Characteristic features of antifungal agents
Drugs that have the properties of eliminating fungus are called antifungal, antibacterial, or antimycotic. The products are effective in combating pathogenic microflora that causes fungal growth. Medicines have a wide spectrum of action, which helps treat several diseases. The appointment should take place after consultation with the attending physician to prevent the formation of unpleasant consequences.
There are drugs:
- made from natural products;
- created from synthetic components through a chemical compound.
In recent years, the diagnosis of fungal infection has been heard much more often, due to many reasons. The infection can be caused by taking antibiotics that weaken the natural microflora in the intestines, which leads to decreased immunity. The cause of the disease can be poor-quality shoes, lack of hygiene and a number of other factors. There are several types of drugs in this group depending on the scope and strength of action. There are creams, ointments, solutions and tablets that help cope with fungal pathogens.
Antimycotics have fungastatic and fungicidal effects. Drugs in tablet form are prescribed to kill fungal spores. Pathogenic microflora is blocked at the reproduction stage, without spreading throughout the body. This action is ensured due to the fungistatic properties of the agents in this group.
The active substance of antimicrobial drugs penetrates the blood, moving through the vessels to the lesion. The action time is quite long, which contributes to the complete destruction of spores of pathogenic microflora. The incoming components and the active substance are excreted by the urinary system.
Each group of drugs is responsible for a specific scope of action, which is associated with a set of ingredients during production:
- Ketoconazole helps block fungal synthesis at the cell membrane level;
- Itraconazole has a detrimental effect on ergosterol, which is one of the important components of the fungus;
- fluconazole stops the production of new fungal spores and destroys existing ones;
- terbinafine works with ergosterol at the formation stage, which is suitable for preventing infection;
- griseofulvin prevents fungal cells from multiplying, which has a beneficial effect on well-being.
Modern methods of treating patients with mycoses of the feet
What is the reason for the increase in the incidence of mycoses of the feet? What are the possible consequences of foot mycoses?
| Figure 1. Intertriginous-dyshidrotic mycosis of the feet |
Mycoses of the feet (MS) are fungal diseases (dermatophytic, yeast, mold), affecting mainly the skin and nails of the feet (hands), similar in clinical, epidemiological, pathogenetic and therapeutic respects.
Their treatment is an urgent medical problem, primarily due to their widespread distribution.
At least 20-30% of patients suffering from the most common dermatoses (eczema, neurodermatitis, psoriasis), and almost every second patient with somatic and neuroendocrine pathologies have MS. In the general population, their frequency ranges from 5-10 to 15-20%.
The increase in the incidence of MS is currently due to unfavorable socio-economic and environmental living conditions, an increase in immunodeficiency conditions, insufficient medical care, and deterioration of epidemiological control.
Acute forms of MS with hyperemia, edema, vesiculopustules, cracks and erosions (Fig. 1) are painful, make it difficult to wear shoes and move, and when complicated by lymphangitis, lymphadenitis, mycids - poor general health, fever, adynamia.
| Figure 2. Hypertrophic type of nail damage. Nails are thickened, crumble, and look like wood eaten by bugs |
Chronic MS causes disfiguring changes in the nails of the hyper-, normo- and atrophic (onycholytic) types (Fig. 2, 3, 4). In 15-25% of patients with MS, the fungal process spreads primarily to large skin folds (Fig. 5, 6), then to other areas of the skin (Fig. 7 a, b).
Along with fairly superficial mycotic rashes, deep skin-subcutaneous nodes can form. They are most often localized on the skin of the legs (Fig. 8), less often on the face (Fig. 9), and even less often on the scalp. In such patients, vellus or long hair of the ectotrix or endoectotrix type are often affected.
The consequences of MS, especially long-term ones, are quite serious.
Firstly, under the influence of fungi and their metabolic products (enzymes, antibiotics, pigments, toxins), polyvalent sensitization is formed. This affects the increase in the frequency of allergic changes in the skin, mucous membranes and blood vessels: occupational allergic and eczematous complications, drug intolerance, especially penicillin antibiotics, are three times more frequent; Vasculitis and polynoses become more pronounced. Superinfection and mycogenic sensitization aggravate the course, provoke more frequent relapses of seborrheic and atopic dermatitis, eczema and psoriasis, hemoderma and dermatoses with impaired keratinization processes.
| Figure 3. Normotrophic type of nail damage. Stripes and spots in the nails. Maintains normal shape and consistency of nails |
Secondly, ubiquitous bacteria easily penetrate through erosions and cracks in the macerated, loosened stratum corneum of patients with MS (“the gate of infection”). Almost three times more often, patients with MS experience bacterial complications - from pyodermatitis to recurrent erysipelas of the legs with severe complications - lymphostasis and elephantiasis in 40% of them. Bacterial complications are characterized by resistance to therapy, since bacteria, under the influence of antibiotic substances produced by fungi, acquire increased resistance to antibiotics.
| Figure 4. Atrophic (onycholytic) type of nail damage. Nails separate from the nail bed |
Thirdly, in MS, the frequency of plantar warts increases fourfold compared to the general population (from 0.6 to 2.4%). Calluses and hyperkeratosis almost always form in areas where mycotic eruptions are located, especially in areas of pressure. This is facilitated by the aflatoxin-like substances of the fungi themselves, as well as their enhancement of the growth and development of papillomaviruses, the causative agents of palmoplantar and anogenital warts.
Treatment of patients with MS should be comprehensive and include antifungal drugs for general (systemic) and external use, as well as pathogenetic agents.
Prescribing systemic antimycotics to MS patients with onychomycosis triples the effectiveness of treatment.
| Figure 5. Iris-shaped foci of mycosis |
Currently, practical mycology has at its disposal three effective systemic antimycotics - azole compounds: itraconazole (Orungal) and fluconazole (Diflucan), as well as an allylamine derivative - terbinafine (Lamisil). Daily and course doses of each drug are given in Table 1. Most often, lamisil and orungal are used in the treatment of patients with MS. Both drugs have fungicidal and fungistatic activity against dermatophytes, yeasts and molds. The use of both drugs makes it possible to achieve success in 80-94% of cases in the treatment of MS patients with multiple onychomycosis in an outpatient setting and without subjecting patients to a painful nail removal procedure. Both drugs are keratinotropic, lipophilic, quickly enter the stratum corneum of the skin and nails and remain there for a long time, allowing for relatively short courses of therapy.
Preference, especially in the treatment of patients with dermatophytic MS with onychomycosis, should be given to lamisil due to its greater selectivity of action against fungi and fewer adverse reactions and complications.
| Figure 6. Garland-shaped foci of mycosis in the axillary region |
The differences are related to the mechanisms of action of the drugs. Although both of them interfere with the synthesis of ergosterol in the cytoplasmic membranes of fungal cells, this occurs at different levels of sterol metabolism.
Lamisil acts early, at the level of the squalene epoxidase cycle, inhibiting the enzyme - fungal squalene epoxidase, which is 10 thousand times more sensitive than the similar human enzyme. Orungal acts at later stages of sterol metabolism, inhibiting the enzyme 14-a-dimethylase, which is involved not only in the synthesis of fungal ergosterol, but also cholesterol, steroidogenic hormones, enzymes, and some vitamins. In this regard, even with a gentle regimen of using orungal, a decrease in libido is possible in 0.2% of patients, and potency in 0.2% of patients. Lamisil has no negative effects on endocrine organs.
Both drugs are metabolized in the liver using cytochrome P-450, but orungal, in addition, interacts with this enzyme, disrupting the metabolism of many medications that it affects in one way or another (Table 2). Liver complications from increased levels of liver enzymes to the possibility of developing hepatitis are higher with Orungal than with Lamisil (0.3-5% versus 0.1%, respectively).
Table 1. General antifungal agents for mycoses of the feet
| A drug | Company (country) | Release form | Dosage regimen |
| Lamisil | Novartis (Switzerland) | Tablets of 0.125 and 0.25 g in a package of 14 pcs. | Adults are prescribed 1 tablet (250 mg) per day daily: for onychomycosis of the hands - for 6-8 weeks, for total damage to many nails - from 3 to 6 months, or in 10-day courses of 250 mg/day. daily with 10-day breaks, or 250 mg/day. 1 month daily, next month - 250 mg/day. every other day and then 250 mg/day. 1 time per week before nails grow (4-6 months) |
| Orunggal | Janssen-Cilag (Belgium) | Gelatin pink-blue capsules of 0.1 g in a package of 15 capsules | Prescribe 2 capsules (200 mg) morning and evening, 4 capsules (400 mg) per day for 1 week, break - 3 weeks. If the skin of the feet is affected, 1-2 cycles are necessary, with onychomycosis of the hands and distal onychomycosis of the feet - 3 cycles, with total damage to many nails - 5-6 cycles. |
| Diflucan | Pfizer (USA) | Capsules 0.05; 0.1; 0.15; 0.2 g in packs of 1, 7 and 10 capsules | Prescribe 150 mg once a week: for onychomycosis of the hands for 8-10 weeks, for onychomycosis of the feet for 20-36 weeks. |
| Forkan | Agio (India) | Capsules of 0.05 and 0.15 g in packs of 1, 7 and 10 capsules | Prescribe 150 mg once a week: for skin lesions - for 8 weeks, onychomycosis of the hands - 8-10 weeks, for onychomycosis of the feet - 20-36 weeks. |
It is impossible not to take into account the different possibilities of absorption of antimycotics in the gastrointestinal tract. If lamisil does not require any special conditions for this, then for optimal absorption of orungal an acidic pH of gastric juice is necessary.
