Adrenaline and norepinephrine - what's the difference?
The content of the article
The connection between adrenaline and norepinephrine does not end with a similar name. Both chemicals belong to the group of catechol amines, synthesized from the amino acid tyrosine into dopamine, which is converted into norepinephrine. Adrenaline is an analogue of norepinephrine, formed as a result of its further transformation, thanks to the catalyzing enzyme - N-methyltransferase.
Each of these chemical compounds has its own functions in the body, and although they usually stimulate the same receptors, they are characterized by different receptor affinities and therefore show similar but different physiological functionality in the sympathetic nervous system.
- Norepinephrine
. Responsible for reactions of arousal state, mood changes and participates in the central regulation of pressure. It stimulates alpha adrenergic receptors. - Adrenaline
. Has a systemic effect. Stimulates all types of alpha-adrenergic and beta-adrenergic receptors.
Structures that produce, store, and release catechol amines into the bloodstream include the adrenal nucleus and neurons of the sympathetic system. The adrenal nucleus is responsible for 80% of the production of adrenaline, and the sympathetic system is responsible for the production of norepinephrine.
Both epinephrine and norepinephrine are responsible for inhibiting (suppressing) insulin secretion and stimulating glucagon release, causing a decrease in blood glucose levels.
How to trigger an adrenaline rush?
The production of adrenaline is associated with a person’s emotional state. Its release can be provoked artificially. For this it is enough:
- watch a scary movie;
- jump with a parachute;
- play dangerous games;
- see something scary, etc.
For some people, it is enough to “wind up” themselves in order for the hormone to begin its independent production. It is impossible to regulate it with products. These are exclusively emotions and the work of the nervous system.
A mind full of anxiety and various obsessive thoughts can trigger the production of the hormone. This is especially true at night, when there is silence in the apartment and various thoughts creep into your head. The receptive brain is able to draw various pictures, which is accompanied not only by fear, but also by an active loss of energy.
To control the stress hormone, it is enough to organize your thoughts. Minimize TV viewing, remove sources of bright light before bed, remove mobile phones and music.
Adrenaline - what is this hormone?
Adrenaline is the name of a hormone produced by the adrenal nucleus, which loosely translated from Latin and Greek means “above the kidney.” It was first isolated in 1895 by the Pole N. Cybulski. The hormone is a biogenic amine and is also found in plants. Colloquially it is called the stress, fight or flight hormone because its action triggers the body's defenses characteristic of life-threatening conditions.
The secretion of large amounts of adrenaline is activated by strong stressful stimuli and causes the body to quickly make extraordinary efforts. Epinephrine, released into the blood, works quickly and is quickly deactivated and degraded by monoamine oxidase and catechol-O-methyltransferase.
An increase in the concentration of adrenaline in the blood causes:
- a sharp increase in blood pressure, causing the brain, heart and muscles to receive higher doses of oxygen;
- increased ACTH secretion, i.e. adrenocorticotropic hormone, which triggers a number of alarm reactions in the body;
- tachycardia, manifested by an accelerated heartbeat;
- expansion of the smooth muscles of the bronchi, due to which the patient breathes easier, and the pupils;
- reduction of itching, angioedema and urticaria symptoms, which are the consequences of contact of an allergic person with a sensitizing substance;
- spasms of blood vessels of the circulatory system: veins, arteries and capillaries;
- decreased secretion of mucus and digestive juices in the digestive system and inhibition of intestinal motility and hunger;
- elevated blood sugar levels (hyperglycemia).
Introduction[edit | edit code]
Adrenalin
– one of the catecholamines, it is a hormone of the adrenal medulla and extra-adrenal chromaffin tissue. Under the influence of adrenaline, the blood glucose level increases and tissue metabolism increases. Adrenaline enhances gluconeogenesis (glucose synthesis), inhibits glycogen synthesis in the liver and skeletal muscles, enhances the uptake and utilization of glucose by tissues, increasing the activity of glycolytic enzymes. Adrenaline also enhances lipolysis (fat breakdown) and inhibits fat synthesis. At high concentrations, adrenaline enhances protein catabolism.
