Dentistry / Media about us / Dermatitis and the role of the Leptotrichia bacterium in their occurrence
Seborrheic and oral dermatitis are one of the pressing problems of dermatocosmetology.
Doctors note that the number of patients with these diseases, which manifest themselves as significant cosmetic defects of the skin in the form of oily sheen, peeling and rashes accompanied by itching, is constantly growing.
Why does dermatitis occur? How does he make himself known? And what to do to cope with this condition? The questions are answered by a dermatovenereologist (adult), dermatovenereologist (children), cosmetologist of the SCNT “NOVOSTOM” Natalya Vladimirovna Musayelova.
When should you take a vaginal flora smear test?
1. Suspected inflammatory changes in the urogenital tract or infection with sexually transmitted diseases 2. Suspicion of a violation of the vaginal microflora (taking antibiotics, poor diet, wearing synthetic underwear, panty liners, etc.) 3. As part of a comprehensive diagnosis during pregnancy (registration, at 30 and 37 weeks of pregnancy), before gynecological interventions (hysteroscopy, separate diagnostic curettage of the uterine cavity and cervical canal, operations on the uterus and/or uterine appendages, medical termination of pregnancy, etc.) 4 For differential diagnosis between diseases of the reproductive (colpitis) and urinary systems (urethritis, cystitis) 5. When pathological discharge from the genital tract appears (white, yellow, curdled, abundant, with an unpleasant odor, etc.).
Causes of intestinal infection in the uterus
The microorganism Escherichia coli is a normal inhabitant of the rectum. When E. coli enters the vagina and then the uterine cavity, it causes inflammation. This may happen due to:
- improper washing technique;
- insufficient genital hygiene;
- wearing tight synthetic underwear, thongs;
- combining anal and vaginal sex;
- change of sexual partner.
The penetration and reproduction of E. coli in the uterus is facilitated by low immunity, sudden temperature changes, menopause, and endocrine disorders in the body. Colonization by pathogenic microflora can be associated with douching, long-term use of antibacterial agents, and chronic infections (general and genital infections).
Prerequisites for the introduction of bacteria may include instrumental medical manipulations, curettage, hysterosalpingography, hysteroscopy, insertion of an intrauterine device, and trauma to the birth canal during childbirth.
We have prepared for you a list of studies that will help you deal with this problem:
30 working days
Gut microbiome
12000 ₽
More details
Detailed description of the study
A woman's genital organs are normally inhabited by many microorganisms. They create favorable physiological conditions and protect the genitals from pathogenic microorganisms. Between themselves, different types of representatives of normal microflora are in balance. A change in their quantitative ratio can lead to an imbalance in this balance: dysbiosis. It can occur due to hormonal disorders, failure to comply with personal hygiene rules, or taking antibiotics.
Dysbiosis can lead to inflammatory diseases of the vagina, uterus, its appendages, and ovaries. Without timely treatment of these diseases, the result may be the inability to conceive and pathologies of pregnancy.
Another common threat to reproductive health is sexually transmitted infections (STIs). The causative agents of some of them are microorganisms that can be reliably identified microscopically.
A flora smear is a microscopic examination of a scraping from the vagina. The study evaluates the following indicators, which indicate the composition of the microflora and the presence of inflammatory or infectious processes:
1. Rod-shaped bacteria are a normal component of the vaginal microflora. If there are too few of them, we can assume dysbiosis or bacterial vaginosis - excessive reproduction of some representatives of the normal microflora. 2. Elements of mushrooms. Normally, fungi can be part of the microflora, but in very small quantities. The presence of actively reproducing fungi of the genus Candida in the smear indicates candidiasis, in other words, thrush. 3. Flat epithelium. These are the cells that line the inside of the genitourinary tract. They are constantly renewed: new ones grow, and old ones peel off and are removed. Such cells should be present in the smear. If there are very few or none at all, it means the lining of the mucous membrane is underdeveloped. If there is too much, most likely inflammation has developed there. 4. Key cells are the same epithelial cells, but surrounded by bacteria. Their presence indicates bacterial vaginosis. 5. Slime. Should be present in the smear in moderate quantities. If there is too much or too little, inflammation can be assumed. 6. Leukocytes (immune cells). Their presence indicates an inflammatory reaction. 7. Trichomonas, Leptothrix, gonococci are the causative agents of STIs. Normally they should not be present in the smear.
The role of leptotrichia in the clinical course of seborrheic dermatitis and principles of treatment
Seborrheic dermatitis is one of the pressing problems of dermatocosmetology, as there is a constant increase in this disease, causing a significant cosmetic defect in the form of thickening of the stratum corneum, oily sheen and peeling of the skin, accompanied by itching. In recent years, the role of Leptotrichia bucalis has been shown in the occurrence of seborrheic dermatitis. Seborrheic dermatitis is based on a chronic inflammatory skin disease associated with an increase in the quantity and change in the quality of sebum with localization in those areas of the scalp and body where the sebaceous glands are developed - the scalp, eyebrows, eyelashes, naso-buccal folds, ears, behind-the-ear spaces, anterior chest area and interscapular area. When the skin of the scalp is affected, thinning and thinning of the hair is observed, very often accompanied by small flour-like or large-plate white scales. You can often see yellowish scales - crusts and hemorrhagic crusts formed as a result of scratching, when the skin of the forehead, behind-the-ear areas, and the area of the ear canals is involved in the process. Macular-erythematous elements, plaques, and papules appear on the smooth skin of the face, back, and chest. A genetic predisposition to certain metabolic characteristics and environmental influences on the development of the disease cannot be ruled out.
