Benefits for the body
Taurine should be taken by those who want to live longer. This substance has an antioxidant effect, inhibits the effects of free radicals, and prevents their negative effects on the body.
Note! The amino acid is produced by the human body in small quantities. Therefore, it is advisable to additionally obtain this nutrient externally from food or nutritional supplements.
With a lack of taurine, problems with the liver, heart, vision arise, and the functioning of the brain deteriorates. If the amino acid is normal, then it produces the following effect:
- improves brain function, tissue metabolism, digestion;
- normalizes the metabolism of fats, calcium and potassium, energy balance;
- relieves seizures, making taurine effective for epilepsy;
- stimulates the production of gamma-aminobutyric acid;
- regulates the release of prolactin and adrenaline;
- increases blood flow;
- removes bad cholesterol and excess water from the body;
- reduces appetite;
- increases endurance during physical activity;
- prevents retinal diseases and visual impairment, improves microcirculation in the conjunctiva.
Now Foods, Taurine, Double Strength, 1000 mg, 100 Vegetarian Capsules
★★★★★
635 rub.
More details
Taurine is useful for diabetes, as it increases tissue sensitivity to insulin and reduces the risk of vascular complications. This substance also lowers blood pressure and produces a vasodilating effect.
Interesting! In diabetes, taurine does not affect blood sugar levels. However, it reduces insulin resistance.
In case of liver diseases, taurine increases blood flow, normalizes metabolism, and launches recovery processes. It has a nutrient and hepatoprotective effect, helps with alcohol intoxication.
The video describes this nutrient in more detail:
Taurin (doctor Elena Seregevna Golesheva)
The feasibility of using taurine in the treatment of non-alcoholic fatty liver disease
In recent years, non-alcoholic fatty liver disease (NAFLD) has been considered as an integral component of metabolic syndrome (MS). MS is a complex of interrelated factors, including insulin resistance, impaired carbohydrate metabolism, abdominal-visceral obesity, arterial hypertension, atherogenic dyslipidemia, etc. The liver in MS is one of the main target organs [1, 2]. According to a number of sources, the incidence of liver pathology in patients with MS ranges from 37 to 64%.
NAFLD: etiology, pathogenesis, goals of therapy
The etiological factors for the development of NAFLD include metabolic disorders and endocrinopathies (insulin resistance or diabetes, obesity, gout, hyperlipidemia, hypothyroidism, hyperthyroidism, Cushing's syndrome, etc.); violation of the processes of digestion and absorption (pathology of the pancreas, small intestine, malabsorption syndrome, excess nutrition, fasting, parenteral nutrition, bacterial overgrowth syndrome in the intestine); the effect of drugs, chemical substances, phytotoxins, fungal toxins; infections; anemia, cardiovascular and respiratory failure, etc. [3, 4]. NAFLD has several stages of development: from simple steatosis to steatohepatitis, fibrosis and cirrhosis of the liver. Symptoms characteristic of liver diseases are absent in most patients, only some of them note minor discomfort or pain in the right upper quadrant of the abdomen [1].
In the majority of patients, NAFLD progresses favorably, without significant clinical and morphological changes. Since liver puncture is not always possible, the true prevalence of this disease in the population is unknown. More often, patients turn to doctors for other reasons, for example, about arterial hypertension (AH), cholelithiasis, coronary heart disease (CHD), peripheral vascular diseases, etc. [5, 6].
In this regard, treatment is prescribed only to patients with a high risk of NAFLD progression or in the presence of pronounced changes in liver biochemical parameters (increased activity of alanine aminotransaminase (ALT) and aspartate aminotransaminase (AST) in the blood by 2-3 times or more). MetS causes an extremely high risk of developing type 2 diabetes, coronary artery disease and other diseases associated with atherosclerosis [7–10], as well as fatty liver disease [2]. Among the mechanisms of liver damage, it is necessary to highlight a violation of the synthesis and excretion of bile in hepatocytes, activation of lipid peroxidation (LPO), and inhibition of the activity of the reticuloendothelial system of the liver.
