Pharmacological properties of the drug Eligard
Leuprorelin acetate is a synthetic non-peptide analogue of natural gonadotropin-releasing hormone, which, with prolonged use, inhibits the secretion of pituitary gonadotropin and inhibits testicular steroidogenesis in men. It is more effective than the natural hormone and its effects are reversible after stopping treatment. The administration of leuprorelin acetate initially leads to an increase in circulating levels of LH and FSH, resulting in an increase in the levels of gonadal steroids, testosterone and dihydrotestosterone in men for some time. With prolonged use of leuprorelin acetate, the levels of LH and FSH decrease. In men, testosterone levels drop to castration levels (50 ng/dL). This occurs within 3–5 weeks after the start of treatment. The average testosterone level after 6 months of treatment is for leuprorelin acetate 7.5 mg - 6.1 (±0.4) ng/dl and leuprorelin acetate 22.5 mg - 10.1 (±0.7) ng/dl, respectively, which is comparable to its level after bilateral orchiectomy. In all patients participating in the clinical study, when using leuprorelin acetate 7.5 mg, the castration level was achieved after 6 weeks (in 94% of patients before the 28th day and in 98% before the 35th day); leuprorelin acetate 22.5 mg - in all patients the castration level was achieved after 5 weeks (in 99% of them - before the 28th day). Most patients had testosterone levels below 20 ng/dL. Prostate-specific antigen levels decreased by 94% with a dose of 7.5 mg for 6 months and by 98% with a dose of 22.5 mg, respectively. Research results have shown that with long-term treatment, testosterone levels remain below castration levels for up to 7 years and even until the end of life. Absorption : in patients with advanced prostate carcinoma, after the first injection of leuprorelin acetate 7.5 mg, the maximum concentration of leuprorelin in the blood serum increases sharply to 25.3 ng/dL 4-8 hours (Cmax) after injection; after administration of leuprorelin acetate 22.5 mg - Cmax increases to 127 ng/dl after 4.6 hours. After an initial increase after each injection (plateau phase from 2 to 28 days after administration of leuprorelin acetate 7.5 mg and from 3 to 84 days after administration of leuprorelin acetate 22.5 mg), serum levels remained relatively stable for leuprorelin acetate 7.5 mg 0.28-1.67 ng/ml and leuprorelin acetate 22.5 mg - 0.2-2.0 ng/ ml. There are no data on the accumulation of the substance with repeated injections. Distribution : The mean volume of distribution of leuprorelin after intravenous administration to healthy male volunteers was 27 L. Binding to human plasma proteins in vitro for leuprorelin acetate 7.5 mg was 43-49%, for leuprorelin acetate 22.5 mg - 47-49%, respectively. Elimination : When 1 mg of leuprorelin acetate was administered intravenously to healthy volunteers, the average clearance was 8.34 L/h with a final half-life of 3 hours. Elimination studies have not been conducted.
The role of Eligard in the treatment of prostate cancer
| Konstantin Mikhailovich Figurin Doctor of Medical Sciences, Professor of the Department of Urology of the Russian Cancer Research Center named after. N.N. Blokhin RAMS [email protected] |
| Alexander Vladimirovich Khachaturyan Researcher, Department of Urology, Russian Cancer Research Center named after. N.N. Blokhin RAMS [email protected] |
Prostate cancer (PCa) in 2007 ranked 4th in Russia (8.9%) in the structure of cancer diseases and 1st place (60%) in terms of growth.
The choice of treatment method depends on the stage and extent of the tumor process. Thus, for stages T1–T3a in the absence of regional and distant metastases, radical surgery is optimal; for a group of patients with a good prognosis at these stages of the disease, the use of external beam radiation therapy is indicated.
Hormonal therapy for prostate cancer is widely used in patients with various stages of the disease: as a palliative treatment in patients with advanced and metastatic tumor processes, as neoadjuvant therapy in patients before radiation therapy, and as adjuvant therapy in patients with high-risk prostate cancer after surgical treatment and radiation therapy.
