Symptoms of gastritis with low acidity, treatment and diet
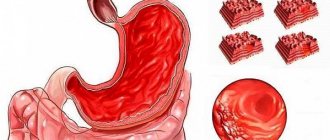
Gastritis with low acidity is a common type of inflammation of the gastric mucosa. With it, the acidity level of gastric juice and its volume decrease, which causes a decrease in the stomach’s ability to digest food. In addition to improper digestion, this disease entails even greater danger. The natural level of acidity protects the stomach from the penetration of infections into the intestinal cavity.
With low acidity, there is a possibility of intestinal infections and inflammatory processes. Like any form of this disease, gastritis with low acidity causes regular abdominal pain, and can also transform into gastroduodenitis, stomach cancer and peptic ulcers.
Reasons for development
Gastritis with low acidity or hypoacid is an inflammation of the gastric mucosa, in which the glands that produce hydrochloric acid gradually atrophy. Because of this, the acidity of gastric juice decreases, it can no longer dissolve and digest food as effectively, as a result of which the absorption and assimilation of nutrients is impaired and deficiency states develop.
Since this disease is most often diagnosed in old age, the main reasons for its development are considered to be poor lifestyle choices: overeating, alcohol and cigarette abuse, and decreased physical activity.
The main reasons for the development of the disease:
- Internal - have less importance in the development of this disease, these include: other inflammatory diseases of the gastrointestinal tract, endocrine disorders, the formation of antibodies to the cells of the gastric mucosa.
- External – overeating; coarse, difficult to digest food, the habit of eating very salty, spicy, hot foods, fried and canned foods; smoking; alcohol abuse; Helicobacter pylori infection.
Unfavorable external and internal factors cause inflammation and damage to the gastric mucosa, cells lose the ability to quickly regenerate, the functioning of the glands is gradually disrupted, less and less hydrochloric acid and gastric juice are produced, and the cells atrophy. The motility of the stomach and intestines is also disrupted, and the contents of the duodenum are refluxed into the stomach, causing the mucous membrane to become even more inflamed.
Acidity - what's the point?
As the specialist notes, gastric acidity is a characteristic of the concentration of hydrochloric acid in gastric juice, which is measured in pH units. Hydrochloric acid is produced by the cells of the fundic glands, they are called parietal glands.
There are several types of pH environments in gastroenterology:
- increased (maximum pH 0.86);
- reduced (minimum pH 8.3);
- neutral or normal (1.5-2.0 pH.).
“Only the last type is considered healthy. With a normal pH environment, the gastrointestinal tract quickly and well digests incoming food and neutralizes toxins and infections that come with it. If the acid level deviates in any direction, the person begins to experience unpleasant symptoms,” notes the therapist.
Look into the stomach. Why do gastroscopy through the nose Read more
Types of disease
Depending on the location and accompanying symptoms, gastritis can be of the following types:
- Atrophic gastritis with low acidity. Thinning of the mucous membrane is observed, tissues die and lose their protective function. It is divided into antral and diffuse. A severe decrease in the level of acid in the stomach is the most dangerous condition, as it can provoke cancer. The exact cause of its development has not yet been established, but overeating, poor diet, and taking hormonal medications and antibiotics as self-medication play an important role.
- Chronic gastritis of the stomach with low acidity. This disease, in turn, is divided into the stage of compensation, partial compensation and decompensation. The chronic variant develops slowly: initially, acidity increases significantly. If treatment is not started, the acid-producing cells die and little is produced. Acidity returns to normal. With further progression, atrophy (death) of the gastric mucosa begins, and a chronic version of the disease occurs. Chronic gastritis with decreased secretion is often caused by the bacterium H. Pylori.
Prevention and treatment of gastritis
As we have already noted, there are no universal treatment regimens for gastritis and diets, which is due to the variety of varieties of this disease. Until recently, medicine did not know any effective methods of therapy at all. Nutritional correction was most often used. For example, from the diet of patients with gastritis with high acidity, dishes and foods that irritate the walls of the stomach and increase acid secretion were excluded. They recommended drinking Borjomi mineral water, baking soda and medications, which could only reduce the acidity level and alleviate the symptoms of gastritis. Effective means appeared only in the 80s.
Today, gastritis can be successfully treated: the main thing is not to waste time, not to experiment with self-medication and not to panic, since the psychosomatic factor also plays a big role, notes the gastroenterologist at the clinic. N.I. Pirogova Victoria Sergeevna Semyonova.
Prevention of gastritis: useful tips
- Stick to a balanced and varied diet. Food must enter the stomach regularly. “Rhythm of nutrition” plays an even more important role in the prevention of gastritis than diet.
- Wash your hands, food and utensils thoroughly. Be careful if you are dining in a public place.
- Drink clean water at room temperature - it improves the secretion of the stomach walls.
- Include foods rich in prebiotics and probiotics in your diet, for example, milk, chicory, soy, cereals, and white cabbage. They are useful not only for the microflora of the stomach, but also for the immune system.
- Play sports whenever possible. WHO recommends at least 150 minutes of physical activity per week.
- Find out your blood glucose and cholesterol levels, and get tested for Helicobacter pylori. Elevated readings may indicate serious problems.
- Don't forget to take care of your dental health and oral hygiene.
- The daily requirement of vitamin B12 for an adult is 2.4 mcg. Remember this.
