Author:
Polyakov Innokenty Evgenievich pediatrician
Quick transition Treatment of bronchitis in children
Bronchitis is an inflammation of the mucous membrane of the walls of the bronchi, a kind of tubes designed to transport air from the upper parts of the respiratory tract (nose, larynx, trachea) to the final parts (alveoli), where gas exchange and oxygen saturation of the blood directly occur.
The bronchi branch, starting from two large main bronchi (one per lung), ending with the smallest bronchioles (inflammation of the bronchioles - bronchiolitis).
Bronchitis can be acute, chronic, recurrent (recurring) and obstructive.
How does bronchitis manifest?
The main symptom of bronchitis is cough. There may also be an increase in temperature, an accompanying runny nose, nasal congestion, pain and sore throat and other symptoms of a common ARVI. Strictly speaking, simple bronchitis is a type of ARVI.
The vast majority of bronchitis is acute (that is, the cough lasts no more than 2–4 weeks). The terms “recurrent” and “chronic” have little application to children; in most cases they only mask the true cause: bronchial asthma, bacterial protracted bronchitis, cystic fibrosis, primary ciliary dyskinesia, interstitial lung diseases, etc.
In most modern English-language sources, acute bronchitis is not distinguished from other “cold” diseases and is described in the context of ARVI, since it is most often caused by the same respiratory viruses (respiratory syncytial virus, rhinovirus, parainfluenza viruses, influenza, etc.). The only difference is in the main localization of the inflammatory process during ARVI: inflammation in the nose and throat - nasopharyngitis, inflammation in the larynx and vocal folds - laryngitis, in the bronchi - bronchitis. The tradition of considering bronchitis as a serious complication of acute respiratory viral infection, requiring great anxiety and mandatory antibiotic therapy, has no more justification than the automatic prescription of antibiotics on the third day of fever.
Diagnosis of bronchitis
Bronchitis is a clinical diagnosis, that is, the doctor makes it only on the basis of a survey and examination of the patient. The presence of typical complaints (runny nose, cough, malaise, fever) and typical wheezing when listening to the lungs with a stethoscope, as well as the absence of other reasons that explain these symptoms, is a necessary and sufficient condition for diagnosing bronchitis. Wheezing during bronchitis is symmetrically scattered over the entire surface of the lungs, and not localized only in one area (as happens, for example, with lobar pneumonia). Wheezing can be dry (occur when air passes through narrowed, swollen bronchi without phlegm) and wet (occur when air passes through the bronchi in which phlegm accumulates). Often, both types of wheezing are present at the same time, or dry wheezing is heard in the first days of the disease, then, as the natural course of the disease progresses, they turn into wet wheezing.
Treatment of bronchitis
Bronchitis, like other forms of ARVI, is a typical self-limiting disease. In most cases, no drug treatment is required. It is important to create favorable conditions for the child to recover: sufficient drinking, maintaining an optimal microclimate (temperature and humidity) in the room, using antipyretic drugs if necessary. And of course, it is worth protecting your child from tobacco smoke.
It is worth noting that coughing in children, especially young children, is much less effective in coughing up mucus; they simply have not yet learned to cough “correctly.” Fortunately, not only coughing removes phlegm, people have a special mucociliary clearance system - tiny microcilia that rhythmically move and push mucus higher and higher through the respiratory tract. Adequate fluid intake into the body and a normal microclimate help the child quickly remove all the mucus formed due to inflammation and facilitate recovery.
There is no effective treatment against the viruses that cause ARVI and bronchitis. Drugs that in our country are called “antiviral” or “immunomodulatory” in the context of the treatment of ARVI have no proven effectiveness and are not used in developed countries. Doctors at the Rassvet clinic do not recommend taking them for bronchitis. The same can be said about “mucolytics” and “expectorants” used for wet coughs. They have been tested many times in independent studies and have not been shown to be effective for coughs in children (the group receiving the placebo recovered on average in the same time frame as the group receiving the drug). It is even believed that up to the age of 5 years, such drugs can worsen the course of a cough, since they increase the volume of sputum, and young children cough it up extremely ineffectively. Antitussives (used against dry coughs) have more than modest evidence of effectiveness, but can still be prescribed for a hacking cough if parents see at least some relief from them.