A major contribution to the development of hormonal therapy for prostate cancer was made by the American oncologist surgeon and physiologist Charles Brenton Huggins. In 1939, he conducted a series of experiments showing changes in the volume and chemical composition of prostate secretions in dogs under various hormonal conditions. In 1941, a series of his articles was published, which described the experience of treating patients with prostate cancer using estrogens or surgical castration. In 1966, C. Huggins was awarded the Nobel Prize in Physiology or Medicine for his discoveries in the field of hormonal treatment of prostate cancer. Prostate adenocarcinoma is a hormone-dependent tumor that is represented by three cell populations:
- hormonal-dependent, the growth of which requires androgenic stimulation;
- hormonally sensitive, growing without androgen stimulation, but slowing down their growth in the absence of androgens;
- hormonally insensitive, the growth of which is not affected by androgenic stimulation. Thus, the main focus of scientists’ work in developing methods of hormonal therapy for prostate cancer was various ways to reduce testosterone levels in order to block tumor growth. For this, the following methods were used:
- surgical castration;
- estrogen-based drugs;
- luteinizing hormone-releasing hormone (LHRH) agonists;
- LHRH antagonists;
- antiandrogens;
- alpha-reductase inhibitors;
- use of ketokenazole.
It should be noted that the significant disadvantages of the first two methods include psychological trauma in patients and the impossibility of intermittent therapy during surgical castration; gynecomastia, increased risk of cardiovascular complications and thromboembolism in patients receiving estrogens.
In 1974, leuprorelin, a synthetic non-peptide analogue of natural gonadotropin-releasing hormone, was first synthesized. Gonadotropic hormones belong to the subclass of tropic hormones of the anterior pituitary gland, the physiological function of which is to regulate the functioning of the gonads. This event can be considered a breakthrough in hormonal therapy for PCa, since the use of LHRH agonists allowed testosterone levels to be achieved below 50 ng/dL, which was equivalent to performing surgical castration. However, the side effects were less pronounced than with estrogen treatment.
Side effects of LHRH agonists include hot flashes, decreased libido and erectile dysfunction, and decreased bone mineral density.
In 1989, the use of LHRH agonists in the form of depot preparations was first proposed. In this case, leuprorelin is injected into the fatty tissue in the form of a reconstituted solution and forms a depot, exerting an effect over a period of 1 to 6 months, depending on the dosage of the drug.
In the modern use of LHRH agonists in the treatment of patients with prostate cancer, the drug Eligard, the active substance of which is leuprorelin, is widely used.
The table below shows data from various authors on the use of Eligard in the form of a depot in various dosages.
Table 1. Use of Eligard in the form of a depot in various dosages
Currently, the castration testosterone level is considered to be 20 ng/dL. The use of Eligard makes it possible to achieve this level in 95% of cases, which is an advantage of the drug compared to traditional LHRH analogues. To understand how Eligard works, consider the physiological chain: hypothalamus - pituitary gland - testicles - prostate gland. Luteinizing hormone releasing factor LHRH, also called gonadotropin-releasing hormone (GnRH), is a hypothalamic neurohormone and is produced by neurosecretory cells of the hypothalamus.
LHRH stimulates the anterior pituitary gland, which leads to the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) into the systemic circulation. Administration of LHRH agonists leads to a short-term increase in the secretion of gonadotropic hormones, the so-called flare syndrome. Then comes desensitization of the LHRH receptors of the pituitary gland, which leads to inhibition of its gonadotropic function. At 3–5 weeks after leuprolide administration, testosterone levels decrease to castration levels of 50 ng/dL. The advantage of Eligard is its various dosages, allowing you to create a depot of the drug for 1 month - 7.5 mg, 3 months - 22.5 mg, 6 months - 45 mg.
Foreign authors conducted a number of studies to determine the possibilities of using Eligard in various dosages - 7.5; 22.5 and 45 mg.