- Avoid taking aspirin and other NSAIDs. If, in the treatment of any disease, the doctor prescribed antibiotics and drugs to improve intestinal microflora, then you need to drink both. Don't neglect advice.
- Try to neutralize the stress factor of gastritis: rest, don’t worry and get enough sleep.
How to get gastritis: bad advice
- Smoke;
- Drink more alcohol;
- Put yourself on a strict diet;
- Skip breakfast or lunch;
- Drink strong coffee on an empty stomach, hot drinks and plenty of soda;
- Forget that not all food is healthy;
- Put yourself on a vegetarian diet, which does not take into account the body's daily need for proteins, vitamins B12 and B9.
- Eat fresh fish without worrying about the quality of its processing;
- Optimize your time: work, run, watch an exciting movie while eating;
- Don't be afraid of gastritis or be too afraid of it.
How is gastritis treated at the clinic named after.
N.I. Pirogov in St. Petersburg, you can find out at this link. Make an appointment with a gastroenterologist now so as not to let gastritis ruin your life!
First signs
The disease is accompanied by characteristic signs of a local and general nature:
- belching;
- nausea;
- regurgitation;
- a feeling of heaviness and pressure in the epigastric region after eating;
- unpleasant sensation in the mouth (especially in the morning);
- heartburn;
- burning in the epigastrium.
Immediately after eating, a dull pain occurs in the epigastric zone; Moreover, the pain sensation increases in a standing position and when walking. Intestinal dyspepsia is very often observed: rumbling, flatulence. With low acidity, diarrhea usually occurs, which worsens significantly after drinking milk or eating fatty foods.
Symptoms
The more acidity is reduced, the more clearly the symptoms of gastritis with low acidity will appear:
- Signs of excessive bacterial growth include rumbling, loose stools, milk intolerance, and bloating. If gastritis is accompanied by frequent diarrhea, weight loss may occur and signs of mineral or vitamin deficiency may develop.
- Dystrophy - signs of deficiency of B vitamins, as well as C, E, D, protein deficiency (weight loss, “polished” or coated tongue with a thick white coating).
- Dyspepsia - loss of appetite, feeling of heaviness or fullness in the stomach, belching of rotten food, bad breath (cocosmia), unpleasant taste, nausea.
- Dull, aggravated after eating, without clear localization, aching pain that occurs due to stretching of the stomach.
- Development of anemia due to decreased absorption of iron and vitamin B12 (due to Castle factor).
Since inflammation of the stomach also affects other parts of the digestive system, hypoacid gastritis is often accompanied by diseases such as enterocolitis, cholecystitis, and pancreatitis.
Sit down at the table with an appetite
The following is true not only when a diet is used for atrophic gastritis, but in general. Dishes should be appetizing. Although older people may experience an attack of hunger, they still more often sit down to the dinner table without desire or pleasure. To improve your appetite, add some of your favorite spices, onions, garlic, and sour fruits to your food.
The diet should contain enough animal and plant proteins. Try to diversify your dishes - include various cereals, pasta, legumes, vegetables, and fruits in your weekly menu. Give preference to easily digestible foods - fish, poultry, eggs, dairy products.
Carbohydrates - day-old bread, cereals, dried fruits - as well as animal and vegetable fats correct body weight. Your menu includes butter, sour cream, cheese, vegetable oil (at least 1 tablespoon per day), nuts, seeds.
Don't forget about foods that are sources of vitamins. Let me remind you that vitamin C is contained in vegetables, fruits, berries, especially black currants, sea buckthorn and rose hips. Vitamins D and E - unrefined vegetable oil, egg yolk, liver. B vitamins – brown bread, nuts, whole grains, rice, peas, cabbage, milk, meat.
Patients with cardiovascular pathologies need foods rich in potassium and magnesium. Dried apricots, black currants, raisins, prunes, potatoes, green peas contain a lot of potassium, and bran, buckwheat, and beans contain a lot of magnesium. Sources of phosphorus, zinc, calcium, iron - cauliflower, cucumbers, walnuts, wheat, fish, liver, meat.
Diagnostics
A gastroenterologist and endoscopist are involved in the diagnosis and treatment of gastritis with low acidity. The specialist examines the patient and conducts a number of examinations:
- morphological studies;
- X-ray of the stomach;
- esophagogastroduodenoscopy;
- endoscopic biopsy;
- gastroscopy;
- determination of pepsinogen level;
- gastric probing with intragastric pH-metry;
- examination of gastric juice;
- diagnosing pylori using stool ELISA, PCR testing, detection of antibodies in the blood and a breath test for this microorganism.
The purpose of these studies is not to confuse the disease with other pathologies and to make an accurate diagnosis. Based on the examination results, the gastroenterologist prescribes a treatment regimen. If required, the attending physician will refer you for a consultation with a nutritionist, who will create an appropriate diet. In some cases, to eliminate concomitant diseases, consultation with other specialists of a narrow focus (cardiologist, therapist) is required.
Gastritis or functional dyspepsia?
The term “gastritis” is usually used to refer to various inflammatory and degenerative changes in the gastric mucosa. But in fact, the disease itself is quite rare and can only be diagnosed using a biopsy during a gastroscopy procedure.
