Dimephosphon®
Dimephosphone is taken orally after meals with water.
The course of treatment depends on the nature of the disease and lasts from 3 days to 2 months.
In complex therapy of the following diseases and conditions:
For acute and chronic cerebrovascular accidents, consequences of ischemic and hemorrhagic strokes,
traumatic brain and neurosurgical trauma
for adults, 15 ml (1 tablespoon) 3-4 times a day. The duration of the course is 2-3 weeks, in some cases up to 6 weeks.
During planned neurosurgical operations
15 ml (1 tablespoon) for 5 days before and 2 months after surgery.
For osteochondrosis
adults: 10 ml (1 dessert spoon) 3-4 times a day for 2-3 weeks, improvement is observed on the 8-10th day of treatment.
For multiple sclerosis
adults: 100 mg/kg (45 ml) per day - 15 ml (1 tablespoon) 3 times a day for 10 days in the autumn-spring period monthly.
For chronic nonspecific lung diseases with signs of respiratory and pulmonary heart failure
adults: 15 ml (1 tablespoon) 3-4 times a day. Course - 7-10 days. The use of dimephosphone does not relieve asthma attacks and does not affect the frequency of use of beta-agonist aerosols.
For vegetative-vascular dystonia of the parasympathetic type
adults 15 ml (1 tablespoon) 3 times a day for 2-3 weeks, children over 12 years old 50 mg/kg (10-15 ml) 3 times a day for 3 weeks.
For chronic cerebrovascular insufficiency due to atherosclerosis and hypertension
15 ml (1 tablespoon) 3 times a day for 2-3 weeks.
For migraine
15 ml (1 tablespoon) 3 times a day for 2-3 weeks.
For Meniere's disease
15 ml (1 tablespoon) 3 times a day for 3 weeks.
For respiratory diseases, acidosis, atonic bronchial asthma and hay fever
adults are prescribed 15-25 ml, children are prescribed 15-25 ml, children are prescribed a dose of 75-100 mg/kg: children under 3 years old - 5 ml (1 teaspoon), 3-8 years old - 10 ml (1 dessert spoon), over 8 years old - 15 ml (1 tablespoon) 3 times a day, in severe cases - 4 times a day for 4-5 weeks.
For atonic bronchial asthma in combination with hay fever
prescribed 2-3 weeks before the onset of deterioration and taken throughout the entire flowering period. For dosing, you can use the measuring cup included in the package.
Externally
For infectious-inflammatory-allergic diseases of the skin and mucous membranes
in the form of bandages, turundas and lotions with a solution daily for
3-14 days.
For complex treatment of acne
wipe the skin 3-4 times a day, apply lotions in the evening.
With erysipelas
- lubricate the inflammation area 3 times a day for 3-5 days.
On the area of seams and places where the knitting needles exit
Apply gauze pads soaked in dimephosphone daily for 7-14 days.
For the prevention of radiation mucositis
- gauze wipes soaked in dimephosphone are placed in the projection of the radiation beams 20 minutes before dose exposure.
Possibilities of using the drug Dimephosphone in neurology and neurosurgery
The original domestic drug Dimephosphone (dimethyloxobutylphosphonyl dimethylate) was synthesized in 1952 by A. N. Pudovik at the Institute of Organic and Physical Chemistry named after. A. E. Arbuzova[1]. It belongs to the group of metabolics and is a dimethyl ester of 1,1-dimethyl-3-oxobutylphosphonic acid, which has anti-acidotic and antioxidant effects. Dimephosphone has been produced since 1983; during clinical use, vaso- and neurotropic activity of the drug was also discovered.
The antioxidant effect is realized by preventing the activation of lipid peroxidation and increasing the activity of antioxidant enzymes in brain tissue [8].
Dimephosphone enhances energy processes in the brain both directly - acting directly on mitochondria - and indirectly - by stimulating and increasing tissue consumption of thyroid hormones, which is accompanied by activation of energy and catabolic processes in cell mitochondria. It also exhibits the properties of some neurotransmitters: it has GABAergic, N-cholinergic and dopaminergic activity.
The anti-acidotic effect of the drug is realized through the intensification of the renal and pulmonary mechanisms for regulating the acid-base state, enhancing intraorgan blood flow and tissue metabolism. In addition, when using Dimephosphone, the content of lactic and pyruvic acids in brain tissue decreases. Unlike known anti-acidotic drugs, which directly affect the acidity of the blood by introducing an appropriate alkaline solution, the drug produces its effect by interfering with metabolic processes.