The literature provides numerous data on possible pathogenetic mechanisms of liver damage in MS, as well as on the role of the liver in the development and progression of MS. The liver is the only organ where bile acids are synthesized. The accumulation of free fatty acids in the liver leads to impaired permeability of cell membranes, including for glucose, and impaired utilization of glucose by hepatocytes, which contributes to increased tissue resistance to insulin and the maintenance of hyperglycemia. Under conditions of insulin resistance, lipids accumulate in the liver and synthesize large amounts of very low-density lipoproteins (VLDL), which are quickly modified into low-density lipoproteins (LDL) and, oxidized by free radicals, are a leading factor in the development of atherosclerosis [7, 10, 11] .
An increase in the concentration of cholesterol (CH) in cells leads to changes in the composition, physical properties and functions of cell membranes: receptor-mediated endocytosis, reactivity of membrane-bound enzymes, membrane permeability to ions and metabolites. Maintaining a certain concentration of cholesterol in plasma membranes ensures the necessary constancy of the physical properties and physical state of the membrane bilayer of a normally functioning cell, which underlies cholesterol homeostasis and is maintained by the balance of cholesterol intake and removal from the body. Thus, a vicious circle is formed: constant hyperinsulinemia depletes the secretory apparatus of beta cells of the pancreas, which first leads to high fasting glycemia, decreased glucose tolerance and subsequently to type 2 diabetes [12], hyperinsulinemia suppresses the breakdown of fats, which contributes to the progression of obesity. In turn, adipocytes of visceral adipose tissue secrete free fatty acids, which enter directly into the portal vein of the liver [13].
Recently, many works have appeared devoted to the study of the effect of hyperglycemia on the metabolism of nitric oxide as the main link in the mechanism of the pathogenesis of endothelial dysfunction. With chronic hyperglycemia, there is a local decrease in the rate of nitric oxide synthesis in the vascular endothelium, which contributes to the occurrence of ischemia [14]. An increase in oxygen consumption by hepatocytes is accompanied by the formation of active radicals and an increase in the reaction of lipid peroxidation (LPO). The substrate for LPO is free fatty acids, highly reactive compounds, the accumulation of which stimulates the development of inflammatory reactions [15].
Impaired metabolism and absorption of bile acids and excessive absorption of lithocholic acid lead to intrahepatic cholestasis as a result of damage to cholangiocytes by toxic bile acids, hepatic dyscholia and disruption of the chemical composition of bile. Primary bile acids - cholic and chenodeoxycholic - are synthesized in the liver from cholesterol, conjugated with glycine or taurine and secreted as part of bile. Secondary bile acids, including deoxycholic and lithocholic, are formed from primary bile acids in the colon by bacteria. Ursodeoxycholic acid and a number of other secondary bile acids are formed in negligible quantities. In chronic cholestasis, an increased amount of these acids is detected. Normally, the ratio of the amount of bile acids conjugated to glycine and taurine is 3:1. The sulfur-containing amino acid taurine forms conjugates with bile acids in the liver. The resulting conjugates, for example taurocholic and taurodeoxycholic acids, are part of bile and, being surfactants, contribute to the emulsification of fats in the intestine. Recently, it has been found that taurine helps improve energy and metabolic processes, normalizes the function of cell membranes, and stimulates reparative processes in dystrophic diseases.
The progression of steatohepatitis depends on the level of activity of the pathological process in the liver. Non-alcoholic steatohepatitis is characterized by a benign and asymptomatic course. However, histological changes are found in almost half of patients, and 20% develop cirrhosis. In this regard, all efforts aimed at treating patients with non-alcoholic steatohepatitis are considered as prevention of liver cirrhosis. This goal determines the main goals of therapy: normalization of body weight through diet and physical activity; withdrawal of hepatotoxic drugs; normalization of carbohydrate, lipid and purine metabolism parameters; an increase in the content in hepatocytes of amino acids necessary for the synthesis of apoproteins and coenzymes for the synthesis of VLDL; reduction of endotoxemia; normalization of the activity of lipid peroxidation processes; removal of toxic metabolites; inhibition of inflammation in liver tissue, etc.
