Attention!
The information in the article is for reference only and cannot be used for self-diagnosis or self-medication. To decipher the test results, contact a specialist.
There is no such person who has never suffered from bronchitis in his life. It affects people of any age. In adults, if bronchitis develops, it is mild and does not have any health consequences.
Severe obstructive bronchitis most often affects children. The younger the child, the more complex the disease. It is less treatable. Sometimes it takes on a rapid course that threatens the baby’s life.
Obstructive bronchitis, what is it?
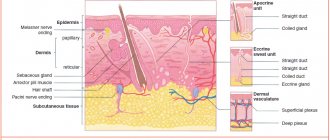
Obstructive bronchitis is classified as an inflammatory lesion of the bronchial tree. It affects the mucous membrane lining the inside of the bronchi. Edema narrows the lumen of these structures. Inflammation during bronchitis spreads throughout the entire thickness of the bronchial wall. The function of the ciliary epithelium is impaired.
The disease occurs with symptoms of obstruction, which are expressed in impaired bronchial patency. In children, obstructive bronchitis occurs with attacks of unproductive cough, which is accompanied by noisy whistling breathing.
Such patients are characterized by forced expiration, rapid breathing and distant wheezing. Obstructive bronchitis in children develops at any age. More often than other age groups, it affects children aged six months to 5 years.
The disease is more often registered in children with allergies, weakened immunity and the presence of a genetic predisposition, frequent and prolonged viral respiratory infections. The number of cases of obstructive bronchitis in children is steadily increasing.
How does oxygen get into the blood?
Through the thin walls of the alveoli, oxygen enters the blood vessels. Here it is picked up by “transport” - hemoglobin
, which is contained in red blood cells. At the same time, carbon dioxide enters the opposite direction - into the alveoli - from the blood, which is removed from the body when exhaling. Oxygenated blood is sent from the lungs to the left side of the heart, from where it is distributed throughout the body through arteries. As soon as the oxygen in the blood is used up, the blood flows through the veins to the right side of the heart and from there back to the lungs.
Causes of bronchitis
Primary obstructive bronchitis in children is often caused by viruses. The following pathogens affect the bronchial tree:
- parainfluenza virus type 3;
- respiratory syncytial virus;
- enterovirus;
- influenza viruses;
- adenoviruses;
- rhinovirus.
Often the manifestation of obstructive bronchitis in a child is preceded by a cold. The disease is repeatedly caused by other pathogens of persistent infections, which include:
- chlamydia;
- mycoplasma;
- herpesvirus;
- pathogens of whooping cough, parawhooping cough;
- cytomegalovirus;
- mold fungi.
Often, with repeated cases, the opportunistic microflora of the respiratory tract is activated. Allergic reactions play a significant role in the development of bronchial inflammation in children. Relapses of obstructive bronchitis are facilitated by infection with worms and foci of chronic infection (sinusitis, tonsillitis, caries). Factors that provoke the development of exacerbations include:
- physical fatigue;
- hypothermia;
- neuropsychic stress;
- congenital failure of protective barriers;
- unfavorable climate;
- poor environmental stop;
- decreased immunity;
- lack of vitamins.
Passive smoking, as well as irritation of the ciliary epithelium by dust particles and chemicals, play an important role in the development of obstructive bronchial inflammation in children.
Classification of bronchial cancer
The histological (based on the appearance of tumor cells under a microscope) classification of bronchopulmonary cancer includes four main types of tumors:
- Small cell cancer occurs mainly in smokers, is highly aggressive, spreads quickly and is difficult to treat. It accounts for about 12% of all cases of bronchopulmonary cancer.
- Squamous cell carcinoma , together with the next two types, combines into a group of non-small cell tumors , which account for more than 80% of all cases of lung cancer. The risk of developing squamous cell carcinoma is strongly associated with smoking.
- Adenocarcinoma is most common among women and nonsmokers. Unlike squamous cell carcinomas, adenocarcinomas are usually smaller in size and tend to grow in the peripheral parts of the lung. A separate subgroup of bronchoalveolar adenocarcinomas is distinguished.
