Every home medicine cabinet should have an effective pain reliever. And it’s very good when it can be taken for various symptoms. In such cases, one complex drug replaces several others, which significantly saves money.
Today, pharmacies offer many products, so it is very difficult to choose. Pyatyrichatka tablets have become very popular lately. This is a complex drug that has several therapeutic effects:
- Anesthetic,
- Antipyretic,
- Sedative,
- Relieves the inflammatory process,
Before using Pyatyrichatka, you must study the instructions in detail.
Use of the drug 5-nok
It is recommended to take the tablets during or after meals.
Adults: 400–800 mg per day, divided into 4 doses. The average daily dose is 400 mg (100 mg 4 times a day). In severe cases, the daily dose is increased to 800 mg (200 mg 4 times a day).
Children aged 1 to 14 years: the usual average daily dose is 200–400 mg (50–100 mg 4 times a day).
Children aged 2 to 12 months: the daily dose is determined at the rate of 25 mg/kg per day, divided into 4 doses. The drug can be taken for 1 month; for chronic infections, 5-NOK can be prescribed in repeated courses of 2 weeks with 2-week breaks (the course of treatment can last several months).
Form, composition and effect of the drug
The product is available in the form of white tablets with a yellowish tint. They have a cylindrical shape with a section in the middle.
The complex effect is ensured by the composition.
Components of "Pyatyrichatka":
- Metamizole sodium (300 mg),
- Paracetamol (200 mg),
- Caffeine benzoate (50 mg),
- Fenofarbital (10 mg),
- Codeine phosphate (5 mg).
Each of the active substances presented has its own function, thus ensuring a complex effect.
Metamizole relieves pain, lowers temperature, relaxes the muscles of the uterus, urinary and bile ducts. Paracetamol also has an antipyretic effect and slightly relieves pain. Caffeine, which is part of the drug, ensures the penetration of analgesics through barriers and stimulates the centers of the medulla oblongata.
Phenobarbital has calming properties, relieves spasms, and reduces muscle tone. In addition, this component activates the work of other active substances included in the composition. Codeine acts as a sedative, an anesthetic, it reduces the level of excitability of the cough center. This component is narcotic in nature, so the drug should be used only in the indicated doses and when absolutely necessary.
The first positive effect after administration is observed within half an hour, the full therapeutic effect occurs after two hours.
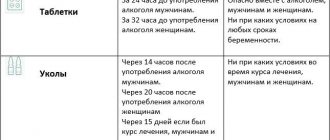
Tablets "Pyatyrichatka" have a strong effect on the body. Active substances are absorbed in the intestines, processed in the liver and excreted by the kidneys. The period of complete exit from the body is up to 5 days. Should not be taken with alcohol, this will put double stress on the internal organs, especially the liver. .
Special instructions for the use of the drug 5-nok
in case of moderate renal failure (creatinine clearance above 20 ml/min), half the usual daily dose should be prescribed. In severe renal failure (creatinine clearance below 20 ml/min), treatment with 5-NOC is contraindicated.
For liver failure, half the usual daily dose is prescribed. The safety of the drug during pregnancy and lactation has not been established; Despite the lack of data, prescribing the drug is not recommended.
The effect on the ability to drive vehicles and machinery has not been established.
Tactics for using uroseptics in general practice
To this day, uroseptics remain the main means of pathogenetic therapy for urinary tract infections. The most important way to increase the effectiveness of treatment is not only the creation and implementation of new uroantiseptics, but also improving the tactics of using existing agents. Drugs that are classified as uroseptics are summarized in Table. 1.
Table 1. Pharmacological drugs related to uroseptics
— oxolinic acid (gramurin) — cinoxacin (cynobac) — nitroxoline (5-NOK) — nalidixic acid (nevigramon, negram) — pipemidic acid (palin, pimidel, pipem) — nitrofural (furacilin) — nitrofurantoin (furadonin, nitrofurantoin) — nifuratel (macmiror) - nifurtoinol - furazidin (furagin) - furazolidone (furazolidone) - methenamine (uroflux) - trimethoprim (trimopan, triprim) |
The problem of optimal choice of uroseptic in the treatment of a particular patient dictates the need to answer many questions. First of all, it is necessary to find out the localization of the urinary tract infection, determine the type of pathogen and its sensitivity to the selected uroseptic, the severity of the inflammatory process, and the functional state of the kidneys. In addition, it is necessary to have a clear understanding of the pharmacokinetics and pharmacodynamics of the drug.
