gastritis
bloating
diarrhea
sour taste in mouth
Helicobacter pylori
What are the consequences of changes in stomach acidity?
The main danger of increasing the secretory function of the stomach is the development of an inflammatory process in the mucous membrane of the organ, followed by its damage and the development of structural defects. A change in the pH of the gastric environment is always accompanied by clinical symptoms, the severity of which depends on the severity of the inflammatory process and the nature of the structural and functional disorders.
general information
In 80% of cases, the cause of the development of the inflammatory process with high acidity of the stomach is the microorganism Helicobacter pylori, which disrupts the natural protective properties of the stomach and leads to damage to the epithelium of the organ. Gastritis with high acidity can develop in people regardless of age, including children.
Other factors predisposing to the development of this condition include:
- Regular exposure to stress on the body.
- Poor nutrition, predominance of fried and fatty foods in the diet, as well as deep-fried dishes.
- Abuse of so-called snacks.
- Long-term or uncontrolled use of drugs from the group of non-steroidal anti-inflammatory drugs. Frequently eating food that is too hot or too cold. In addition, people with thyroid diseases, diabetes mellitus and gout have a high predisposition to the development of hyperacid gastritis.
Why is high acidity dangerous?
Gastric juice contains hydrochloric acid, which is necessary to break down food components. To prevent the acidic environment from damaging the walls of the stomach, protective mucus is produced. With increased acidity of the stomach, destruction of the mucous protective layer is observed, followed by the formation of an inflammatory process, the formation of erosions and ulcers.
Clinical symptoms
Inflammatory damage to the organ with increased secretion of gastric juice often worsens during the off-season, in the autumn or spring months. Symptoms of high stomach acidity include:
- Drawing or cramping pain in the epigastric region, which often intensifies after eating. In the acute course of the inflammatory process, the pain may be accompanied by vomiting, which brings temporary relief.
- Heartburn, which is caused by acidic stomach contents refluxing into the esophagus.
- Belching sour.
- Bad breath.
- Stool disorders such as constipation or diarrhea.
Other symptoms of increased stomach acidity during gastritis include weakness, dizziness, increased sweating, excessive gas formation in the intestines (flatulence), increased salivation, increased or decreased appetite, and the appearance of a white or gray coating on the surface of the tongue. Reduced stomach acidity is accompanied by symptoms such as decreased appetite, a feeling of heaviness in the epigastrium, and rotten belching.
Low stomach acidity
Stomach acid plays an important role in the human body - it is both a protective mechanism against ingested pathogens, and an activator of gastric juice enzymes and an assistant to enzymes in the digestion of proteins.
Low stomach acidity develops as a result of 3 main reasons:
- Gastric atrophy
- Taking medications that reduce gastric acidity (proton pump inhibitors, H2-histamine blockers)
- Removal of part of the stomach due to stomach cancer or as a bariatric treatment option (if the patient is severely obese, part of his stomach is removed for subsequent rapid weight loss)
I think it is worth covering in more detail the topic of atrophic gastritis as the reason for the decrease in the production of hydrochloric acid by the stomach.
With atrophy of the gastric mucosa, the number of glands gradually (over many years and decades) decreases and finally disappears completely. The production of hydrochloric acid first decreases and then stops altogether.
The main causes of gastric atrophy are Helicobacter pylori infection and autoimmune gastritis.
Helicobacter pylori is a bacterium that can lead to inflammation in the stomach; constant chronic inflammation contributes to gland atrophy. This process usually affects the antrum (outlet) of the stomach.
Autoimmune gastritis is a chronic disease that develops due to the fact that the human body, for unknown reasons, begins to perceive its own stomach cells as foreign and produces antibodies against them, which leads to inflammation and atrophy of the gastric glands. In autoimmune gastritis, the body and fundus of the stomach are mainly affected.
In the world, approximately 50% of people are infected with Helicobacter, and autoimmune gastritis occurs in approximately 1-2% of the population.
Of course, not all people infected with Helicobacter will develop such severe gastric atrophy that the secretion of hydrochloric acid will decrease. Moreover, with mild atrophy, the secretion of hydrochloric acid often remains normal.
In the presence of autoimmune gastritis, usually over the course of many years, atrophy becomes quite serious , and the presence of concomitant Helicobacter pylori infection aggravates the situation.
On average, the prevalence of atrophic gastritis worldwide is about 30%, most patients are people over 40 years of age.
About 2.5–5% of these people have progressive (moderate to severe) atrophic gastritis and an almost achlorid stomach in people over 50 years of age.
Reduced acidity and atrophy of the stomach leads to an increased risk of developing various infections , excessive growth of bacteria in the stomach and small intestine, deterioration of food digestion, and, accordingly, a deterioration in the absorption of vitamins and minerals. The absorption of vitamin B12 and iron slows down especially sharply, and the absorption of calcium, folic acid, and vitamin C is also worse.
Gastric atrophy and decreased secretion of hydrochloric acid can manifest as symptoms from the gastrointestinal tract, as well as from other organs, but you should know that in about half of the cases a person does not feel any symptoms for a long time.