Often what is called gastritis is functional dyspepsia (a set of disorders of the digestive system). The term “gastritis” is also mistakenly used to mean gastroesophageal reflux disease (GERD) or irritable bowel syndrome (IBS).
Currently, the diagnosis of “gastritis” is usually made in the presence of morphological signs discovered after undergoing a series of medical examinations, in particular, after laboratory identification of the main causative agent of the disease - the bacterium Helicobacter pylori (H. Pilory), histological studies and FGDS.
Complications
With prolonged inflammation in the gastric mucosa, atrophic gastritis with low acidity can occur, which is characterized by changes in cell structure and their death.
As a result of atrophic processes, the number of properly functioning cells decreases, and it becomes difficult for them to secrete enzymes and mucus in the required volume, which disrupts the absorption of nutrients. If the disease becomes chronic, the gastric mucosa becomes thinner and food is not completely digested and absorbed.
The danger of this disease is that often, without treatment, it turns into cancer (according to statistics, the probability of the disease is more than 10%). Cancer processes can occur due to insufficient antitumor protection of the mucosa. To avoid tumor processes and further complications, it is important to be thoroughly examined and begin therapy at an early stage.
Bacterial gastritis: is Helicobacter pylori really dangerous?
As we have already noted, bacterial gastritis, the culprit of which is the bacterium Helicobacter pylori (Helicobacter), is common in 80-90% of cases of all gastritis. This bacterium is transmitted through household contact (through dishes, kisses), and in the stomach it exhibits extremely aggressive behavior. In a short time, it multiplies in the mucous membrane and secretes destructive enzymes - urease. Under their influence, urea, which is contained in the stomach, turns into ammonia. Thus, Helicobacter breaks down the protective mucus, exposing the stomach wall, and then provokes inflammation, ulcers and metaplasia, which carries an oncological risk.
The bacterium Helicobacter pylori has been studied relatively recently. It was discovered in 1979 by Robin Warren
- Pathologist at the Royal Perth Hospital.
He studied the contents of the stomachs of patients with gastritis and accidentally discovered in many of them a spiral-shaped bacterium that multiplied safely even in a very acidic environment. A few years later, a desperate scientist-enthusiast named Barry Marshall
drank a test tube of Helicobacter cultures, after which he almost died from severe gastritis. In 2005, both researchers were awarded the Nobel Prize for their discoveries.
Today, WHO names the bacterium Helicobacter pylori as the No. 1 cause of stomach cancer worldwide. But don’t rush to get scared!
It is interesting that carriers of this bacterium in developed countries are 25-30% of the population, in Russia and Japan - 60-80%, and in Africa - 100%. And this has been going on for several millennia. Yes, predisposition to gastritis also depends on the population. In the body of a healthy person, there is a constant war between the immune system and Helicobacter pylori. The bacterium wins only sometimes, so many Helicobacter carriers do not develop inflammation of the stomach wall.
However, according to the European consensus recommendations and the Kyoto global agreement, treatment and observation for Helicobacter pylori is still necessary. Especially for residents of countries with a high risk of developing stomach cancer (Russia and Japan), as well as patients who are at risk for gastritis, that is, with poor heredity, concomitant pathologies, vitamin B12 deficiency, etc.
The gold standard for diagnosing Helicobacter are special test strips based on contact of blood with a reagent, as well as a 13C-urease breath test. If the result is positive, the patient is prescribed a gastroscopy. To get rid of Helicobacter pylori, a course of antibiotic therapy is usually sufficient. However, as we already know, antibiotics are not good for our stomach, since they also kill beneficial microorganisms. Therefore, only a doctor can select the necessary medications after studying the anamnesis and examination. The presence of Helicobacter pylori itself usually does not provoke gastritis - additional triggers are needed.
To prevent Helicobacter pylori invasion in the stomach, you should regularly visit the dentist (since this bacterium lives comfortably not only in the stomach, but also between the teeth, in tartar) and, of course, keep your hands, dishes, vegetables and fruits clean. If one of the family members is diagnosed with Helicobacter, this does not mean at all that you need to panic, quarantine the carrier of the virus and urgently treat everyone in the family.
How to treat gastritis with low acidity?
Typically, treatment of gastritis with low acidity is long-term and complex. Since this disease is characterized by problems with juice secretion, drugs are usually prescribed that can stimulate the normal functioning of this function. A medicine is also prescribed to restore gastric motility.
The gastritis treatment program includes:
- suppression of the active inflammatory process in the gastric mucosa - antibiotics and antimicrobial agents are prescribed to which the pathogen is sensitive (the drugs and their dose are prescribed by a gastroenterologist);
- replacement and enzymatic therapy - for this purpose pepsin, hydrochloric acid, complex enzymatic preparations (panzinorm, festal, mezim, enzistal) are used;
- restoration of impaired motility of the digestive tract - use drugs that activate the movement of the food bolus through the gastrointestinal tract and eliminate spasm of intestinal smooth muscles;
- vitamin therapy - it allows you to eliminate the symptoms of hypovitaminosis in patients;
- A mandatory component of the treatment of gastritis with low acidity is the use of diet.
Before prescribing treatment, it is necessary to conduct a comprehensive examination of the patient and determine the acidity of the stomach, as well as examine the condition of the mucous membrane (fibrogastroduodenoscopy and fluoroscopy are required).
Digestive insufficiency and its correction from the position of a gastroenterologist in Korolev
O.I.