One of the most valuable properties of Dimephosphone is its ability to influence the mechanisms of regulation of cerebral circulation and the function of the nervous system. It has been experimentally established that the drug reduces the phenomena of circulatory hypoxia, improves the regulation of cerebral circulation, normalizes the reactivity of cerebral vessels and blood supply to the brain and improves venous outflow. In addition, Dimephosphon normalizes neuromediation, has a beneficial effect on the electrical activity of the brain, and restores the sleep-wake cycle [1].
Recently, electrophysiological studies at the neuromuscular junction demonstrated that Dimephosphone has ion channel blocking properties. This explains why it, like phenytoin, exhibits anticonvulsant and antiarrhythmic activity. The channel blocking property of Dimephosphone may be directly related to the calcium-dependent effects of this drug [2].
The drug is available in the form of a 15% solution for oral administration in bottles of 100 and 200 ml.
The presence of vasoactive, neuroprotective, antioxidant, antihypoxic and neurotropic effects of Dimephosphone justifies the possibility of its use in various forms of cerebral pathology. Over more than 30 years of use of Dimephosphone in practical medicine, numerous clinical studies have been conducted that have demonstrated its effectiveness in various forms of pathology of the nervous system.
A long-term experimental clinical study assessing the effectiveness of Dimephosphone in the treatment of victims with TBI was conducted in Kazan[6]. Over 7 years, 2324 patients with severe TBI were treated in the intensive care unit, whose treatment regimen included Dimephosphone. When comparing the processes of restoration of consciousness and reflexes with and without the use of the drug, faster positive dynamics were noted in relation to the emergence of consciousness, restoration of adequacy of behavior and reflexes in patients receiving Dimephosphone. When using Dimephosphone, the normalization of respiration and systemic hemodynamics accelerated, the drug contributed to the rapid regression of focal brainstem and hemispheric symptoms. As a result, a decrease in the average mortality rate in patients with severe TBI was recorded to 27% versus 38.6% in the previous period, when Dimephosphone was not part of the course of treatment. Thus, the inclusion of Dimephosphone in the complex treatment of patients with severe TBI led to a reduction in mortality by 30%.
In 1994, the results of a study assessing the effect of Dimephosphone on the cerebral circulation regulation system in patients with brain tumors were published[5]. We observed 53 patients aged from 5 to 66 years with tumors of various histological structures of supra- and subtentorial localization who received monotherapy with Dimephosphone. It has been shown that a five-day course of treatment with Dimephosphone (30 mg/kg orally 3 times a day) in the preoperative period improves the regulation of cerebral circulation in patients with cerebral tumors. The drug restored the linear velocity of blood flow in the internal jugular veins and the impaired reactions of pulse blood filling to a unified anti-orthostatic load. At the same time, the reactions of the internal carotid arteries and basilar artery to stress with carbogen inhalation were normalized. In conditions of high intracranial pressure caused by an additional volumetric tumor process, liquor hypertension and cerebral edema, the use of the drug led to the restoration of the activity of regulatory mechanisms of circulatory support of both chemical and physical homeostasis and increased their tolerance to surgical trauma. During the treatment, a decrease in motor and speech disorders, easing of headaches, improved sleep, and stabilization of hemodynamics and breathing were noted.
In patients who received Dimephosphone before surgery, by the end of the first day, normal reactivity of cerebral vessels was recorded near the area of surgical intervention, in contrast to patients who did not receive Dimephosphone as a preoperative pharmacological correction [5].
Dimephosphone also demonstrated a good effect in the treatment of 49 patients with cerebrovascular accidents caused by surgical trauma and thrombosis of the internal carotid arteries[12]. Patients took 15 ml of the drug 3 times a day for 14 days. In cases of cerebrovascular accidents caused by surgical trauma, rapid regression of neurological disorders occurred during a course of drug use. Dimephosphone relieved headaches caused by vasospasm well. In cases of severe spasm of the peripheral parts of the middle cerebral artery, transcranial Dopplerography revealed a decrease in elevated values of systolic and average blood flow velocity and normalization of the systolic-diastolic ratio. Using the hydrogen clearance method, the normalizing effect of Dimephosphone on the initially low reactivity of cerebral vessels was revealed.