Adrenaline has the ability to increase blood pressure by constricting blood vessels in the skin and other small peripheral vessels and speed up the breathing rate. The level of adrenaline in the blood increases, including with increased muscle work or a decrease in sugar levels. The amount of adrenaline released in the first case is directly proportional to the intensity of the training session. Adrenaline causes relaxation of the smooth muscles of the bronchi and intestines, dilation of the pupils (due to contraction of the radial muscles of the iris, which have adrenergic innervation). It is the property of sharply increasing blood sugar levels that has made adrenaline an indispensable tool in removing patients from a state of deep hypoglycemia caused by an overdose of insulin.
Adrenaline[edit | edit code]
Source:
Clinical Pharmacology by Goodman and Gilman Volume 1
.
Editor
: Professor A.G.
Gilman Ed.
: Practice, 2006.
Adrenaline is a powerful stimulant of both α and β adrenergic receptors, and therefore its effects are varied and complex. Most of the effects that are given in table. 6.1, occur in response to the administration of exogenous adrenaline. At the same time, many reactions (for example, sweating, piloerection, dilated pupils) depend on the physiological state of the body as a whole. Adrenaline has a particularly strong effect on the heart, as well as on blood vessels and other smooth muscle organs.
Arterial pressure
. Adrenaline is one of the most powerful pressor substances. When administered intravenously in pharmacological doses, it causes a rapid increase in blood pressure, the degree of which directly depends on the dose. At the same time, systolic blood pressure increases more than diastolic blood pressure, that is, pulse blood pressure increases. As the reaction to adrenaline subsides, the average blood pressure may temporarily become lower than the initial value and only then return to its previous value.
The pressor effect of adrenaline is due to three mechanisms: 1) direct stimulating effect on the working myocardium (positive inotropic effect), 2) increase in heart rate (positive chronotropic effect), 3) narrowing of resistive precapillary vessels of many areas (especially skin, mucous membranes and kidneys) and pronounced narrowing veins At the height of the rise in blood pressure, heart rate may decrease due to a reflex increase in parasympathetic tone. In small doses (0.1 mcg/kg), adrenaline can cause a decrease in blood pressure. This effect, as well as the biphasic effect of large doses of adrenaline, is explained by the higher sensitivity of β2-adrenergic receptors (causing vasodilation) to this substance compared to α-adrenergic receptors.
Figure 10.2. Effects of intravenous infusions of epinephrine, norepinephrine and isoprenaline in humans. Allwood et al., 1963.
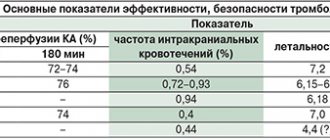
With subcutaneous or slow intravenous administration of adrenaline, the picture is somewhat different. With subcutaneous administration, adrenaline is absorbed slowly due to local vasoconstriction: the effect of such an injection of 0.5-1.5 mg of adrenaline is the same as with intravenous infusion at a rate of 10-30 mcg/min. There is a moderate increase in systolic blood pressure and cardiac output due to the positive inotropic effect. OPSS decreases due to the fact that activation of β2-adrenergic receptors of skeletal muscle vessels predominates (muscle blood flow increases); as a result, diastolic blood pressure decreases. Since mean blood pressure, as a rule, increases slightly, compensatory baroreflex effects on the heart are weakly expressed. Heart rate, cardiac output, stroke volume, and left ventricular stroke work all increase as a result of both a direct stimulatory effect on the heart and increased venous return (the latter indicated by increased right atrial pressure). At a slightly higher infusion rate, OPSS and diastolic blood pressure may not change or slightly increase, depending on the dose, and, consequently, the relationship between the activation of α- and β-adrenergic receptors in different vascular territories. In addition, compensatory reflex reactions may develop. A comparison of the effects of intravenous infusion of epinephrine, norepinephrine and isoprenaline in humans is shown in Fig. 10.2 and in table. 10.2.
Table 10.2. Reactions to intravenous infusion of epinephrine and norepinephrine in humans"
Blood vessels
. Adrenaline acts primarily on arterioles and precapillary sphincters, although veins and large arteries also respond to it. The vessels of different organs respond to adrenaline in different ways, which leads to a significant redistribution of blood flow.
Exogenous adrenaline causes a sharp decrease in skin blood flow due to narrowing of precapillary vessels and venules. This is why blood flow in the hands and feet decreases. In the mucous membranes, when adrenaline is applied locally, hyperemia develops after the initial vasoconstriction. It is apparently caused not by the activation of β-adrenergic receptors, but by the vascular response to hypoxia.