The lipophilicity of Lamisil, its secretion by the sebaceous glands, pronounced antibacterial and anti-inflammatory properties, along with antifungal properties, as well as the connection with chylomicrons and lymphatic transport determine its special effectiveness in patients with complicated forms of dermatophytosis - infiltrative-suppurative, follicular-nodular with the formation of mycotic granulomas, neutrophilic abscesses .
Table 2. Possible interactions between antifungals and other medications
| Antifungal drugs | Other medications |
| Lamisil | Cimetidine, rifampicin |
| Orungal | Erythromycin, tetracycline, amphotericin B, cyclosporine, cimetidine, terfenadine, hydroquinone, isoniazid, rifampicin, phenobarbital, phenotoin, carbamazepine, hypoglycemic agents, midazolam, triazolam, warfarin, tolbudamide, nifidipine and other calcium conduction blockers, antacids and H2 antagonists, oral contraceptives |
Therapy with Lamisil in a daily dose of 250 mg cures patients with MS with skin lesions in two weeks in 100% of cases, mycoses with lesions of the nails of the hands in 6-8 weeks in 94% of cases. When toenails are affected, the results of treatment depend on the nature, severity, area of the lesion, and duration of therapy. If single nails from the distal and/or lateral edges are changed, cure occurs after 9-12 weeks of therapy in 94-100% of patients. There was an increase in the percentage of those cured from 88% after 12 weeks of treatment to 94% with further observation for 48 weeks after completion of treatment. Total damage to many nails of the hypertrophic type requires a longer course of therapy, up to 22-24 weeks, to cure 80-94% of patients.
We proposed a slightly different regimen for the use of Lamisil, taking into account its long-term absorption into the nails, the stability of the concentration in them, despite continued use for more than 8-12 weeks, and the need to sanitize the deep tissues of the matrix and nail bed. In our opinion, it is advisable to take Lamisil until completely healthy nails grow back. With a constant daily dose of 250 mg, Lamisil is taken daily only in the first month, every other day in the next month, and once a week in all subsequent months. At the same time, nails are sanitized with a variety of fungicidal-keratolytic agents. We studied the effectiveness of therapy using this method for two years using the example of 36 somatically burdened patients with multiple total lesions of the nails. Cure occurred in 80.6% of them. No side effects were noted, except for complaints of weakness and drowsiness in some patients. Shifting the administration of Lamisil to the evening hours neutralized these phenomena. The proposed scheme for the use of Lamisil deserves further study, since it allows, with a reduced course dose, to obtain a high percentage of cure and avoid adverse reactions and complications.
| Figure 7. Common foci of mycosis in the same patient |
Orungal is currently prescribed in a pulse mode - during the week of each month, two capsules (200 mg) in the morning and evening, followed by a three-week break.
After 3-6 cycles of therapy in this regimen, cure is observed in 70-85.6% of patients with MS, including those with multiple onychomycosis caused by a combined dermatophyte-yeast flora.
Adverse reactions from lamisil therapy occur in the first weeks of use and depend little on the daily dose. They are 10.4% at 250 mg per day and 11% at 500 mg per day. Adverse reactions and complications from orungal range from 7 to 12.5%, depending on the dose and duration of use.
Most often, both drugs cause dyspepsia, abdominal pain, discomfort, nausea, and rarely vomiting. Some patients taking Lamisil note disturbances in taste sensitivity.
The second most common place is occupied by skin itching and skin rashes (erythematosquamous, urticarial, eczema-like, acneiform, extremely rarely Stevens-Johnson syndrome).
| Figure 9. Infiltrative-suppurative lesion |
Some patients, when taking either drug, experience minor headaches, dizziness, malaise, decreased attention, weakness, and drowsiness.
In addition to the above-mentioned antifungal agents, the bistriazole drug fluconazole (Diflucan) is used to treat patients with MS with onychomycosis. It is prescribed 150 mg once a week for 8-24 weeks for onychomycosis of the hands, 20-36 weeks for onychomycosis of the feet. The drug is well tolerated and highly effective; it provides cure in 83-92% of cases.
Therapy with systemic antimycotics should be supplemented with external fungicidal-keratolytic agents, especially when nails are affected.
If there are contraindications to the prescription of systemic antifungal drugs, as well as if only the skin and single nails from the distal or lateral edges are affected, you can limit yourself to only external antifungal drugs.
To cure affected nails, keratolytic and fungicidal agents are usually alternated. For example, they clean the nails after softening them using a 20% urea patch (ureaplast), and then soak them in fungicidal solutions (5% tincture of iodine, iodoxun No. 1-3, 1% solution of exoderil or clotrimazole, fitex, nitrofungin ).
Antifungal varnishes that deserve attention are: batrafen (8% ciclopiroxalamine) and loteryl (5% omorolfine). Their antifungal effect is combined with penetrating properties. This is important, since the pathogens of onychomycosis not only penetrate the entire nail, but also penetrate into the deep areas of the nail bed. The use of varnishes for 3-6 months provides a cure for 53-66.7% of MS patients with onychomycosis. The release form and regimen of use of medications for the treatment of nails are given in table. 3.
Table 3. Drugs for the treatment of fungal nail infections
| A drug | Firm, institution (country) | Dosage form. Active beginning | Release form | Mode of application |
| Ureaplast Mikoplast | TsKVI (Russia) | Patch. Urea 20% | 25 g in jars | Cut off or scrape off the top (shiny) layer of the nail and apply the plaster mass in a layer of 1-2 mm, fix it with an adhesive plaster. Nails are cleaned after 2-3 days. The number of cleanings depends on the area and nature of the nail damage. Next, the nails are treated with fungicidal drugs for 7-10 days, as well as softening drugs (ureaplast, soap and soda baths) |
| Mycospor | Bayer AG (Germany) | Ointment. Bifonazole 1%, urea 40% | Nail set: ointment in a 10 g dispenser, strips of adhesive plaster, scraper | The composition is applied to the nails under an adhesive plaster once a day. Clean your nails the next day (24 hours later) after a 10-15% soap and soda bath. The number of cleanings depends on the area and severity of nail damage. Apply 1% mycospore cream to the cleaned nail bed once a day. |
| Lotseryl Lotsetar | Roche Switzerland | Varnish. Omorolfine 5% | Nail set: 2.5 - 5 ml of polish, swabs soaked in alcohol, in foil; spatulas, nail files | The varnish is applied to a previously flattened nail, cleaned after application of 20% ureoplast (see above). The nail is degreased with an alcohol swab. The varnish is applied once a week, drying thoroughly. Clean your nails once a week. Duration of varnish application: from 2 months. up to 1 year |
| Batrafen | Hoechst (Germany) | Varnish. Cyclopyroxalamine 8% | Nail set: varnish in a bottle of 3 and 6 ml; tampons soaked in alcohol in foil; spatulas, nail files | The varnish is applied to the flattened and cleaned nail after it has been degreased with an alcohol solution in the 1st month. 3 times a week, in the 2nd - 2 times a week, from the 3rd month. — 1 time per week. The total duration of treatment should not exceed 6 months. |
To treat the skin of MS patients, both old, well-proven drugs (iodine, sulfur, tar, quinosol, undecylenic, salicylic, lactic, benzoic acids) and new drugs of the azole, allylamine, morpholine series are widely used. They are used in the form of solutions, lotions, powders, aerosols, creams, ointments, and collodion compositions. Domestic multicomponent formulations often include penetrant dimethyl sulfoxide (dimexide).