In patients with consequences of thrombosis of the internal carotid arteries, motor and speech disorders decreased during a course of use of Dimephosphone. At the same time, the drug effectively eliminated migraine-like headaches. The duration of the analgesic effect with a single dose was up to three hours. Dimephosphone was well tolerated by patients: no side effects from the gastrointestinal tract were noted, there were no local or allergic reactions[12].
Based on the Research Institute of Neurosurgery named after. N. N. Burdenko assessed the effect of Dimephosphone on the functional state of stem structures in neurosurgical patients in the early postoperative period [15]. In patients after removal of tumors of the hypothalamic-pituitary and pontobulbar localization with a clinical picture of transient ischemic brain damage, impaired consciousness with intact central mechanisms of visceral-autonomic regulation, the use of Dimephosphone in a daily dose of 40–60 mg/kg provided regression of cerebral and focal symptoms starting from 2–3 -th day from the start of therapy. At the same time, there was a tendency towards normalization of the EEG pattern.
In patients with tumors of the hypothalamic-pituitary localization who received Dimephosphone, in comparison with the control group, where this drug was not used, there was a tendency to more rapid restoration of circulating blood volume after surgery, which was probably due to the normalization of the functions of the paraventricular nuclei of the hypothalamus. In case of tumors of the fourth ventricle, the use of Dimephosphone made it possible to prevent the development of heart failure of central origin. A similar stress-protective effect of Dimephosphone was observed in patients in the acute period of TBI, and it was most pronounced with symptoms of damage to the midbasilar structures of the brain. In patients receiving Dimephosphone, there was a tendency to reduce the depth of disturbance of consciousness [15].
In 1996, the results of the use of Dimephosphone in the treatment of Meniere's syndrome were published[16]. In a hospital setting, 30 patients aged 26 to 70 years received monotherapy with the drug in a daily dose of 45 ml for 2–3 weeks. The duration of observation of the treated patients was 1.5 years. A stable positive effect was observed in 67% of patients. At the same time, the best results were observed with a relatively short duration of the disease (up to 5 years), unilateral damage to the labyrinth, and vestibular disorders at the onset of the disease. With the “cochlear” onset of the disease, the effectiveness of treatment was 50%. The data obtained on the positive effect of Dimephosphone in patients with damage to the peripheral part of the cochleovestibular analyzer due to hydrops of the labyrinth are most likely associated with the anti-acidotic effect of the drug, as well as with its beneficial effect on microcirculation in the vessels of the vertebrobasilar system.
According to the results of a clinical trial of the drug Dimephosphon [11], in patients with vegetative dystonia syndrome, its three-week course led to an improvement in subjective status: patients had reduced headaches and dizziness, improved sleep, and smoothed out the phenomena of hypochondria and irritability. Manifestations of angiodystonia decreased, pulse and blood pressure levels stabilized. A tendency towards leveling cerebral vascular dystonia was observed in the results of rheoencephalography. Among patients suffering from migraine, relief of headache attacks under the influence of Dimephosphone was not observed; the frequency of attacks remained unchanged throughout the entire period of taking the drug. At the same time, in the interictal period, most patients noted a subjective improvement in their condition: neurosis-like layers disappeared, sleep improved, and senestopathic manifestations decreased.
The effect of Dimephosphone on the dynamics of neurological deficit in patients with diseases of the spinal cord and its roots has been studied[7]. Dimephosphone was prescribed orally 15 ml (2.25 mg) 3-4 times a day for 2-3 weeks. In 14 patients with radiculopathy, after removal of a herniated disc, on the 3rd–4th day of treatment with the drug, radicular pain and numbness in the projection of the dermatomes of the affected roots disappeared. In cases of spinal circulation disorders caused by dyscirculatory myelopathy, under the influence of Dimephosphone, organic disorders were significantly reduced: paraparesis regressed and the functions of the pelvic organs were restored.
The authors also provide the results of treatment of a patient with lower paraplegia after total removal of an extramedullary spinal cord tumor. During treatment with Dimephosphon, rapid regression of motor disorders, warming below the upper level of conduction disorders and a decrease in leg pain were noted [7].
The results of treatment of patients with chronic cerebral circulatory disorders in the vertebrobasilar region aged from 26 to 60 years who took Dimephosphone for 3 weeks were analyzed[10]. In vertebrobasilar vascular insufficiency, Dimephosphone reduced headaches, dizziness, tinnitus, gait instability, and also improved memory and concentration. The corrective effect of Dimephosphone in the vertebrobasilar area was associated with inhibition of the development of tissue edema and improvement of the rheology of circulating erythrocytes. The drug smoothes shifts in the microblood supply of the spinal cord and medulla oblongata and has an antihypoxic effect on brain structures.