That is, we cannot eradicate the very cause of bronchitis or influence the pathogenesis of the disease; we have to wait until the immune system does its job. But there is good news: the child’s body is quite capable of coping with respiratory viruses, this is inherent in nature. Bronchitis is an unpleasant but not dangerous disease.
Cough is a very worrying symptom for parents; it is constantly heard and reminds that the child is sick, but the child much less than his parents (if it bothers him at all).
Separately, it should be said about bronchitis, accompanied by broncho-obstructive syndrome - excessive narrowing of the lumen of the bronchi, caused not only by inflammatory edema of the bronchial wall and accumulation of sputum in its lumen, but also by spasm of smooth muscles in the bronchi. In Russia it is usually called “obstructive bronchitis”, in the West virus-induced wheezing, virus-induced asthma, or simply wheezing (“wheezing”). With this type of bronchitis, special wheezing occurs, they are called “wheezing” or “musical”, and in some cases they are so loud that you can hear them even without a stethoscope, just from the child’s mouth in a quiet room, or you can feel the vibration of the child’s chest with your palms. Obstructive bronchitis can lead to respiratory failure and this is the only bronchitis for which we can effectively treat with medications (bronchodilators, inhaled steroids and some others). If bronchial obstruction leads to severe respiratory failure, the child may need to be hospitalized for active treatment.
In some cases, antibiotics may be required. Antibiotics have no effect on a viral infection, but bronchial obstruction can develop due to certain bacterial pathogens, and viral bronchitis can be accompanied by bacterial complications. The need for antibiotics may be indicated by a “second wave” of fever, lack of improvement over a long period of time, deterioration of the condition, the appearance of additional symptoms (for example, ear pain), and inflammatory changes in blood tests. In such situations, it is always worth showing the child to the doctor and deciding on the need for antibiotic therapy.
Information for parents of premature babies born before 35 weeks gestational age
Dear parents, Your baby was born premature.
From the first minutes of his life, he is monitored and the necessary assistance is provided by experienced specialists: anesthesiologists-resuscitators and neonatologists. Their main task is to save the life of your child and try to prevent possible serious diseases that arise due to the immaturity of the body at the time of premature birth. Such diseases of premature newborns also include pathological development of the eyes - retinopathy of prematurity (ROP). ROP is one of the main causes of blindness, low vision and visual impairment in children from an early age in all developed countries of the world. The main cause of ROP is the premature birth of a child: the earlier the child is born and with a lower body weight, the more often he develops retinopathy and the more severe it is. Thus, the incidence of ROP among children with a birth weight of less than 1000 g reaches 90%. In addition, if a child has concomitant diseases from other organs, the severity of retinopathy is aggravated.
Thus, premature babies need a mandatory and timely examination by an ophthalmologist!
All premature babies normally have signs of eye immaturity and the process of retinal formation is not complete. After the birth of a child, the retina can develop in two ways: 1) normal growth of retinal vessels, or 2) pathological - development of ROP. Using modern examination techniques, an ophthalmologist identifies all changes in the maturing retina in a premature baby.
The first examination by an ophthalmologist of a premature baby is carried out, regardless of the location of the child, at 3-4 weeks of his life, and for extremely premature babies (born at 22-26 weeks of gestational age) at 30-31 weeks from conception. As a rule, during this period only signs of immaturity of the child’s eyes are revealed, but sometimes the first signs of ROP can be observed, which in most cases appear at 4-6 weeks of a premature baby’s life.
In what cases does bronchitis in a child require special attention?
If cough and wheezing occur in a child with a serious heart defect or in a premature child under 2 years of age, if life has forced you to “without Google” understand the meaning of the terms “bronchopulmonary dysplasia”, “acute respiratory distress syndrome”, if your child initially has serious lung diseases.
If a child’s intense cough lasts more than 4 weeks, if the child regularly suffers from severe bronchitis, if wheezing in the lungs is a regular companion to his colds, or wheezing occurs regardless of whether the child has ARVI or not, if ordinary colds regularly require justified antibacterial therapy - in all these cases, bronchitis can pose a serious danger and requires increased attention and, most likely, consultation with a pulmonologist.
