in cancer?
- Features of the treatment of ascites in cancer patients
- Conservative therapy
- Surgical treatment of ascites
- Methods for diagnosing ascites
- Possible complications of ascites
- Forecast
- Prevention of ascites
- Prices
Euroonco doctors specialize in working with patients with ascites. Features of our treatment of ascites:
- We provide comprehensive treatment. During laparocentesis (a puncture of the abdominal wall to remove fluid from the abdomen), we install temporary or permanent peritoneal catheters, as well as port systems. This allows the patient not to be limited in movement.
- If this is indicated, the patient is prescribed a special diet with limited water and salt load.
- If ascites occurs due to cancer, chemotherapy may be performed. Thanks to this, we achieve improvement in the condition of patients with ascites in advanced ovarian and colon cancer.
- Intracavitary chemotherapy is effective. After the fluid is removed, a chemotherapy drug is injected into the abdominal cavity. In approximately half of the cases, repeated evacuation of the fluid is not required for at least 2 months.
When a patient with cancer and ascites switches to complex therapy, laparocentesis is required 2–3 times less often than usual.
How does ascites manifest?
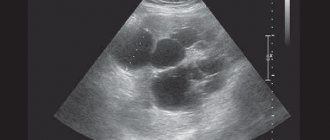
If there is a small amount of fluid in the abdominal cavity, this does not manifest itself in any way. In addition, this is normal: the human body produces and absorbs approximately 1.5 liters of fluid in the abdominal cavity per day. At the initial stage of ascites, patients have no special complaints, and the pathological condition can only be detected during an ultrasound examination.
When ascites progresses, a person feels heaviness in the abdomen and dull aching pain in the lower part. Subsequently, difficulty breathing, indigestion (nausea, belching, stool disorders) and urination problems occur. In the most severe forms, ascites significantly worsens health, discomfort appears in the abdomen, shortness of breath occurs, early satiety occurs, an umbilical hernia forms, and swelling of the lower extremities appears.
5–10 liters of fluid, and sometimes 20 liters, can accumulate in the abdominal cavity. Because of this, internal organs are strongly compressed, intra-abdominal pressure increases, and the diaphragm is pushed into the chest cavity. This entails severe difficulty breathing. Due to the fact that resistance to blood flow increases in the abdominal organs, heart failure occurs. The consequence of long-term ascites is a violation of the drainage of the lymphatic system. Because of this, there is also a violation of lymphatic drainage in the lower extremities and, as a result, their swelling. There may also be a backflow of lymph into the internal organs. As a result, cancer cells enter healthy organs from the affected lymph nodes. This can trigger the development of metastases in the liver, stomach, pancreas and other organs.
When there is more than one liter of fluid in the abdominal cavity, ascites can be noticed during a routine examination: the abdomen is enlarged or deformed, in an upright position it looks saggy, in a supine position the abdomen is flattened, the sides look swollen (the so-called “frog belly”). In thin patients, the navel often protrudes. A person may also experience hydrothorax, the presence of fluid in the pleural cavity. Typically, this condition develops in patients with congestive heart failure with long-standing ascites.
Mild or moderate ascites develops in 15 to 50 percent of patients in the early stages of cancer. In later stages, severe ascites occurs in 7 to 15 percent of patients.
In patients with advanced advanced cancer, exudative pleurisy is most common.
Book a consultation 24 hours a day
+7+7+78
Diagnosis of the disease: independent and medical
The first sign of hydrocele development is swelling in the scrotum area. It can spread to only one testicle, or it can be bilateral. On palpation you may feel pain. Discomfort also occurs from wearing tight underwear or tight trousers. With chronic hydrocele, there is no pain, no redness, no tissue hyperthermia. However, even in this case, an adult man feels severe discomfort, especially when walking.
Although hydrocele is not a life-threatening disease, it can mask other serious pathologies - tumors, infections, etc. If the dropsy itself becomes infected, this requires surgical intervention and quite long-term therapy.
