September 22, 2020
Gastritis is an inflammation of the gastric mucosa, leading to disruption of its secretory function
Gastritis is an inflammation of the gastric mucosa, leading to disruption of its secretory function. During the inflammatory process, food entering the stomach is poorly digested, which leads to impaired absorption of nutrients.
Chronic gastritis affects about 60-85% of the world's population, including young people aged 18 to 35 years. Due to the modern rhythm of life, gastritis has begun to occur more often in children aged 5 to 13 years. Among all diseases of the gastrointestinal tract, gastritis is the most common; a common “marker” of gastritis is the appearance of pain in the stomach. American scientists Marshall and Warren received the Nobel Prize for their discovery of the infectious mechanism of gastritis, caused by the microorganism Helicobacter pylori. This microorganism has been identified in the mucous membranes of many patients suffering from chronic gastritis.
Causes of gastritis
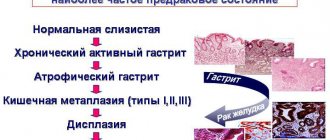
As previously mentioned, the main trigger of the disease is infection with the bacterium Helicobacter Pylori. Excessive proliferation of this bacterium in the stomach leads to irritation of the intestinal mucosa and provokes gastric ulcers. Helicobacter is also considered a serious factor in the development of stomach and small intestine cancer. Scientists are inclined to contact and household transmission of infection from the patient and the carrier. Abuse of drugs that can irritate the walls of the stomach, which include anti-inflammatory drugs and drugs containing acids, also provokes the development of gastritis.
Strong alcoholic drinks, carbonated drinks, and drinks containing acid cause irritation and chemical burns to the walls of the stomach. Smoking, in turn, stimulates excessive secretion of gastric juice, so at the treatment stage the patient is advised to give up the bad habit. If we talk about dietary habits, a diet containing insufficient fiber prevents the gastrointestinal tract from working properly. A diet rich in processed foods and low in fresh foods leads to increased secretion of gastric juices, which irritate the stomach walls.
Excessive alcohol consumption can irritate the stomach lining, making it more vulnerable to infection. Gastritis may be associated with other diseases, including HIV/AIDS, Crohn's disease, and parasitic infections. Nervous factors and various types of stress are of great importance in the development of chronic gastritis. Chronic gastritis also often develops against the background of other diseases of the gastrointestinal tract (chronic enterocolitis, helminthic infestations, diseases of the liver, biliary tract, gall bladder, pancreas). Endocrine diseases and metabolic diseases (thyroid disease, diabetes mellitus, iron deficiency anemia) play an important role in the manifestation of the disease. Genetic factors are also important, that is, the transmission of the disease by inheritance.
Causes
External reasons:
- malnutrition (dry food, snacks, poor chewing of food contribute to the appearance of mechanical injuries to the gastric mucosa, excessive consumption of salty and spicy foods contributes to irritation of the mucous membrane, too cold or hot food - thermal damage to the mucous membrane);
- damage to the stomach by Helicobacter pylori and other bacteria and fungi;
- foreign bodies entering the stomach;
- smoking and excessive drinking (which release caustic chemicals into the stomach);
- long-term use of medications (in particular glucocorticoid hormones, acetylsalicylic acid, NSAIDs, iron supplements, etc.);
- exposure to radiation on the mucous membrane;
- contact with mucous membranes of alkalis, acids and other toxic substances;
- parasitic infestations;
- chronic stress (acute stress gastritis can be a consequence of a serious illness, injury, life-threatening conditions, etc.).
Internal reasons:
- genetic predisposition (presence of gastritis in close relatives);
- duodenogastric reflux (reflux of fluid from the duodenum into the stomach);
- autoimmune processes that damage stomach cells;
- chronic infectious diseases (including salmonellosis, coronavirus, rotavirus infections, etc.);
- metabolic disorders;
- endocrine disorders;
- lack of vitamins, etc.
Symptoms
Often gastritis is asymptomatic; symptoms indicating the disease may be aching or sharp burning pain in the pit of the stomach, which appears or intensifies during or after eating, heartburn, nausea, vomiting, flatulence, constant belching and heaviness in the abdomen, unreasonable weight loss , unpleasant taste in the mouth, heaviness, feeling of pressure in the chest.