In humans, therapeutic doses of epinephrine cause an increase in muscle blood flow. It is partly due to a sharp activation of β2-adrenergic receptors, only to a small extent compensated by activation of α-adrenergic receptors. Against the background of α-adrenergic blockers, the dilation of muscle vessels becomes even more pronounced, peripheral vascular resistance and mean blood pressure decrease (paradoxical reaction to adrenaline). On the contrary, against the background of non-selective beta-blockers, blood vessels narrow and blood pressure rises sharply.
The effect of adrenaline on cerebral blood flow is mediated by changes in blood pressure. In therapeutic doses, adrenaline causes only a slight constriction of cerebral vessels. When sympathetic tone increases under stress, cerebral vessels also do not constrict, which is physiologically justified - a possible increase in cerebral blood flow in response to increased blood pressure is limited by autoregulation mechanisms.
At doses that have little effect on mean blood pressure, epinephrine increases renal vascular resistance, reducing renal blood flow by approximately 40%. All renal vessels participate in this reaction. Since GFR changes only slightly, the filtration fraction increases sharply. Excretion of Na+, K+ and SG decreases; diuresis may increase, decrease or remain unchanged. The maximum rates of tubular reabsorption and secretion do not change. As a result of the direct effect of adrenaline on beta-adrenergic receptors of juxtaglomerular cells, renin secretion increases.
Under the influence of adrenaline, the pressure in the pulmonary arteries and veins increases. The reason is not only the direct vasoconstrictor effect of adrenaline on the lungs, but also, of course, the redistribution of blood in favor of the small circle due to the contraction of powerful smooth muscles of the systemic veins. At very high concentrations, epinephrine causes pulmonary edema due to increased filtration pressure in the pulmonary capillaries and possibly increased capillary permeability.
Under physiological conditions, adrenaline and stimulation of the sympathetic cardiac nerves cause an increase in coronary blood flow. This is observed even when doses of epinephrine are administered that do not increase aortic pressure (that is, coronary perfusion pressure). This effect is based on two mechanisms. First, as heart rate increases, the relative duration of diastole increases (see below); however, this is partially counteracted by a decrease in coronary blood flow during systole due to more powerful contraction of the heart and compression of the coronary vessels. If, in addition, the pressure in the aorta increases, then coronary blood flow in diastole increases even more. Secondly, an increase in the strength of contractions and oxygen consumption by the heart leads to the release of vasodilatory metabolites (primarily adenosine); the action of these metabolites overcomes the direct constricting effect of adrenaline on the coronary vessels.
Heart
. Adrenaline has a powerful stimulating effect on the heart. It acts predominantly on β1-adrenergic receptors of the cells of the working myocardium and conduction system, since these receptors predominate in the heart (there are also α- and β2-adrenergic receptors, although their content in the heart greatly depends on the type of animal).
Recently, the role of β1- and β2-adrenergic receptors in the regulation of the heart in humans, and especially in the development of heart failure, has attracted great interest. Under the influence of adrenaline, heart rate increases, and arrhythmias often occur. Systole is shortened, the strength of contractions and cardiac output increase, the work of the heart and its oxygen consumption increase sharply. The efficiency of the heart, measured by the ratio of work to oxygen consumption, decreases. The primary effects of adrenaline include an increase in the strength of contractions, the rate of increase in pressure in the phase of isovolumic tension and the decrease in pressure in the phase of isovolumic relaxation, a decrease in the time to reach maximum intraventricular pressure, an increase in excitability, an increase in heart rate and automatism of cells of the conduction system.
By increasing heart rate, adrenaline simultaneously shortens systole, so that the duration of diastole usually does not decrease. This is achieved, in particular, due to the fact that activation of β-adrenergic receptors is accompanied by an increase in the rate of diastolic relaxation. The increase in heart rate is due to the acceleration of spontaneous diastolic depolarization (phase 4) of the cells of the sinus node; in this case, the membrane potential quickly reaches a critical level at which an action potential occurs (Chapter 35). The amplitude and slope of the action potential also increase. Migration of the pacemaker within the sinus node is often observed (due to the activation of latent pacemakers). Adrenaline increases the rate of spontaneous diastolic depolarization in Purkinje fibers, which can also lead to activation of latent pacemakers. These changes are not observed in working cardiomyocytes, since in phase 4 they do not register spontaneous diastolic depolarization, but a stable resting potential. In high doses, adrenaline can cause ventricular extrasystoles - harbingers of more serious rhythm disturbances. When using therapeutic doses in humans, this is rarely observed, however, in conditions of increased sensitivity of the heart to adrenaline (for example, under the influence of certain drugs for general anesthesia) or during myocardial infarction, the release of endogenous adrenaline can cause ventricular extrasystoles, ventricular tachycardia and even ventricular fibrillation. The mechanisms of this phenomenon are poorly understood.