In our clinic "SANMEDEXPERT" hydrocele is diagnosed in the following ways:
- Survey - the specialist will ask you how long ago you noticed a swelling in the scrotum area, whether there were similar symptoms before, whether treatment was carried out;
- Lifestyle assessment - you will have to answer questions from a specialist about whether you have had any injuries or surgeries in this area of the body, what pathologies (in particular, inflammatory ones) you have suffered from before, whether you could have damaged the scrotum during shaving and other household manipulations;
- Studying your family history - tell the specialist if this happened to your closest relatives (father, brother);
- Physical examination - an objective examination of the genital organs and scrotum with palpation, during which a specialist will determine the location and extent of swelling;
- Ultrasound examination - as a result of this diagnostic procedure, our specialist will identify the specifics of the problem and the reason for the enlargement of the organ, evaluate the characteristics of the contents and differentiate hydrocele from a tumor;
- Diaphanoscopy - this event will be required if the ultrasound does not give an objective result; its essence lies in pointing a special light device at the enlarged half of the scrotum and assessing the shade of the liquid accumulating in it;
Hydrocele treatment should not be delayed. The only option for adequate treatment of the pathology today is surgery. When performed correctly, it provides a prolonged effect and guarantees protection against relapses.
What causes fluid to accumulate?
With ascites, a pathological accumulation of fluid occurs in the abdominal cavity. The fact is that in some diseases the regulation of water-salt metabolism and normal fluid circulation in the abdominal cavity are disrupted. The reason may be:
- Oncological diseases: secondary peritoneal carcinomatosis, lymphoma and leukemia, metastases in the hepatic portal area, primary mesothelioma.
- Diseases of the liver and its vessels: liver cancer, portal hypertension, liver cirrhosis, veno-occlusive disease, Budd-Chiari disease.
- Peritonitis (inflammation of the peritoneum) of various origins: pancreatic, fungal, parasitic, tuberculous.
- Congestive heart failure, constrictive pericarditis.
- Other diseases: ovarian tumors and cysts (Meigs syndrome), pancreatic cyst, Whipple's disease, sarcoidosis, systemic lupus erythematosus, myxedema.
Euroonco treats ascites of various origins. But since our main work is related to the treatment of malignant neoplasms, a significant part of our patients are cancer patients.
Causes of pathology in adults
In many cases, pathology develops as a symptom of a number of diseases, including:
- Portal hypertension;
- Cirrhosis;
- Hepatitis;
- Thrombosis of the liver veins.
It is possible that the cause of the pathology is blood oncology, as well as pathologies whose nature has nothing in common with the tumor.
Heart failure can also cause pathology. Problems associated with lymph circulation and the activity of organs such as the thyroid gland and kidneys can also cause pathology.
Protein deficiency
Classification and types of ascites
Classically, depending on the level of protein in ascitic fluid, ascites is divided into exudative (25 g/l or more) and transudative (<25 g/l). This allows us to indirectly judge the reasons. Currently, a more accurate indicator is used - the serum albumin-ascitic albumin gradient (SAAG):
- When SAAG is more than 1.1, the cause of ascites is usually pathologies such as cirrhosis, congestive heart failure, and Budd-Chiari disease. They are associated with increased pressure in the portal vein.
- If SAAG is less than 1.1, it can be assumed that the accumulation of fluid in the abdomen is caused by pancreatitis or cancer.
According to the clinical course, the following types of ascites are distinguished:
- Depending on the severity of the course: 1 degree. There are no clinical manifestations; the diagnosis is established by ultrasound (determining the level of free fluid in the abdominal cavity).
- 2nd degree. Slight visual enlargement of the abdomen.
- 3rd degree. Significant visual enlargement of the abdomen.
- Resistant to diuretics: treatment with diuretics in combination with a diet in which sodium chloride intake is limited to less than 2 g per day is ineffective (no effect after 1 week of therapy).
Diet
Provides for reducing fluid intake, as well as salt, due to the fact that it retains fluid in the body. Doctors recommend the Avicenna diet. Such a diet for ascites involves almost complete abstinence from fatty foods, eating nuts in large quantities, and abandoning fresh fruits in favor of dry ones.