The Perrez-Mareno study included 120 patients, of whom 117 (97.5%) received Eligard therapy at a dosage of 7.5 mg once a month for 6 months. PSA levels ranged from 0.1 to 639.0 ng/ml, with a mean PSA level of 32 ng/ml. Upon reaching 42 days from the start of the study, all patients achieved a castration testosterone level of less than 50 ng/dl. After 6 months of therapy, in 96% of patients, the PSA level dropped below 4 ng/ml, the average PSA level was 3.2 ng/ml. The average testosterone level at the same time was 6.12 ng/dL, with values in the group ranging from 3 to 27 ng/dL.
Chu et al. in 2002, they conducted a multicenter study that lasted 6 months, which included 117 patients with prostate cancer. Of these, 111 received treatment with Eligard at a dosage of 22.5 mg every 3 months throughout the study. As is the case with the use of this drug at a dosage of 7.5 mg, the “flash” effect, accompanied by an increase in the concentration of LH in the blood, was observed in the first week of treatment. Then, over the course of 2–4 weeks, the LH level decreased to normal, and on the 48th day it was practically undetectable.
On the 35th day from the start of the study, all patients achieved a castration testosterone level of less than 50 ng/dl. At the 6th month of treatment, 104 of 111 patients had testosterone levels less than 20 ng/dL, which was 94%. The average testosterone level at this time was 10.1 ng/dl.
The average PSA level before treatment was 86.4 ng/ml and decreased by more than 98% at the 6th month of treatment, reaching a level of 1.7 ng/ml. In 2006, Crawford et al. conducted a multicenter 12-month study that included 111 patients with prostate cancer, of which 103 (93%) completed the study completely. The average period during which testosterone reached castration levels below 50 ng/dL was 21 days.
After a year from the start of the study, 99% of patients had testosterone levels below 50 ng/dL and 88% below 20 ng/dL. The average PSA level for the same period was 1.2 ng/ml. When analyzing the side effects of Eligard, the authors noted hot flashes from mild (33.3%) to moderate (24.35%), burning in the injection area (14.4 and 0.9%, respectively), nausea (7.2 and 4.5 %), testicular atrophy (5.4%) and gynecomastia (3.6%). The uniqueness of Eligard lies in the use of the innovative Atrigel system. The packaging of the drug includes 2 syringes: the first contains the active substance - leuprorelin acetate lyophilisate, the second contains the biodegradable polymer Atrigel.
To prepare a solution of the drug, it is necessary to remove the syringes from the packaging, remove the protective caps from them and carefully connect them. Then mix the solution by alternately pressing the syringe pistons. After mixing, it is necessary to disconnect the syringe in which Atrigel was located and fix a sterile needle in its place.
The drug is injected into the tissue of the anterior abdominal wall; its entry into the blood vessels is unacceptable.
Under the influence of water, the Atrigel polymer precipitates in the subcutaneous fatty tissue and the drug hardens. As the drug gradually biodegrades, the active substance is released. Thanks to the use of Atrigel, it became possible to create dosage forms with a higher content of the drug substance - 7.5, 22.5 and 45 mg.
B. Tombal, in his article from 2005, cites the opinion of a number of authors that the use of this administration system in combination with high doses of the drug leads to an improvement in its pharmacokinetics, which provides a better therapeutic effect - a decrease in testosterone to a castration level of less than 20 ng/dL observed in 95% of patients.
Abouelfadel et al. They also note that the use of the drug in the form of a 6-month depot helps to significantly improve the quality of life of patients. Eligard has a stable and well-controlled effect; its use reduces the frequency of local adverse events in the injection area and requires fewer doctor visits, which is important for patients with limited mobility and those living in remote areas. The drug can also be used for neoadjuvant therapy of prostate cancer.
Thus, Eligard is a convenient and effective drug for the treatment of patients with prostate cancer; it is also the only depot drug from the group of LHRH agonists, which can be administered once every 6 months, which significantly improves the quality of life of patients.