Some effects of adrenaline on the heart are due to an increase in heart rate and are not observed under conditions of an imposed rhythm or are inconsistent. These include, for example, changes in the repolarization of working cardiomyocytes of the atria and ventricles and Purkinje fibers. An increase in heart rate itself causes a shortening of the action potential, and therefore the refractory period.
Conduction in the system of Purkinje fibers depends on their membrane potential at the moment of arrival of the excitation wave. Severe depolarization leads to conduction disturbances, from slowing to blockade. Under these conditions, adrenaline often restores normal membrane potential, and thereby conductivity.
Adrenaline shortens the refractory period of the AV node (although in those doses at which heart rate decreases due to a reflex increase in parasympathetic tone, adrenaline can also cause an indirect prolongation of this period). In addition, epinephrine reduces the degree of AV block caused by heart disease, certain medications, or increased parasympathetic tone. Against the background of increased parasympathetic tone, adrenaline can cause supraventricular arrhythmias. In adrenaline-induced ventricular arrhythmias, parasympathetic influences also appear to play a role, leading to a slowdown in the frequency of sinus node discharges and AV conduction velocity. This is confirmed by the fact that the risk of such arrhythmias is reduced with drugs that reduce parasympathetic effects on the heart. The increase in cardiac automaticity under the influence of adrenaline and its arrhythmogenic effect are effectively suppressed by β-blockers, such as propranolol. Most structures of the heart also contain α1-adrenergic receptors; their activation leads to a lengthening of the refractory period and an increase in the strength of contractions.
Cardiac arrhythmias have been described in humans after accidental intravenous administration of adrenaline in doses intended for intravenous administration. Ventricular extrasystoles occurred, followed by polytopic ventricular tachycardia or ventricular fibrillation. Adrenaline pulmonary edema is also known. Under the influence of adrenaline in healthy individuals, the amplitude of the T wave decreases. In animals, when relatively high doses are administered, other changes in the T wave and ST segment are observed: the T wave, after a decrease, becomes biphasic, and the ST segment deviates in one direction or another from the isoline. The same changes in the ST segment are observed in patients with coronary artery disease with spontaneous or adrenaline-induced angina, and therefore these changes are attributed to myocardial ischemia. In addition, epinephrine and other catecholamines can cause the death of cardiomyocytes, especially when administered intravenously. Acute toxic effects of adrenaline are manifested by contracture damage to myofibrils and other pathomorphological changes. Recently, the question of whether prolonged sympathetic stimulation of the heart (for example, in heart failure) can cause apoptosis of cardiomyocytes has been actively studied.
Gastrointestinal tract, uterus and urinary tract
. The effect of adrenaline on different smooth muscle organs depends on which adrenergic receptors predominate in them (Table 6.1). Its effect on blood vessels is of the utmost physiological importance; the impact on the gastrointestinal tract is not nearly as significant. Typically, adrenaline causes relaxation of gastrointestinal smooth muscle due to the activation of both α- and β-adrenergic receptors. Intestinal tone and the frequency of its spontaneous contractions decrease. The stomach usually relaxes, and the pyloric sphincter and cecal sphincter contract, but these effects depend on the initial tone. If this tone is high, then adrenaline causes relaxation, and if it is low, it causes contraction.
The effect of adrenaline on the uterus depends on the type of animal, the phase of the menstrual (estrous) cycle, pregnancy and its stage, as well as the dose. In vitro, adrenaline causes contraction of the stripes of both pregnant and non-pregnant human uteruses due to activation of α-adrenergic receptors. In vivo, the effect of adrenaline is more complex; in the last month of pregnancy and during pregnancy, it causes, on the contrary, a decrease in the tone and contractile activity of the uterus. In this regard, selective β2-agonists (for example, ritodrine and terbutaline) are used in cases of threatened preterm labor, although their effectiveness is low. The effects of these and other tocolytic agents are discussed below.
Adrenaline causes relaxation of the detrusor muscle (due to activation of beta-adrenergic receptors) and contraction of the vesical triangle and bladder sphincter (due to activation of α-adrenergic receptors). This (as well as increased contractions of the smooth muscles of the prostate gland) can lead to difficulty starting urination and urinary retention.
