Home | About us | Delivery | Advertisers | Login | Registration
The pharmacy is closed on Sundays and holidays.
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2021 Pharmacy 84.
The value of hyoscine butyl bromide in the treatment of abdominal pain
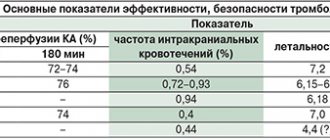
LA Samuels (Samuels LA Pharmacotherapy update: Hyoscine Butylbromide in the treatment of abdominal spasms // Clinical Medicine: Therapeutics. 2009. Vol. 1. P. 647–665) begins a literature review on the value of hyoscine butylbromide in the treatment of abdominal spasmodic pain, with stating that abdominal pain is one of the most common reasons for seeking medical help after headache, back pain and dizziness. Abdominal pain can be a symptom of both transient and self-resolving disorders, and life-threatening conditions requiring immediate medical intervention. Establishing the correct diagnosis when interpreting abdominal pain can be very difficult, since various diseases are hidden behind it, which is the task of general practitioners, surgeons, internists, emergency medicine specialists, pediatricians, gastroenterologists, urologists, and gynecologists. Hyoscine butyl bromide (or scopalamine-N-butyl bromide, N-butylscopolammonium bromide and butylscopolamine) according to the mechanism of its therapeutic effect is a neurotropic antispasmodic. Acetylcholine (ACCh) serves as the main neurotransmitter of the parasympathetic nervous system and acts on 2 types of receptors - muscarinic and nicotinic cholinergic. When stimulated, the preganglionic nerve releases ACh into the ganglion, and it acts on the nicotinic receptors of the postganglionic neurons. The postganglionic neuron then releases ACh to excite muscarinic receptors in the target organ. Several types of muscarinic receptors are known; from the point of view of the mechanism of action of hyoscine butylbromide, the most interesting are the M3 receptors located in the smooth muscles of blood vessels, bronchi and the gastrointestinal tract (GIT), as well as various glands of the respiratory system and GIT. Stimulation of these receptors leads to indirect vasodilation (due to the formation of nitric oxide), bronchoconstriction, increased gastrointestinal motility, and increased glandular secretion. M3 receptors are also found in the ciliary body and muscles of the iris, where they are involved in accommodation and control pupil size. M2 and M3 receptors are found in the organs of the genitourinary system. Hyoscine butyl bromide has a dual mechanism of action. Firstly, it blocks the action of ACh on muscarinic smooth muscle receptors, eliminates spasm of smooth muscles of the gastrointestinal tract and genitourinary tract, and also reduces the motility of these organs. Secondly, hyoscine butyl bromide is a non-competitive blocker of nicotinic receptors, due to which an antisecretory effect is realized, which is manifested by a decrease in the secretion of the digestive glands. The action of Buscopan is realized throughout the gastrointestinal tract, including its upper and lower sections. Therefore, it is prescribed for spasms that occur in various parts of the gastrointestinal tract, for biliary colic, cystitis, urethritis and primary dysmenorrhea. Hyoscine butyl bromide is used to prevent gastrointestinal spasms before diagnostic studies (X-ray, endoscopic retrograde cholangiopancreatography, colonoscopy). Hyoscine butyl bromide is a quaternary ammonium compound; its molecule is polarized and retains polarity regardless of the pH of the environment. In this regard, when administered orally, the drug is insignificantly absorbed (8%), and systemic bioavailability is less than 1%. Despite the low blood levels that are recorded transiently, hyoscine butyl bromide and/or its metabolites are detected at the sites of action. When administered intravenously, the drug does not penetrate the blood-brain barrier and has low binding to plasma proteins. LA Samuels provides a summary of studies of hyoscine butyl bromide for abdominal colic and irritable bowel syndrome (IBS), renal colic, dysmenorrhea, as well as its potential in childbirth and diagnostic procedures. Abdominal pain (“nonspecific colic”) and IBS The basis for the prescription of hyoscine butyl bromide for nonspecific colicky abdominal pain is its antimuscarinic effect. Clinically, this effect is manifested by relaxation of the smooth muscles of the gastrointestinal tract with a decrease or disappearance of the spasm felt by the patient. This effect was objectively demonstrated in a study of the electrical and biomechanical activity of the stomach: intravenous administration of 20 mg of hyoscine butyl bromide led to a decrease in the mechanical motility index by 50.9%, and an electrical motility index decreased by 36.5% [1]. Efficacy and safety of hyoscine butyl bromide at a dose of 10 mg 3 times a day. in comparison with paracetamol 500 mg 3 times/day, their combination and placebo were studied for recurrent cramping abdominal pain [2]. 