Kostyukevich Digestion is a set of processes that ensure the processing and transformation of food products into simple chemical compounds that can be absorbed by the cells of the body. This process ensures the replenishment of energy and plastic resources, and therefore is necessary for the life of the body. Digestion is a complex multi-stage process: Stage 1: oral Stage 2: gastric Stage 3: in the duodenum Stage 4: in the small intestine Stage 5: in the large intestine Any disturbances can lead to serious consequences for the body. In the oral cavity, primary hydrolysis of carbohydrates occurs under the action of amylase and maltase in saliva. Disturbances in the synthesis of salivary enzymes will not have such pronounced consequences as with pancreatic insufficiency. However, the lack of pancreatic amylase can to some extent be compensated for by salivary amylase. This explains such a clinical symptom in patients with chronic pancreatitis as hypersalivation. Mechanical and chemical processing of food occurs in the stomach. Mechanical is provided by the motor activity of the stomach, chemical is carried out by enzymes of gastric juice. The initial hydrolysis of proteins occurs in the stomach. Crushed and chemically processed food masses mixed with gastric juice form liquid or semi-liquid chyme. Digestion in the small intestine. The main processes of digestion and absorption of nutrients occur in the small intestine. The role of its initial section, the duodenum, is especially important. Pancreatic, intestinal juices and bile are involved in the digestion process. With the help of enzymes that make up pancreatic and intestinal juices, hydrolysis of proteins, fats and carbohydrates occurs. The exocrine activity of the pancreas consists of the formation and secretion of 1.5–2.0 liters of pancreatic juice into the duodenum. Pancreatic juice is represented by proteolytic, lipolytic and amylolytic enzymes. Alpha amylase, lipase and nuclease are secreted in an active state; proteases - in the form of proenzymes. Pancreatic alpha-amylase breaks down polysaccharides into oligo-, di- and monosaccharides. Pancreatic lipase, active in the presence of bile salts, acts on lipids, breaking them down into monoglycerides and fatty acids. Intestinal juice is the secretion of glands located in the mucous membrane of the small intestine. An adult produces 2–3 liters of intestinal juice per day. Intestinal juice contains more than 20 enzymes that provide the final stages of digestion of all nutrients. There are 2 main stages of digestion:
- Cavity;
- Parietal (membrane).
Cavity digestion occurs with the help of enzymes entering the cavity of the small intestine (pancreatic juice, bile, intestinal juice). As a result of cavity digestion, large molecular substances (polymers) are hydrolyzed to oligomers. Their further hydrolysis occurs in the area adjacent to the mucous membrane and directly on it. Parietal digestion in a broad sense occurs in the glycocalyx zone and on the surface of microvilli. Glycocalyx adsorbs digestive juice enzymes from the cavity of the small intestine. Hydrolysis products arrive at the apical membranes of enterocytes, into which intestinal enzymes are built in, carrying out their own membrane digestion, as a result of which monomers are formed that can be absorbed. Digestion in the large intestine. The role of the large intestine in the process of digesting food is small, since food is almost completely digested and absorbed in the small intestine, with the exception of plant fiber. In the colon, chyme is concentrated by absorbing water, feces are formed and removed from the intestine. Absorption of electrolytes, water-soluble vitamins, fatty acids, and carbohydrates also occurs here. At each of these stages, changes may occur that lead to disturbances in digestion (maldigestion) and/or absorption of food (malabsorption), which will have inevitable clinical consequences. Digestive insufficiency is a discrepancy between the digestive system’s ability to digest and absorb nutrients and the volume and/or composition of incoming food. Digestive insufficiency accompanies a wide range of diseases of the gastrointestinal tract, and can also occur in a healthy person due to an unbalanced diet or too much food eaten, and therefore is very common in the daily practice of a gastroenterologist. Clinical manifestations of digestive insufficiency are found in 25–41% of the population [1]. The term “dyspepsia” is used to refer to numerous symptoms associated with digestive disorders. Manifestations of dyspeptic syndrome traditionally include [2]:
- Heartburn
- Nausea and vomiting
- Belching
- Unpleasant sensations (discomfort or pain) in the epigastric region
- Flatulence
- Stool disorders.
Symptoms of dyspepsia can be observed both together and separately and accompany almost any disease of the gastrointestinal tract. At the same time, each of them has a different origin and different mechanisms of occurrence, and also requires completely different approaches to treatment, which makes it inappropriate to so broadly combine all symptoms with a single term. Currently, the main pathophysiological mechanisms of digestive insufficiency can be classified as follows: 1. Insufficiency of cavity digestion, the causes of which are:
- Diseases of the pancreas, both hereditary and acquired (chronic pancreatitis, condition after pancreatectomy, pancreatic cancer, cystic fibrosis).
- Secretory insufficiency of the stomach (atrophic gastritis, postgastrectomy syndrome).
- Bile acid deficiency or asynchronism of bile flow into the small intestine during biliary obstruction, hepatitis, cirrhosis, cholelithiasis, after cholecystectomy.
- Inactivation of digestive enzymes in gastroduodenitis, duodenal ulcer, dysbacteriosis of the small intestine.
- Disturbances in the transit of intestinal contents and disturbances in the mixing of enzymes with food chyme in duodenal and gastrostasis, intestinal pseudo-obstruction, irritable bowel syndrome.