Respiratory system
. The effect of adrenaline on the respiratory system comes down mainly to relaxation of the smooth muscles of the bronchi. The powerful bronchodilatory effect of adrenaline is further enhanced under conditions of bronchospasm - which occurs, for example, during an attack of bronchial asthma or as a result of taking certain medications. In such cases, adrenaline plays the role of an antagonist of bronchoconstrictor substances, and its effect can be extremely strong.
The effectiveness of epinephrine in bronchial asthma may also be associated with the suppression of antigen-induced release of inflammatory mediators from mast cells and, to a lesser extent, with a decrease in the secretion of tracheobronchial glands and a decrease in mucosal edema. Suppression of mast cell degranulation is due to activation of β2-adrenoreceptors, and the effect on the bronchial mucosa is due to activation of α-adrenoreceptors. However, in bronchial asthma, the anti-inflammatory effects of substances such as glucocorticoids and leukotriene antagonists are much stronger (Chapter 28).
CNS
. The adrenaline molecule is quite polar, so it does not penetrate the blood-brain barrier well and does not have a psychostimulating effect in therapeutic doses. Restlessness, anxiety, headache and tremor, which often occur with the administration of epinephrine, are explained rather by its effects on the cardiovascular system, skeletal muscles and metabolism; in other words, they can arise as a result of a mental reaction to somatic and vegetative manifestations characteristic of stress. Some other adrenergic agents are able to penetrate the blood-brain barrier.
Metabolism
. Adrenaline affects many metabolic processes. It increases the concentrations of glucose and lactic acid in the blood (Chapter 6). Activation of α2-adrenergic receptors leads to inhibition of insulin production, and β2-adrenergic receptors - vice versa; When adrenaline acts, the inhibitory component predominates. By acting on the P-adrenergic receptors of the α-cells of the pancreatic islets, adrenaline stimulates the secretion of glucagon. It also inhibits tissue glucose uptake, at least in part through inhibition of insulin production, but also possibly through a direct effect on skeletal muscle. Glucosuria is rarely caused by adrenaline. In most tissues and most animal species, epinephrine stimulates gluconeogenesis by activating β-adrenergic receptors (Chapter 6).
Acting on beta-adrenergic receptors of lipocytes, adrenaline activates hormone-sensitive lipase, which leads to the breakdown of triglycerides to glycerol and free fatty acids and an increase in the level of the latter in the blood. Under the influence of adrenaline, basal metabolism increases (when using normal therapeutic doses, oxygen consumption increases by 20-30%). This is mainly due to increased breakdown of brown adipose tissue.
Other effects
. Under the influence of adrenaline, the filtration of protein-free fluid into the tissue increases. As a result, the BCC decreases and the relative content of red blood cells and proteins in the blood increases. Normally, ordinary doses of adrenaline have almost no such effect, but it is observed with shock, blood loss, arterial hypotension and general anesthesia. Adrenaline causes a rapid increase in the number of neutrophils in the blood, apparently due to a decrease in their marginal position mediated by β-adrenergic receptors. In both animals and humans, adrenaline accelerates blood clotting and fibrinolysis.
The effect of adrenaline on the exocrine glands is weak. In most cases, their secretion is somewhat reduced, partly due to vasoconstriction and reduced blood flow. Adrenaline increases tear production and causes the formation of a small amount of viscous saliva. With systemic administration of adrenaline, piloerection and sweating almost do not occur, but with intradermal administration of adrenaline or norepinephrine in low concentrations, they are quite pronounced. This effect is eliminated by α-blockers.
Irritation of the sympathetic nerves almost always causes the pupils to dilate, but adrenaline instilled into the eyes does not have this effect. At the same time, it usually causes a decrease in intraocular pressure, both in normal conditions and in open-angle glaucoma. The mechanism of this is not clear: apparently, there is both a decrease in the formation of aqueous humor due to vasoconstriction, and an improvement in its outflow (Chapter 66).