1637 patients (after placebo for 1 week) were randomized into 4 groups depending on treatment, which lasted 3 weeks. Pain severity (as measured by visual analogue scale (VAS) and verbal rating scale) was statistically significantly reduced in all treatment groups compared to placebo. Treatment was well tolerated in all groups, and the incidence of side effects did not differ significantly between groups (including placebo). GN Tytgat has published reviews of the literature regarding the use of oral and parenteral hyoscine butyl bromide for the treatment of cramping abdominal pain and other clinical indications [3,4]. The first of these analyzed 10 placebo-controlled studies that examined the effectiveness and safety of oral and rectal administration of hyoscine. The effectiveness of the drug was established in all studies, which is considered by the authors as evidence supporting the use of the drug for abdominal pain associated with cramps [3]. The second review provides evidence on the use of GBB for the treatment of colic/spasm; to improve diagnostic testing; for parenteral administration for the treatment of biliary and renal colic, spasms of the genitourinary tract; as well as during childbirth and as palliative treatment. The author concluded that hyoscine butylbromide is fast-acting and highly effective and well tolerated, which supports its use in a range of indications related to acute abdominal cramps, labor and delivery for palliative care, and diagnostic and therapeutic abdominal procedures. which can be difficult with spastic contractions [4]. The effect of hyoscine butylbromide has also been studied for abdominal pain caused by a functional disorder. A double-blind, randomized, parallel-group comparative study was conducted, which included 712 patients with IBS. Patients for 4 weeks. hyoscine butyl bromide + paracetamol, hyoscine butyl bromide, paracetamol or placebo were prescribed. The VAS was used to assess symptoms. By the end of treatment, more than 75% of patients in the hyoscine butyl bromide group experienced symptom relief [5]. There was a statistically significant decrease in the intensity of abdominal pain in the hyoscine butyl bromide group compared to placebo and paracetamol. Renal colic L.A. Samuels cites 6 studies involving 755 patients that evaluated hyoscine butylbromide as an adjunctive analgesic (along with morphine and indomethacin) compared with placebo, nonsteroidal anti-inflammatory drugs (NSAIDs), and other antispasmodics. It was concluded that hyoscine butyl bromide is effective in the treatment of renal colic, either alone or in combination with opioids and NSAIDs. It should be noted that the speed of onset and duration of the analgesic effect is better when prescribing NSAIDs. Dysmenorrhea LA Samuels reviews 2 studies using hyoscine butyl bromide for primary and secondary dysmenorrhea. In the first double-blind crossover study of 120 women, hyoscine butylbromide and paracetamol were compared with lysine clonixinate and proprinox and placebo. Both treatment groups showed a significant reduction in subjective pain ratings compared to placebo. A long-term, open-label study examined the combined use of lysine clonixinate and hyoscine butyl bromide during 3 consecutive menstrual cycles in 30 women. Women initially reported very severe (10.7%), severe (42.9%) or moderate (46.4%) pain. By the end of the study, moderate pain persisted in only 1 patient. Labor Some authors have studied the effects of hyoscine butyl bromide as a labor accelerator, with the argument that if labor pain cannot be safely eliminated, then the duration of labor (and therefore labor pain) may be safely reduced. The use of hyoscine butyl bromide led to a