The manifestation of the disease depends on the type of disease. For example, acute gastritis begins suddenly, often after food poisoning. Pain occurs in different areas of the stomach depending on the location of inflammation, and intensifies when taking foods that irritate the mucous membrane. The main symptoms of the acute phase of the disease: heartburn, vomiting, belching, frequent gas, bloating, headache, rapid heartbeat, dizziness, increased salivation or extreme thirst. Chronic gastritis is sluggish, symptoms in adults may vary, but this pathology is mainly characterized by belching with a characteristic odor, constant heartburn, a feeling of pain and heaviness, loss of appetite, diarrhea or constipation, coating on the tongue, and weight loss.
Depending on the form and type of gastritis, different treatments are prescribed, so it is important to see a doctor immediately.
Diagnostics.
Diagnosis of chronic gastritis is based on identifying complaints, collecting anamnesis, objective examination and conducting laboratory and instrumental examination methods.
The patient is recommended to undergo a clinical blood test, a biochemical blood test - ALT, AST, total bilirubin, amylase, glucose. The gold standard for diagnosis is an FGDS; to diagnose Helicobacter pylori infection, a urease breath test or a stool test for Hp Ag is used.
Additional methods:
- Ultrasound of the abdominal organs;
- with atrophy of the gastric mucosa - determination in the blood: pepsinogen 1, pensinogen 2, gastrin 17;
- determination of antibodies in the blood to gastric parietal cells and intrinsic Castle factor;
- determination of the level of vitamin B12 in the blood.
Treatment of gastritis
In order to recover from gastritis, it is necessary to follow an individual diet and take a set of medications that will help restore the acid balance of the gastric mucosa.
The treatment regimen depends on the type of gastritis. Treatment is divided into the treatment of gastritis with low acidity using replacement therapy drugs, secretion stimulation drugs, improving microcirculation and symptomatic therapy. Treatment of gastritis with high acidity is carried out using such groups of drugs as secretolytics (proton pump inhibitors, H2-histamine blockers), antacids or alginates, gastroprotectors, which have a protective effect on the mucous membrane of the stomach and duodenum. Also, if the patient is diagnosed with the bacterium Helicobacter pylori, antibiotic therapy is prescribed.
Back to articles
Stomach acidity
The acid produced in the stomach is necessary for the digestion of food, for the absorption of iron, calcium, vitamin B12 and certain medications (for example, thyroxine and ketoconazole). Due to the high acidity of gastric juice, swallowed microorganisms, including bacteria and viruses, are destroyed. This prevents the development of infection and excessive growth of bacteria in the small intestine.
However, excessively high levels of acid secretion pose a risk to the integrity of the gastric and duodenal mucosa. Therefore, the secretion of gastric acid must be precisely regulated and produced according to needs.
Acid is produced by the parietal cells of the stomach. Their work is tightly controlled by numerous mechanisms, including the vagus nerve, gastrin, histamine, ghrelin, somatostatin, and glucagon-like peptide. Thanks to all these mechanisms (some of which are still not fully understood), the correct secretion of hydrochloric acid is ensured.
We wrote about reduced stomach acidity in a previous article:
Now we will talk about increased stomach acidity.
There are several reasons for increased stomach acidity:
- The most significant and dangerous reason is a tumor that produces gastrin in huge quantities. Gastrin is the main stimulator of hydrochloric acid secretion, so its production increases many times.
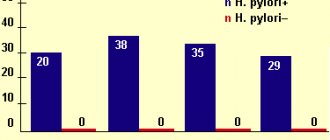
- Helicobacter pylori infection. In some patients infected with this bacterium, the secretion of hydrochloric acid increases.
- Taking painkillers, aspirin. These drugs reduce the production of bicarbonates - bicarbonates alkalize (make less acidic) the contents in the outlet of the stomach and duodenum.
- Increased production of hydrochloric acid for unknown reasons (probably congenital). As we have already discussed, the process of regulating its formation is complex; at what stage the “breakdown” occurs is not known; literature data on this topic is scarce and very outdated. As a rule, this increase is not so significant and if the patient is not bothered by it in any way, then this situation does not require diagnosis and treatment.
So, why is high stomach acid dangerous and why do we need this information at all?