Adrenaline itself does not cause excitation of skeletal mice, but it facilitates conduction at neuromuscular synapses, especially with prolonged and frequent irritation of motor nerves. Stimulation of α-adrenergic receptors (obviously α-adrenergic receptors) at the endings of motor somatic nerves increases the amount of released acetylcholine, apparently due to increased Ca2″ entry into these endings; It is interesting that in the endings of the autonomic nerves, activation of a2-adrenergic receptors leads, on the contrary, to a decrease in the release of the mediator. This may partly explain the short-term increase in muscle strength when adrenaline is injected into the arteries of the limbs in patients with myasthenia gravis. In addition, adrenaline has a direct effect on white (fast) muscle fibers, prolonging their active state and thereby increasing maximum tension. A more important physiological and clinical effect is the ability of epinephrine and selective β2-agonists to enhance natural tremor. This ability is due, at least in part, to a β-adrenergic receptor-mediated increase in muscle spindle discharge.
Epinephrine reduces the concentration of K+ in the blood, mainly through β2-adrenergic receptor-mediated uptake of K+ into tissues, and especially skeletal muscles. This is accompanied by a decrease in renal K+ excretion. This feature of β2-adrenergic receptors is used in the treatment of familial hyperkalemic periodic paralysis, a disease characterized by attacks of flaccid paralysis, hyperkalemia and depolarization of skeletal muscles. The selective β2-adrenergic agonist salbutamol appears to partially restore the ability of muscles to capture and retain K+ in such patients.
Large doses or repeated administrations of epinephrine and other adrenergic drugs cause arterial and myocardial damage in animals. This damage can be so severe that necrotic foci appear in the heart, indistinguishable from infarction. The mechanism of this action is not clear, but it is quite effectively prevented by α- and beta-blockers and calcium antagonists. Similar lesions occur in patients with pheochromocytoma or after long-term administration of norepinephrine.
Pharmacokinetics
. As already mentioned, adrenaline when taken orally is ineffective, as it quickly oxidizes and conjugates in the gastrointestinal mucosa and in the liver. Its absorption during subcutaneous administration occurs slowly due to local vasospasm, and in case of arterial hypotension (for example, shock) it can slow down even more. With intramuscular administration, adrenaline is absorbed faster. In emergency cases, it is sometimes necessary to administer intravenous adrenaline. When inhaling nebulized solutions of adrenaline, even quite concentrated (1%), it acts primarily on the respiratory tract, although systemic reactions (for example, cardiac arrhythmias) have also been described, especially at a high total dose.
Elimination of adrenaline occurs quickly. The main role in it is played by the liver, which is rich in COMT and MAO, both enzymes responsible for the metabolism of adrenaline (Fig. 6.5). Normally, the content of adrenaline in the urine is very low, but with pheochromocytoma, the concentration of adrenaline, norepinephrine and their metabolites increases sharply.
There are several adrenaline preparations. They are intended for use for different indications and for administration in different ways: there are preparations for injection (usually subcutaneous, but in special cases - intravenous), inhalation, and topical use. In an alkaline solution, adrenaline is unstable: in air it first turns pink due to oxidation with the formation of adrenochrome, and then turns brown due to the formation of polymers. Adrenaline for injection exists in the form of solutions of 1:1000, 1:10,000 and 1:100,000. Adults are usually administered 0.3-0.5 mg of adrenaline subcutaneously. If you need to get a quick and reliable effect, then administer intravenous adrenaline with caution. In this case, adrenaline should be diluted and administered very slowly; the dose rarely exceeds 0.25 mg, except in cases of circulatory arrest. Epinephrine in suspension is slowly absorbed when administered subcutaneously; This drug should never be given intravenously. There is also a 1:100(1%) solution for inhalation. Every precaution must be taken to ensure that this solution is not confused with the 1:1000 (0.1%) solution for injection: parenteral administration of the 1:100 solution may cause death.
Side effects and contraindications
. Unpleasant side effects of adrenaline include restlessness, throbbing headache, tremors, and palpitations. All these effects quickly disappear if the patient is reassured and advised to lie down.
There are also more severe complications. The use of large doses of adrenaline or its too rapid intravenous administration can lead to a sharp increase in blood pressure and hemorrhagic stroke. Arrhythmias caused by adrenaline, in particular ventricular ones, are known. In patients with coronary artery disease, adrenaline can cause an attack of angina.
Epinephrine is usually contraindicated in patients taking non-selective β-blockers; in these conditions, the predominant activation of vascular α1-adrenergic receptors can cause a sharp rise in blood pressure and hemorrhagic stroke.