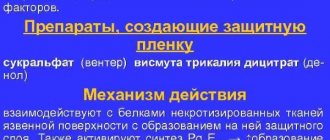
The use of taurine in the treatment of NAFLD and MS
The basic method in the treatment of NAFLD is the use of hepatoprotectors. The main mechanisms of action of hepatoprotectors: increasing the neutralizing function of hepatocytes as a result of increasing the reserves of glutathione, taurine, sulfates, increasing the activity of enzymes involved in the oxidation of xenobiotics; stabilization and repair of cell membrane structures as a result of stopping lipid peroxidation reactions and binding oxidation products; stimulation of the oxidation of fatty acids and acetate; increased synthesis and content of glycogen in liver cells; restoration of transport systems for bile components.
The search for effective drugs with lipid-lowering properties for the treatment of metabolic disorders continues. Taurine-based drugs have proven themselves in the complex treatment of patients with CVD and type 2 diabetes. Taurine is non-toxic, does not bind to proteins, has an antioxidant, detoxifying and osmoregulatory effect, and helps reduce the synthesis of nitric oxide in macrophages [16]. A positive effect of taurine-based drugs on the lipid spectrum of the blood was noted. Taurine is a substance that is not metabolized by the liver and is directly included in metabolism. Combining with cholic acid, taurine forms so-called paired bile acids and is directly involved in the absorption of fats and fat-soluble vitamins, and also promotes the degradation of cholesterol [17]. Thus, taurine can be used to correct and prevent metabolic disorders in the treatment of NAFLD.
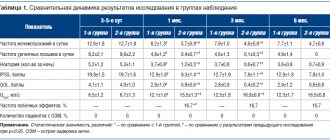
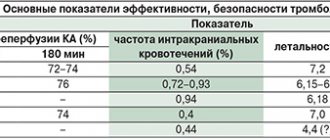
A double-blind, placebo-controlled comparative study was conducted at the Central Research Institute of Gastroenterology (Moscow), which assessed the clinical effectiveness of taurine in patients with NAFLD and type 2 diabetes (mild course, impaired glucose tolerance) in comparison with placebo. The study included 40 patients who met the inclusion criteria. Duration and regimen of treatment: patients received the drug Dibikor (company) at a dose of 0.5 g 2 times a day 20 minutes before meals for 3 months. Concomitant therapy: patients with type 2 diabetes (impaired glucose tolerance) continued to take the therapy prescribed by the endocrinologist: metformin hydrochloride 1000 mg per day; patients with coronary artery disease, hypertension, and hypertension took amlodipine 5 mg per day and enalapril maleate 20 mg per day. The criteria for effectiveness were the dynamics of clinical and biochemical blood parameters (total bilirubin, ALT, AST, alkaline phosphatase (ALP), gamma-glutamyl transpeptidase (GGTP), glucose), lipid spectrum (cholesterol, LDL cholesterol, HDL cholesterol, TG), weight loss . After the end of the study, in order to compare the results, the patients were divided into 2 groups: the first group - patients who received taurine (Dibikor), the second group - patients who received placebo. To process the data, the standard statistical package Statistica 6.0 was used using nonparametric estimation methods (Wilcoxon-Mann-Whitney test). The critical level of significance in the study was set to ≤ 0.05.