- Large cell carcinoma consists of large, undifferentiated cells.
Depending on how much the tumor tissue has lost its normal features, poorly differentiated and highly differentiated tumors are distinguished. The first ones are more aggressive.
When choosing treatment, the location of the tumor foci is of great importance. Depending on this indicator, bronchopulmonary cancer is divided into two types:
- Central - the tumor is located in the bronchi of the 1st–3rd order (main lobar, segmental).
- Peripheral - the tumor is located in the smaller bronchi.
Write to an oncologist
Pathogenesis of obstructive bronchitis in children
The pathogenesis of the disease has a complex structure. When a virus invades, inflammatory infiltration of the mucous membrane lining the bronchi occurs. Various groups of leukocytes migrate in large numbers in its tissue. Inflammatory mediators are released - histamine, prostaglandin, cytokines. Edema of the bronchial wall develops.
Then the smooth muscle fibers in the wall of the bronchi contract, causing bronchospasm to develop. Goblet cells activate the secretion of bronchial secretions. Mucus has increased viscosity. A disorder of the ciliated epithelium occurs. Mucociliary insufficiency develops. The process of coughing up mucus is disrupted.
The lumen of the respiratory tract is blocked by bronchial secretions. This creates ideal conditions for the proliferation of the bronchitis pathogen. The submucosal and muscular layer of the bronchi is exposed to inflammation. Peribronchial interstitial tissue is included in the process. Lung tissue is not involved in inflammation.
Causes of bronchial cancer
A normal cell turns into a tumor cell when certain changes occur in its genes. It is impossible to say exactly why, in one case or another, genetic defects arose that led to malignant transformation. But there are known factors that significantly increase the risk of the disease. They are called risk factors .
The main risk factor for bronchopulmonary cancer is smoking. The likelihood that a person will be diagnosed with a malignant tumor directly depends on the length of smoking, the daily number of cigarettes smoked, the age at which the person started smoking, and the brand of cigarettes (tobacco quality, carcinogen content). Not only active but also passive smoking is dangerous. If someone constantly smokes in an apartment, the risk of lung cancer is increased for all its residents.
Other risk factors:
- Occupational hazards: workers in mines, factories producing cement, glass and fiberglass.
- Contact with chemicals, some volatile substances, asbestos.
- Air pollution with radon , a radioactive gas that is naturally released from the soil when uranium decays.
- It can accumulate indoors.
Classification and stages of development of obstructive bronchitis in children
There are three forms of obstructive bronchitis - bronchiolitis, acute and recurrent. Bronchiolitis often affects children under 2 years of age. This is how their body responds to the introduction of rhinovirus or respiratory syncytial infection. It is preceded by a mild ARVI. As the condition worsens, respiratory and heart failure develops. With this form, characteristic moist, fine-bubble wheezing appears on inhalation and exhalation.
Acute bronchial obstruction most often occurs in children aged three to five years. It is caused by parainfluenza and influenza viruses, adenovirus. First, the temperature rises to high numbers. Other symptoms of ARVI appear. Then manifestations of respiratory failure increase. The child has difficulty breathing. The muscles of the neck and shoulders are involved in the breathing process. Whistling sounds occur when exhaling. Exhalation becomes difficult and lengthens.
Recurrent obstructive bronchitis occurs at any age. It is caused by: mycoplasma, cytomegalovirus, herpes virus, Epstein-Barr virus. Bronchial obstruction increases gradually. This occurs at normal or low-grade fever. Nasal congestion, runny nose and infrequent coughing are noted. Shortness of breath is moderate. The general condition is almost unaffected. According to the course of the disease, the following forms are distinguished: acute, protracted, recurrent and continuously relapsing.
Human lungs: brief characteristics of the organ
The functioning of the brain, the release of energy, and the breakdown of useful substances with the help of oxygen directly depend on the functioning of the respiratory system. The respiratory organs include the nose, mouth, larynx, trachea, and bronchi, which are part of the lungs.