Only after answering these questions does the choice of drug become truly optimal.
Speaking about the localization of infection, we must not forget that even the same patient may have different microflora in the kidney parenchyma and in the urinary tract.
As a rule, in the early stages of the disease, a monoinfection is detected; with a longer course of the process, in the case of inadequate antibacterial therapy, microbial associations appear, including up to two or three types of pathogens, often both gram-negative and gram-positive.
The most common pathogens are Escherichia coli and enterococci (i.e., obligate intestinal flora), as well as the hemolytic variant of Escherichia coli, Proteus, Pseudomonas aeruginosa, Staphylococcus aureus, and Klebsiella. Moreover, associations of various types of pathogens with pyelonephritis occur in 20-45.5% of cases. In approximately 15% of cases of chronic pyelonephritis, it is not possible to identify the pathogen in the usual way, either in urine cultures or in cultures of renal tissue. Pathogens that have transformed into forms lacking cell walls (L-forms) and mycoplasmas require complex diagnostic media and techniques for their detection.
Identification of the pathogen allows you to select the most effective uroseptic. Currently, there are clear recommendations on the choice of uroseptic depending on the pathogen, and there is a lot of information on this issue in the literature. In situations where urine culture and flora sensitivity results cannot be expected, standardized antibacterial regimens may be used. For example, it is possible to use gentamicin, if necessary in combination with cephalosporins, or a combination of carbenicillin (pyopene) with nalidixic acid, colymycin with nalidixic acid.
Currently, in severe forms of urological infection - pyelonephritis, urosepsis, in case of resistance to other classes of antimicrobial substances, in the presence of multiresistant strains of bacteria - it is recommended to use fluoroquinolone antibiotics.
If it is necessary to carry out therapy with uroseptics for a long time, with changing drugs every 7-10 days, it is advisable to consistently use drugs that act on the bacterial wall and on the metabolism of the bacterial cell. Sequential use of penicillin and erythromycin, cephalosporins and chloramphenicol, cephalosporins and nitrofurans is recommended to prevent the survival of protoplast and L-form bacteria.
All of the listed groups of uroseptics penetrate well into the tissues of the genitourinary system and urine, where concentrations sufficient to obtain a therapeutic effect are created. At the same time, checking the excretory function of the kidneys is mandatory in each case. With pronounced sclerotic changes and damage to the glomerular apparatus of the kidneys, the success of treatment decreases, and when glomerular filtration decreases to 30 ml/min, there is no point in carrying out antibacterial therapy, since it is impossible to obtain a therapeutic therapeutic concentration of drugs in the renal parenchyma. In addition, the risk of developing toxic effects increases sharply. A decrease in the functional capacity of the kidneys forces us to pay special attention to the nephrotoxicity of the drugs used.
Fluoroquinolones, oxacillin, methicillin, carbenicillin from the penicillin group, macrolides, cephalosporins, and chloramphenicol have virtually no nephrotoxic effects.
Ampicillin, lincomycin, nitrofurans, nalidixic acid, and some long-acting sulfonamides have slight nephrotoxicity. In the presence of renal failure, tetracyclines become nephrotoxic. Aminoglycosides (gentamicin, streptomycin, torbamycin, kanamycin) are always highly nephrotoxic.
The nephrotoxic effects of the drugs are enhanced by severe dehydration and while taking diuretics.
One of the most important criteria for choosing a drug is urine pH. Aminoglycosides and macrolides exhibit maximum effectiveness in an alkaline environment at pH = 7.5–9.0; as urine pH decreases, their activity decreases. The effectiveness of cephalosporins, fluoroquinolones, glycoproteins, tetracyclines, and chloramphenicol does not depend on urine pH. In an acidic environment at pH ≤ 5.5, penicillins, derivatives of naphthyridine, nitrofuran, quinolone, 8-hydroxyquinolone, and metepamine are most effective. All these drugs significantly reduce their activity as the environment becomes alkalized.