The leading role in the pathogenesis of seborrheic dermatitis of the scalp and dandruff is assigned to the pathogen Pityrosporum - yeast-like lipophilic fungi. These fungi are a permanent component of the microflora of healthy skin in more than 90% of the population with tropism around the sebaceous glands, because use the secretion of the sebaceous glands for their growth and development. Pityrosporum ovale or according to another classification Malassezia futur is more often found on the scalp. Pityrosporum orbiculare - on the skin of the trunk and face. Stressful situations worsen the course of seborrheic dermatitis due to changes in hormonal levels and metabolic disorders. The level of secretion and qualitative composition of sebum is determined by genetic and hormonal factors. Seborrheic dermatitis occurs more often in men than in women.
The most “problematic” category of patients are men aged 45–50 years. Obviously, this is due to hormonal imbalances in the form of decreased testosterone levels. In the overwhelming majority of such patients, we also observed liver dysfunction - from the phenomena of fatty hepatosis to minimal changes in the form of slight hyperbilirubinemia, fluctuations in the level of liver enzymes. Thus, the above reasons lead to the spread and increase in the number of previously saprophytic microorganisms and the development of foci of inflammation with disruption of the immune skin response, sebum secretion and keratinization of the epidermis.
In recent years, the interest of dermatovenerologists in anaerobic microorganisms, namely bacteria of the genus Leptothrichia and Leptothrix, has increased. According to the ninth edition of Bergey (1993), leptotrichia are assigned to the kingdom Procaryotae, division 1 Gracilicutes, family Bacteroidacea, genus Ltptotrichia, type species Leptotrichia bucalis, inhabitant of the human oral cavity. Leptotrichia look like straight or slightly curved rods with a diameter of 1.0 - 1.5 microns with pointed or rounded ends. Grammar, motionless. Two or more cells unite into septate filaments up to 200 microns thick and intertwine with each other, forming “felt”. In the micropreparation, filamentous rods consist of alternating light and dark areas, reminiscent in their structure of transverse striations (“slagbaum”).
With prolonged parasitism of leptotrichia on the mucous membranes of the oral cavity and genital organs, leptotrichosis infection leads to a general decrease in the resistance of the macroorganism, which is a trigger factor in the development of seborrheic dermatitis.
Diagnostics. Scrapings from the lesions are studied. The main criterion for diagnosing leptotrichosis lesions is the detection of the pathogen (10-15 bacteria in all fields of view) with the presence of inflammatory elements (leukocytes, histiocytes). Without the absence of inflammatory elements, it should probably be considered a bacterial carriage, which, under certain conditions of the macroorganism, can transform into a leptotrichosis infection. The tonsils, the lateral and posterior parts of the pharynx, the tongue, and the vaginal part of the cervix are mainly affected. Leptotrichosis is a pseudomycotic lesion of the oral mucosa. Objectively: a grayish-whitish coating initially appears on the mucous membrane of the oral cavity, tongue, arches of the soft palate and on the mucous membranes of the genitals, transitioning to a light brown, brown color, which cannot be easily removed with a spatula.
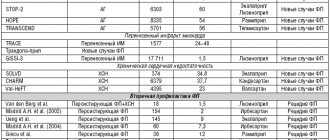
The diagnosis of the disease is made on the basis of characteristic clinical data and the microscopic picture of the specimen stained according to Romanovsky-Giemsa. We studied the role of leptotrichosis infection in the pathogenesis and clinical picture of seborrheic dermatitis: microscopy of leptotrichia, immunological parameters, the influence of complex treatment with immunocorrective and specific therapy on the clinical picture of seborrheic dermatitis in combination with leptotrichosis. Under our supervision in 2021 there were 49 patients with seborrheic dermatitis, in 2021 - 32.
Microscopy revealed spores and pseudomycelium of the genus Candida in scrapings from the mucous membrane of the hard palate - 29 patients, and leptotrichia with elements of inflammation from the tongue in 38 patients. Therefore, the correct interpretation of bacterioscopic preparations should be carried out, taking into account that the treatment of candidiasis and leptotrichosis is not the same. Under microscopy, the filaments of Leptothrix are often straight, do not branch, do not bud, and do not have fruiting organs. The abundance of leptothrix in all fields of vision, in combination with active exudation on the surface of leukocytes, is regarded as leptotrichosis. In patients with seborrheic dermatitis, microscopy of the tongue revealed leptotrichia. As a result of mycological studies of pathological material of the smooth skin of the face, neck, chest, back (scales in patients with seborrheic dermatitis, contents of elements), piterosporal fungi were found in 17 patients out of 39 patients with leptotrichosis. It has been established that the bulk of the studied immunological parameters in patients do not undergo significant deviations from the parameters of healthy individuals and lie within the limits of individual fluctuations, and only the phagocytic activity of neutrophils is significantly suppressed. The phagocytosis process averaged 45 + 8.7 with a norm of 58 + 7.1, the phagocytic number was 1.33 + 0.11 with a norm of 3.8 + 1.1, and the completion rate was 1.5 + 0.14 with a norm of 1.9 +0.7.