For acute inflammatory phenomena in the form of edema, hyperemia, exudation and eczematization, lotions with disinfectants and astringents are prescribed. For these purposes, you can use a combination of antimycotics with corticosteroids (creams Triderm, Lotriderm, Travocort, Pimafucort, Mycozolon, Pivazone), salts or metal oxides (dactosin, cincostatin). Lamisil spray relieves acute inflammation well. The pronounced anti-inflammatory effect of Lamisil is enhanced by the rapid evaporation of propellants. The drug does not cause irritation when applied to cracks and erosion of blisters and pustules formed after opening. Foci of mycosis resolve after 7-10 days of daily irrigation with Lamisil spray, and fungi are no longer detectable microscopically.
| We must not forget that patients with MS, especially the common forms, represent a constant mobile source of dispersal of fungi in the environment. Therefore, persons suffering from MS are not allowed to visit sports and sanatorium-resort institutions, as well as sports and recreation centers. If the skin and nails of the hands are affected, work in any sphere of public service is unacceptable (order of the Ministry of Health of the Russian Federation dated March 14, 1996) |
In patients with squamous manifestations of MS, as well as after acute inflammatory phenomena have subsided, a variety of fungicidal agents are used. Along with the above, medications based on clotrimazole (canesten, clotrimazole, candid, fungicide, canizon), econazole (pevaril, ecodax, ekalin), miconazole (daktarin, mycotar), ketoconazole (nizoral), isoconazole (travogen) are widely used.
Allylamine derivatives deserve high praise - powder, 1% solution and cream of naftifine (exoderil), as well as 1% cream and aerosol of terbinafine (Lamisil).
Active antimycotics of other groups, which also have penetrating properties, include powder, 1% solution and cream of tolnaftate, 1% solution and cream of batrafen, 0.5% cream of omorolfine.
Patients with MS often develop plantar warts. To destroy them, use electro-laser cryodestruction, cauterization with potassium permanganate and trichloroacetic acid, two to six times treatment with a 30% solution of hydrogen peroxide in one or two days, with a 25% solution of podophyllin once a day, three days in a row, five to ten minute treatment (until uniform yellow coloration) with the ampoule preparation Solcoderm. You can use the milky juice of celandine or dandelion, which is applied to the wart (protecting the surrounding skin) up to 20 times during the day.
Pathogenetic therapy, on the one hand, increases the effectiveness of treatment with systemic and external antimycotics in patients with MS, and on the other, reduces adverse reactions and complications. These remedies are as varied as the pathology against which MS occurs.
To correct immunological disorders in patients with MS, five-day courses of therapy with methyluracil 0.5 g three times a day are used; diucifon 0.2 g twice a day; three-day cycles of levamisole therapy at 150 mg with weekly breaks; 10-day courses of tactivin, 1 ml of 0.1% solution daily, subcutaneously; Thymalin 5 mg or thymogen 100 mg in a 0.25% solution of novocaine intramuscularly every other day; polyoxidonium 6 mg in a 0.25% novocaine solution twice a week, for a course of 10 injections. A combination of immunocorrectors with adaptogens and antioxidants is advisable: ginseng, eleutherococcus, zamanikha, dibazol, sea buckthorn oil, linetol, vitamin E, essentiale. Useful food supplements: Stimulin with pantocrine, ginseng, radiola rosea, leuzea; apilactin with royal jelly and pollen; propovit with propolis and citric acid; mumivit with purified mumiyo.
Patients with exudative forms of MS are prescribed hyposensitizers: calcium preparations, 30% sodium hyposulfite solution, 1 tbsp. spoon three times a day; 10-day courses of histoglobulin injections from 0.25 to 2 ml every other day. It is effective to administer small doses (no more than 1 ml) of autologous blood intramuscularly every other day, in five-day cycles with three-day intervals, for a course of 2-3 cycles.
Taking into account the frequent vascular pathology, patients with MS are prescribed angioprotectors and drugs that improve tissue trophism: nicotinic acid preparations, including long-acting ones (enduracin), andecalin, trental, troxevasin; physiotherapeutic procedures: inductothermy of sympathetic ganglia, electro- and iontophoresis with iodine preparations, ultrasound in the area of regional lymph nodes. Self-massage of the lower extremities and “stretching” gymnastics of the spine are useful.
To eliminate dystrophic changes in the nails, monthly courses of therapy with zinc oxide 50 mg three times a day or 1% copper sulfate 8 drops three times a day in combination with vitamin and microelement complexes such as Complivit, Vitrum, Unicap, Duovit, Multitabs, endura.
The lack of sulfur and sulfur-containing amino acids is compensated with the help of foods rich in these substances (eggs, cottage cheese, herbs, as well as mineral waters containing them).
The lack of gelatin and pectin, which causes brittleness and splitting of nails, is compensated for with fish and meat jellies, fruit and berry jellies, marmalade, and fortified drinks with pectin.
For dry, ichthyotic skin, the use of vitamins A in the form of retinol acetate, retinol palmitate, aevit, or beta-carotene in the form of 2% water-soluble vetoron, 10-15 drops per day, or carinate, 1 tablet, is indicated. twice a day. Food supplements such as rialam, splat-clamin, and VEL spirulina are useful.
More complete information on various aspects of mycoses of the feet can be gleaned from the book of Candidate of Medical Sciences V. M. Rukavishnikova.
The monograph examines the epidemiology of foot mycoses in modern conditions, the mechanisms of their development; Typical and, most importantly, atypical variants are described in detail. Much attention is paid to skin and nail damage due to eczema, psoriasis, lichen planus, pyococcal infections, scabies, syphilis and their differences from fungal ones.
The book describes in detail effective antifungal agents and new dosage forms in the form of varnishes and shampoos, considering their properties, mechanism of action, tolerability, compatibility with other medications, adverse reactions and complications.
Data on effective methods of preventing foot mycoses are presented, listing new disinfectants, antifungal fabrics, cosmetic and hygiene preparations and devices, vitamin-microelement complexes and food additives.
The book is illustrated with photographs of mycoses and dermatoses in the palmoplantar localization, microscopic histological and ultrastructural preparations of fungi, diagrams and tables, and is equipped with a recipe for therapeutic and prophylactic agents usually used for the treatment and prevention of mycoses of the feet.
Full information about the publication can be obtained at: Moscow, st. Pyatnitskaya, 50/2, tel: (095) 956-8221, JSC "MSD".
Rules for the use of antifungal agents
When prescribing drugs of this group, the patient must be prepared to strictly follow the doctor’s recommendations. You cannot make prescriptions or change the dosage on your own - this will lead to relapse or serious complications. The tablets have a wide spectrum of action, so almost all body systems are involved in treatment. It is necessary to drink the medicine at the same time - this will enhance the therapeutic effect.
The medications are taken during meals with sufficient amounts of water. Before prescribing antimicrobial tablets, the doctor takes into account the state of the gastric microflora - in case of low acidity, taking tablets from the azole group is prohibited. But if the doctor decides to urgently use these medications, then they must be combined with a liquid with a high acid content - orange or lemon juice. Women during pregnancy and breastfeeding should avoid taking medications from the azole group.
The choice of antimycotic drugs in the complex treatment of patients with oral candidiasis
M. O. Nagaeva Candidate of Medical Sciences, Associate Professor of the Department of Therapeutic Dentistry of the State Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation
M. G. Chesnokova Doctor of Medical Sciences, Professor, Department of Microbiology, Virology and Immunology of the State Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation
I. V. Anisimova Candidate of Medical Sciences, Assistant of the Department of Therapeutic Dentistry of the State Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation
The true incidence of oral candidiasis in Russia is unknown, since it is not officially registered, so publications on this problem in the domestic literature are few [5]. Colonization of mucous membranes by Candida fungi in practically healthy people ranges from 15 to 40% and can increase to 80% against the background of any pathology.
The relevance of research
Increased growth of the fungus, leading to the development of candidiasis, is observed when local and systemic immunity is impaired.
Exogenous infection is also possible. Superficial mucosal candidiasis also occurs in practically healthy individuals. Deep candidiasis develops with severe immunodeficiency against the background of candidal stomatitis, glossitis or pharyngitis. Fungi penetrate into the blood through damaged mucous membranes, causing fungemia and sepsis.
Treatment of candidiasis should be individual for each patient, taking into account the localization and severity of the process and the possibility of a chronic stage of the disease, taking into account the immune status and the presence of other diseases. Etiotropic treatment is the most important component of the complex treatment of patients with oral candidiasis. Eradication of the pathogen is the first step, after which one can proceed to the prevention of relapses and correction of local and general predisposing factors. Etiotropic therapy can be local (in the case of isolated candidiasis of the oral cavity) and systemic (if the infectious process spreads to the lower parts of the digestive tract, skin, and other mucous membranes). Systemic therapy for candidiasis of the oral mucosa is prescribed, as a rule, only for certain indications: chronic hyperplastic candidiasis, erosive-ulcerative form of candidiasis; oral candidiasis due to diabetes mellitus, immunodeficiency state; with ineffective local therapy.
The list of antifungal drugs is huge, and every year new drugs appear in the form of rinses, solutions, and tablet forms. The main group of specific drugs consists of antimycotic agents, but today the sensitivity of Candida fungi to them is variable and often insufficient. However, susceptibility testing is not considered routine, is not always available, and is not generally considered a standard practice in patient management. Susceptibility tests are considered useful in cases where we are dealing with deep infections caused by non-albicans Candida species. In these cases, especially if the patient has already been previously treated with antifungal azoles, the possibility of microbiological resistance should be considered.