Studies conducted at the Kazan State Medical Academy found that Dimephosphone can have a beneficial effect on the clinical course of multiple sclerosis [9]. The researchers observed 21 patients with the cerebral form of multiple sclerosis, whose average age was 32.6 years. Dimephosphone was administered orally at a dose of 15 ml (2.25 mg) 3 times a day for 10 days. Clinical improvement was observed in 16 patients (76.2%). Subjectively, it was expressed in improved well-being and increased mood. Objectively, there was a decrease in tremor and unsteadiness when walking. In a number of cases, nystagmus disappeared and strength in the legs increased. Proprioceptive reflexes improved, and in some cases spasticity decreased. There were no side effects or worsening of the disease while taking the drug.
The effectiveness of Dimephosphone in patients with ischemic stroke and dyscirculatory encephalopathy (DE) was studied by the team of the Central Military Clinical Hospital named after. P. V. Mandryka (Moscow)[4]. For 20–25 days, 50 patients aged 64–80 years with this form of cerebral pathology took Dimephosphone orally at a daily dose of 45 ml. While taking the drug, headaches and dizziness decreased or completely stopped, and memory also improved. In a number of cases, the clinical manifestations of acute vestibular syndrome disappeared. When performing ultrasound echopulsography of the main artery, an increase in its lumen was noted while taking Dimephosphone. At the same time, the drug, without having a pronounced vasodilator effect, had a positive effect on the metabolism of ischemic brain tissue. The treatment was well tolerated by the patients.
On the basis of the Institute of Clinical and Experimental Neurology named after. P. M. Sarajishvili (Georgia) conducted a study of the effectiveness of the drug Dimephosphone in acute and chronic vascular diseases of the brain in comparison with cinnarizine [13]. We observed 54 patients with acute cerebrovascular accidents (ischemic and hemorrhagic strokes) and 102 with chronic ones.
Dimephosphone turned out to be more effective against manifestations of vestibular dysfunction in both acute and chronic cerebrovascular accidents. In patients with cerebral stroke during therapy with Dimephosphone, after 3–4 days the general condition improved and focal symptoms decreased. Positive dynamics were more often observed when the lesion was localized in the vertebrobasilar region. In 42.6% of cases of ischemic stroke, complete recovery was recorded. In chronic cerebrovascular accidents, already on the 2nd–3rd day of taking Dimephosphone, a decrease in both subjective vestibular disorders and objective ones was observed: nystagmus, vestibular hypo- or hyperreflexia, imbalance in simple and sensitized Romberg poses. Compared with the use of cinnarizine, regression of the vestibulo-atactic syndrome when taking Dimephosphone occurred in a shorter time and was more persistent[13].
In order to assess the possibility, effectiveness and safety of using the drug Dimephosphon in patients with DE in 2013 at the Department of Nervous Diseases of the Institute of Professional Education of the First Moscow State Medical University named after. I.M. Sechenov conducted an open comparative study to study the effectiveness of three methods of treating non-motor manifestations of DE: monotherapy with Dimephosphone, the use of Dimephosphone in combination with vinpocetine, as well as the isolated use of vinpocetine [14].
MATERIALS AND METHODS
The study involved 58 patients with different stages of DE. The average age of the patients was 70.4 ± 7.0 years (from 60 to 83 years); There were 13 men, 45 women. The first stage of DE was present in 8.6%, the second stage in 84.5%, and the third stage in 6.9% of patients.
Depending on the treatment method, three groups of patients were formed: monotherapy with vinpocetine (n = 20), monotherapy with Dimephosphone (n = 20) and combined treatment with Dimephosphone and vinpocetine (n = 18). The groups did not have statistically significant differences in age and gender composition, as well as in the severity of DE.
Dimephosphone was prescribed at a dose of 45 ml/day, vinpocetine at a dose of 15 mg/day. When taken in combination, patients took Dimephosphone together with vinpocetine. The course of taking the drugs was 21 days.
Before treatment, all patients were assessed for cognitive performance using the Mini-Mental State Examination (MMSE), emotional status using the Hospital Anxiety and Depression Scale, and sleep quality using the Subjective Sleep Characteristics Questionnaire. Repeated testing on the same scales was performed on the 21st day of treatment, and the results were entered into the patients’ outpatient records.