Treatment Based on the results of microscopic examinations and studies of the immune status, the clinical picture of patients with seborrheic dermatitis and leptotrichosis, complex therapy was used. For treatment, staphylococcal and combined bacteriophage were used by applying to the tongue or rinsing the mouth with 20 - 40 ml 1-2 times a day. The course of treatment is 8-10 days. Alternating applications of Betadine liquid to the tongue were carried out: bacteriophage in the morning, Betadine liquid in the evening. Immunoglobulin was administered parenterally 1-2 times a week. The course of treatment included 5 injections. All patients received specific therapy. It included the following drugs: Trichopolum 0.25, 2 tablets 2 times a day for 10 days, or Tiberal 1 tablet 2 times a day for 14 days. Patients with combined flora received antimycotic treatment. Of the 39 patients, 32 achieved clinical cure, which consisted of complete cleansing of the affected areas from plaque and elimination of subjective complaints. Erythema and inflammatory rashes on the smooth skin of the face and trunk resolved, hyperkeratosis decreased, and the feeling of itching disappeared. In 7 patients, the plaque became softer and was easily removed.
During a control microscopic examination after treatment, no leptotrichia were found in 29 patients, and single leptotrichia in 10 patients. These patients received a repeat course of specific therapy. Combinations of drugs were prescribed: miramistin, clotrimazole solution, sporobacterin, as well as thymogen, myelopid, decaris, nizoral, orungal. Metrogyl gel, 2% nizoral cream, clotrimazole, lamisil, lotion and cream “Elocom” and “Elocom-S” were used as local forms.
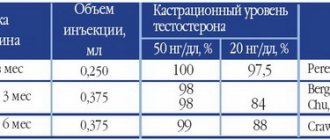
No relapses of the disease were detected during the observation period. Observations were carried out over time after 1, 3, 6 months. When studying the immune status over time, there is a tendency towards normalization of immunogram parameters within 3 months. Consequently, the results of the complex method of treating patients with seborrheic dermatitis and leptotrichosis that we use are quite effective and pathogenetically substantiated, which must be taken into account when choosing a method of treating these diseases.
Symptoms
Leptotrichosis has pronounced symptoms:
- White deposits form on the surface of the mucous membrane. As a rule, they are localized on the root of the tongue, tonsils, and dorsum of the tongue.
- Dense plaques develop under the plaque, which are clearly visible if the deposits are removed.
- The patient feels a burning sensation and pain in the oral cavity. Sometimes these symptoms are so severe that it becomes difficult for the patient to speak or eat.
- There are small “tweezers” on the surface of the plaques, which cause a sore throat and a feeling of a foreign body.
Prevention of intestinal infection in the uterus
Since the main route of infection is upward, it is important to prevent Escherichia coli from entering the vagina. To prevent intestinal infection from entering the vagina and then the uterus, it is recommended
:
- wash from front to back;
- do not overuse douching;
- keep the intimate area clean and dry;
- wash yourself after urination or sexual intercourse;
- refuse to use deodorized intimate hygiene products;
- avoid unprotected sex.
In medical genetics, you can undergo research to determine your susceptibility to diseases of internal organs and detect the prerequisites for dysfunction of the immune system.
Treatment for intestinal infection in the uterus
The goals of therapy are:
- elimination of E. coli;
- prevention of chronic inflammation;
- restoration of the menstrual cycle;
- preservation of a woman's reproductive function.
Both acute and chronic inflammatory processes in the uterus caused by an intestinal infection require antibacterial therapy. For symptomatic treatment, painkillers, restorative and immunostimulating agents, and probiotics with lactobacilli are used. Physiotherapy is used to treat damaged endometrium and restore the menstrual cycle.
Symptoms of intestinal infection in the uterus
Inflammation occurs at the site of damage to the mucous layer; due to swelling, it thickens and becomes loose. With weak immune defense, an intestinal infection can spread to the muscular layer of the uterus. Signs of inflammation appear 3–4 days after infection of the endometrium:
- low-grade or high fever;
- chills;
- general deterioration of health;
- pain in the lower abdomen, radiating to the lower back or groin area;
- vaginal discharge of a purulent-serous nature, possibly with admixtures of ichor.
With chronic inflammation in the uterus caused by an intestinal infection, women complain of irregular menstruation, constant aching pelvic pain, and intermenstrual spotting.
Laboratory diagnostics can identify the infection and determine its sensitivity to antibiotic therapy. The severity of the inflammatory process is determined by a clinical blood test. Ultrasound can confirm inflammation.