The purpose of our study was to determine the sensitivity to antimycotics of strains of fungi of the genus Candida isolated from patients with oral candidiasis.
Materials and methods
At the Department of Therapeutic Dentistry of Omsk State Medical Academy and State Clinical Hospital No. 1 in Omsk, we conducted a clinical examination of 48 patients with complaints of pain and burning in the oral mucosa. The examination was carried out according to the algorithm proposed by Nedoseko V.B., Anisimova I.V. (2003) [3].
As part of a comprehensive examination of patients, a microbiological examination of material obtained by scraping from the mucous membrane of the dorsum of the tongue was carried out. The biomaterial was collected before treatment was prescribed using a dry sterile swab without the use of a transport medium. Before taking microbiological material, patients were advised to refrain from eating and hygiene procedures. The microbiological material was placed in a sterile transport tube and delivered to the bacteriological laboratory within two hours. In order to isolate facultative anaerobic microorganisms and yeast-like fungi of the genus Candida, the biomaterial was inoculated on nutrient media. A series of successive twofold dilutions of the material from 102 to 1012 was prepared. To isolate staphylococci, the corresponding dilutions were inoculated onto yolk-salt agar; to identify streptococci, inoculation was carried out on blood agar with sodium azide. To isolate bacteria of the genus Haemophilus and Neisseria, the material was inoculated on chocolate agar with lincomycin, enterobacteria on Endo medium, and enterococcal agar was used to detect enterococci.
To isolate fungi of the genus Candida, the biomaterial was inoculated on Sabouraud and Candiselect medium.
To identify fungi, cultural properties were assessed on Candisilect medium; biochemical identification was carried out using the Auxocolor test system.
To determine the sensitivity of yeast-like fungi of the genus Candida to antimycotic drugs (nystatin, amphotericin B, clotrimazole, fluconazole, itraconazole), the classical disk diffusion method and Fungitest were used.
To set up the disk diffusion method, a culture suspension was prepared in an isotonic sodium chloride solution, 1 ml of the suspension was poured onto the surface of the Mueller-Hinton medium. The results were recorded by measuring the diameter of the zone of inhibition of culture growth to the antimycotic.
To conduct the Fungitest, a suspension of fungi was prepared from a pure culture grown on Sabouraud’s medium—the first calibrated inoculum with a turbidity corresponding to the standard of 3 x 106 fungi/ml.
A 1:20 dilution of the primary solution was added to the suspension medium to obtain a standard inoculum (103 CFU/ml). The standard inoculum was added to the wells of the microplate. Incubated for 48 hours.
Research results and discussion
When examining 48 patients, we identified 23 patients with signs of oral candidiasis. All patients complained of pain, burning, and dry mouth. In 60.8% (14 patients) clinical signs of chronic atrophic candidiasis were detected (Fig. 1), in 39.2% (9 patients) chronic hyperplastic candidiasis was detected (Fig. 2).
Rice. 1. Patient K., 65 years old. Chronic atrophic candidiasis of the oral cavity
Rice. 2. Patient I., 69 years old. Chronic hyperplastic candidiasis of the oral cavity. Candida infection
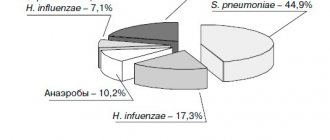
As a result of microbiological examination of material from the oral cavity of 23 patients, 75 strains of opportunistic microorganisms were isolated and identified (48 strains of Candida albicans, 27 strains of opportunistic bacteria). Most of the isolated microorganisms were sown in significant concentrations (104 CFU - 29.3%, 106 CFU 40.0%, 108 CFU - 22.7%). At the same time, Candida albicans was most often found in association with S. epidermidis (104 CFU, 106 CFU), E. faecalis (104 CFU, 106 CFU), S. salivarius (106 CFU). When determining the sensitivity of Candida albicans fungi to antimycotic drugs, 18 (37.5%) strains with signs of resistance were identified. The greatest resistance of the isolated fungal strains was determined to nystatin (33% of sensitive strains) (Fig. 3).
Rice. 3. Sensitivity to antimycotics in the disk diffusion method
The sensitivity of Candida albicans to itraconazole, ketoconazole, 5-fluorocytazine and miconazole was 100% (Fig. 3, 4).
Rice. 4. Sensitivity to antimycotics in the Fungitest method
When determining sensitivity to fluconazole using the disk diffusion method, 94.4% of strains sensitive to fluconazole were identified. When using the Fungitest method, sensitivity to fluconazole at concentration 8 was 88.8%, to fluconazole at concentration 64 - 100%. 94.4% of C. albicans strains were sensitive to clotrimazole. All isolated strains were sensitive to amphotericin B(64); only 66.6% of strains were sensitive to amphotericin B(8). When determining sensitivity to amphotericin B by the disk diffusion method, 77.4% of the studied strains showed sensitivity.
Conclusion
When prescribing etiotropic treatment for patients with oral candidiasis, it is necessary to take into account the results of a mycological study with determination of sensitivity to antifungal drugs, since the isolated strains of Candida albicans showed resistance to antifungal drugs in 37% of cases. When choosing a method for determining sensitivity to antifungal drugs, it is necessary to take into account that the disk diffusion method is indicative; Fungitest has pronounced specificity and high sensitivity. In addition, the methods differ in the spectrum of antimycotics. Thus, to ensure the optimal choice of antifungal drugs in practice, we can recommend the use of two methods - both disc diffusion and the Fungitest method.
- Anisimova I.V. Clinic, diagnosis and treatment of diseases of the oral mucosa / I.V. Anisimova, V.B. Nedoseko, L.M. Lomiashvili. - M.: Medical book, 2008. - 194 p.
- Borovsky E.V. Diseases of the mucous membrane of the oral cavity and lips / E.V. Borovsky, A.L. Mashkilleyson. - M.: Medpress, 2001. - 320 p.
- Nedoseko V.B. Algorithm for examining a patient with diseases of the mucous membrane of the oral cavity and lips /V. B. Nedoseko, I. V. Anisimova // Institute of Dentistry. — 2003, No. 2 (19). - pp. 32-36.
A complete list of references is in the editorial office
Azole group tablets
It is quite difficult to cure mycosis, but with a correctly calculated dose of drugs it is possible. Here you just need to follow the prescribed regimen and not miss a dose. This group is produced on the basis of synthetic components. The tablets are effective in the fight against lichen, fungal infections of nails and skin with hair, problems in the intimate area, and candidiasis. The effect of the substance is fungistatic, which is especially useful when infected with bacteria from the Candida series. The most effective drugs in this group are Itraconazole, Ketoconazole and Fluconazole.
Indications for use
Antifungal drugs are used for diseases caused by pathogenic fungi - mycoses: deep (or systemic) mycoses, in which fungi affect internal organs and the central nervous system - aspergillosis, cryptococcosis, coccidioidomycosis, histoplasmosis, blastomycosis; superficial mycoses (or dermatomycosis) of the skin, scalp, nails - pityriasis versicolor, microsporia, trichophytosis, epidermophytosis, onychomycosis, mycosis of the ear canal.
In addition, antifungal drugs are used for candidiasis of the mucous membranes of the oral cavity, pharynx, esophagus, skin, genital organs - vaginal candidiasis, candidiasis of internal organs.
Polyene drugs against fungus
Products from this series are used to combat fungi of the genus candidiasis, but can be used to treat trichomonas, dermatomycitis and pseudoallescheria. Tablets are considered to have a broad spectrum of action, which expands the possibilities of application. You can treat fungus of the skin, mucous surfaces - stomatitis, thrush, lesions in the gastrointestinal tract. You cannot take polyenes on your own - this requires precise dosage and the correct dosage regimen. The best drugs in this group are Griseofulvin, Nystatin, Levorin and Amphotericin B.
Antifungal and anti-inflammatory drugs
07.03.2018
Salicylic ointment is a medicine indicated for chronic eczema , psoriasis , dyskeratosis, ichthyosis, oily seborrhea, acne , warts, calluses . It is applied to the affected surface 2-3 times a day.
The drug is contraindicated in case of hypersensitivity to salicylic acid and in childhood. Side effects are rare. These are local reactions in the form of skin rash, itching, burning, as well as allergic reactions .
Amphotericin B is an antifungal antibiotic intended for the treatment of candidiasis of the skin and mucous membranes, as well as candidiasis of the gastrointestinal tract and internal organs, chronic granulomatous and disseminated forms of candidiasis , coccidioidosis, histoplasmosis, chromomycosis, mold mycoses. The ointment is applied to the affected areas of the skin in a thin layer 2-4 times a day. The course of treatment for candidiasis of skin folds is 1-3 weeks, for diaper rash in children - 1-2 weeks, for lesions of the interdigital spaces and paronychia - 2-4 weeks.
liver and kidney dysfunction , diseases of the hematopoietic system, diabetes mellitus , and hypersensitivity to its components. When used externally, a burning sensation, tingling sensation, skin flushing, and rarely dry skin are possible.