Main symptoms of low stomach acidity
Main gastrointestinal symptoms include: epigastric pain, abdominal heaviness after eating, early satiety, heartburn (due to non-acid reflux), bloating, diarrhea or constipation.
Also clinically, atrophic gastritis and reduced gastric acidity are often manifested by anemia, which develops as a result of vitamin B12 and/or iron deficiency. The most common symptoms are the following: general weakness and fatigue, shortness of breath, pallor of the skin and mucous membranes, irritability and deterioration of mood, decreased cognitive abilities, perversion of taste - the desire to eat inedible objects (for example, soil or chalk), peripheral neuropathy and paresthesia (impaired sensitivity hands and feet - tingling and pinching sensation, numbness or, on the contrary, increased sensitivity of the skin), muscle weakness, lack of coordination. Decreased absorption of vitamin B12 and folic acid is accompanied by an increase in blood homocysteine levels, which can increase the risk of thrombosis, heart attacks and strokes.
Also, deterioration in calcium absorption can lead to osteoporosis (excessive bone fragility), which is manifested by pain in the bones/muscles, frequent bone fractures with minor trauma.
How to diagnose gastritis with reduced secretion of hydrochloric acid?
Quite a lot of methods for diagnosing reduced secretion of gastric acid are described in the literature, but most of them are either too complicated to perform and uncomfortable for the patient, or have very low sensitivity and insufficient evidence base.
I would like to note that quite often people over 50 years old come to the appointment and report with full confidence that their acidity is very low, their stomach “almost does not work.” And they gained confidence in this because once upon a time they were given an FGDS with a quick acidity test and were informed that their stomach was hypoacid, that is, there was very little acid. But I would like to note that the vast majority of these patients are fine with acidity (which is clarified during further examination), and the tests carried out in those days were extremely unreliable and showed hypoacidity . But currently there is a reverse trend - similar quick tests performed during FGDS, only now they diagnose high acidity in most patients. However, in foreign literature and recommendations, these tests are not mentioned as methods for diagnosing acidity levels, which means that these tests have not undergone reliable studies of sensitivity and specificity, therefore, the quality of these tests should also be doubted.
Therefore, in real clinical practice, it is worth relying on a blood test called “gastropanel” (the ratio of pepsinogen I/pepsinogen II, gastrin-17 and antibodies against H. pylori is studied), as well as an informative FGDS with multiple biopsies (according to OLGA or OLGA-M ) to determine the activity of inflammation in the stomach, the degree of atrophy and the presence of H. pylori - by the degree of atrophy one can indirectly judge the ability of the stomach to produce hydrochloric acid.
FGDS with biopsy according to OLGA or OLGA-M is the gold standard for diagnosing atrophic gastritis and identifying precancerous changes in the stomach.
If atrophic gastritis is detected, the patient is always tested for the presence of Helicobacter pylori infection. However, it must be remembered that in case of severe gastric atrophy with reduced secretion of hydrochloric acid, tests such as the C13-urease breath test and stool for antibodies to Helicobacter may be false negative. Therefore, in the case of serious atrophy, the best indicator of the presence of the microbe will be a biopsy of the gastric mucosa or detection of antibodies to Helicobacter IgG (antibodies in the blood - only if eradication of this microbe has not been carried out previously).
If the presence of Helicobacter pylori infection is detected, it must be eliminated with the help of antibiotics.
If there is B12 deficiency and/or atrophy of the body or fundus of the stomach, in addition to testing for Helicobacter, the doctor will always examine the patient for the presence of autoimmune gastritis. In this case, blood is taken for antibodies to gastric parietal cells and intrinsic Castle factor.
Currently, there is no specific treatment for autoimmune gastritis; only observation and elimination of vitamin and mineral deficiencies are indicated.
Patients with reduced gastric acidity, depending on the location of the atrophy, may be prescribed vitamin B12 for life (usually an intramuscular injection once a month), iron supplements, calcium supplements, folic acid, as well as other macro- and microelements, depending on their deficiency in a particular person. patient.
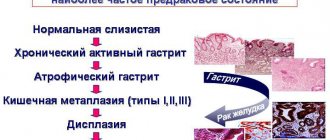
Patients with atrophic gastritis have an increased risk of developing stomach cancer and should undergo regular FGDS with biopsy (at least once every 3 years).
As for medications containing gastric enzymes (such as acidin, pepsin), the effectiveness of their use has not been proven, they are not mentioned in any recommendations, and their use refers rather to alternative medicine. Also, the effectiveness of any specific diet for low stomach acidity has not been proven, so meals should be regular, comply with modern ideas about proper nutrition, and also take into account the patient’s individual food tolerance (if any foods cause pain or other unpleasant sensations, it is recommended to avoid eating them).