Manifestations of increased stomach acidity may include the following:
- Heartburn. However, you need to understand that in most cases, heartburn occurs due to excessively frequent and prolonged reflux of stomach acid into the esophagus. The mechanism here is multicomponent and often the problem is not so much the level of acidity as the very fact of the stomach contents entering the esophagus. Even if the acidity level of the stomach is normal, this is enough to “burn” the esophagus. For heartburn, it is not recommended to determine the level of acidity in the stomach, since this information will not affect treatment tactics (not to be confused with determining acidity in the ESOPHAGUS, which in certain cases is necessary to select a treatment method!).
- Formation of ulcers in the stomach.
In 1910, the concept was recognized: “No acid, no ulcer.” In 1984, after the discovery of the role of H. pylori, the concept was radically changed: “No H. pylori - no ulcer.”
Yes, if the secretion of hydrochloric acid is increased many times (as in gastronomy - Solinger-Ellison syndrome), then ulcers actually form in the stomach and duodenum, and can even be in the esophagus and the initial part of the jejunum).
If the formation of gastric juice is not increased as significantly as in Solinger-Ellison syndrome, then, as a rule, acid alone is not enough to form ulcers - the presence of Helicobacter pylori infection and/or taking painkillers, aspirin is necessary.
For ulcers, the standards include diagnosis and treatment of Helicobacter (about 90% of all ulcers are associated with it), determination of gastrin levels (only if gastrinoma is suspected) and discontinuation of painkillers/aspirin if the patient was taking them (if cancellation is not possible, medications are prescribed for stomach protection). The standards do not include determining the level of acidity , since its moderate increase will not affect the treatment tactics (an exception may be the suspicion of the absence or sharp decrease in the production of hydrochloric acid by the stomach - here the determination of acidity can be useful and will affect the treatment tactics).
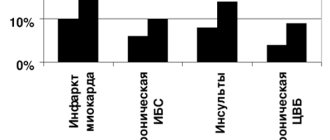
- Epigastric pain not associated with the formation of ulcers. The diagnosis sounds like functional dyspepsia (formerly chronic gastritis). Yes, indeed, approximately 20-25% of patients with functional dyspepsia have increased acidity of gastric juice. However, patients with dyspepsia in most cases benefit from treatment with drugs that reduce acidity, regardless of whether it was initially elevated or not (there is no exact correlation between the level of response to treatment and the level of acidity before treatment), so there is little point in defining it. And if the symptoms are eliminated, then further reducing acidity is pointless and unsafe.
Let's summarize the above: usually it is not too important for us to know that the patient's acidity is increased (with the exception of gastrinoma, and this is very rare), since this will not affect the treatment tactics:
- have an ulcer - we treat Helicobacter
- there is pain without an ulcer - we are treated according to the dyspepsia protocol
- there is heartburn - we modify the diet and weight, treat with drugs that reduce acidity (even if it is normal)
In clinical practice, the Gastropanel blood test is usually used to diagnose acidity levels ; in rare cases (usually as part of clinical studies), gastric pH-metry .
In most cases, the level of acid secretion is determined if there is a suspicion of a decrease in the level of its production, the cause of which is gastric atrophy. This really matters for the choice of treatment tactics and monitoring of the patient. Therefore, in Western countries, the Gastropanel blood test is used everywhere and is carried out by general practitioners to decide on the need for further FGDS and consultation with a gastroenterologist. Decisive is the presence of signs of Helicobacter pylori infection (analysis is included in the Gastropanel), signs of atrophy, signs of gastrinoma.
If a person has symptoms of functional dyspepsia (pain, burning, feeling of fullness and heaviness in the epigastrium) and heartburn, then he really has a subjective feeling that “too much acid is being produced” and this may be partly true (but as we discussed earlier - perhaps it’s not just the excess acid or not at all), so the diet can have a positive effect. It's no secret that certain foods stimulate the production of hydrochloric acid more strongly. Therefore, the first thing to do in case of the symptoms described above is to reconsider your eating habits - eat regularly, try to limit too sour, spicy, smoked, fried foods, as well as coffee, alcohol and fast food in your diet. But we remember that food should be tasty and nutritious - eating just chicken breast with buckwheat is also not an option. Diets that are too strict can do more harm than good and make the situation worse.
If changing your diet does not help, you should definitely consult a doctor to receive adequate examination and treatment.