2. The second group is associated with dysfunction of parietal digestive enzymes, for example, lactase deficiency. In both the first and second cases, a large amount of undigested nutrients remains in the intestinal cavity, which leads to a disruption in the composition of the internal environment of the intestine, incl. changes in pH, osmotic pressure, chemical composition. These changes lead, on the one hand, to secondary damage to the intestinal mucosa and even greater disruption of the digestive processes, and, on the other hand, to a change in the composition of the intestinal microflora, which aggravates existing disorders. Disorders of parietal digestion develop due to:
- disaccharidase deficiency (congenital and acquired lactase deficiency);
- dystrophic changes or death of enterocytes (celiac enteropathy, sarcoidosis, Crohn's disease, bacterial overgrowth).
Gastrogenic digestive insufficiency develops in hypoacid conditions after gastric resection. As a result, the secretion of gastric juice decreases, and due to insufficient secretin stimulation of the pancreas, pancreatic secretion also decreases. It is important that low gastric secretion also leads to microbial contamination of the small intestine, which, in turn, contributes to the inactivation of digestive enzymes. Gastrogenic digestive insufficiency can be manifested by a feeling of heaviness in the epigastric region, nausea, belching, and vomiting. Pancreatic insufficiency. Despite the variety of causes that cause digestive disorders, the most severe disorders are associated with diseases of the pancreas (PG), since it is the most powerful source of digestive enzymes. Exocrine pancreatic insufficiency is divided into primary and secondary [3]:
- primary pancreatic insufficiency is caused by diseases of the pancreas itself, as a result of which the synthesis of enzymes is reduced;
- with secondary pancreatic insufficiency, the amount of digestive enzymes is sufficient, but their action is not fully realized for one reason or another. Secondary pancreatic insufficiency is divided into hepatogenic (cholegenic), gastrogenic, enterogenic and vascular [4].
In hepatogenic insufficiency, the activation of lipase in the intestinal lumen is impaired due to a reduced amount of bile acids or asynchrony of the flow of bile, pancreatic enzymes and chyme into the duodenum. Gastrogenic pancreatic insufficiency develops due to insufficient secretin stimulation of the pancreas. In addition, reduced gastric secretion is compensated for some time by functional tension of the pancreas, which gradually leads to its depletion. Enterogenous pancreatic insufficiency is mainly associated with bacterial contamination. It is important that in the development of this deficiency, not only damage to the mucous membrane of the small intestine by pathogenic and opportunistic flora, but also endotoxins secreted by this flora is important. Vascular pancreatic insufficiency develops when microcirculation in the intestinal wall is impaired. Pancreatic insufficiency is clinically manifested by increased intestinal motility, increased frequency of stools, polyfecal matter, steatorrhea, flatulence, and changes in appetite. Clinical manifestations of lipase deficiency develop before the decrease in amylase and protease activity. This is due to the earlier development of disturbances in lipase production by the pancreas compared to other enzymes and to the more rapid inactivation of lipase in the intestine.
Correction of digestive insufficiency
The main direction in the treatment of patients with syndromes of impaired digestion and absorption, especially when it is impossible to eliminate the causes of their development, is replacement therapy with enzyme preparations. About 150 years ago, the Dutch doctor D. Flesch used an aqueous extract from the pancreas of calves to treat steatorrhea in a patient with diabetes mellitus, but many aspects of the use of enzyme preparations still remain controversial. Considering the variety of nosological forms and pathogenetic mechanisms associated with digestive disorders, the range of indications for the use of enzyme preparations is quite wide. These indications are divided into several groups [5,9]. I. Diseases of the pancreas: chronic pancreatitis with pain and dyspeptic syndromes, with external and intrasecretory insufficiency; conditions after resection of the pancreas; large cysts, pancreatic tumors; diabetes; congenital hypoplasia (Shwachman, Joganson-Blizzard syndromes) or its atrophy (Clark-Hadvild syndrome), etc. II. Stomach diseases: chronic gastritis with decreased gastric secretion or achylia; conditions after gastric resection. III. Diseases of the small and large intestines: chronic enteritis; bacterial overgrowth. IV. Diseases of the liver and biliary tract: cholestatic liver diseases; conditions after cholecystectomy; chronic cholecystitis with hypomotor dysfunction of the gallbladder. V. Motility disorders of the digestive tract of a functional or other origin: functional dyspepsia, gastro- and duodenostasis of another origin; dysfunction of the gallbladder and/or sphincter of Oddi. VI. Other indications: conditions after irradiation; enzyme deficiency in older people (“aging” digestive organs); binge eating; monotonous food; long bed rest; sedentary lifestyle; preparation for ultrasound, etc. Moreover, the choice of enzyme preparation for each nosological group will be different. Currently, enzyme preparations used in clinical practice must meet certain requirements [6]:
- good tolerance;
- absence of significant adverse reactions;
- optimal action in the pH range 5–7;
- resistance to hydrochloric acid, pepsins and other proteases;
- content of a sufficient amount of active digestive enzymes;
- have a long shelf life.
Enzyme products are classified according to their release form into non-shelled and shelled. Based on their composition, enzyme agents are classified as follows [6]:
- Extracts of the gastric mucosa, the main active ingredient of which is pepsin.