Medical observation program for premature infants in the first year of life “Catching up and growing”
Medical observation program for premature infants in the first year of life “Catching up and growing”
“Catching up and growing” program
is aimed at solving the problems of children born prematurely or with pathology in the neonatal period. The program is implemented on the basis of a department created for children under 3 years of age, with the involvement of doctors specializing in the treatment and rehabilitation of children born with low and extremely low body weight.
The program includes scheduled preventive examinations, instrumental and laboratory tests in accordance with the schedule provided by the Order of the Ministry of Health of the Russian Federation*, home visits by a pediatrician for illnesses, and telephone support.
1. Preventive examinations by a pediatrician/neonatologist are carried out
- in the first month of life – once every 10 days – at home,
- in the second month – 2 times – at home
; - from the third month
–
1 time per month
– in an outpatient setting.
2. In the period from 1 to 3 months of life, taking into account the corrected age and depending on the timing determined by the pediatrician, a full medical examination is carried out, including:
- Examinations by an ophthalmologist, neurologist, orthopedic surgeon, otorhinolaryngologist;
- General clinical blood test, general urine test;
- Ultrasound examinations of the brain (neurosonography), abdominal cavity and genitourinary system, hip joints; echocardiography;
- Audiological screening;
- A routine examination by a pediatrician/neonatologist, including a clinical examination, antopometry, consultation with parents regarding the health and development of the child, recommendations for care, preventive measures, feeding, daily routine and further dynamic observation.
Next, comprehensive preventive examinations are carried out:
at 6 months of age:
- Examinations by a pediatrician, ophthalmologist, orthopedic surgeon, neurologist;
- General clinical blood test, general urine test;
- Electrocardiography
at 9 months:
- Examination by a pediatrician, neurologist;
- General clinical blood test, general urine test;
at 12 months:
- Examinations by a pediatrician, neurologist, ophthalmologist, otorhinolaryngologist, orthopedic surgeon, psychologist, dentist;
- Electrocardiography, echocardiography;
- General clinical blood test with glucometry, general urinalysis;
- Coprological examination, scraping for enterobiasis, stool analysis for helminth and lamblia eggs.
3.
On the recommendation of the attending physician, the plan of preventive examinations may include consultations with a cardiologist, endocrinologist, gastroenterologist, nephrologist, urologist, as well as unscheduled consultations with a neurologist, ophthalmologist, orthopedic surgeon, and otolaryngologist.
In addition, the program provides:
- Assigning a personal pediatrician
with the ability to contact him by phone daily from 8.00 to 19.00 - Additional laboratory tests
- as prescribed by the attending physician; - Additional ultrasound and functional diagnostic tests -
on the recommendation of a doctor; - General massage with a specialist visiting your home
(10 sessions); - Outpatient appointments with a pediatrician for illness
- without restrictions; - Consultation with a psychologist
for mother/parents as part of family support after the birth of a child; - Preparation of medical documentation (certificates, medical reports of established forms);
- Support by the curator of medical observation programs by phone +7(499)110-29-67, +7
on weekdays from 9.00 to 18.00
The cost of the program is 180,000 rubles.
When paying, installment payment may be provided:
- 50% - upon concluding an annual service agreement,
- you can pay the remaining 50% within 3 months.
To prevent severe RSV-associated lower respiratory tract infections, children at high risk of RSV infection who have permanent registration in Moscow can receive injections of palivizumab (Synagis). The procedure is carried out at the Center for Restorative Treatment of children under 3 years of age born with low and extremely low body weight, free of charge, under the compulsory medical insurance policy.
You can receive all necessary studies and consultations not included in the Annual Medical Care Program, as well as vaccinations with vaccines from foreign manufacturers, with a 10% discount.
You can get detailed information about medical monitoring programs for children by calling:
+7(499)110-29-67, +7.
*Order of the Ministry of Health of the Russian Federation dated August 10, 2017. No. 514n, section “On the Procedure for conducting preventive medical examinations of minors”
Prevention of bronchitis
In general, prevention is the same as for ordinary acute respiratory viral infections - nonspecific: ventilation, hand washing, social distancing, etc. All this became widely known with the spread of Covid-19. There are no specific drugs for the prevention of acute respiratory viral infections, as well as drugs to “strengthen the immune system.” The only exception is the influenza vaccine, but the influenza virus is only one of many causes of bronchitis.