Nystatin is an antifungal drug intended for the prevention and treatment of diseases caused by yeast-like fungi of the genus Candida, candidiasis of the skin , mucous membranes ( mouth , vagina ) and internal organs (gastrointestinal tract, lungs , kidneys ). For prophylactic purposes, it is prescribed to prevent the development of candidiasis during long-term treatment with penicillin and antibiotics of other groups, especially with oral use of tetracycline antibiotics, chloramphenicol, neomycin and others, as well as in weakened and depleted patients. When treating fungal infections of the mucous membranes and skin, nystatin ointment can be used. It can be combined with oral nystatin. For candidiasis of the lower intestines , colpitis and vulvovaginitis, rectal suppositories and vaginal globules containing 250,000 and 500,000 units each are used. They are administered 2 times a day, respectively, into the rectum or vagina ; The average course duration is 10–14 days.
Contraindications and side effects are the same as when taking amphotericin B.
Fluconazole is a broad-spectrum antifungal agent that has a powerful antifungal effect against the causative agents of candidiasis , thrush , some forms of lichen , dandruff (Candida, Microsporum, Cryptococcus neoformans, Trichophyton). Fluconazole is used for skin mycoses (including mycoses of the feet, groin area), pityriasis versicolor , onychomycosis, deep endemic mycoses, systemic cadidosis, cryptococcosis, for the prevention of fungal infections in patients with reduced immunity .
For candidiasis , mycoses of the feet, body, and groin area, 150 mg is prescribed once a week, treatment duration is 2–4 weeks. For cryptococcal infections, candidemia, disseminated candidiasis , and other invasive candidiasis infections, 400 mg is prescribed on 1 day, then 200–400 mg 1 time per day.
For deep endemic mycoses - 200-400 mg per day for a long time up to 2 years. The duration of therapy is determined individually; it can be 11–24 months for coccidioidomycosis, 2–17 months for paracoccidioidomycosis, 1–16 months for sporotrichosis, and 3–17 months for histoplasmosis. For children over one year of age, fluconazole is administered once a day at the rate of 1–3 mg/kg (for candidiasis of the mucous membranes) and 3–12 mg/kg (for systemic candidiasis or cryptococcosis) depending on the severity of the disease.
Fluconazole is contraindicated in case of hypersensitivity to its components, pregnancy , or in children under 1 year of age.
When using the drug, side effects are possible: nausea , headache, discomfort in the abdominal cavity, increased activity of liver enzymes, severe liver , headache, dizziness ; rarely - convulsions, agranulocytosis, leukopenia, thrombocytopenia; very rarely - skin rash, anaphylactic reactions.
Pimecrolimus is an anti-inflammatory drug indicated for atopic dermatitis ( eczema ). It is recommended for both short-term and long-term use in adults, adolescents and children (from 3 months). Prescribed externally 2 times a day.
The drug is contraindicated in case of hypersensitivity to its components.
When taking pimicrolimus, side effects are possible: burning at the site of application of the cream, local reactions (irritation, itching and redness of the skin, rash, pain, paresthesia, peeling, dryness, swelling, skin papillomas, boils), skin infections (folliculitis), suppuration, deterioration course of the disease, herpes simplex, dermatitis caused by the herpes simplex virus (eczema herpes ), molluscum contagiosum. In rare cases, alcohol intolerance appears (immediately after drinking alcohol, facial , rash, burning, itching or swelling were usually observed).
Dioxomethyltetrahydropyrimidine + sulfadimethoxine - trimecaine + chloramphenicol - a combined drug with antimicrobial, anti-inflammatory and local anesthetic effects, accelerating wound healing. Indicated for the treatment of purulent wounds in the first phase of the wound process. It is applied topically in the form of applications. Sterile gauze pads are soaked in the ointment and loosely filled into the wound. Dressings are performed daily until the wound is completely cleansed of purulent-necrotic masses. The ointment can be injected into purulent cavities through a drainage tube using a syringe.
The drug is contraindicated in case of hypersensitivity to its components.
When used, local allergic reactions in the form of skin rash are possible.
Published in Medicines Premium Clinic
How to take tablets against fungal pathogens
Treatment with drugs of this group is carried out only under the supervision of the attending physician and on strict recommendations. It is impossible to violate the regime - this can provoke complications in the course of the disease. You should not change the dosage and regimen yourself. Tablets are part of a group of broad-spectrum drugs that affect almost all areas of the body during treatment.
Fungus of nails, skin and hair is one of the most common diseases detected during examination. The reasons for this are poor nutrition, environmental conditions and indiscriminate use of medications. Treatment is complex and takes a lot of time. The doctor makes combined prescriptions, which may include Nystatin, Itraconazole, Fluconazole, Clotrimazole, Ketoconazole. In each case, the scheme is selected individually - the age, physical data of the patient and tests are taken into account.
Candidiasis is a serious disease that quickly spreads throughout the body. The disease can be detected early with regular examination by a doctor. The initial form is easily treated by taking topical tablets. But for the acute stage, stronger drugs are required, where a course of drugs will be required for 14-21 days. Pimafucin, Diflucan and Clotrimazole are used for treatment.
Onychomycosis (nail fungus) can be eliminated with topical solutions, ointments and gels. If a large area is affected, the doctor may decide to prescribe broad-spectrum agents. In this case, Fluconazole, Ketoconazole, Nizoral, Itraconazole, Flucostat or Terbinafine are used. Here the doctor takes into account many factors - the site of infection, the degree of the disease, age and medical indications.
Mycoses of smooth skin
Among the widespread fungal diseases today, the most common are mycoses of smooth skin, such as microsporia, trichophytosis, lichen versicolor, mycosis of the feet (hands), and candidiasis. Sources of infection can be sick animals (cats, dogs, mouse-like rodents, cattle, etc.), as well as humans. In recent years, there has been an increase in the number of diseases caused by opportunistic fungi, among which superficial forms of candidiasis are most often recorded. Such a wide prevalence of these mycoses can be explained by the massive use of modern therapeutic agents, the environmental situation and other factors that reduce the body's defenses. One of the reasons for the significant prevalence of mycoses is the weakening of sanitary educational work in recent years. Due to insufficient awareness about the sources and ways of spreading infection, as well as adequate preventive measures, patients turn to the doctor late, and therefore mycoses become chronic, including in children suffering from mycoses of the scalp and smooth skin.
Microsporia is a fungal disease caused by various types of fungi of the genus Microsporum. In Russia, microsporia, which has spread over the last 50 years, is caused by a zoophilic fungus - fluffy microsporum (Microsporum canis), which parasitizes the skin of cats, dogs, and less often other animals. Infection from a sick person is observed in 2% of cases.
Epidemiology . Infection in 80-85% of cases occurs as a result of direct contact with a sick animal or through objects contaminated with the fur of these animals. Infection of children can also occur after playing in the sandbox, since the causative agent of microsporia is highly resistant to environmental factors and can remain viable in infected scales and hair for up to 7-10 years. Children often suffer from microsporia.
Clinic . After 5-7 days from the moment of infection, lesions appear on smooth skin, which can be observed on both open and closed parts of the body (children love to pick up animals and put them in bed with them). The lesions are round or oval in shape, pink or red, with clear boundaries, a raised ridge along the periphery, covered with blisters and thin crusts, with peeling in the center. The lesions are usually small, from 1 to 2 cm in diameter, single or multiple, sometimes merging. In 85-90% of patients, vellus hair is affected.
Treatment . If there are single foci of microsporia on smooth skin without damage to vellus hair, you can limit yourself to only external antifungal agents. The lesions should be lubricated with alcohol tincture of iodine (2-5%) in the morning, and sulfur-salicylic ointment (10% and 3%, respectively) should be rubbed in in the evening. You can rub the following antimycotics 2 times a day: mycozolon, mycoseptin, travogen or 1 time a day in the evening - mifungar cream, mycospor - until the clinical manifestations resolve. In case of multiple lesions of smooth skin and single lesions (up to 3) involving vellus hair, it is recommended to prescribe the antifungal antibiotic griseofulvin at the rate of 22 mg per 1 kg of the child’s body weight, in 3 doses after meals, in combination with exfoliating the stratum corneum of the epidermis in keratolytic lesions means (salicylic acid 3.0, lactic or benzoic acid 3.0, collodion up to 30.0). The lesions are lubricated with one of these products 2 times a day for 3–4 days, then 2% salicylic ointment is applied under compress paper for 24 hours, the detached scales of the stratum corneum of the epidermis are removed with tweezers and vellus hair is epilated. If during a control study carried out using a fluorescent lamp or microscope, affected hair is detected, the procedure is repeated. Detachment of the stratum corneum of the epidermis and manual hair removal of vellus hair can be carried out after using the “sealing” method. The lesions are sealed in a tile-like manner with strips of adhesive plaster for 2-3 days, this causes an aggravation of the process, which, in turn, facilitates hair removal.