The lung is one of the paired, most voluminous human organs. In a healthy state, it is pink-red in color, the structure is soft, spongy.
The average volume of the organ is 3 liters, but 450-500 ml is enough for inhalation and exhalation. In people who are actively involved in swimming, the lung volume reaches 5 liters.
For a deep breath, about two liters of atmospheric air are used. With such breathing patterns, a reserve remains in the organ, thanks to which the level of oxygen in the alveoli is maintained at the required level.
In the tissues of each lung, venous and arterial blood constantly moves, and lymphatic vessels are present. It also contains nerve cells that are closely connected with blood vessels and bronchi.
In the first month of pregnancy, the rudiments of the main organ of the respiratory system are already formed in the fetus, and by the fifth month its constituent elements are designated. The organ continues to grow until the age of 25, as the growing organism constantly needs oxygen.
Symptoms of obstructive bronchitis in children
At the onset of the disease, the clinical picture is dominated by manifestations of ARVI. Dyspeptic symptoms are possible in small children. Bronchial obstruction often occurs on the first day of illness. Bronchitis is manifested by the following symptoms:
- increase in respiratory rate (up to 60 per minute);
- prolongation of exhalation;
- dyspnea;
- breathing is noisy, wheezing;
- auxiliary muscles are involved in the act of breathing;
- the anteroposterior size of the chest increases;
- flaring wings of the nose;
- cough with scant sputum, paroxysmal in nature;
- sputum discharge is difficult;
- pale skin;
- cyanosis of the lips;
- cervical lymphadenitis.
Bronchial obstruction persists for up to a week. Then its manifestations gradually subside as inflammation in the bronchi subsides. Children under six months of age develop acute bronchiolitis. Inflammation in the bronchi is accompanied by severe respiratory failure.
Lung location
The lungs are located in the middle of the chest. They are protected and supported by a frame of ribs, 12 on the left and right. On the back side, the organs are protected by the spinal column.
To ensure the ability to breathe, there is muscle tissue between the ribs; the bones are fixed to the sternum by cartilage. From the back, the lungs are located 2-3 cm above the collarbones.
From below, the organ borders the diaphragm, which separates the peritoneum and chest. On the right side, under the lung, is the liver. On the left side, the heart is adjacent on top, and partly the stomach is below. The exact location of a person’s lungs can be clearly seen in the photo.
Complications of obstructive bronchitis in children
Acute obstructive bronchitis is complicated by the transition to a continuously relapsing form. It is formed against the background of secondary bronchial hyperreactivity. It develops due to various factors: passive smoking, untreated infections, hypothermia or overheating, frequent contacts with people infected with ARVI.
In children under three years of age, bronchitis is complicated by pneumonia. This is associated with difficulties in evacuating thick sputum. It closes the lumen, disrupting the ventilation of the pulmonary segment. When bacterial flora attaches, inflammation develops. This complication occurs rarely. It occurs only in weakened children.
Stages of bronchial cancer
Bronchopulmonary cancer is divided into stages depending on how far the tumor has spread in the body. In this case, they are guided by the generally accepted TNM classification. The letters in it mean:
- T—size of the primary lesion, degree of invasion into adjacent tissues.
- N - damage to regional (close to the primary tumor) lymph nodes.
- M—presence of distant metastases.
Depending on these indicators, the stage of the tumor is determined, which is designated by Roman numerals I–IV.
Diagnosis of obstructive bronchitis in children
To make a diagnosis, the child is examined by a pediatrician or pulmonologist. During the examination, the doctor performs auscultation (listening to the chest with a phonendoscope) and percussion (tapping).
To diagnose obstructive bronchitis, use:
- radiography (fluorography) – required to identify changes in the pulmonary pattern and exclude pneumonia;
- tracheobronchostoscopy - secretion, ulceration of the mucous membrane, fibrin deposits are detected in the bronchi;
- sputum culture tank - examination of material to search for the pathogen with determination of sensitivity to antibiotics;
- detection of antibodies to various viruses;
- PCR to isolate viral antigen;
- spirography - study of external respiration function;
- blood gas analysis;
- Peak expiratory flow study;
- spirography - measures the volume and speed of exhaled air
- skin allergy tests are carried out to exclude the allergic nature of the pathology.