Vaccination against pneumococcal disease may protect against bacterial complications of bronchitis caused by Streptococcus pneumoniae.
Monoclonal antibodies against respiratory syncytial virus (Synagis, palivizumab) can be used in children at risk for severe bronchiolitis (premature children under 6 months born at 35 weeks or earlier). However, this method is only suitable for certain groups of children.
Thus, detecting wheezing in a child’s lungs and diagnosing bronchitis should not cause horror in parents if the child does not belong to a risk group. The child’s own immune system and simple parental care will in most cases ensure a complete recovery in 1–3 weeks. Less commonly, medications or even hospitalization may be required, but the prognosis for bronchitis is almost always favorable.
The article presents our own experience of using the drug "Palivizumab" (Synagis) for passive immunoprophylaxis of ARVI, complicated by frequent episodes of obstructive bronchitis or pneumonia in young children with bronchopulmonary dysplasia. The justification for the use of Synagis is the undoubted fact of the presence of respiratory syncytial virus in the structure of ARVI pathogens, which served as a recommendation for the use of the drug in 50 countries around the world and in most countries “Palivizumab” was included in the standards for the prevention of RSV infection.
Experience with the drug Palivizumab (Sinagis) for passive immunization RSV-infected at bronchopulmonary dysplasia in infants
The article provides a personal experience with the drug palivizumab (sinagis) for passive immunization of SARS, complicated by frequent episodes of obstructive bronchitis or pneumonia in infants with bronchopulmonary dysplasia. The rationale for the use of sinagis is undoubtedly the presence in the structure of the SARS causative of respiratory syncytial virus, which was the recommendation for the use of the drug in 50 countries around the world and in most of palivizumab agents entered the standards of prevention RSV - infection.
Bronchopulmonary dysplasia (BPD) is a chronic disease of the immature lungs that develops in newborns, mainly very premature infants, after respiratory distress syndrome and/or pneumonia in the early neonatal period. With this disease, the bronchioles and lung tissue are affected: in some areas of the lung, the healthy structure is replaced by connective tissue and fibrosis develops, in others, swelling of the lung tissue occurs, resulting in emphysema. The alternation of areas of fibrosis and emphysema creates a characteristic pathomorphological and clinical picture of bronchopulmonary dysplasia. Often, pulmonary vessels are involved in areas of fibrosis: damage to the lung tissue occurs due to impaired oxygen saturation of the tissue and release of carbon dioxide. The frequency of BPD depends on the child’s body weight at birth: with a weight of 500-1000 g, the disease occurs in 33-64% of children, with a weight of 1000-1500 g - in 3-6%, with a weight of more than 1500 g - in 1-2%. In rare cases, BPD also develops in children born at term. Predisposing factors to the development of BPD in full-term infants, as well as in premature infants, are mechanical ventilation during meconium aspiration, pneumonia, or surgery. A feature of the clinical picture of BPD is respiratory failure in newborns who are on mechanical ventilation or after mechanical ventilation, when children receive oxygen through a mask for a long time. Cough, wheezing, shortness of breath, i.e. signs of pulmonary obstruction often persist despite spontaneous breathing. The severity of BPD is determined by the state of oxygen dependence at 36 weeks of postconceptional age for children under 32 weeks of age or at 56 days of life for children born after 32 weeks of gestation. The most common manifestation of exacerbation of BPD in the form of obstructive syndrome is observed during acute respiratory viral infection, among the causative agents of which the respiratory syncytial virus selectively affects this contingent of children. Respiratory syncytial virus (RSV) infection is a significantly more common cause of death in children in their first year of life than influenza virus (1). RSV infection can be life-threatening in infants under 12 weeks of age, premature infants, infants with congenital heart defects, and those with bronchopulmonary dysplasia (2). Today there is an effective method for preventing RSV infection: this is passive immunoprophylaxis in children at high risk by introducing antibodies to the RSV virus into the child’s body to prevent severe forms of infection caused by RSV. Palivizumab (Synagis) is the world's first drug with proven effectiveness for passive immunoprophylaxis of severe forms of RSV infection in children from high-risk groups (3). The mechanism of action of Synagis is the suppression of the activity of the F protein, which ensures the penetration of the virus into the cell. In most countries (there are more than 50), where the use of Synagis is recommended, it is included in the standards for the prevention of RSV infection.