Application
. There are few indications for prescribing adrenaline. As a rule, its effects on the heart, blood vessels and bronchi are used. In the past, epinephrine was used to relieve bronchospasm, but selective β2-agonists are now preferred. An important indication is allergic reactions (especially anaphylactic) to medications and other allergens. Epinephrine is administered together with local anesthetics to prolong their action (the mechanism appears to be local vasospasm). With asystole of various origins, adrenaline can restore the activity of the heart. Locally, adrenaline is used to stop bleeding, for example, during tooth extraction (systemic reactions are possible) or gastroduodenoscopy. Finally, adrenaline is used for post-intubation laryngeal stenosis or false croup. The clinical use of epinephrine will be discussed below when other adrenergic agents are discussed.
Adrenaline is a neurotransmitter
Neurotransmitters are substances with a diverse chemical structure that meet certain criteria:
- produced in the bodies of nerve cells and their endings and stored in synaptic vesicles;
- respond to electrical stimuli through which they are released and then connect to specific receptors, after which they induce a response in postsynaptic neurons;
- when introduced into the body from the outside, they act by analogy with substances naturally produced by the body;
- After performing their function in the body, they are removed from the site of action by a certain mechanism.
Adrenaline meets all of the above criteria, being a neurotransmitter characterized by synaptic and extrasynaptic release. It is also a peripheral pain mediator that temporarily increases the body's tolerance to pain.
Indications for use
Adrenaline is used in many areas of medicine:
Allergology - during the occurrence of acute allergic reactions during anaphylactic shock caused by the body's reaction to allergens, and anaphylactoid situations that can occur suddenly, due to the body's reaction to factors that did not previously cause sensitization;
Ophthalmology - for the treatment of open-angle glaucoma;
Cardiology - in the treatment of cardiogenic shock;
ENT and dentistry - decongestants of the mucous membrane. Used after bleeding procedures - removal of teeth, tonsils;
Anesthesiology - because in combination with local anesthetics it prolongs the analgesic effect.
Contraindications to taking adrenaline
Adrenaline is a life-saving drug, so there are no absolute contraindications to its use. In case of life-threatening conditions provoked by anaphylactic shock or other symptoms listed in the indications, you should immediately give the drug and then call an ambulance.
In other cases, if possible, relative risk factors should be excluded before administering epinephrine, which include:
- hyperthyroidism;
- arterial hypertension;
- pulmonary embolism;
- cardiovascular diseases;
- renal failure;
- pregnancy;
- cardiac ischemia.
Dosage and routes of administration
Epinephrine can be purchased at pharmacies as a clear solution in a pre-filled syringe. This form allows for quick, intuitive and independent administration of the drug to children and adults.
The drug with adrenaline should be injected only into the muscle located in the anterolateral part of the thigh. The injection site is then massaged to disperse the drug more quickly throughout the body.
The volume of drug administration is calculated based on the patient’s body weight. It is suggested that both children and adults weighing more than 30 kg should receive a single dose of 0.3 ml of epinephrine. Each prefilled syringe is a single-use product containing 1 ml of drug.
Although the amount of the drug recommended for a single administration, i.e. 0.3 ml, less than in a syringe, the medicine cannot be reused. If symptoms do not improve or worsen, a second, same dose may be given from the next syringe.
Children weighing less than 30 kg also need to take a dose of 0.3 ml of adrenaline, since the design of the syringe does not allow the administration of a different amount of the drug.
The advantage of a prefilled syringe is that it has a built-in lock, preventing you from injecting a larger dose of the drug than recommended. This is a huge advantage, because the condition of the patient who has to inject himself with adrenaline often interferes with clear thinking and precise movements.
The drug should be used immediately after the onset of symptoms of shock: redness of the skin, angioedema, breathing problems, cardiovascular problems and urticaria. After taking adrenaline, you should always call an ambulance.
Other routes of administration of adrenaline (inhalation or sublingual form) and doses of the drug can only be used by physicians.
Outpatient and inpatient treatment
The Mental Health Clinic successfully combines the treatment of panic attacks both with medication and through psychotherapy. Most often, treatment for panic attacks is carried out on an outpatient basis, but there are also options for inpatient placement. The attending physician will select an antidepressant that will help relieve acute symptoms and draw up a treatment plan, including the prevention and relief of possible recurrences of panic attacks. Patients who clearly know how to help themselves when the disease manifests itself experience significantly less fear of the manifestation of a crisis, which reduces general anxiety and raises the emotional background in general. However, the most important psychiatric help for panic attacks is to conduct active psychotherapeutic work with the patient. This will allow you to find the root cause of the disease and, by completely eliminating it, get rid of the disease forever.