- Pancreatic enzymes, represented by amylase, lipase and trypsin (for example, Panzinorm forte-N).
- Combined enzymes containing pancreatin in combination with bile components, hemicellulose and other additional components.
These enzyme preparations are by no means interchangeable. Different groups have clear and strict indications and contraindications for use, neglect of which can lead not only to the lack of the expected result, but also cause various side effects.
- The first group of enzymes is mainly aimed at correcting gastric secretory dysfunction. These drugs are used primarily for hypoacid atrophic gastritis, usually in combination with prokinetics.
- Preparations containing only pancreatic enzymes are used primarily for replacement therapy in the presence of exocrine pancreatic insufficiency, as well as to create “functional rest” for the organ in the presence of an exacerbation of the disease, especially accompanied by intraductal hypertension. For this purpose, drugs containing the main pancreatic enzymes are used - lipase, trypsin, chymotrypsin and amylase (for example, Panzinorm forte-N). The drugs differ from each other primarily in the number of enzymes, as well as in the form of release. The amylase included in the complex decomposes starch and pectins into simple sugars - sucrose and maltose. Proteases (chymotrypsin, trypsin), respectively, are involved in the hydrolysis of proteins. In addition, they reduce pancreatic secretion via a feedback mechanism and regulate intestinal motility. Lipase is involved in the hydrolysis of neutral fat. Pancreatin preparations do not affect the function of the stomach, liver, motility of the biliary system and intestines, but reduce the secretion of pancreatic juice.
- In addition to pancreatic enzymes, the combination drugs also include bile acids, pepsin, and hemicellulase. The introduction of bile acids into the drug significantly changes its effect on the motility of the gastrointestinal tract, the function of the stomach and biliary tract. These drugs stimulate pancreatic secretion and choleresis, enhance intestinal and gallbladder motility. The presence of hemicellulase in the enzyme preparation ensures the breakdown of plant polysaccharides.
However, it should be borne in mind that combination drugs should be avoided in case of liver pathology, since bile acids enter the enterohepatic circulation and are metabolized in the liver, which increases its functional load. Given the stimulating effect on pancreatic secretion, the drugs should not be taken in case of intraductal hypertension or exacerbation of pancreatitis. In the presence of bacterial overgrowth syndrome, before administering bile acids, it is necessary to carry out selective decontamination of the small intestine in order to avoid deconjugation of bile acids by microflora. Deconjugated bile acids damage the mucous membrane of the gastrointestinal tract with the subsequent development of osmotic and secretory diarrhea. Thus, each group of enzyme preparations has its own, strictly limited indications for use. The use and prescription of drugs according to indications within this framework contribute to the normalization of digestive processes and improvement of the patient’s condition. Incorrect use of various groups of enzymes leads to discredit of these drugs, lack of positive effect or deterioration of the patient's condition. Even within the same group, drugs differ in the quantitative composition of their components, production method and form. The difference in the structure of pancreatic enzymes justifies the variety of their clinical applications.
Clinical features of the use of enzyme preparations
Currently, there is a concept of using high doses of enzymes for replacement therapy for primary exocrine pancreatic insufficiency and low doses for the correction of functional changes and secondary pancreatic insufficiency [7]. 1. Prescription of enzyme preparations for diseases of the pancreas. A. To compensate for exocrine pancreatic insufficiency, highly active enzyme preparations containing large doses of enzymes are usually used. Replacement therapy is necessary for diseases accompanied by atrophy of more than 90% of the organ parenchyma [8]. The dose of enzymes depends on the degree of exocrine insufficiency, as well as on the patient’s ability to follow a diet. For exocrine pancreatic insufficiency, a single dose of enzymes ranges from 20 to 40 thousand units. lipases. The drugs are taken with food 3 times a day. The effectiveness of therapy is assessed clinically and laboratory (scatological examination, excretion of fat in feces, elastase test). The drugs are well tolerated, but in exceptional cases, with prolonged use of more than 50,000 units of lipolytic activity, fibrosing colopathy and urolithiasis may develop. Therefore, the dose of enzymes should not exceed the required one. B. Another indication for the use of pancreatin preparations is the creation of “functional rest” of the pancreas during exacerbation of chronic pancreatin, intraductal hypertension to relieve pain. Treatment of pancreatitis with pain requires a strict diet in combination with hyposecretory drugs, antispasmodics and pure pancreatin preparations. The latter, through a feedback mechanism, inhibit their own pancreatic secretion, reducing intraductal hypertension and leading to relief of pain. To create functional rest for the gland, enzymes are prescribed in a slightly different regimen: 15–20 minutes before meals, 3 times a day. 2. For hyposecretory diseases of the stomach, decreased gastric motility, it is advisable to use both pancreatin preparations and combined enzyme preparations, the action of which is aimed at compensating for disturbances in the activity of the gastric mucosa. Preparations containing pepsin are taken at the rate of 0.2–0.5 g of pepsin per meal, 2–3 times a day before or during meals. These drugs should not be prescribed for diseases associated with increased acid formation, as well as for painful forms of chronic pancreatitis. Since hypoacid conditions are in most cases accompanied by secondary pancreatic insufficiency, combined enzyme preparations can be considered the drugs of choice. 3. To treat hypomotor biliary dyskinesia, enzyme preparations containing bile acids are used, which stimulate the contractile activity of the gallbladder and normalize the biochemical properties of bile. 4. To treat patients with impaired motor function and tone of the colon, in addition to antispasmodics and laxatives, digestive enzymes are used, which contain bile components that cause increased intestinal motility and help resolve constipation. 5. For functional dyspepsia, in elderly patients, with a sedentary lifestyle, as well as to relieve symptoms of overeating, it is advisable to occasionally take small doses of enzymes containing bile components, which creates optimal conditions for the digestion and absorption of nutrients in the small intestine. One of the enzyme preparations that meets all modern requirements for this group of medicinal substances is Panzinorm forte-N. Panzinorm forte-N contains in each tablet pork pancreatin with enzyme activity: lipase 20,000 units Ph.Eur., amylase 12,000 units Ph. Eur.. protease 900 units Ph. Eur. Indications for use of the drug are:
- Insufficiency of exocrine pancreatic function (chronic pancreatitis, cystic fibrosis, etc.)