Also, liquid food (borscht, soup) should be replaced with broth with additives in the form of celery, parsley, fennel. The diet for ascites does not regulate how much meat the patient should eat, but all meat should be lean (chicken, turkey, rabbit).
How to treat ascites?
There are several main methods for treating ascites in patients with cancer:
- conservative therapy (aldosterone antagonists, diuretics) - aimed at normalizing water-salt metabolism and reducing the formation of fluid in the abdominal cavity;
- laparocentesis - puncture of the abdominal wall under ultrasound control; used not only for removing fluid, but also for installing drainage, which will serve for long-term removal of fluid;
- palliative surgical operations - peritoneovenous shunt, omentohepatophrenopexy, deperitonization of the abdominal walls and others.
Traditional methods of treating ascites caused by cancer do not have proven effectiveness and safety, therefore they are not used at Euroonko.
If you come to our clinic with ascites due to cancer, we recommend getting a second opinion regarding the treatment of the underlying disease from our clinical oncologists and chemotherapists.
Clinical case
A 59-year-old woman, Sh., was diagnosed with stage IV ovarian cancer (adenocarcinoma), ascites, and chronic pain syndrome 2 b according to the ShVO. The patient noticed an increase in the abdomen up to 120 cm in circumference, difficulty breathing, and weight loss. Specific treatment at the place of residence was denied. According to the patient, she was “sent home to die.” Read more…
A 59-year-old woman, Sh., was diagnosed with stage IV ovarian cancer (adenocarcinoma), ascites, and chronic pain syndrome 2 b according to the ShVO.
The patient noticed an increase in the abdomen up to 120 cm in circumference, difficulty breathing, and weight loss. Specific treatment at the place of residence was denied. According to the patient, she was “sent home to die.” Patient Sh. was urgently hospitalized in the specialized department of Euroonko, after active symptomatic therapy aimed at normalizing blood counts and restoring water and electrolyte balance, a peritoneal port was installed. Resolution of ascites was carried out under the control of plasma protein levels. The use of peritoneal ports allows for the removal of ascitic fluid in fractional doses, which ultimately eliminates the occurrence of serious complications in the form of hemorrhagic syndrome associated with hemodilution and coagulopathy as a result of massive entry of ascitic contents into the venous bed.
After stabilization of the general condition, against the background of nutritional support, antiemetic and antisecretory therapy, patient Sh. received specific chemotherapy treatment with good effect. Upon resolution of ascites in the presence of a peritoneal port, intra-abdominal chemotherapy became possible.
Six months after the described hospitalization, the patient returned to her usual lifestyle and continues to receive systemic treatment on an outpatient basis under the supervision of a team of Euroonco specialists. The response to treatment is regarded as positive in the absence of ascites and a total reduction in the size of the lesions by more than 70%. Combined treatment in the format of systemic and local (intra-abdominal) therapy with implantation of a port system is the optimal treatment regimen for this group of patients. In the practice of Euroonco doctors, such cases occur on a regular basis. Hide
In what cases is surgery needed for hydrocele?
Surgery for hydrocele is a complex but necessary stage of treatment. It is needed:
- With a significant amount of dropsy, causing inconvenience and cosmetic discomfort
- For pain syndrome
- In case of infertility or pathological changes in the spermogram
- With a rapid increase in the volume of dropsy
By contacting me with a problem such as hydrocele, you can be sure that you will receive the most effective and safe treatment using modern technologies.
What causes ascites to develop in cancer?
The most common cancers that cause fluid accumulation are:
- ovarian cancer (in 25–30 percent of patients),
- mammary cancer,
- uterine cancer,
- stomach cancer,
- colon cancer.
The accumulation of fluid in the abdominal cavity during cancer occurs due to the fact that the peritoneum (the membrane lining the inside of the abdominal wall and covering the organs located in it) is affected. Tumor cells settle on its parietal and visceral layers, resulting in disruption of lymphatic drainage. This causes deterioration in fluid absorption. Typically caused by tumors of the gastrointestinal tract and ascites in ovarian cancer.