0
Your rating: No
Use of the drug Eligard
Eligard 7.5 mg is prescribed as a subcutaneous injection once a month. The administered solution forms a drug depot, which ensures the constant release of leuprorelin acetate for 1 month. Eligard 22.5 mg is prescribed as a subcutaneous injection once every 3 months. The administered solution forms a drug depot, which ensures the constant release of leuprorelin acetate for 3 months. Treatment of hormone-dependent prostate cancer with Eligard is a long-term treatment and should not be interrupted after improvement or remission occurs. Introduction. The contents of two pre-filled sterile syringes should be mixed immediately before administering Eligard as a subcutaneous injection. Getting the drug into an artery or vein is unacceptable! As with other drugs prescribed subcutaneously, the site of Eligard administration must be periodically changed. The response to treatment with the drug should be monitored by observing the clinical manifestations of the disease and measuring the level of prostate-specific antigen in the blood serum. If the patient's response to treatment is insufficient, it is advisable to check whether testosterone levels have reached or remain at castration levels. The mixture is prepared according to the instructions. After mixing, the solution should be administered immediately. Unused solution should not be used. Clinical studies have not been conducted in patients with hepatic or renal impairment.
Prostate cancer (PCa) in 2009 in the structure of cancer incidence in Russia occupied 2nd place or 10.7% and first place or 153.27% in terms of the increase in incidence over the past 10 years. [1] The choice of treatment for prostate cancer depends on the stage and extent of the tumor process. Thus, for stages T1-T3a in the absence of regional and distant metastases, radical surgery is optimal; for a group of patients with a good prognosis at these stages of the disease, the use of external beam radiation therapy is indicated. Hormonal therapy for prostate cancer is widely used in patients with various stages of the disease: as a palliative treatment in patients with advanced and metastatic tumor process, as neoadjuvant therapy in patients before radiation therapy, and as adjuvant therapy in patients with high-risk prostate cancer after surgery. treatment and radiation therapy. The American oncologist and physiologist Charles Brenton Huggins made a great contribution to the development of hormone therapy for prostate cancer. In 1939, he conducted a series of experiments showing changes in the volume and chemical composition of prostate secretions in dogs under various hormonal conditions. In 1941, a series of his articles were published, which described the experience of treating patients with prostate cancer using estrogens or surgical castration. In 1966, Charles Huggins was awarded the Nobel Prize in Physiology or Medicine for his discoveries in the field of hormonal treatment of prostate cancer. Prostate adenocarcinoma is a hormone-dependent tumor that is represented by three cell populations
- hormonal-dependent, the growth of which requires androgenic stimulation.
- hormonally sensitive, growing without androgen stimulation, but slowing down their growth in the absence of androgens.
- hormonally insensitive, the growth of which is not affected by androgenic stimulation.
Thus, the main focus of scientists’ work in developing methods of hormone therapy for prostate cancer was various ways to reduce testosterone levels in order to block tumor growth. For this, the following methods were used:
- surgical castration.
- estrogen-based drugs.
- luteinizing hormone releasing hormone (LHRH) agonists.
- LHRH antagonists.
- anti-androgens.
- alpha reductase inhibitors.
- use of ketokenazole.