The results of treatment for smooth skin microsporia are monitored using a fluorescent lamp or microscopic examination for fungi. The first control study is done after the resolution of clinical manifestations, then 3-4 days before the first negative test, and then after 3 days. The criteria for cure are resolution of the lesions, absence of luminescence and three negative tests on microscopic examination.
During the treatment, bed and underwear are disinfected: boiling in a soap-soda solution (1%) for 15 minutes (10 g of laundry soap and 10 g of caustic soda per 1 liter of water); ironing outerwear, furniture covers, and bedding five times with a hot iron through damp cloth.
Prevention. The main measure to prevent microsporia is compliance with sanitary and hygienic rules (you cannot use other people’s underwear, clothes, etc.; after playing with animals, you must wash your hands).
Trichophytosis is a fungal disease caused by various types of fungi of the genus Trichophyton. Trichophytons can be anthropophilic, parasitic on humans, and zoophilic, whose carriers are animals. Anthropophilic trichophytons include Trichophyton (Tr.) tonsuraus and Tr. violaceum, to zoophiles - Tr. mentagrophytes var gypseum and Tr. verrucosum.
Epidemiology. With superficial trichophytosis, caused by anthropophilic fungi, infection occurs through close contact with a sick person or indirectly through household items. Often children become infected from their mother, grandchildren from grandmothers suffering from a chronic form of the disease. The incubation period lasts up to a week. In zooanthroponotic trichophytosis, the sources of infection are sick animals: cattle, rodents. The highest incidence of this type of trichophytosis is recorded in the fall, which is associated with field work: it is at this time that the likelihood of infection through hay and straw increases. The incubation period ranges from 1–2 weeks to 2 months.
Clinic. On smooth skin with superficial trichophytosis, lesions can appear on any part of the skin - face, neck, chest, forearms. They have clear boundaries of a round or oval shape, with a raised ridge along the periphery of a bright red color; they are larger in size than in microsporia. The lesions are reddish-bluish in color, with peeling, nodules on the surface; in the chronic form, they develop on the skin of the buttocks, knee joints, forearms, less often the back of the hands and other parts of the body; the lesions do not have clear boundaries. Lamellar peeling is observed on the skin of the palms and soles. Vellus hairs are often affected.
With trichophytosis, caused by zoophilic fungi, the disease on the skin can occur in three forms: superficial, infiltrative and suppurative. Lesions are usually located on open areas of the skin. With a superficial form, they are round or oval in shape, with clear boundaries, a raised ridge along the periphery, on which bubbles, crusts, a pink center, and a bright red ridge are visible. The lesions are larger in size than with microsporia. Sometimes they are located around natural openings - eyes, mouth, nose. In the infiltrative form, the lesions rise above the skin level and are accompanied by inflammatory phenomena - infiltration. The suppurative form is characterized by the development of tumor-like formations, bright red in color, covered with purulent crusts due to the addition of a bacterial infection. When the lesion is compressed, pus is released from the hair follicles and pain is noted. The disease is accompanied by a violation of the general condition, sometimes the temperature rises. After the resolution of clinical manifestations, cicatricial atrophy of the skin remains at the site of former lesions. Clinical forms of zooanthroponotic trichophytosis can transform into one another.
Diagnostics. The diagnosis of trichophytosis is established on the basis of the clinic and when the fungus is detected during microscopy of pathological material, and the type of pathogen is determined using cultural examination.
Treatment. Treatment is carried out with antimycotics for external use. The lesions are lubricated with tincture of iodine (2-5%) during the day, and sulfur-salicylic ointment (10% and 3%, respectively) or mycoseptin is rubbed in in the evening. You can carry out monotherapy with ointment or cream (kanison, mifungar, mycozoral, mycospor (bifosin), exoderil, mycozoral, etc. In the infiltrative form, 10% sulfur-tar ointment is prescribed to resolve infiltration 2 times a day. Treatment of the suppurative form of trichophytosis begins with removing crusts from the affected area using bandages with 2% salicylic ointment, which are applied for several hours. After removing the crusts, vellus hair is epilated. Then apply lotions with solutions that have a disinfectant and anti-inflammatory effect (furacilin 1:5000, rivanol 1:1000 , potassium permanganate 1:6000, ichthyol solution (10%), etc.). As a result of this treatment, the hair follicles are freed from pus, inflammatory phenomena are reduced. Next, sulfur-tar ointment (5-10%) is prescribed for resorption of the infiltrate (5-10%) in the form of rubbing or under wax paper.After the infiltrate has resolved, antimycotics are used for external use (see superficial form of trichophytosis).In cases where vellus hair is affected in lesions on smooth skin, the stratum corneum of the epidermis is detached, followed by hair removal. To do this, you can use salicylic collodion (10-15%), milky-salicylic-resorcinol collodion (15%). If there is no effect, griseofulvin is prescribed orally at a daily dose of 18 mg per 1 kg of body weight, in 3 divided doses after meals daily until a negative test for fungi, then every other day. As an alternative method, terbinafine (Lamisil, Exifin) can be prescribed to adults 250 mg (1 tablet) once a day after meals every day, children weighing up to 20 kg - 62.5 mg, from 20 to 40 kg - 125 mg , over 40 kg - 250 mg in combination with antimycotics for external use.
The criteria for cure for trichophytosis are resolution of clinical manifestations and three negative fungal test results at three-day intervals.
Prevention. Prevention of trichophytosis depends on the type of pathogen. With superficial trichophytosis caused by anthropophilic fungi, the main preventive measure is to identify the source of infection, and it can be children suffering from superficial trichophytosis, or adults suffering from a chronic form of the lesion. In recent years, cases of chronic trichophytosis have been observed in middle-aged and older children. For suppurative trichophytosis, preventive measures are carried out jointly by medical workers, epidemiologists and veterinary services.
Mycosis of the smooth skin of the feet (hands). In a number of countries, up to 50% of the population suffers from mycosis of the feet. This disease is more common in adults, but in recent years it has often been observed in children, even infants.
Etiology. The main causative agents of mycosis of the feet are the fungus Trichophyton rubrum (T. rubrum), which is isolated in almost 90% of cases, and T. mentagrophytes var. interdigitale (T. interdigitale). Damage to the interdigital folds, which may be caused by yeast-like fungi, is recorded in 2-5% of cases. The anthropophilic fungus Epidermophyton floccosum is rarely isolated in our country.
Epidemiology. Infection with mycosis of the feet can occur in the family through close contact with a patient or through household items, as well as in a bathhouse, sauna, gym, or when using someone else's shoes and clothes.
Pathogenesis. The penetration of fungi into the skin is facilitated by cracks and abrasions in the interdigital folds caused by sweating or dry skin, abrasion, poor drying after water procedures, narrowness of the interdigital folds, flat feet, etc.
Clinic. Clinical manifestations on the skin depend on the type of pathogen and the general condition of the patient. The T.rubrum fungus can cause damage to the skin of all interdigital folds, soles, palms, dorsum of the feet and hands, legs, thighs, inguinal-femoral, intergluteal folds, under the mammary glands and axillary area, trunk, face, and rarely the scalp. The process may involve vellus and long hair, nail plates of the feet and hands. When the skin of the feet is affected, there are 3 clinical forms: squamous, intertriginous, squamous-hyperkeratotic.
The squamous form is characterized by the presence of peeling on the skin of the interdigital folds, soles, and palms. It can be flour-shaped, ring-shaped, lamellar. In the area of the arches of the feet and palms, an increase in the skin pattern is observed.
The intertriginous form is the most common and is characterized by slight redness and peeling on the lateral contact surfaces of the fingers or maceration, the presence of erosions, superficial or deep cracks in all folds of the feet. This form can transform into dyshidrotic, in which vesicles or blisters form in the area of the arches, along the outer and inner edges of the feet and in the interdigital folds. Superficial blisters open with the formation of erosions, which can merge, resulting in the formation of lesions with clear boundaries and oozing. When a bacterial infection is attached, pustules, lymphadenitis and lymphangitis occur. In the dyshidrotic form of mycosis, secondary allergic rashes are observed on the lateral and palmar surfaces of the fingers, palms, forearms, and shins. Sometimes the disease becomes chronic with an exacerbation in spring and summer.