In order to increase the alkalinity of urine, it is possible to prescribe a dairy-vegetable diet and sodium bicarbonate. To reduce the pH of urine (acidify it), increase the consumption of bread and flour products, meat and eggs. Ammonium chloride, ascorbic acid, methionine, hippuric acid (which is found, for example, in cranberry juice) are prescribed. Any substance that reduces urine pH below 5.5 inhibits the development of bacteria in the urine.
In the presence of microbial associations, it is possible to use a combination of two uroseptics.
Fluoroquinolones have good compatibility with most antimicrobial drugs and the absence of adverse reactions during combined antibacterial therapy.
β-lactams (penicillins, cephalosporins), aminoglycosides and polypeptides have a synergistic effect and can be combined in severe forms of infection. Moreover, all of the listed groups of antibiotics exhibit antagonism when interacting with tetracyclines, macrolides, and lincomycin.
Levomycetin, tetracyclines and macrolides show indifference when prescribed together. Nitrofurantoin weakens the effect of nalidixic acid. It is considered inappropriate to prescribe the following combinations: furagin with chloramphenicol, furagin with sulfonamides, chloramphenicol with sulfonamides, methenamine with sulfonamides.
Both the choice of drug combination and the required duration of course therapy and the route of drug administration depend on the location of the infection, the severity of the process, and the pathogen.
Doses of drugs for course therapy are given in table. 2. When carrying out treatment, it should be remembered that resistance of microorganisms develops to some drugs. This should be especially taken into account if intermittent therapy is necessary. Preference should be given to drugs to which resistance develops relatively slowly: these are fluoroquinolones, ampicillin, chloramphenicol, depot sulfonamides. Resistance to furagin develops especially slowly, so this drug is the most important when carrying out long-term intermittent treatment.
Resistance of microorganisms to nalidixic acid, oxolinic acid, tetracyclines, streptomycin, and cephalosporins develops quite quickly and often.
Given the above, you should always find out which drugs were used in previous therapy and evaluate the degree of their effectiveness.
It is also necessary to clarify the side effects that occurred during previous therapy and take into account the possibility of their occurrence during the treatment.
All of the above indicates that even with a mass of recommendatory literature with a large number of different treatment regimens, the approach to the treatment of urinary tract infections cannot be mechanical and requires an individual choice of treatment tactics for each specific patient.
Literature
- Padeiskaya E. N. The importance of fluoroquinolones in the treatment of urinary tract infections // Breast Cancer. No. 10. P. 477-478.
- Bertrand G., Katzung. Basic and clinical pharmacology. T. 2.
- Barkhanova A. G., Zakharova G. Yu. Use of antibacterial drugs in chronic pyelonephritis. Tutorial. Moscow, 1977. P. 23.
- Nephrology in 2 vols. edited by I. E. Tareeva.
Questions that a general practitioner should answer when choosing a uroseptic
- At what pH of the environment is the uroseptic effect optimally realized?
- What is the possibility of the combined use of uroseptics, their interactions, synergism or antagonism of action?
- What is the required duration of course therapy to obtain the best effect?
- How quickly does drug resistance develop?
- What is the most appropriate route of administration of the drug?
- What is the optimal dose needed to treat a particular patient?
- What is the nephrotoxicity of uroseptic?
- What are the possible side effects?
Indications for use
The tablets create a complex effect on the body, so they are widely used. Most often they are used in such cases:
- Relief of severe pain syndromes: radiculitis, severe pain and muscle pain,
- Treatment of neuralgia – inflammation of peripheral nerves,
- Headache and migraine,
- Toothache,
- Colds and acute respiratory viral infections, to relieve the inflammatory process and reduce temperature, especially in cases of fever,
- Reducing severe menstrual pain.
The need to take the drug and its interaction with other drugs is determined by the attending physician. It is not recommended to use with other painkillers, as well as sedatives, including herbal products.