- Chronic inflammatory-dystrophic diseases of the stomach, intestines, liver, gall bladder; conditions after resection or irradiation of these organs, accompanied by impaired digestion of food, flatulence, diarrhea (as part of combination therapy).
- To improve food digestion in patients with normal gastrointestinal function in case of dietary errors.
Preparation for x-ray and ultrasound examination of the abdominal organs. The dose is determined individually depending on the degree of digestive disturbance. The duration of treatment can vary from a single dose or several days (if the digestive process is disrupted due to errors in the diet) to several months or years (if constant replacement therapy is necessary). It is important to remember that each group of enzyme preparations has its own indications. Prescribing drugs strictly according to these indications contributes to the effective normalization of digestive processes, avoids side effects and leads to an improvement in the clinical condition of patients. Improper use of enzyme preparations leads not only to the lack of the desired positive effect, but even to a deterioration in the patient’s condition, which contributes to the discrediting of these drugs. Normalization of such a complex process as digestion is a labor-intensive process that requires significant effort on the part of both the doctor and the patient. Therapy should be comprehensive and based on the pathogenetic mechanisms of the development of digestive insufficiency in this particular patient.
Literature
- Ivashkin V.T., Sheptulin A.A. and others. A short guide to gastroenterology. – M.: Publishing house. House of M-Vesti, 2001.
- Grigoriev P.Ya., Yakovenko A.V. Clinical gastroenterology. M.: MIA, 2001. p. 693.
- Gubergrits N. B., Khristich T. N. Clinical pancreatology. - Donetsk: Lebed, 2000.
- Petukhov V. A., Turkin P. Yu. Exocrine pancreatic insufficiency in cholelithiasis: etiopathogenesis, diagnosis and principles of treatment // Rus. honey. magazine - 2002. - T. 10. - No. 4. - P. 167–171.
- Gubergrits N. B., Lukashevich G. M. Enzyme preparations: from theory to practice. - Donetsk: Lebed, 2002.
- Shcherbakov pancreatic insufficiency and its treatment. Pharmaceutical Bulletin No. 28 (227), 2001.
- Grigoriev P.Ya., Yakovenko E.P. Recommendations for the use of enzyme preparations for the syndrome of impaired digestion and absorption. Treatment doctor, No. 5–6, 2001, pp. 48–50, 52.
- Sarles H., Pastor J., Pauli AM, Barthelemy M. Determination of pancreatic function. A statistical analysis conducted in normal subjects and in patients with proven chronic pancreatitis (duodenal intubation, glucose tolerance test, determination of fat content in the stools, sweat test) // Gastroenterol. 1963. Vol. 99. P. 279–300.
- Pchelintsev M.V. Pancreatic enzyme preparations, selection criteria for a general practitioner. New St. Petersburg doctor. Vedomosti, No. 1, 2001, pp. 63–66.
Digestive insufficiency and its correction from the position of a gastroenterologist. Kostyukevich O.I. Russian Medical Journal. Diseases of the digestive system. 2008. Vol. 10, No. 1, p. 10-14.
Folk remedies to increase stomach acidity
Low stomach acidity requires very serious attention and treatment. But often very positive results can be achieved by properly selected nutrition.
- A drink made from sea buckthorn berries is very useful.
- A very healthy and tasty habit: half an hour before meals you need to drink a few sips (50–70 grams) of honey water, for which you need to dissolve half a teaspoon of honey in warm water.
- For low stomach acidity, apricots in any form have proven themselves very well - fresh, dried (apricots, dried apricots) - and apricot juice.
- A decoction or infusion of rosehip, which is also very good to drink before meals, perfectly helps regulate low stomach acidity.
- Fresh cucumbers also slightly increase the acidity of gastric juice if they are properly chopped (the finer the better).
- Grapes are useful - it is recommended to eat up to 150 grams of fresh grapes 20 minutes before meals.
- Fresh turnip salad has long been used to increase acidity: fresh turnips must be grated and seasoned with vegetable oil (salt should be taken to taste, but not overused).
- Beans help increase and normalize the acidity of gastric juice.
- Freshly prepared carrot juice is very useful, which should be drunk shortly before meals, a quarter glass.
- With low stomach acidity, the benefits of blueberries are generally recognized, which can be used in pies, dumplings, and compotes.
- A long-term and persistent increase in the acidity of gastric juice ensures the consumption of a variety of meat foods. However, it should be remembered that for any diseases of the gastrointestinal tract, you should choose only lean meat (this could be lean pork, veal, rabbit, skinless poultry).