The child is prescribed laboratory tests (general analysis and blood biochemistry, level of C reactive protein).
How does breathing happen?
Before birth, the baby receives oxygen directly from its mother's blood, so its lungs are filled with fluid and do not work. At the moment of birth, the baby takes his first breath, and from that moment his lungs work without rest. The respiratory center of the brain constantly receives signals about how much oxygen the body requires at any given moment. For example, if a person is sleeping, he needs much less oxygen than when he is running for the bus. The brain sends messages along nerves to the breathing muscles, which help regulate the amount of air entering the lungs. As soon as this signal is received, the diaphragm expands and the muscles stretch the chest outward and upward. This maximizes the volume that the lungs can occupy in the chest. When you exhale, the diaphragm and intercostal muscles relax, reducing the volume of the chest. Due to this, air is pushed out of the lungs.
Treatment of obstructive bronchitis in children
Children with bronchitis are often treated on an outpatient basis. Indications for hospitalization include age up to one year, the child’s serious condition, and the presence of concomitant pathologies. The main treatment is etiotropic therapy. It includes antiviral or antibacterial drugs.
Pathogenetic therapy includes selective bronchodilators or inhaled glucocorticosteroids. They are inhaled through a compressor nebulizer. The following drugs are prescribed as symptomatic therapy:
- diluting sputum - they facilitate its evacuation;
- expectorants - activate the movements of the cilia and promote coughing;
- antipyretics;
- non-steroidal anti-inflammatory drugs;
- restoratives (vitamins, immunomodulators).
During the recovery period, physiotherapy, massage and breathing exercises are prescribed.
Methods for diagnosing bronchial cancer
Usually the tumor is detected using x-rays. CT and MRI help to clarify its size, location, number of foci and their degree of invasion into surrounding tissues. Bronchoscopy is used - an endoscopic examination, during which a special instrument in the form of a long flexible hose - a bronchoscope - is inserted into the bronchial tree and the mucous membrane is examined.
During bronchoscopy, a biopsy can be performed: a fragment of a pathologically changed area of the mucous membrane can be obtained and sent to the laboratory for cytological and histological examination.
A biopsy can be performed in other ways: using a needle inserted into the lung through the chest wall, during thoracoscopy, or thoracentesis. You can also do a cytological examination of the sputum to look for cancer cells.
PET scanning helps detect small metastases. During this study, sugar with a special radioactive label is introduced into the body. The radiopharmaceutical accumulates in tumor cells and makes the lesions visible in pictures taken using a special device.
If necessary, the doctor may prescribe other diagnostic methods.
Surgical treatment of bronchopulmonary cancer
Surgical tumor removal is often the main treatment for local bronchial and lung cancer when there are no isolated metastases. The goal of radical surgery is to completely remove the tumor tissue. Depending on the size and location of the lesions, different types of surgical interventions are used:
- Removal of the entire lung - pneumonectomy .
- Removal of a lobe of the lung - lobectomy .
- Removal of a segment of the lung - segmental resection .
- Removal of the tumor with some surrounding healthy tissue - wedge resection .
- Removal of affected lymph nodes - dissection, lymphadenectomy .
The operation can be performed openly (through an incision) or endoscopically ( video-assisted thoracoscopic surgery , or VATS ).
Chemotherapy
Chemotherapy drugs are drugs that destroy actively reproducing cells. Thus, their target in the body is primarily tumor cells, but healthy cells can also be affected, which is why chemotherapy is often accompanied by side effects. Modern doctors know how to reduce their risk and how to deal with them.
Like radiation therapy, chemotherapy for bronchial and lung cancer can be adjuvant, neoadjuvant, or can act as the main method of treatment. Different chemotherapy drugs with different mechanisms of action are used. Typically, your doctor will prescribe a combination of two or more drugs. Combinations are selected depending on the type and stage of the tumor.