Statistical analysis used the Pearson Chi-square test with Bonferroni correction for multiple comparisons. Differences in indicators between groups were considered statistically significant at p values <0.05.
RESULTS
The table shows comparative data between the study groups by the number of patients who received improvement in any of the non-motor indicators assessed. Responders were determined by the total scores of the corresponding questionnaires; a change of more than 0% was considered an improvement.
Table Number of patients with improvement in non-motor manifestations of dyscirculatory encephalopathy during treatment, n (%)
* The differences between the group of patients taking only Dimephosphone and the group of vinpocetine monotherapy are statistically significant (p < 0.05).
** The difference between the group of patients taking Dimephosphone with vinpocetine and the group of vinpocetine monotherapy is statistically significant (p < 0.05).
Note. Responders for individual non-motor indicators were determined by a change in the total scores of the corresponding questionnaires by more than 0%.
As can be seen from this table, in the groups of patients receiving Dimephosphone as monotherapy and Dimephosphone together with vinpocetine, there was a greater number of responders on all scales. Monotherapy with Dimephosphone contributed most to improving subjective assessment of sleep and reducing anxiety levels. The combined use of Dimephosphone and Vinpocetine was accompanied by the most pronounced positive dynamics of indicators on the MMSE scale and the level of depression on the hospital scale.
During the treatment period, some patients receiving only Dimephosphone complained of stomach pain and heartburn, but these sensations did not require discontinuation of the drug. When taking Dimephosphone with vinpocetine during the course of treatment, a single increase in blood pressure to 160 mm Hg was observed. Art. (in one patient), stomach pain (in two patients), heartburn and staggering when walking (in one patient). No side effects were observed with the isolated use of vinpocetine.
DISCUSSION
The results obtained in this study confirmed the effectiveness of Dimephosphone in the treatment of non-motor manifestations of DE. The effect of Dimephosphone, a drug belonging to the group of antiacidotic drugs, turned out to be comparable to the effect of vinpocetine, a “classical” vasodilator that improves cerebral circulation. It is known that the main mechanism of action of vinpocetine on cerebral blood flow is its antivasoconstrictor effect [17]. This effect is realized by blocking vascular noradrenergic reactions. The clinical effect of Dimephosphone is determined by the normalization of the acid-base state in acidosis of various etiologies, due to which the drug has a vasoactive, antioxidant and membrane-stabilizing effect. In our study, the use of Dimephosphone in patients with chronic cerebrovascular insufficiency for 21 days was accompanied by a statistically significant (p < 0.05) improvement in cognitive functions and sleep indicators, as well as a decrease in anxiety levels.
Among the non-motor disorders assessed, the use of Dimephosphone resulted in the greatest improvement in subjective sleep characteristics. This observation seems to us very important, since elderly and senile patients are characterized by a high prevalence of sleep disorders [3]. Improving the quality of sleep when taking Dimephosphone may help reduce the dose of sleeping pills already taken, the use of which among patients in older age groups should be limited due to undesirable side effects.
The greatest degree of reduction in non-motor disorders in chronic cerebrovascular insufficiency was observed during combination treatment with Dimephosphone in combination with vinpocetine. Along with improvements in sleep indicators, cognitive functioning and a decrease in anxiety levels, a decrease in depression levels was also observed during combination therapy.
The study showed good tolerability of the drug Dimephosphone. Side effects were noted in only 12% of cases. Symptoms of upper gastrointestinal irritation—stomach pain and heartburn—were observed. All adverse reactions were mild and did not require drug discontinuation or corrective therapy. In general, the data on the tolerability of Dimephosphone obtained in our work are comparable with the results of the mentioned studies and the data of the review by L. Z. Podorozhanskaya et al. (1996)[4, 7, 9, 11–13].
CONCLUSION
The presented results of the use of Dimephosphone, including data obtained in our own study, demonstrate the presence of a clinically significant effect of the drug in various forms of CNS pathology. More than 30 years of history of the use of Dimephosphone in domestic neurology and neurosurgery allows us to state the presence of diverse medicinal effects of the drug and a high level of safety of its use.