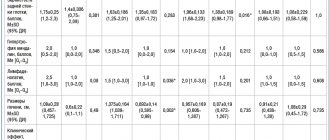
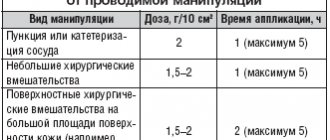
17 children from 3 to 16 months of life were under observation: 16 children were born premature at a gestation period of 28-32 weeks and weighing 760-1720 g. One child was born from a full-term pregnancy with multiple malformations that were compatible with life and required resuscitation care. All children in the neonatal period were on mechanical ventilation. These children were diagnosed with “Bronchopulmonary dysplasia” according to the criteria of the modern domestic working classification of bronchopulmonary diseases in children 2008 (Moscow) already during their stay in the intensive care unit for newborns or in the department of the second stage of nursing at the 1st Children's City Hospital Kazan. Moderate course was observed in 11 (64.8%), severe - in 6 (35.2%). Among the concomitant pathologies in all premature children, the following were identified: retinopathy of prematurity - children were examined with a retinal camera, consulted with an ophthalmologist and, if necessary, they underwent surgical correction; cerebral pathology, mainly of hypoxic or mixed origin, of varying severity, but without severe, incurable complications. Children with BPD were admitted to the pulmonology department with acute bronchitis, bronchiolitis or pneumonia. Before this admission, each child had several episodes of acute respiratory viral infection complicated by obstructive bronchitis or pneumonia. A thorough analysis of the medical history, the results of clinical, instrumental and laboratory examinations did not exclude complicated RSV infection in the observed patients, which served as a rationale for passive immunoprophylaxis of its relapses. For this purpose, 9 patients with BPD, after the elimination of the acute bronchopulmonary process clinic, received the drug "Synagis": 1 child - 4 injections, one child - 3 injections, 6 children - 2 injections each and one child - one dose. The choice of "Synagis" was determined by the severity of BPD, the age of the child, the number of episodes of ARVI and its complications and the time of year - from November to March inclusive. "Synagis" was administered intramuscularly into the outer lateral region of the thigh, a single dose was 15 mg per 1 kg of body weight with an interval of 1 month. For repeated injections, children were admitted to a day hospital for 2 days: on the first day they underwent a clinical examination and examination; in the absence of contraindications, Synagis was administered and the child was observed for another day. No early side effects were observed. During the month following the introduction of Synagis, contact with the child’s parents was carried out via mobile communications: no complications were identified in any case. Observation of children who received passive immunoprophylaxis of RSV infection since November 2011. to June 2012 inclusive, showed that only one child had a relapse of ARVI with obstruction syndrome.
The study showed the undoubted clinical effectiveness of the use of the drug "Palivizumab" (Synagis) for the purpose of passive immunoprophylaxis of recurrent acute respiratory viral infections and, in particular, RSV infection in children with BPD. This contributed not only to a reduction in the number of episodes of exacerbation of the disease, but also, obviously, to a reduction in the risk of chronicity of bronchopulmonary pathology in young children. Continued follow-up of patients until the age of three will contribute to a final judgment about the development of chronic lung disease or its prevention in children with BPD who received Synagis.
A.V. Kuznetsova, I.V. Rusakova, I.V. Sitdikova, A.R. Khaertynova, F.S. Pirogova, L.F. Netfullova, K.Z. Zakirov
Children's City Hospital No. 1, Kazan
Kuznetsova Alevtina Vasilievna - Doctor of Medical Sciences, Consulting Professor
Literature:
1. Thompson WW, Shay DK, Weinttaub E. et. al. Mortality associated with influenza and respiratory syncytial virus in the United States // JAMA. - 2003. - Vol. 289. - P. 179-86.
2. Patrusheva Yu.S., Kulichenko T.V. Laboratory diagnosis of respiratory syncytial viral infection in children // Questions of diagnostics in pediatrics. - 2009. - T. 1, No. 1. - P. 24-27.
3. Modified Recommendations for Use of Palivizumab for Prevention of Respiratory Syncytial Virus Infections Committee on Infectious Diseases // Pediatrics. - 2009. - Vol. 124. - P. 1694-1701.