As a result of the study, the following data were obtained: drug tolerability was assessed as good in 16 patients (50%) taking taurine (Dibikor), as satisfactory in 4 patients (12.5%), no unsatisfactory assessment was noted. Among patients taking placebo, good tolerability was noted in 10 patients (31.25%), satisfactory in 2 (6.25%), and no unsatisfactory assessment was recorded. Based on these results, it can be concluded that there was no significant difference between the drug and placebo in terms of tolerability. During treatment, 20 patients noted an improvement in their general well-being (of which 18 took Dibikor and 2 took placebo): a decrease in fatigue – 11 patients; reduction in the frequency of attacks of shortness of breath - 3 patients, attacks of angina - 4 patients; could not characterize changes in the well-being of 2 patients. During the initial examination, excess body weight was detected in 50% of patients. Patients receiving taurine noted faster weight loss - on average by 1 kg per month, which was confirmed by objective data.
Analysis of biochemical blood parameters before treatment showed an increase in ALT and AST levels. At the same time, the ALT concentration was higher than the AST concentration. Patients in the first group had a significantly more pronounced lipid-lowering effect (decrease in cholesterol levels) of therapy than in patients receiving placebo (the levels of cholesterol and LDL increased insignificantly, the reason for the significant increase in HDL is not yet clear). TG levels did not significantly decrease in patients taking Dibicor. While taking taurine, the levels of alkaline phosphatase (ALP), cholesterol, LDL, and glucose decreased, and in patients taking placebo, they increased (Tables 1, 2). It is important to note that ALT is a more specific marker of hepatocyte damage than AST, due to its predominant localization in the liver parenchyma. Another specific liver enzyme is gamma-glutamyl transpeptidase (GGTP), the level of which was also elevated in 35 patients (87.5%). An increase in bilirubin levels was detected in 5 patients (12.5%), the maximum value did not exceed 41.1 µmol/l. Lipid spectrum indicators (total lipid content, LDL, TG) in the examined patients were increased. Taking Dibikor statistically significantly improved the indicators of bilirubin, AST, ALT, cholesterol, fibrinogen, weight, body mass index (BMI) (Table 3, 4).
Conclusion
As a result of the study, the following conclusions were made: taking the drug Dibicor is well tolerated by patients, has a lipid-lowering and hepatoprotective effect, helps reduce body weight and improve the well-being of patients; the use of taurine in NAFLD leads to an improvement in carbohydrate and fat metabolism and can be recommended for the treatment and prevention of NAFLD. Thus, the use of taurine-based drugs in the treatment of MS and NAFLD is advisable not only at the stage of liver tissue damage or carbohydrate metabolism disorders confirmed by laboratory data, but also to prevent their development.
Indications for use
Taurine is used in cardiology as well as ophthalmology. Preparations based on this substance can be taken by healthy people, athletes and vegetarians. But the medicine is most useful for elderly patients, since their amino acid production gradually decreases and the risk of age-related diseases increases.
Indications for use of taurine:
- cardiovascular failure;
- hypertension, arterial hypertension;
- epilepsy;
- nervousness, insomnia;
- diabetes mellitus type 1 and 2;
- diabetic retinopathy;
- cataracts, age-related visual impairment;
- liver diseases, namely fatty hepatosis, hepatitis;
- drug intoxication in the treatment of heart disease.
The supplement is prescribed as an adjuvant to the main therapy.
Attention! The amino acid is sometimes used in the treatment of cancer. According to official studies, in cancer patients the level of taurine is minimal, and chemical drugs reduce it even more.
Are there possible harmful effects?
Quite often you can hear opinions about the negative effects of taurine on the body. In 2008, a scientific study found that the amount of this amino acid used in drinks did not cause side effects.11 The danger lies in the rest of the ingredients in these supplements.
Caffeine and other stimulants act synergistically with taurine. This combination of components, a real “energy mixture,” may be harmful to people with problems with the heart or nervous system. In any case, before using this or that product, you should consult a specialist. In cases where there are disturbances in the functioning of the heart, rapid excitability, and sleep problems, it is necessary to abandon the use of such energy supplements.