Introduction
Autonomic dysfunction is a common syndrome characterized by a wide range of multisystem autonomic disorders, often combined with anxiety. In these cases, patient complaints of decreased memory, attention, and thought processes, which impede professional and social activities, are obligatory. In this regard, when choosing a drug for the treatment of anxiety-associated autonomic dysfunction, it is necessary to take into account, in particular, its effect on cognitive functions.
Many of the psychotropic drugs used to treat anxiety relieve vegetative symptoms well, but can aggravate cognitive impairment, which reduces the patient’s satisfaction with the treatment effect, increasing his maladjustment. In this regard, it is important to use drugs that do not have anticholinergic and muscle relaxant effects. These requirements are met by the drug mebicar, a synthetic compound (a derivative of bicyclic biureas) with tranquilizing ability [1]. Mebicar reduces feelings of anxiety, restlessness, reduces irritability, and has a mild sedative effect. The targets for the action of mebikar are the structures included in the limbic-reticular complex and the emotional zones of the hypothalamus. The wide range of pharmacological effects of mebicar is explained by its integrative effect on the serotonin, adrenergic, cholinergic and GABAergic systems. Along with the main stress-protective and anxiolytic effect, the drug has a pronounced nootropic effect: improves memory, mental functions, increases logic, coherence and speed of thinking, improves attention and mental performance, helps normalize mental functions in general under conditions of stress and overload. Mebicar does not have a muscle relaxant effect and does not impair coordination, which significantly distinguishes it from benzodiazepine tranquilizers [1-5]. Mebicar improves the quality of sleep, facilitating the process of falling asleep, normalizes sleep structure and reduces the frequency of anxious dreams, without having a direct hypnotic effect and without causing daytime drowsiness, which allowed the drug to be classified as a “daytime” tranquilizer. In combination with other psychotropic and hypnotic drugs, Mebicar enhances the hypnotic effect. Additional effects of mebicar are its modulating effect on lipid metabolism, due to the ability to change the ratio of high and low density lipoproteins, which helps reduce the concentration of cholesterol in the blood [6], as well as the ability to improve myocardial trophism by increasing coronary blood flow, reducing blood viscosity and intravascular aggregation erythrocytes [7, 8]. Mebicar does not cause euphoria or addiction. All this justifies the possibility of its use in various fields of medicine, including neurology.
The purpose of the study was to study the effectiveness of Mebikar in patients with autonomic dysfunction combined with anxiety disorder.
Hypothesis: Mebicar, while effectively eliminating symptoms of mild to moderate anxiety and autonomic disorders in patients with autonomic dysfunction, should not have a negative effect on cognitive function.
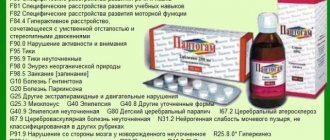
Dimephosphone concentrate for the preparation of intravenous solution 1g amp N 5
Dimephosphone concentrate d/pig solution iv 1g amp N 5
Dosage form
concentrate for the preparation of solution for intravenous administration.
Description
Colorless or yellowish transparent liquid with a peculiar odor.
Compound:
1 ampoule contains:
Active ingredient: dimethyloxobutylphosphonyl dimethylate (Dimephosphon®) – 1.0 g.
Pharmacological properties
Pharmacodynamics
Dimephosphone exhibits anti-acidotic, membrane-stabilizing, anti-inflammatory and antioxidant properties, normalizes blood flow and metabolism of brain tissue, reduces heart and pulmonary failure, improves the regulation of blood circulation, including cerebral circulation.
The anti-acidotic effect is realized due to the intensification of the renal and pulmonary mechanisms of regulation of the acid-base state, increased intraorgan blood flow and tissue metabolism, and dimephosphone also reduces the content of lactic and pyruvic acids in brain tissue.
Dimephosphone stabilizes cell membranes, restoring the reactivity of cerebral vessels, improving the functions of the cerebral hemispheres and the brain stem, reduces the depth of disturbances of consciousness, restores the sleep-wake cycle, reflexes, the arcs of which close through the brainstem, reduces the severity of the pyramidal, cerebellar, vestibular, visual and auditory disorders.
The antioxidant effect is achieved by preventing the activation of lipid peroxidation and increasing the activity of antioxidant enzymes in brain tissue.
Dimephosphone enhances energy processes in the brain both directly, acting directly on mitochondria, and indirectly, stimulating the pituitary-thyroid system, increasing tissue consumption of thyroid hormones, which is accompanied by activation of energy and catabolic processes in cell mitochondria. Shows the properties of some neurotransmitters (GABA-positive, N-cholinergic and dopaminergic activity).