We can help you! Call us
Side effects and adrenaline overdose
Like any drug, epinephrine can cause side effects. The most common:
- anxiety, restlessness, difficulty breathing;
- weakness of the body, headaches, dizziness, body tremors;
- pale skin;
- nausea and vomiting;
- tachycardia and pronounced palpitations;
- weakened blood circulation in the form of cold extremities;
- increased activity of the sweat glands.
Overdosing on epinephrine is difficult because of the precisely measured doses of the drug in pre-filled syringes and their design, which prevents more adrenaline from being injected. However, dangerous erroneous intravascular administration of the drug can occur, which can result in cerebral hemorrhage.
Taking too much adrenaline can also cause acute pulmonary edema, which can lead to death.
Consequences of deficiency and excess of adrenaline
Epinephrine deficiency is a rare condition that may result from genetic defects and insufficiency of the adrenal glands that produce it.
Elevated levels of adrenaline in the blood are also rare, however, if they occur, it may indicate the development of tumors in the adrenal glands and neuroendocrine tumors and lead to hypertension.
The consequences of untreated long-term elevated adrenaline levels are kidney and heart damage. Symptoms of increased adrenaline in the blood are similar to the increase in its amount caused by stressful situations.
Symptoms
The symptoms of a panic attack can vary from person to person. This is due to the fact that symptoms are the results of the human body’s struggle with unexpected chemical processes, and exactly how this struggle will manifest itself depends on the individual characteristics of the person. During a panic attack, you may experience difficulty breathing (a feeling that your throat is swelling), rapid heartbeat, and pulsating blood in your temples. A person may feel sick, feel either hot or cold, or feel uncontrollable trembling. But in the end, the most difficult feeling is a feeling of sudden and overwhelming fear or panic.
Adrenaline test
If symptoms occur - prolonged acceleration of the heart rate, persistent increased sweating, increased blood pressure and severe headaches, a test for the concentration of methoxycatecholamines (which includes adrenaline and norepinephrine) in the urine should be performed. This test is more adequate than samples taken from blood, since the act of drawing blood can be stressful for the patient, and thus the concentration of adrenaline in the blood will increase.
Approximately 3 days before the examination, it is recommended to give up coffee, tea, citrus fruits, chocolate and vanilla. You should also minimize your exposure to stress and not engage in intense sports.
In a special urine container purchased from a pharmacy, samples should be collected within 24 hours. Between adding additional urine to the container, store it covered in the refrigerator and then submit it to the laboratory.
Functions
To understand the biological role of adrenaline, you need to remember that it is the main effector (transmitting signals from the centers of the brain to the executive organs) neurotransmitter of the sympathetic department of the autonomic system. Adrenaline is responsible for the response known as “fight or flight”, which occurs in times of danger. Due to an increase in the concentration of the neurotransmitter, physiological processes occur:
- Increased heart rate and strength.
- Expansion of the lumen of the bronchi.
- Reduction of the vascular lumen of the arterioles of the skin while simultaneously expanding the diameter of the vessels located in the muscle tissue.
- Acceleration of the process of glycogenolysis (breakdown of glycogen to glucose).
- Increased secretion of renin (an element of the renin-angiotensin system involved in the regulation of blood pressure).
- Acceleration of the process of lipolysis (breakdown of fats).
The main functions of catecholamines are associated with maintaining mental and physical activity. These transmitters affect the speed and quality of intellectual information processing. The concentration of catecholamines increases with mental and physical stress. Adrenaline gives a natural doping effect. If the secretion of the hormone increases, a person becomes hardy and resistant to stress of any type.
A decrease in the rate of catecholamine production is accompanied by a deterioration in performance, a slowdown in mental processes, a deterioration in mood, and the development of a depressive state. The main function of the hormone adrenaline is to adapt the body to stress. A long-term increase in the concentration of the hormone in the blood helps to build muscle mass and increase the size of the myocardium. Other features:
- Helps increase the permeability of cell membranes to glucose.
- Accelerates the breakdown of carbohydrates and fats.
- Helps increase blood pressure.
The mechanism of action of adrenaline in biochemistry is based on instant distribution throughout the body along with the bloodstream, due to which it quickly activates the work of all organs and systems, preparing the body to counteract a dangerous or stressful situation. The concentration of the hormone in the blood at the time of stress can increase 100 times in a few seconds (compared to the norm).