It is worth noting that an overdose is practically impossible, since the excess content of this amino acid is excreted in the urine. A 2008 study confirms this—athletes who took taurine for a week had a 13-fold increase in plasma levels of taurine, but no increase in muscle concentrations.12
Contraindications, precautions
The main contraindications to taking taurine are individual intolerance and children under 18 years of age. However, the amino acid can be harmful if it is also used for the following diseases:
- kidney disease;
- gastritis with high acidity, stomach ulcer;
- diarrhea;
- cholecystitis, cholelithiasis.
Relative contraindications are pregnancy and breastfeeding.
Note! Despite the fact that taurine does not have a toxic effect on the fetus, a supplement based on this substance should be taken under the supervision of a doctor when carrying a child.
Dosage and regimen
The dosage of taurine depends on the indication. It should be consumed 20-30 minutes before meals. In case of increased stomach acidity, the drug must be taken after meals. Otherwise, it will irritate the gastric mucosa.
For cardiovascular diseases, dietary supplements are sufficient to drink 250 mg 2 times a day. The course of admission is 1 month.
Patients with type 1 and type 2 diabetes mellitus should take 1 capsule of taurine with a concentration of 500 mg 2 times a day. The course of treatment is 3-6 months.
Attention! For diabetics, the maximum daily dose is 1.5 g, for patients with heart disease - 3 g. Athletes can take up to 5 g per day.
For epilepsy, it is recommended to take the drug with taurine at night. For pregnant and lactating women, the dose should be selected by a doctor.
How much should I take?
Taurine is produced as a separate preparation and is included in many multi-component products. It is present in almost any pre-workout complex or energy drink, and its amount can exceed the average daily requirement
, which is
400 mg per day
. In specialized sports supplements, the concentration of taurine may be different: from 200 to 2000 mg. This dosage should not confuse people who train, since during intense physical activity the need for taurine increases and the body can absorb more of the substance.
The maximum daily dose, when taken, you can be sure that no side effects will be observed during the rest of your life, is three grams. In this case, the substance is taken as a dietary supplement in addition to the food consumed.10 Higher doses have also been tested and proven to be well tolerated, but there is insufficient experimental data to suggest the lifelong safety of these doses.
Reviews about the application
Leave feedback about the supplement. Write what pros and cons you found:
| Leave your review | |
| 1 2 3 4 5 | |
| Send Cancel | |
Send your review
Taurine tablets and capsules
Average rating: Number of reviews: 0
Based on the reviews, the following advantages were identified:
- supplements are really effective for type 1 and type 2 diabetes;
- the composition, in addition to taurine and useful substances, does not contain harmful impurities;
- improve vision;
- support the functioning of the heart, liver, pancreas;
- normalize blood pressure;
- reduce swelling.
However, buyers claim that in case of ophthalmological diseases it is necessary not only to drink dietary supplements, but also to use eye drops.
The role of taurine in metabolic diseases
Mitochondrial disease (MELAS)
The characteristic symptoms of MELAS (mitochondrial encephalomyopathy, lactic acidosis, stroke-like episodes) also develop with taurine deficiency [34], which is explained by the similarity of the pathophysiology of these two conditions. MELAS is caused by specific point mutations in the region of DNA encoding leucine tRNA (tRNALeu(UUR))[8]. The mutations appear to alter the structure of the tRNA, preventing the conjugation of taurine to the uridine base tRNALeu(UUR). Modification of the uridine base alters the interaction of the UUG codon with the AAU anticodon tRNALeu(UUR), thereby altering UUG decoding [35]. Taurine deficiency also appears to result in decreased formation of the taurine conjugate, 5-taurinomethyluridine-tRNALeu(UUR), which is associated with decreased mitochondrial taurine content [8]. Taurine deficiency reduces the expression of UUG-dependent proteins, including ND6, a subunit of complex I. Because ND6 plays an important role in complex I assembly, taurine-mediated reduction in ND6 levels leads to the conditions noted in MELAS: lactic acidosis, decreased complex I activity, and oxygen consumption. Impaired respiratory chain function results in increased superoxide production and decreased ATP production, which plays a central role in the development of myopathy and encephalopathy in MELAS.