When a tumor or metastases forms in the liver, the cause of ascites is different: the venous system of the liver is compressed and the natural venous outflow from the intestine is disrupted. This type of ascites develops quickly and usually lasts longer and is more severe. 15 percent of cases of fluid accumulation in the abdominal cavity due to cancer occur in this particular form.
Abdominal lymphoma causes ascites through blockage and effusion (leakage) of lymph from the intra-abdominal lymph ducts.
Features of the treatment of ascites in cancer patients
In hospitals that do not specialize in the treatment of cancer, the approach to patients with ascites may be ineffective due to the characteristics of this condition. For example, the main treatment may be the use of diuretics, aldosterone antagonists, and dietary changes to limit water and salt load. The effectiveness of this approach for reducing portal hypertension is relative; in cancer patients, ascites is caused by peritoneal carcinomatosis. Therefore, conservative therapy cannot be the main treatment method in such patients.
Typically, fluid is removed from the abdomen using laparocentesis (abdominal paracentesis). This is a surgical procedure that is performed by a surgeon and an anesthesiologist-resuscitator.
Conservative therapy
Conservative therapy is used in the treatment of small and moderate ascites. In other words, if there are no tiring and debilitating symptoms: pain, rapid breathing (tachypnea), etc. Up to 65% of patients have an improvement in their condition when treated with diuretics - this way you can remove up to 1 liter of fluid per day.
In the later stages of cancer, reducing salt and water intake can reduce quality of life. Therefore, at Euroonko such diet correction is rarely prescribed.
Book a consultation 24 hours a day
+7+7+78
Surgical treatment of ascites
Ascites in cancer must be treated surgically when it:
- Refractory, that is, ascites that cannot be treated conservatively.
- Large ascites, that is, if it is necessary to remove up to 6–10 liters of fluid at a time (this difficult procedure is carried out for strict medical reasons).
- Giant ascites. In this case, a combined operation is needed, which includes removing a large volume of fluid (up to 5–7 liters) on the first day and removing the remaining volume at a rate of no more than 1 liter per day for 7–10 days.
In the classic version, laparocentesis is performed on an empty bladder, the patient sits down, and the seriously ill person is placed on his side.
It is dangerous to perform laparocentesis without observing the rules of asepsis and antisepsis. Therefore, the release of fluid is carried out only in a specialized medical institution with a license to perform surgical interventions and with a hospital. If the patient is in serious condition, it is difficult for him to move, an ambulance team is called for him.
First, local anesthesia is performed, then, under ultrasound guidance, a puncture is made with a trocar (an instrument in the form of a thin tube with a sharp end) along the midline of the abdomen or along the line connecting the navel to the iliac crest. Usually no more than 5–6 liters of liquid are removed at a time. To prevent blood pressure from dropping sharply and vascular collapse, the fluid is released slowly.
In accordance with the classical technique, the patient needs to lie for several hours on the side free from the puncture. If at this time a small amount of liquid continues to be released, then a reservoir is applied, which is removed after a day or two.
If it is necessary to remove a large amount of liquid, then a loss of protein and salts occurs, which becomes the cause of protein deficiency. To prevent such a complication, the patient is given albumin. With repeated puncture, another complication may arise - fusion of the omentum (part of the peritoneum) or intestine with the anterior wall of the abdomen. Because of this, intestinal function deteriorates significantly, and during subsequent punctures serious complications can develop.
With the modern approach to laparocentesis, fluid drainage occurs primarily through a permanent peritoneal catheter. At the same time, the deficit in circulating blood volume is replaced by plasma expanders (from the English plasma expander - increasing plasma volume). Typically, 10–20% albumin solutions are used for this. In some cases, aminosteril, polyglucin, rheopolyglucin (dextran-40), hemacell and new starch-based preparations (refortan, stabizol, HAES-steril) can be used instead of albumin. This alternative only helps to compensate for fluid deficiency in the blood, but these drugs do not affect protein deficiency.