Diagnostics
One of the key methods for determining the acidity of the stomach is to conduct a urease breath test to identify the bacterium Helicobacter pylori. Also, PCR and ELISA studies are performed to identify antibodies to this microorganism. Other mandatory research methods for suspected gastritis with high acidity include:
- Endoscopic examination of the stomach (gastroscopy). Using this method, the condition of the stomach, esophagus and duodenum is assessed. If necessary, during the examination, fragments of the mucous membrane are taken (biopsy).
- Intragastric pH-metry. To conduct the study, a pH-metric transnasal probe is used, which is connected to an autonomous recording unit. If the pH of the gastric contents is less than 1.5 units, then the diagnosis of hyperacid gastritis is confirmed.
An ultrasound examination of the abdominal organs may be prescribed as an auxiliary examination method.
Causes of hypoacid gastritis
The reasons due to which this disease appears can be external and internal.
External ones include:
- abuse of tobacco products and alcoholic beverages;
- improper diet, spicy, fried, fatty, smoked foods;
- abuse of medications with side effects on the gastric mucosa;
- harmful effects of chemicals and radioactive substances;
Internal include:
- gastrointestinal pathologies and disorders of the immune system;
- impaired metabolism, liver, pancreas and thyroid glands;
- various genetic abnormalities in the development of the mucous membrane.
Hypoacid gastritis most often affects adults and males. Children and women are less susceptible to this disease.
Treatment
Information on how to reduce stomach acidity should be obtained from a gastroenterologist. Any options for self-medication at home using improvised means are not only ineffective, but can also lead to the development of complications. For symptoms of gastritis with high acidity, diet and treatment include exclusion from the diet of fried and fatty foods, smoked meats, fast food, alcohol, canned meat, fish and vegetables, spices, seasonings, and sauces. You should eat in small portions, 4-5 times a day. Dishes must be prepared mainly by steaming or boiling. In case of increased acidity of the stomach, diet No. 1 according to Pevzner is prescribed.
For symptoms of gastritis with low acidity, treatment and diet include recipes for dishes that stimulate the acid-forming function of the stomach.
To treat high stomach acidity, traditional medicine uses the following groups of pharmaceuticals:
- Antibacterial drugs that are effective for hyperacid gastritis caused by the bacterium Helicobacter pylori.
- Enveloping agents.
- Proton pump inhibitors.
- Antacids.
- H2 histamine blockers.
- Bismuth preparations.
To maintain normal gastric acidity, it is important to maintain a balance of normal gastric microflora. For this purpose, it is recommended to use metaprebiotics, which contain a natural nutrient substrate for gastric and intestinal bacteria. Metaprebiotic Stimbifid Plus helps not only restore the balance of normal gastric and intestinal microbiota, but also promotes the eradication (destruction) of Helicobacter pylori. Also, metaprebiotic components accelerate the process of restoration of the gastric epithelium.
Symptoms and signs of the disease
The symptoms of such gastritis are associated with the severity of the disease. At the very beginning, they may not be noticeable at all. But later complaints with hypoacid gastritis are as follows:
- pain in the upper abdomen (sometimes radiating under the ribs on the left side);
- feeling of discomfort (feeling of heaviness, bloating);
- belching “rotten eggs”, metallic taste in the mouth, tongue with a gray coating;
- poor appetite;
- frequent diarrhea or constipation;
- nausea, excessive salivation;
- chronic fatigue, headaches, low performance;
- weight loss, changes in sleep patterns.
During a severe exacerbation, other signs may be added: rapid heartbeat, fainting.
How to diagnose hypoacid gastritis
If you notice similar symptoms, you should consult a specialist in the field of gastroenterology for diagnosis. To determine the clinical picture and make a correct and accurate diagnosis, the doctor usually conducts an examination, finds out complaints and prescribes tests and studies, as a result of which the type of pathology and how affected the gastric mucosa is determined. To determine chronic hypoacid gastritis use:
- visual examination of the stomach using a gastroscope (gastroscopy);
- endoscopic biopsy (taking material for biopsy);
- pH-metry of the acidity of secreted gastric juice;
- blood tests and coprogram.
Having collected a complete picture as a result of instrumental and laboratory studies, the doctor proceeds to drawing up a treatment program.
How is acidity determined?
If a person is worried about stomach pain, he is interested in how to find out whether the acidity of the stomach is increased or decreased.
The most physiological method for determining whether a person has increased or decreased acidity is to conduct intragastric pH-metry, which allows you to determine the level of acidity directly in the gastrointestinal tract. Such a study is carried out using acidogastrometers - special pH devices equipped with probes and sensors. This method is suitable for determining acidity in different parts of the stomach. Depending on the task that the diagnostician sets himself, determining what kind of environment in the stomach can be:
- short-term – lasts for several hours;
- express assessment – within 20 minutes;
- daily – assessment of acid production throughout the day;
- endoscopic – the study is carried out during endoscopic diagnosis.
The aspiration method is also used. When using it, the contents of the stomach are taken using a fractional probe, which is used to collect gastric secretions from the stomach and intestines. However, during the process, the stomach contents from different zones are mixed, and as a result, the diagnostician receives a distorted result, which is only approximate.