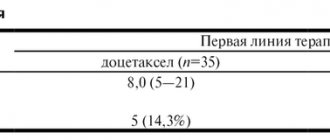
It should be noted that the significant disadvantages of the first two methods include psychological trauma in patients and the impossibility of intermittent therapy during surgical castration; gynecomastia, increased risk of cardiovascular complications and thromboembolism in patients receiving estrogens. In 1974, leuprorelin, a synthetic non-peptide analogue of natural gonadotropin-releasing hormone, was first synthesized. Gonadotropic hormones belong to the subclass of tropic hormones of the anterior pituitary gland, the physiological function of which is to regulate the functioning of the gonads. This event can be considered a breakthrough in hormonal therapy for PCa, since the use of LHRH agonists allowed testosterone levels to be achieved below 50 ng/dL, which was equivalent to performing surgical castration. However, the side effects were less pronounced than with estrogen treatment. Side effects of LHRH agonists include hot flashes, decreased libido and erectile dysfunction, and decreased bone density. In 1989, the use of LHRH agonists in the form of depot drugs was first proposed. In this case, leuprorelin is injected into the fatty tissue in the form of a reconstituted solution and forms a depot, exerting an effect for 1 to 6 months, depending on the dosage of the drug. In the modern use of LHRH agonists in the treatment of patients with prostate cancer, the drug Eligard, the active substance of which is leuprorelin, is widely used. The table below shows data from various authors on the use of Eligard depot in various dosages: Table 1. Clinical studies using Eligard
| Leuprorelin dosage | Injection volume (ml) | Castration testosterone level | Authors | |
| 50 ng/dl | 20 ng/dl | |||
| 7.5 mg, once a month | 0.250 | 100% | 98% | Perez-Mareno 2002 |
| 22.5 mg, once every 3 months | 0.375 | 98% | 84% | Chu 2002 |
| 45.0 mg, once every 6 months | 0.375 | 99% | 88% | Crawford 2006 |
Currently, the castration testosterone level is considered to be 20 ng/dL. The use of Eligard makes it possible to achieve this level in 95% of cases, which is a competitive advantage of the drug in comparison with traditional LHRH analogues. To understand how Eligard works, consider the physiological chain: hypothalamus - pituitary gland - testicles - prostate gland. Luteinizing hormone releasing hormone (LHRH), also called gonadotropin releasing hormone (GnRH), is a hypothalamic neurohormone and is produced by neurosecretory cells of the hypothalamus. LHRH stimulates the anterior pituitary gland, which leads to the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) into the systemic circulation. Administration of LHRH agonists leads to a short-term increase in the secretion of gonadotropic hormones, the so-called “flare phenomenon”. Then comes desensitization of the LHRH receptors of the pituitary gland, which leads to inhibition of its gonadotropic function. At 3-5 weeks after the administration of leuprorelin, the testosterone level decreases to castration level - 50 ng/dl. The advantage of Eligard is its various dosages, allowing you to create a depot of the drug for 1 month - 7.5 mg, 3 months - 22.5 mg, 6 months - 45 mg. Foreign authors conducted a number of studies to determine the possibilities of using Eligard in various dosages - 7.5 mg, 22.5 mg and 45 mg. The Perrez-Mareno study included 120 patients, of whom 117 (97.5%) received Eligard therapy at a dosage of 7.5 mg once a month for 6 months. PSA levels ranged from 0.1 to 639.0 ng/ml, with a mean PSA level of 32 ng/ml. Upon reaching 42 days from the start of the study, all patients achieved a castration testosterone level of less than 50 ng/dl. After 6 months of therapy, in 96% of patients, the PSA level dropped below 4 ng/ml, the average PSA level was 3.2 ng/ml. The average testosterone level at the same time was 6.12 ng/dl, with values in the group ranging from 3.0 to 27.0 ng/dl. [4] Chu et al. in 2002, they conducted a multicenter study that