Some patients with ascites undergo omentohepatophrenopexy. This is a laparoscopic operation in which the omentum is sutured to areas of the surface of the liver and diaphragm. Due to the fact that contact occurs between the omentum and the liver, conditions appear for the absorption of ascitic fluid by nearby tissues. If the patient has peritoneal carcinomatosis, surgery is performed to a limited extent. Typically, in such patients, omentohepatophrenopexy becomes part of palliative treatment.
Questions about the article
Ruslan
November 29, 2021 at 06:45 pm
Hello, Bergman's surgery was performed on November 23, 2021. Hydrocele on the left 75 ml. The stitches haven't been removed yet. It doesn’t hurt, but sometimes it’s a little painful. Is it possible to masturbate on the 7th day after surgery?
Anton Evgenievich Rotov
November 30, 2021 at 08:58
I think it's already possible
Konstantin
October 24, 2021 at 08:38
2 weeks ago I had a hydrocele operation according to Bergman. After the operation I had a fever for 2 weeks. On the 2nd day after the operation, the doctor examined the inside after removing the drainage, and said that there was nothing there, no infection either. The temperature was not high, up to 38. When taking painkillers, the temperature dropped. And every day the temperature became lower, and now it has passed. Is this a normal reaction of the body? And now when I touch the testicle, it is somehow large and very hard. There is also pain in the lower abdomen, on the side of the operated testicle, what could it be?
Anton Evgenievich Rotov
October 24, 2021 at 08:39
What you are describing is probably due to post-operative swelling that is more severe than normal due to inflammation. As a rule, the swelling completely disappears within 2-3 months. If in doubt, do an ultrasound of the scrotum
Vyacheslav
September 23, 2021 at 08:09 pm
Hello, on September 7, 2021, Bergman had an operation to remove a hydrocele. As of September 22, 2021, there are a number of problems that concern me, although I have been to the local doctor, I want to make sure that everything is in order. The first problem: somewhere around the 18th, the seam began to bleed from the edges, at the moment there is a “detachment” of the skin from above, but it does not cause any painful sensations (the local surgeon said that the seam had come apart, there was no need to stitch it up, he advised treating it twice a day with Chlorhexidine ) it’s already the 22nd, in my opinion, the seam divergence has not decreased, and I don’t understand how it will heal if it “peeled off”; there is still some liquid in the formed depression due to the seam divergence. Please tell me how normal this is and should I panic? Enough time has already passed, but the seam still doesn’t fit. The second question is how much is it acceptable to enlarge the scrotum after surgery, at the moment, compared to what was, of course, much less (there was 200 ml of water), but now there is swelling, I can hardly feel the testicle
Anton Evgenievich Rotov
September 23, 2021 at 08:18 pm
I am afraid that it will not be correct to assess the condition of the wound in absentia and draw any conclusions. Therefore, I will speak in general terms. Incomplete healing of the wound at this time is acceptable, although usually the wound is already closed by this time. Postoperative swelling of the soft tissues of the scrotum can persist for up to 3 months. If you still have doubts about the course of the postoperative period and you are not sure about the attending physician, then it is better to see another specialist
Peter
June 15, 2021 at 04:38 pm
A month ago I had a Winkelmann operation for hydrocele. The stitches have disappeared, the swelling is still there, but smaller, the wounds are also still present, but there is no bleeding from them. Can I already have sex or is it better to abstain for now?
Anton Evgenievich Rotov
June 15, 2021 at 04:39 pm
Sexual activity can be resumed
Eugene
March 4, 2021 at 12:18 pm
Thank you very much for the answer!
Methods for diagnosing ascites
If more than 500 ml of fluid has accumulated in the abdomen, symptoms of ascites can be identified by a doctor during an examination. Ultrasound is used to confirm the diagnosis. Sometimes ascites is discovered accidentally during an ultrasound or computed tomography scan of the abdomen, which is performed for another reason.
Euroonco operates a comprehensive gastrointestinal screening program, which helps assess the condition of the digestive system. It, in particular, includes an ultrasound of the abdominal cavity with determination of the level of free fluid. This helps diagnose ascites at an early stage.