Dimephosphone reduces heart and pulmonary failure by restoring the resistance of peripheral vessels (arterial and venous).
Dimephosphone improves the regulation of cerebral circulation without having a pronounced vasodilator effect, but has a positive effect on the metabolism of brain tissue during ischemia and improves venous outflow. The effectiveness of the clinical use of the drug in various forms of cerebrovascular insufficiency is associated with its ability to increase the resistance of nerve cells to ischemia, reduce edema and, therefore, improve microcirculation.
Pharmacokinetics
Easily passes through histohematic barriers and is distributed to various organs and tissues. The highest concentrations are created in the brain, heart and spleen. Three days after a single administration of dimephosphone, only trace concentrations remain in the body.
Dimephosphone is excreted unchanged mainly in the urine in an amount of 11-15% of the drug (up to 70% of the excreted amount of the drug is excreted during the first 12 hours).
Indications for use
As part of complex therapy:
Chronic cerebrovascular accidents, in the intermediate and long-term period of traumatic brain and neurosurgical injuries, consequences of ischemic and hemorrhagic strokes, Meniere's disease.
Contraindications
Epilepsy, chronic renal failure grade 2 - 3 (creatinine clearance less than 40 ml/min), individual intolerance, children under 18 years of age.
Directions for use and doses
In complex therapy:
Chronic cerebrovascular accidents, in the intermediate and long-term period of traumatic brain and neurosurgical injuries:
intravenous injection - 1 g (1 ampoule) of the drug, diluted in 10 - 20 ml of sterile water for injection or 0.9% sodium chloride solution 1 - 4 times a day for 10 - 14 days;
or intravenous drip - 1 g (1 ampoule) of the drug, diluted in 200 - 400 ml of sterile water for injection or 0.9% sodium chloride solution 1 - 4 times a day for 10 - 14 days.
Consequences of ischemic and hemorrhagic strokes:
intravenously in a stream - 1-2 g (1-2 ampoules) of the drug, diluted in 10 - 20 ml of sterile water for injection or 0.9% sodium chloride solution 1 - 4 times a day for 10 - 15 days;
or intravenous drip - 1-2 g (1-2 ampoules) of the drug, diluted in 200 - 400 ml of sterile water for injection or 0.9% sodium chloride solution 1 - 4 times a day for 10 - 15 days.
Meniere's disease:
intravenously in a stream - 1 g (1 ampoule) of the drug, diluted in 10 ml of 0.9% sodium chloride solution 1 - 3 times a day for 10 days, then it is recommended to continue the course of treatment with the drug Dimephosphon®, solution for oral and external use application, in accordance with the instructions for use.
Side effect
Drowsiness and deterioration in concentration (dissipate by 3–4 days after the first administration of the drug).
Overdose
Symptoms: increased severity of side effects.
special instructions
If drowsiness occurs in the first days of taking the drug, you should refrain from driving vehicles and activities that require increased attention and a high speed of psychomotor reactions.
There have been no strictly controlled clinical studies of the safety of Dimephosphon® in children.
Interaction with other drugs
No interactions with other drugs have been identified.
Use during pregnancy and breastfeeding
Strictly controlled clinical studies of the safety of the use of Dimephosphon® during pregnancy and breastfeeding have not been conducted.
Currently, there is insufficient data on the use of Dimephosphone® concentrate for the preparation of a solution for intravenous administration during pregnancy to assess the teratogenic effect of Dimephosphone.
Taking this into account, the drug Dimephosphon® concentrate for the preparation of a solution for intravenous administration should be prescribed during pregnancy and breastfeeding only if the expected benefit from its use outweighs the potential risk to the fetus or infant.
Animal studies have not revealed any harmful effects on the embryo or its development.
Impact on the ability to drive vehicles and machinery
When using the drug, you should refrain from driving vehicles and activities that require increased attention and reaction speed.
Release form
Concentrate for the preparation of solution for intravenous administration 1.0 g.
1 g of the drug in colorless glass ampoules.
5 ampoules are placed in a blister pack.
1 or 2 strip packaging along with instructions for use are placed in a cardboard box
Storage conditions
In a place protected from light, at a temperature not exceeding 250 C.
Keep out of the reach of children.
Best before date
3 years.
Do not use after the expiration date stated on the package.
Conditions for dispensing from pharmacies
Available with prescription