lasted 6 months, which included 117 patients with prostate cancer. Of these, 111 received treatment with Eligard at a dosage of 22.5 mg every three months throughout the study. As with the use of this drug at a dosage of 7.5 mg, the “flash” effect, accompanied by an increase in the concentration of luteinizing hormone (LH) in the blood, was observed in the first week of treatment. Then, over 2-4 weeks, the LH level decreased to normal levels, and on the 48th day it was practically undetectable. On the 35th day from the start of the study, all patients achieved a castration testosterone level of less than 50 ng/dl. At the 6th month of treatment, 104 of 111 patients had testosterone levels less than 20 ng/dL, which was 94%. The average testosterone level at this period was 10.1 ng/dl. The average PSA level before treatment was 86.4 ng/ml and decreased by more than 98% at the 6th month of treatment, reaching a level of 1.7 ng/ml. [5] In 2006, Crawford et al. conducted a multicenter 12-month study, which included 111 patients with prostate cancer, of which 103 (93%) completed it completely. The average time for testosterone to reach castration levels below 50 ng/dL was 21 days. After a year from the start of the study, 99% of patients had testosterone levels below 50 ng/dL and 88% below 20 ng/ml. The average PSA level at the same period was 1.2 ng/ml. When analyzing the side effects of Eligard, the authors noted mild (33.3%) to moderately severe (24.35%) hot flashes, burning in the injection area (14.4% and 0.9%, respectively), nausea (7.2% and 4.5%), testicular atrophy (5.4). %) and gynecomastia (3.6%). [6] The uniqueness of Eligard lies in the use of the innovative Atrigel system. The packaging of the drug includes two syringes: one contains the active substance - leuprorelin acetate lyophilisate, the second contains the biodegradable polymer Atrigel. To prepare a solution of the drug, it is necessary to remove the syringes from the packaging, remove the protective caps from them and carefully connect them. Then mix the solution by alternately pressing the syringe pistons. After mixing, it is necessary to disconnect the syringe in which Atrigel was located and fix a sterile needle in its place. The drug is injected into the tissue of the anterior abdominal wall; its entry into the blood vessels is unacceptable. Under the influence of water, the Atrigel polymer precipitates in the subcutaneous fatty tissue and the drug hardens. As the drug gradually biodegrades, the active substance is released. Thanks to the use of Atrigel, it became possible to create dosage forms with a higher content of the drug substance - 7.5, 22.5 and 45 mg. B. Tombal, in his article from 2005 [7], cites the opinion of a number of authors that the use of this administration system in combination with high doses of the drug leads to an improvement in its pharmacokinetics, which provides a better therapeutic effect - a decrease in testosterone to a castration level of less than 20 ng /dl is observed in 95% of patients. Abouelfadel et al. [3] also note that the use of the drug in the form of a 6-month depot helps to significantly improve the quality of life of patients. Eligard has a stable and well-controlled effect; its use reduces the frequency of local adverse events in the injection area and requires fewer doctor visits, which is important for patients with limited mobility and those living in remote areas. The drug can also be used for neoadjuvant therapy of prostate cancer. Thus, Eligard is a convenient and effective drug for the treatment of patients with prostate cancer; it is also the only depot drug from the group of LHRH agonists, which can be administered once every 6 months, which significantly improves the quality of life of patients. Literature:
- "Malignant neoplasms in Russia in 2009 (morbidity and mortality)." Ed. IN AND. Chissova, V.V. Starinsky, G.V. Petrova.? M.: FGU “MNIOI im. P.A. Herzen Ministry of Health and Social Development of Russia", 2011.