statistically and clinically significant reduction in the period between drug administration and delivery in the absence of significant adverse reactions on the part of the mother or newborn. Abdominal pain and discomfort during diagnostic procedures In 3 studies, the effectiveness of hyoscine butylbromide compared with placebo (2 studies; 208 patients) and glucagon (1 study; 100 patients) was assessed during sigmoidoscopy and/or colonoscopy. When compared with placebo, a reduction in the duration of the procedure was proven in the group receiving hyoscine butyl bromide [6]. Comparison with glucagon favored the latter for facilitating the endoscopic procedure. There is evidence that intramuscular administration of hyoscine butyl bromide improves image quality in magnetic resonance imaging of the abdominal cavity [7]. It was found that magnetic resonance imaging of the liver and pancreas is slightly better when gastrointestinal motility is reduced by hyoscine butyl bromide. IBS is one of the functional disorders of the gastrointestinal tract, which has enormous medical and social significance. Internists and gastroenterologists most often select drug treatment for abdominal pain specifically in IBS. In this regard, a systematic review and meta-analysis by AC Ford, NJ Talley, BM Spiegel et al. is of great interest. . IBS is characterized by abdominal pain and discomfort and is associated with changes in bowel habits and frequency. According to epidemiological studies, the incidence of IBS in the population ranges from 5 to 20%. The exact cause of IBS remains unknown, although a number of pathological mechanisms have been proposed. Impaired gastrointestinal motility leads to changes in the nature and frequency of stool in some patients. Smooth muscle spasm, visceral hypersensitivity and features of central pain perception underlie the most important symptom of IBS - abdominal pain. There is no doubt that IBS is a chronic condition that is prone to recurrence, which requires effective, simple and safe treatments. Some drugs that had a well-defined mechanism of action to normalize motility in IBS were banned due to their serious side effects. Traditionally, IBS patients have been advised to increase their intake of dietary fiber, which is thought to have a beneficial effect on intestinal transit time. To relieve pain and a feeling of fullness in the abdomen, various antispasmodics are used. Peppermint oil, according to several studies, also has an antispasmodic effect and is an over-the-counter remedy for IBS. Data from clinical studies on the effectiveness of treatment for IBS are usually contradictory; it can be difficult to objectively assess the superiority of one of the compared treatment methods. The findings from systematic reviews were also mixed. Various approaches underlie recommendations for the treatment of patients with IBS. AC Ford, NJ Talley, BM Spiegel, et al. undertook a literature review of Medline (1950 to April 2008) and Embase (1980 to April 2008), the Cochrane Register of Controlled Trials (2007): studies in adult patients with IBS compared fiber, antispasmodics and peppermint oil with placebo or no treatment. The purpose of the systematic review was to determine the effectiveness of fiber, antispasmodics, and peppermint oil in the treatment of IBS. From 615 literary sources, 35 controlled studies were selected for analysis: 9 of them assessing the effectiveness of fiber, 19 of antispasmodics, 3 of fiber and antispasmodics, 4 of peppermint oil. The primary outcome of the systematic review assessed the effectiveness of fiber, antispasmodics, and peppermint oil compared with placebo or no treatment in relieving core symptoms of IBS or abdominal pain after treatment. The duration of treatment was 4 weeks when fiber was prescribed. up to 4 months, antispasmodics – from 1 week. up to 6 months, mint oil – from 4 weeks. up to 3 months The secondary result is to determine the effectiveness depending on the type of fiber or antispasmodic drug and the safety of therapy. Treatment effect was expressed as a relative risk, with a 95% confidence interval estimate of the core symptoms of IBS or abdominal pain persisting with fiber, antispasmodics, and peppermint oil. In 12 studies of 591 patients, 155 (52%) of 300 people given fiber had symptoms that persisted after treatment, compared with 168 (57%) of 291 people given a placebo or low-fiber diet. Thus, the relative risk of persistent symptoms was 0.87 (95% CI 0.76–1.00, p = 0.05), the number of patients who needed to be treated (with fiber to prevent the persistence of symptoms) reached 11 (95% CI 5–100). It is important to note that a separate analysis of the effectiveness of a fiber source such as bran failed to prove their effectiveness (relative risk was 1.02; 95% CI 0.82–1.27), in contrast to psyllium preparations as a source of fiber (0 .78; 95% CI 0.63–0.96). In an analysis of 4 studies (392 patients), 52 of 197 patients (26%) remained symptomatic compared with 127 (65%) of 195 placebo-treated patients. The relative risk of symptom persistence with peppermint oil was 0.43 (95% CI 0.32–0.59). Of greatest interest is the part of the meta-analysis by AC Ford, NJ Talley, BM Spiegel et al., which is devoted to assessing the role of antispasmodics in the treatment of IBS. A total of 22 studies of 12 different antispasmodic drugs were analyzed, which included 1778 patients. Of the drugs with antispasmodic properties currently available to domestic doctors, this review included studies of otilonium, hyoscine butyl bromide, pinaverium, trimebutine, alverine and mebeverine. Overall, 350 (39%) of 905 patients treated with antispasmodics had persistent IBS symptoms, compared with 485 (56%) of 873 in the placebo group: relative risk 0.68 (95% CI 0.57–0.81) . The number needed to treat to prevent persistent IBS symptoms was 5 (95% CI 4–9). When analyzing specific antispasmodic drugs, the best performance indicators were found to be otilonium and hyoscine. In 4 studies of otilonium (435 patients), IBS symptoms persisted in 111 (51%) of 216 patients receiving an antispasmodic, compared with 155 (71%) of 219 receiving placebo: relative risk was 0.55 (95% CI 0. 31–0.97), and the number of patients required for treatment is 4.5 (3.0–10.0). In 3 studies (426 patients) with hyoscine, persistence of IBS symptoms was detected in 63 (29%) of 215 patients compared with 97 (46%) of 211 receiving placebo. The relative risk of persistent IBS symptoms was calculated as 0.63 (95% CI 0.51–0.78). It was with the use of hyoscine butylbromide that the lowest number of patients who needed to be treated to prevent the persistence of symptoms in 1 patient was obtained - 3.5 (2.0–25.0). Some characteristics of the hyoscine butyl bromide studies are presented in Table 1. The total number of patients in 3 studies exceeded 400, and in each of them hyoscine butyl bromide was significantly more effective than placebo. It should be noted that in 1 study the duration of hyoscine administration was 1 month, and in 2 others - 3 months, which indicates that the drug was well tolerated. As recommended by the authors of the systematic review, it makes sense for a general practitioner considering treatment of IBS with antispasmodics to start with hyoscine butylbromide as first-line therapy, with other antispasmodics in mind only if such treatment fails. Three studies using trimebutine (140 patients) were analyzed. In 28 patients (40%) of 70 who used trimebutine, the main symptoms of IBS and abdominal pain persisted, compared with 27 (39%) of 70 patients on placebo. The calculated relative risk was 1.08 (95% CI 0.72–1.61), which did not confirm the effectiveness of trimebutine in treating the main symptoms of IBS. According to data from 13 studies (1379 patients), conclusions were drawn about adverse events while taking antispasmodics. A total of 101 patients (14%) of 704 reported adverse events when taking antispasmodics, compared with 62 (9%) of 675 patients in the placebo group. None of the studies reported serious adverse events. The most common symptoms were dry mouth, dizziness, and blurred vision. The relative risk of adverse events was 1.62 (95% CI 1.05–2.50), the number of patients at risk of harm was 17.5 (7.0–217.0). Thus, hyoscine butylbromide has a dual effect - antispasmodic and antisecretory. He demonstrated his effectiveness with spastic abdominal pain, biliary colic, spasms of the esophagus, and IBS. Its effect is proven “outside the gastrointestinal tract” - with renal colic, dysmenorrhea, childbirth. Guouscin Butilbroomide improves the quality of such a diagnostic study as magnetic resonance imaging, and eliminates pain and spasm with colonoscopy and sigmoscopy.