The squamous-hyperkeratotic form is characterized by the development of foci of hyperkeratosis against the background of peeling. The skin of the soles (palms) becomes reddish-bluish in color, and pityriasis-like peeling is noted in the skin grooves, which extends to the plantar and palmar surfaces of the fingers. Pronounced ring-shaped and lamellar peeling may be detected on the palms and soles. In some patients, it is insignificant due to frequent hand washing.
In children, lesions of smooth skin on the feet are characterized by fine-plate peeling on the inner surface of the terminal phalanges of the toes, usually 3 and 4, or there are superficial, less often deep cracks in the interdigital folds or under the toes, hyperemia and maceration. On the soles, the skin may not be changed or the skin pattern may be enhanced; sometimes ring-shaped peeling is observed. Subjectively, patients are bothered by itching. In children, more often than in adults, exudative forms of lesions occur with the formation of blisters and weeping eczema-like lesions. They appear not only on the feet, but also on the hands.
Rubrophytia of smooth skin of large folds and other areas of the skin is characterized by the development of lesions with clear boundaries, irregular outlines, with an intermittent ridge along the periphery, consisting of merging pink nodules, scales and crusts, with a bluish tint (the color is bluish-pink in the center) . On the extensor surface of the forearms and shins, rashes can be located in the form of open rings. Lesions with nodular and nodular elements are often observed. The disease sometimes occurs as an infiltrative-suppurative trichophytosis (more often in men when localized in the chin area and above the upper lip). Foci of rubrophytosis on smooth skin can resemble psoriasis, lupus erythematosus, eczema and other dermatoses.
The fungus T. interdigitale affects the skin of the 3rd and 4th interdigital folds, the upper third of the sole, the lateral surfaces of the foot and toes, and the arch of the foot. This mushroom has pronounced allergenic properties. With mycosis of the feet caused by T. interdigitale, the same clinical forms of damage are observed as with rubrophytosis, but the disease is often accompanied by more pronounced inflammatory phenomena. In the dyshidrotic, less often intertriginous form, large blisters may appear on the skin of the soles and fingers, along with small blisters; in the case of bacterial flora, with purulent contents. The foot becomes edematous, swollen, and pain appears when walking. The disease is accompanied by an increase in temperature, deterioration of health, development of allergic rashes on the skin of the upper and lower extremities, torso, face, enlargement of the inguinal lymph nodes; the clinical picture is similar to that observed with eczema.
Diagnosis. The diagnosis is established on the basis of clinical manifestations, detection of the fungus by microscopic examination of skin flakes and identification of the type of pathogen by cultural examination.
Treatment. Treatment of mycosis of the smooth skin of the feet and other localizations is carried out with antifungal agents for external use. For squamous and intertriginous forms of lesions on the feet and other areas of the skin, medications are used in the form of a cream, ointment, solution, spray; you can combine a cream or ointment with a solution, alternating their use. Currently, the following medications are used to treat this disease: exifin cream, mycozoral cream, nizoral cream, canizon cream and solution, mycozon cream, mycospor (bifosin) cream, mifungar cream, lamisil cream and spray, mycoterbin cream. These drugs are applied to cleansed and dried skin once a day, the average duration of treatment is no more than 2 weeks. Antimycotics such as travogen, ekalin, batrafen, mycoseptin, mycozolon are used 2 times a day until clinical manifestations resolve, then treatment is continued for another 1-2 weeks, but once a day - to prevent relapse. In nodular and nodular forms of rubrophytosis, after relieving acute inflammatory phenomena using one of these ointments, sulfur-tar ointment (5-10%) is prescribed in order to further resolve the clinical manifestations. For intertriginous and dyshidrotic forms (the presence of only small blisters) of mycosis of the feet, drugs with a combined effect are used, which, along with an antifungal agent, include a corticosteroid, for example mycozolon, travocort, or a corticosteroid and an antibacterial drug - triderm, pimafucort.
In case of acute inflammatory phenomena (wetting, the presence of blisters) and severe itching, treatment is carried out as for eczema: desensitizing agents (intravenous or intramuscular administration of calcium chloride solution (10%), sodium thiosulfate solution (30%), calcium gluconate solution (10%) or calcium pantothenate orally; antihistamines. For external medications, at the first stage of therapy, lotions are used (2% boric acid solution, potassium permanganate solution 1:6000, 0.5% resorcinol solution), 1-2% aqueous solutions of methylene blue or brilliant green, fucorcin. Then they switch to pastes - boron-naphthalan, ichthyol-naphthalan, ACD paste - F3 with naphthalan, if complicated by bacterial flora - lincomycin (2%). At the 2nd stage of treatment after resolution of acute inflammatory phenomena, the above-mentioned antimycotic agents are used.
A drug such as Triderm, which contains, in addition to an antimycotic (clotrimazole 1%), a broad-spectrum antibiotic (gentamicin sulfate 0.1%) and a corticosteroid (betamethasone dipropionate 0), can quickly and effectively eliminate the symptoms of inflammation and itching in the presence of both fungal and bacterial infections. .05%). The presence of Triderm in 2 dosage forms - ointment and cream - makes it possible to use it for different types and at different stages of the pathological process.
If external therapy is ineffective, systemic antimycotics are prescribed: itraconazole in a continuous regimen of 200 mg per day for 7 days, then 100 mg for 1-2 weeks; terbinafine (Lamisil, Exifin) 250 mg once a day every day for 3-4 weeks; fluconazole (150 mg once a week for at least 4 weeks).
Prevention. To prevent foot mycosis, it is necessary to observe, first of all, the rules of personal hygiene in the family, as well as when visiting a bathhouse, sauna, swimming pool, gym, etc.; disinfect shoes (gloves) and linen during the treatment period. After visiting a bathhouse, swimming pool, sauna, to prevent mycosis of the feet, apply Daktarin spray powder to the skin of the interdigital folds and soles.
Tinea versicolor is a fungal disease caused by Malassezia furfur (Pityrosporum orbiculare), a yeast fungus. Lichen versicolor is quite widespread in all countries; young and middle-aged people suffer from it.
Etiology. Malassezia furfur as a saprophyte is found on human skin and, under favorable conditions, causes clinical manifestations.
Pathogenesis. Factors contributing to the development of the disease have not yet been precisely established, however, lichen versicolor is more common in people suffering from excessive sweating, changes in the chemical composition of sweat, diseases of the gastrointestinal tract, endocrine pathology, vegetative-vascular disorders, as well as immune deficiency .
Clinic. The disease is characterized by the presence of small spots on the skin of the chest, neck, back, abdomen, less often the upper and lower extremities, axillary and inguinal-femoral areas, on the head; the spots are initially pink in color and then become light and dark brown; Slight peeling is also observed, sometimes it can be hidden and can only be revealed by scraping. The rashes often merge, forming large areas of damage. After tanning, as a rule, white spots remain as a result of increased flaking. The disease is characterized by a long course with frequent exacerbations.
Diagnosis. The diagnosis is made on the basis of clinical manifestations, when the pathogen is detected in skin flakes during a microscopic examination and in the presence of a characteristic yellow or brown glow under a Wood's fluorescent lamp, as well as a positive iodine test.
Treatment. Currently, there is a sufficient selection of antifungal drugs for topical use that have a pronounced antifungal effect against the causative agent of lichen versicolor. These include imidazole and triazole derivatives, allylamine compounds. During the treatment of the disease, the following is used: exifin cream (applied to cleansed and dried skin in the affected areas 2 times a day for 7-14 days, if necessary, after a 2-week break, the course of treatment can be repeated), nizoral cream, mycozoral ointment, cream and canizon solution, mycozon cream, mifungar cream (prescribed once a day, duration of treatment is 2-3 weeks); lamisil cream and spray; nizoral shampoo (for three days, apply to the affected areas of the skin for 3-5 minutes and wash off in the shower). For common, often recurrent forms of lichen versicolor, systemic antimycotics are more effective: itraconazole (prescribed 100 mg once a day for two weeks, then take a two-week break, repeat the course of treatment if necessary), fluconazole (150 mg once a week within 4-8 weeks). During treatment, it is necessary to disinfect the patient’s clothes, hats, underwear and bed linen by boiling in a 2% soap-soda solution and ironing with a hot iron while wet. Family members of the patient should also be examined.
Prevention. To prevent recurrence of mycosis, it is necessary to use nizoral shampoo. Treatment should be carried out from March to May once a month for 3 days in a row.
Smooth skin candidiasis is a fungal disease caused by yeast-like fungi of the genus Candida.
Etiology. The pathogens are opportunistic fungi that are widely distributed in the environment. They can also be found on the skin and mucous membrane of the mouth, digestive tract, and genitals of a healthy person.
Epidemiology. Infection from the external environment can occur with constant fractional or massive infection with fungi.