- A subcutaneous delivery system for the extended release of leuprolide acetate for the treatment of prostate cancer. Ramon Perez-Marrero, Robert C Tyler Expert Opin. Pharmacother. (2004) 5(2):447-457
- Leuprorelin depot injection: patient considerations in the management of prostatic cancer. Zinelabidine Abouelfadel, E David Crawford. Therapeutics and Clinical Risk Management 2008:4(2) 513–526
- A six-month, open label study assessing a new formulation of leuprolide 7.5 mg for testosterone suppression in patients with prostate cancer. Perez-Marrero, Chu FM Clin. Ter. 2002;24 1092-14
- A clinical study of 22.5 mg LA – 2550: a new subcutaneous depot delivery system for leuprolide acetate for the treatment of prostate cancer. Chu FM, Jayson M, Dineen MKJ Urol 2002; 168:1199-203
- A 12-Month Clinical Study of LA-2585 (45.0 MG): A New 6-Month Subcutaneous Delivery System for Leuprolide Acetate for the Treatment of Prostate Cancer. E. David Crawford, Oliver Sartor, Franklin Chu, Ramon Perez, Gary Karlin, J. Steve Garrett. J Urol 2006; 175:533-536
- How good to current LHRH agonists control testosterone? Can this be improved by Eligard? B. Tombal, R. Berges. Eur. Urol. Suppl. 4 (2005) 30-36
Side effects of the drug Eligard
They mainly arise in connection with the specific pharmacological action of leuprorelin acetate, namely: an increase and decrease in hormonal levels. From the cardiovascular system : hot flashes, blood pressure lability, loss of consciousness, peripheral edema, pulmonary embolism, palpitations, chills, shortness of breath. From the nervous system: hypoesthesia, dizziness, headache, insomnia, disorders of taste, vision, smell, voluntary movements, sleep disturbance, depression, amnesia, and hyperesthesia of the skin. From the gastrointestinal tract: nausea, dry mouth, constipation or diarrhea, flatulence. From the respiratory system : rhinorrhea. From the genitourinary system : dysuria, nocturia, oliguria, urinary tract infections, softness and hypertrophy of the mammary glands, testicular atrophy, testicular pain, infertility, hematuria, acute urinary retention, gynecomastia, impotence, soreness of the mammary glands, decreased libido. From the musculoskeletal system : arthralgia, back pain, muscle cramps, myalgia, muscle weakness. From the laboratory parameters : changes in the general blood test, increased levels of creatinine, phosphokinase, ALT, TG in the blood, prolongation of blood clotting time and prothrombin time, in some cases - thrombocytopenia and leukopenia. Common side effects are malaise and fatigue. Local side effects : very often - transient minor burning/tingling after injection; often - pain, erythema, bruising, itching; rarely - induration and ulceration. In general, these side effects are minor and quickly transient. There may also be a skin rash, alopecia, and increased sweating. Changes in glucose tolerance have been reported.
Special instructions for the use of Eligard
Studies regarding the effect of Eligard on the ability to drive vehicles and operate complex machinery have not been conducted. Due to a feeling of fatigue, dizziness, visual impairment (side effects of treatment or a consequence of the underlying disease), the ability to drive a car and operate machinery may deteriorate. Leuprorelin acetate, like other gonadotropin-releasing hormone agonists, causes a transient increase in serum concentrations of testosterone, dihydrotestosterone and acid phosphatase during the first week of treatment. Patients may experience worsening or new symptoms, such as bone pain, neurological disorders, hematuria, ureteral obstruction, or bladder outlet obstruction. These symptoms usually go away with continued treatment. Ureteral obstruction and spinal cord compression have been reported with the use of gonadotropin-releasing hormone agonists, which may lead to paralysis with or without fatal complications. In cases of spinal cord compression or renal failure, standard treatment for these complications is carried out. Careful monitoring should be carried out during the first few weeks of treatment in patients with metastases in the spine and/or brain, as well as patients with urinary tract obstruction. An additional antiandrogen should be prescribed 3 days before starting leuprorelin therapy and used during the first 2–3 weeks of treatment (to prevent the consequences of the initial increase in serum testosterone levels). In case of a hormone-resistant tumor (lack of clinical improvement despite a decrease in testosterone levels), further therapy with Eligard does not make sense. There have been reports of decreased bone density in men who have undergone bilateral orchiectomy or who have been treated with a gonadotropin-releasing hormone agonist. Antiandrogen therapy increases the risk of fractures due to osteoporosis. In addition to long-term testosterone deficiency, the development of osteoporosis can also be influenced by the following factors: old age, smoking, alcohol consumption, excess body weight, and insufficient exercise. Changes in glucose tolerance have been observed in some patients treated with gonadotropin-releasing hormone agonist, so patients with diabetes mellitus require careful monitoring. After surgical castration, Eligard does not lead to a further decrease in serum testosterone levels in men.