Abstract prepared by Ph.D. ON THE. Lyutov 1 Moscow State Medical University named after I.M. Sechenov
References 1. Americo MF, Miranda JR, Cora LA,. Romeiro FG Electrical and mechanical effects of hyoscine butylbromide on the human stomach: a non–invasive approach // Physiol Meas. 2009. Vol. 30(4). R. 363–370. 2. Mueller–Lissner S., Tytgat GN, Paulo LG et al. Placebo– and paracetamol controlled study on the efficacy and tolerability of hyoscine butylbromide in the treatment of patients with recurrent crampy abdominal pain // Aliment Pharmacol Ther. 2006. Vol. 23 (12). R. 1741–1718. 3. Tytgat GN Hyoscine butylbromide: a review of its use in the treatment of abdominal cramping and pain // Drugs. 2007. Vol. 67(9). R. 1343–1357. 4. Tytgat GN Hyoscine butylbromide – a review on its parenteral use in acute abdominal spasm and as an aid in abdominal diagnostic and therapeutic procedures // Curr Med Res Opin. 2008. 5. Schafer E., Ewe K. The treatment of irritable colon. Efficacy and tolerance of buscopan plus, buscopan, paracetamol and placebo in ambulatory patients with irritable colon // Fortschr Med. 1990. Vol. 108 (25). R. 488–492. 6. Saunders BP, Elsby B., Boswell AM, Atkin W., Williams CB Intravenous antispasmodic and patient-controlled analgesia are of benefit for screening flexible sigmoidoscopy // Gastrointest Endosc. 1995. Vol. 42(2). R. 123–127. 7. Wagner M., Klessen C., Rief M. et al. High-resolution T2-weightedabdominal magnetic resonance imaging using respiratory triggering: impact of butylscopolamine on image quality // Acta Radiol. 2008. Vol. 49(4). R. 376–382.
Other aspects[edit]
tert-
Butyl bromide used to study mass deadenylation of adenine-based nucleosides induced by halogenated alkanes (alkyl halides) under physiological conditions. 2-Bromo-2-methylpropane causes massive deguanylation of guanine-based nucleosides and massive deadenylation of adenine-based nucleosides. [4]
Phase transition from orthorhombic phase III Pmn21 at low temperatures (measured from 95 K) to disordered rhombohedral phase II at 205-213 K. Phase II can exist at 213-223 K, partially coinciding with fcc phase I, which can be observed between 210 -250 K. Phase transitions were also studied at high pressure (up to 300 MPa) [5]
Links[edit]
- "2-Bromo-2-methylpropane - Compound Summary". PubChem Compound
. USA: National Center for Biotechnology Information. March 26, 2005 Identification. Retrieved June 16, 2012. CS1 maint: discouraged parameter (link) - CRC Handbook of Chemistry and Physics 65th ed.
- Reiners, Matthias; Ehrlich, Niko; Walter, Mark D. (2018). “Synthesis of 1,3,5-tri- tert-
butylcyclopent-1,3-diene and its metal complexes Na {1,2,4-(Me 3 C) 3 C 5 H 2 } and Mg {η 5 -1, 2.4- (Me 3 C) 3 C 5 H 2 ) 2 “.
Inorganic syntheses
.
37
: 199. DOI: 10.1002/9781119477822.ch8. - "2-Bromo-2-Methylpropane 135615." H2NC6H4CO2C2H5, drugs, www.sigmaaldrich.com/catalog/product/aldrich/135615?lang=en®ion=US.
- "Structures of 2-bromo-2-methylpropane". Cambridge Structural Data Center (CCDC), www.ccdc.cam.ac.uk/structures/search?id=doi:10.5517/ccvcqmj&sid=DataCite