It is important not only to identify fluid in the abdominal cavity, but also to understand the reasons for its accumulation - this helps to assess the prognosis and prescribe effective treatment. In most cases, the examination includes the following laboratory tests:
- Biochemical blood test - complete biochemical panel. It helps assess the condition and function of the liver, kidneys, and electrolyte levels.
- Blood clotting study.
- Study of ascitic fluid obtained during laparocentesis. For analysis you need a little of it - usually 20 cm³, less than a tablespoon. It examines the level of red and white blood cells, total protein, albumin, amylase, glucose, and examines for pathogenic microorganisms. A cytological examination is performed to help identify cancer cells.
Symptoms
With local dropsy, symptoms depend on the location of the swelling. With severe swelling of the eyelids, the field of vision narrows. Swelling of the feet does not allow wearing usual shoes. Dropsy of the brain leads to disturbances of consciousness, and hydrocele manifests itself as nagging pain in the testicle. Neurological edema is accompanied by dysfunction of the limbs and pain due to compression of the nerve endings.
Systemic dropsy is manifested by the following symptoms:
- dryness and swelling of the skin;
- fluctuations in weight during the day - typical for dropsy in pregnancy;
- a feeling of thirst due to blood thickening due to the effusion of fluid into the interstitial space;
- “pit” symptom: when pressing with a finger, a pit remains in the area of edema;
- the appearance of shortness of breath;
- fast fatiguability.
The absence of acute pain with dropsy masks the danger of the condition. Blood thickening increases the risk of thrombosis, which can lead to acute hypoxia and shock.
In pregnant women, whose internal edema appears only after retention of 3-4 liters of fluid, swelling of the placenta simultaneously occurs, due to which the umbilical cord vessels are compressed and oxygen starvation of the fetus develops.
Diagnostics
Diagnosis of dropsy is not difficult and is based on clinical manifestations and medical history.
If edema is detected, additional studies are carried out to identify the cause of dropsy.
Laboratory methods used:
- general urinalysis - determines the concentrating ability of the kidneys and the integrity of the glomerular apparatus;
- special tests: according to Nechiporenko, Zimnitsky, Addis-Kakovsky - they can detect kidney damage;
- general blood test - allows you to identify inflammatory and allergic processes in the body;
- biochemical tests - determine liver function and the amount of protein in the blood plasma;
- Hormone tests are done to confirm or refute the diagnosis of a tumor of the adrenal gland, pituitary gland, as well as hypofunction of the thyroid gland.
Possible complications of ascites
If a lot of fluid accumulates in the abdominal cavity, the functioning of the internal organs is disrupted, difficulties arise during breathing, as the mobility of the diaphragm is limited, and effusion forms in the pleural cavity.
With increased pressure in the portal vein, bacteria from the intestine can spontaneously penetrate the ascitic fluid and cause spontaneous bacterial peritonitis.
In rare cases, a very serious complication develops - hepatorenal syndrome. This term refers to impaired renal function with severe liver damage, up to severe renal failure. The exact mechanism of development of this condition is unknown, but it is believed to occur due to impaired renal blood flow, excessive use of diuretics and intravenous contrast agents.
Forecast
Ascites in cancer significantly worsens the prognosis. From the moment of diagnosis, only half of the patients remain alive within 1–4 months. The average life expectancy is from 20 to 58 weeks. Timely treatment in a clinic that specializes in working with such patients helps improve survival. With ascites caused by liver cirrhosis, when there is no cancer, the prognosis is better. And a patient whose accumulation of fluid in the abdominal cavity was caused by chronic heart failure, with appropriate treatment, can live for many more years.
Causes
The basis for the development of the disease is pathology: during the normal functioning of the peritoneal cavity, no significant amount of liquid mass is discharged. It is only insignificant, just to avoid adhesions from sliding intestinal loops. The liquid released for this purpose constantly flows back.
When the usual operation of this mechanism is disrupted, the function of secretion of the liquid mass is destabilized, as well as the function of its outflow. The consequence of such destabilization is the accumulation of excess liquid mass inside the abdomen.