Also, to normalize the acidity of gastric juice, decoction and juice of plantain, calamus root, trefoil (also known as trifolium or water trefoil), gentian, marsh cudweed, lingonberry, St. John's wort, buckthorn, rhubarb, yarrow, rowan, centaury, immortelle, aloe, thyme are used and many other herbs, fruits and berries that our land is rich in.
Nutrition after stroke
In her letter, the woman writes about a recent stroke, as well as chronic atrophic gastritis and underweight. Unfortunately, the author did not report what her weight was before the illness, when it dropped and by how much, what she eats, whether she follows a diet, what concomitant diseases caused the stroke, what medications she takes... This information would have made our conversation more substantive.
Post-stroke patients always face two tasks: to recover from a stroke and to prevent another. There is no special diet for such patients. Nutrition is adjusted individually taking into account blood pressure, the severity of atherosclerotic changes in blood vessels and the level of cholesterol in the blood, since it is often elevated in patients with chronic vascular diseases. In particular, for hypertensive patients, neurologists prescribe special drugs - statins - to reduce cholesterol and recommend limiting fat intake to 75-80 g per day, with half coming from vegetable oil.
I advise you to take these dietary features into account if your cholesterol levels are elevated. I also note that patients suffering from hypertension and having had a stroke are more likely to be overweight, which needs to be reduced. For the author of the letter, underweight is determined by one’s state of health.
Diet and proper nutrition
If you have gastritis with low acidity, a strict diet is required. It should include:
- Cereals and pasta. Rice, buckwheat, oatmeal, and semolina are allowed.
- Soups - with low-fat chicken or fish broth, vegetable, vermicelli, cereal, with meatballs.
- Lean meat (chicken, beef, rabbit, turkey). Fish (pike perch, hake, pollock, pike).
- Eggs – no more than 2 pieces per day.
- Seasonings and sauces - vegetable oil, salt, herbs.
- Vegetables - beets, pumpkin, carrots, tomatoes, zucchini, cauliflower.
- Dairy products - cottage cheese, sour cream, mild cheese, milk, yogurt.
- Sweets - biscuits, marshmallows, marshmallows, marmalade.
- Fruits and berries – pureed (jelly, compotes, jelly, soufflé).
- Drinks – tea, rosehip infusion, weak coffee.
- Bakery products - yesterday's white bread, uneatable crackers.
Exclude from the diet:
- Pastries, sweets, fresh bread.
- Soups with mushrooms and fatty broths.
- Legumes, barley, corn and millet porridge.
- Large-grained and rough-skinned berries and dried fruits.
- Hot sauces, store-bought dressings, mayonnaise.
- Fatty meat and fish.
- Cucumbers, bell peppers, cabbage, turnips, radishes, mushrooms. Pickles and marinades are not allowed.
- Fast food, alcohol, carbonated drinks, packaged juices.
It is important that meals are fractional - 5-6 times a day. It is better to snack on vegetable or fruit purees or dairy products.
The diet for gastritis with low acidity is quite loyal - the patient will not suffer from hunger, but at the same time will not experience a feeling of overeating. If the proposed diet is followed for a long time, the symptoms of gastritis will appear less and less often and a long-term remission will occur.
Proper nutrition for gastritis in the acute phase
If gastritis is in the acute phase, the following tactics are usually used:
1.
On the first day, when an attack of reactive gastritis has just occurred, it is better to abstain from food altogether, allow the stomach to rest from digesting food, and allow the mucous membrane to recover a little. From the liquid you can drink slightly warm tea and water. During this period, people usually experience a decreased appetite - this is a deliberate reaction of the body, dictated by its needs for rest.
2.
On the second or third day, you can switch to table No. 1A, which involves taking liquid food, viscous cereal or milk soups, meat and fish purees (from low-fat varieties), and soft-boiled eggs. Butter and vegetable oil are allowed in small quantities. You can drink decoctions, jelly, weak tea (with honey), water.
Fresh fruits and vegetables, baked goods and confectionery, rich meat broths, fermented milk drinks, cheese, coffee, and any soda remain prohibited. Add salt in minimal quantities; you will have to discard spices. Nothing hot, sour, spicy or fatty is allowed.
3.
After the end of the acute period and the onset of remission, a doctor or nutritionist trained in clinical nutrition will prescribe you a special gentle diet. It will have to be followed as long as necessary (in cases with chronic forms of gastritis - throughout your life).
To alleviate the condition during exacerbation of gastritis, adhere to the following menu (an approximate diet that can be recommended by a gastroenterologist or nutrition consultant after the acute symptoms of the attack have been relieved):
Breakfast
- 200 g semolina or rice porridge with a small piece of butter;
- a glass of warm tea with milk.
Snack
- 150 g cottage cheese casserole or steamed cheesecakes;
- 200 ml milk.
Dinner
- 150 g meat puree (lean varieties, for example, boiled chicken fillet);
- 200 g boiled rice (porridge);
- 200 ml compote or dried fruit jelly.
Afternoon snack
- 1 soft-boiled egg;
- 200 ml oatmeal jelly.
Dinner
- 200 g puree from boiled lean fish;
- rosehip decoction.
Before bedtime
- 200 ml milk.