Pathogenesis. Both endogenous and exogenous factors can contribute to the occurrence of candidiasis. Endogenous factors include endocrine disorders (usually diabetes mellitus), immune deficiency, severe somatic diseases and a number of others. The development of the disease is possible after the use of a number of modern medications: broad-spectrum antibiotics, immunosuppressive and hormonal drugs. The occurrence of candidiasis in the interdigital folds of the hands is facilitated by frequent contact with water, as this develops maceration of the skin, which is a favorable environment for the introduction of the pathogen from the external environment.
Clinic. On smooth skin, small folds on the hands and feet are more often affected, less often - large ones (inguinal-femoral, axillary, under the mammary glands, intergluteal). Lesions outside the folds are located mainly in patients suffering from diabetes mellitus, severe general diseases, and in infants.
In some patients, the disease begins in small folds of the skin with the formation of small, barely noticeable blisters on the lateral contacting surfaces of hyperemic skin, the process gradually spreads to the area of the fold, then peeling, maceration appears, or immediately shiny eroded surfaces of a deep red color with clear boundaries appear, with peeling of the stratum corneum of the epidermis along the periphery. The 3rd and 4th interdigital folds on one or both hands are most often affected. The disease is accompanied by itching, burning, and sometimes pain. The course is chronic, with frequent relapses.
In large folds, the lesions are dark red in color, shiny, with a moist surface, with a strip of exfoliating stratum corneum of the epidermis, occupying a significant surface, having clear boundaries and irregular outlines. New small erosions appear around large foci. In children, the process of large folds can spread to the skin of the thighs, buttocks, abdomen, and torso. Painful cracks sometimes form deep in the folds.
Candidiasis of smooth skin outside the folds has a similar clinical picture.
Diagnosis. The diagnosis is made on the basis of a typical clinic when a fungus is detected in scrapings from skin flakes during a microscopic examination.
Treatment. Limited and sometimes widespread acute forms of smooth skin lesions, especially those that developed during therapy with antibacterial drugs, as a rule, are easily treated with local antimycotic agents in the form of a solution, cream, ointment and can resolve even without treatment after discontinuation of antibiotics.
For candidiasis of smooth skin of large folds with acute inflammatory phenomena, treatment should begin with the use of an aqueous solution of methylene blue or brilliant green (1-2%) in combination with indifferent powder and continue for 2-3 days, then antifungal drugs are used until clinical resolution manifestations.
Among the antimycotic agents for candidiasis of smooth skin, the following are used: Canison solution and cream, Mycoson cream, Mifungar cream, Candida cream and solution, Triderm ointment and cream, Pimafucort, Pimafucin, Travocort, Travogen, Nizoral cream, Mycozoral ointment, Ekalin.
For common skin processes and in case of ineffectiveness of local therapy, systemic antimycotics are prescribed: fluconazole (Diflucan, Forkan, Mycosist) - adults at a dose of 100-200 mg, children at a dose of 3-5 mg per kg of body weight, itraconazole (100-200 mg), nizoral (adults 200 mg, children weighing up to 30 kg - 100 mg, over 30 kg - 200 mg) once a day daily, as well as the polyene antibiotic natamycin (adults 100 mg 4 times a day, children 50 mg 2–4 times a day). The duration of treatment is 2–4 weeks.
Prevention. Prevention of smooth skin candidiasis in adults and children consists of preventing its development in people suffering from underlying diseases, as well as in people receiving long-term antibacterial, corticosteroid, and immunosuppressive therapy. To prevent the development of candida infection in children hospitalized in somatic departments and receiving broad-spectrum antibiotics, it is necessary to prescribe fluconazole at the rate of 3 mg per kg of body weight once a day, treatment is carried out during the entire main course of therapy. Patients with intestinal candidiasis are prescribed nystatin 2–4 million units per day or natamycin 50 mg for children and 100 mg for adults 2 times a day for 15 days.
Zh.V. Stepanova, Doctor of Medical Sciences, TsNIIKV
Note!
- In recent years, there has been an increase in the number of diseases caused by opportunistic fungi, among which superficial forms of candidiasis are most often recorded.
- Due to insufficient awareness about the sources and ways of spreading infection, as well as adequate preventive measures, patients turn to the doctor late, and therefore mycoses become chronic
- 50% of the population suffers from mycosis of the feet. Adults get sick more often. Recently, there has been an increase in incidence in children, even infants.
- Treatment of mycosis of the smooth skin of the feet and other localizations is carried out with antifungal agents for external use.
- If external therapy is ineffective, systemic antimycotics are prescribed.
Where to buy antifungal agents
It is better to buy products to combat lichen and fungal pathogens at pharmacy offices, where a quality guarantee is provided and it is possible to select the right kit. In recent years, online pharmacies have been actively developing, making it easier to find and purchase the necessary goods. The largest pharmacy chain “Vasha No. 1” works with a wide range of medical products with a therapeutic effect on the body infected with fungus. Already, the majority of the population of the cities of Moscow and Odintsovo enjoy using this service, which makes it possible to save a certain amount and their own time.
The pharmacy’s website provides the entire range of products with a description of the effects on the body and rules of use, price, payment and purchase. The buyer can choose the right type of product himself, but if necessary, the manager-consultant can provide advice.
Basics of antifungal treatment
The duration of treatment with antifungal drugs is always individual and usually depends on the type of mycosis, as well as the severity of the disease. The minimum course of treatment for vaginal candidiasis (thrush) is from 1 to 3 days. The maximum duration of treatment for nail mycoses (onychomycosis) is up to 6-12 months. On average, the duration of treatment for superficial mycoses is 14-30 days.
For mycoses of the nails and feet, topical use of antifungal drugs should be continued for another 2-3 weeks after the manifestations of the disease disappear in order to avoid exacerbation and return of the disease.
Advantages of the online pharmacy "Aptstore"
The best programmers in the business worked on the website of the pharmacy “Vasha No. 1”, the service turned out to be convenient and simple. This fact is confirmed by a huge number of positive responses from customers. For the convenience of ordering, a “Personal Account” has been created, registration in which will not take much time. You just need to enter your data and tick the required boxes, which will only have a positive effect on further cooperation. Your personal account will contain previously paid applications, products that have aroused interest, and addresses of convenient offices to visit.
It is advisable to fill out all the fields in the client card - this will allow pharmacy staff to build a more informative dialogue and improve their work in the future. You can choose any receiving address that is convenient for your route. Pharmacy offices operate conveniently - they open early in the morning and close at midnight. There are 24-hour offices, so there are no difficulties in receiving goods.
Submitting an order from the warehouse
More and more companies are deciding to sell products from warehouses, which has only had a positive impact on the trading process. This makes it possible to stock up on large volumes of goods without overpaying for transport and storage. provides clients with a simple and convenient website with the help of managers in filling out applications.
The goods are sold much cheaper, which is caused by the absence of a number of expenses that companies with a standard approach to trade incur. After completing the application, an SMS notification is sent to the buyer.
Search and order the required product on the pharmacy website
The programmers of the Vasha No. 1 pharmacy have developed a lightweight and easy-to-use website where finding the right product is quite simple. Any person can handle placing an order and searching - this fact was the first priority of the pharmacy staff.
To search you only need to follow a few simple steps:
- Go to the “Antifungal agents” section, where for convenience the entire range of products with a specific action is collected.
- Enter the first 2-3 letters of the required product into the quick search line - after a few seconds the program will display a list of suitable options.
- The alphabetical index search service is convenient because when you enter the list with the initial character of what you are looking for, you will find what you need.
All purchase data is saved in your personal account, which makes the search many times faster. Therefore, when searching again, the previous one is duplicated or the necessary positions are selected.
On the online site of the pharmacy “Vasha No. 1” you can easily get acquainted with the price of the product, for which you only need to click the mouse cursor on the image - all the information will appear on the monitor. The cost is usually located immediately below the product picture. offers its clients a number of pleasant bonuses and discounts, which helps them save a lot.
Classification of antifungal drugs
Antifungal drugs are classified into:
- antifungals for systemic use: antibiotics: amphotericin B, griseofulvin;
- imidazole derivatives: ketoconazole;
- triazole derivatives: fluconazole, itraconazole, voriconazole, posaconazole;
- allylamines: terbinafine;
- echinocandins: anidulafungin, caspofungin, micafungin;
- antibiotics: nystatin, natamycin;
In addition, there are combination drugs containing an antifungal agent and a corticosteroid (clotrimazole + beclamethasone; isoconazole + diflucortolone; natamycin + neomycin + hydrocortisone), as well as: bifonazole + urea; clotrimazole + gentamicin + calendula extract + yarrow extract; clotrimazole + salicylic acid; miconazole + metronidazole.

![Rice. 2. Relationship between dose of diclofenac (D), naproxen (Nap) and etoricoxib (Eto) and effect size in osteoarthritis [3]](https://irknotary.ru/wp-content/uploads/ris-2-zavisimost-mezhdu-dozoj-diklofenaka-d-naproksena-nap-i-330x140.jpg)